Abstract
To assess the safety of Transtympanic balloon dilatation of the cartilaginous proximal Eustachian tube under endoscopic guidance as it relates to the integrity of the carotid canal in cadaver model. Endoscopic guided Transtympanic dilatations of the cartilaginous proximal end of the Eustachian tube were performed in 15 ears of 8 fresh frozen cadaver heads. CT scans were done before and after dilatation. Images were reviewed by two otologists and one radiologist. Balloon catheter placement and dilatation of the proximal Eustachian tube was feasible in all specimens. Endoscopic examination post dilatation showed a consistent increase in the aperture of the proximal cartilaginous tube in all ears. Review of CT images after dilatation showed no evidence of trauma to the carotid canal in all ears instrumented. Endoscopically guided Transtympanic dilatation of the proximal Eustachian tube is not associated with damage to the carotid canal in cadaver model.
Level of Evidence: 4.
Keywords: Endoscopic ear surgery, Eustachian tube, Transtympanic balloon dilatation, Carotid canal
Introduction
Balloon dilatation of the Eustachian tube has been reported with a significant degree of success and patient safety [1]. Instrumentation of the Eustachian tube is performed by introducing the balloon catheter through the nasopharyngeal opening of the tube and subsequently dilating the cartilaginous segment of the tube [2]. Safety considerations in regard to avoiding possible injury to the carotid artery have limited the area of instrumentation to the distal end of the tube. Other sites of obstruction in the proximal area of the Eustachian tube had been reported in patients undergoing chronic ear surgery [3, 4]. There has been conflicting evidence as to the safety of the carotid artery when using Transtympanic access to the proximal Eustachian tube [5, 6]. Endoscopic ear surgery allows for access and visualization of the protympanic segment of the Eustachian tube including the carotid canal and possibly allowing safe introduction of the balloon catheter anterior to the visualized carotid [7]. This report assesses possibility of damage to the carotid canal during endoscopically guided Transtympanic Eustachian tube dilatation in cadaver heads.
Materials and Methods
Eight fresh frozen anatomic specimens (transected full cadaver heads) were obtained. Pre instrumentation CT scans were obtained 1 day prior to the procedure. The cadaver specimens were left to thaw for 48 h at room temperature before attempted dilatation. This was based on previous experience from pilot work which showed that intubation of the Eustachian tube is very hard when specimens are not fully thawed. After careful removal of ear canal skin and tympanic membrane, endoscopic evaluation of the protympanic segment of the Eustachian tube is performed using 30°, 3 mm, 15 cm rigid endoscope that is introduced anterior to the handle of malleus. The protympanic segment is then assessed for clear impression of the carotid artery canal, presence of blind pouches and for evidence of obstruction beyond that (Fig. 1). Eustachian tube balloon dilatation catheter (Spiggle & Theis, Overath Germany) is used. The catheter is usually shipped with a metal stylet that runs within the catheter. A 30° deflection is bent at the distal 1 cm of the stylet. The proximal end of the stylet is looped to allow for rotating and orienting the deflection at the distal end towards the opening of the Eustachian tube (Fig. 2). The stylet functions like a guide wire and the catheter is fed into the Eustachian tube over the stylet until it is well within the distal tube. The stylet is then removed. Then the balloon is inflated by infusing saline to 10 bar pressure given on the inflating device. At this point, the catheter is easily moving within the Eustachian tube because the distal end of the tube is much larger than the size of the inflated balloon catheter. Then with the balloon inflated, the catheter is pulled out until it’s lodged at the isthmus, which is much smaller than the inflated balloon catheter and would not allow it to be pulled out. Then the balloon is deflated and pulled by half a cm and inflation is performed again. Given the V shape nature of the tube, the surgeon will experience “catheter pull in” to the nasopharynx as it is inflated. This was used to confirm the location of the catheter within the Eustachian tube (Fig. 3). Then the catheter was pulled in small increments and attempt repeat inflation of balloon, checking for the point where the balloon is lodged and stable within the isthmus without the need to hold on to keep it from advancing as it is being inflated (Fig. 4). The pressure is maintained at 10 bar for 2 min and then deflated and pulled out. The protympanum was then re-examined for assessment of trauma and the opening of the cartilaginous tube. Post dilatation CT was performed and assessed by two otologists and one head and neck radiologist for damage to the carotid canal or any fractures within the protympanum.
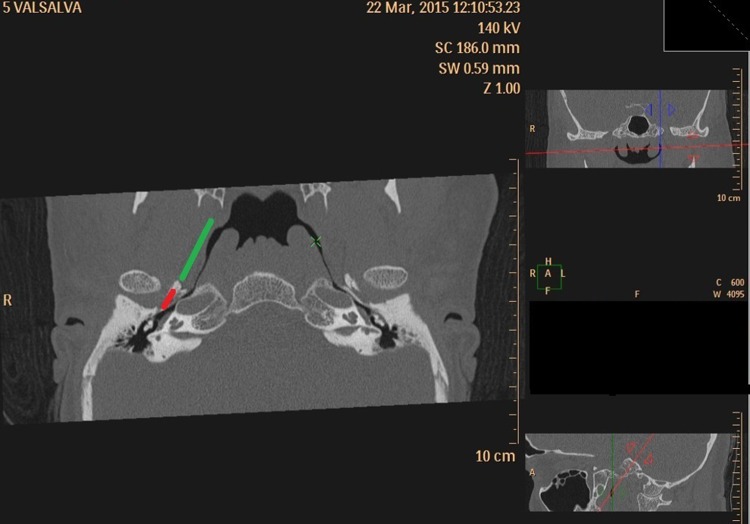
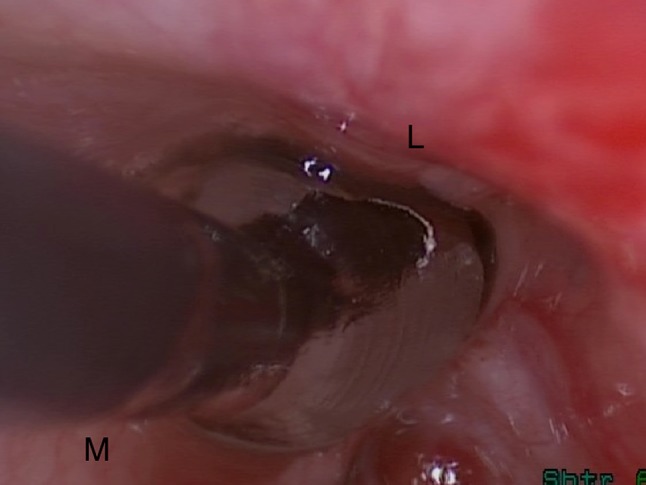
Fig. 1.
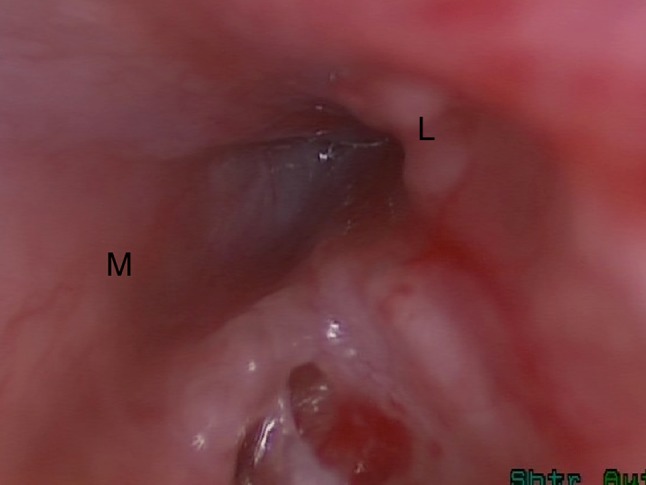
Right ear view of the obstructed protympanic segment of the Eustachian tube. L lateral, M medial
Fig. 2.
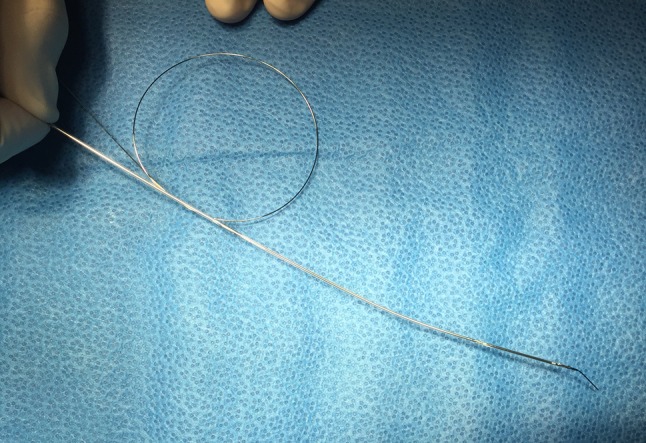
The stylet is angled at its distal end and the proximal end is looped so it can be rotated to direct the distal end angled tip orientation to help directing the catheter toward the opening of the Eustachian tube
Fig. 3.

3D reconstruction of the airspaces in the temporal bone in a Valsalva CT showing the V like shape of the Eustachian tube, and the “catheter pull in” that happens when the balloon is inflated
Fig. 4.
Right ear balloon dilatation of the Eustachian tube using a balloon catheter. L lateral, M medial
Results
All 8 cadaver heads were well preserved through freezing with a near normal quality of the soft tissue. No medical history was available except for negative serological testing for infectious diseases which is done routinely by the specimen supplier. All cadaver specimens were obviously of adults by visual inspection. Pre instrumentation CT scan showed no evidence of dehiscence of the carotid in the protympanum in any of the specimens evaluated. The catheterization procedures described above were performed by multiple practicing otolaryngologists who were instructed on the technique and then supervised and assisted by the second author during hands-on training course on endoscopic ear surgery. 15 dilatations on 8 cadaver heads were performed and we ran out of the balloon catheters for the second side of one specimen. The outline of carotid canal was clearly identifiable in 10 ears, and vaguely identifiable in 6 ears, belonging to 3 anatomic specimens, all bilateral. This seems to relate to degree of pneumatization of the cells surrounding and defining the carotid canal and the tensor tympani muscle bony encasement. Post dilatation, all specimens had visual evidence of dilatation at the proximal cartilaginous opening of the Eustachian tube with no evidence of major trauma. Review of post dilatation CT showed no radiographic evidence of dilatation in the protympanic area. The only radiographic evidence of dilatation was in the distal nasopharyngeal segment of the cartilaginous tube (with air in the dilated tube) which was evident only in 3 ears, two belonging to the same cadaver head. There was no radiographic evidence of disruption to the carotid canal after dilatation in all specimens.
Discussion
Chronic ear surgery has always revolved around removing disease and regaining hearing function without much attention to the pathophysiological process underlying the disease. Since much of the obstruction sites lie out of reach of our traditional instruments, it is always assumed that time and age have resolved any obstruction [3]. Failures in chronic ear surgery have been shown to correlate to persistent Eustachian tube dysfunction [8]. Multiple reports in the literature seem to indicate that the cartilaginous tube and it’s distal segment harbors the site of obstruction [9–11]. However, Linstrom et al. [3] described their experience in using fiber optic flexible mini scopes introduced through the ear during chronic ear surgery to evaluate the patency of the Eustachian tube. Their results indicated that much of the obstruction existed in the protympanic segment of the Eustachian tube. He also found that in cases where the obstruction can be bypassed, the obstructed segment did not extend much beyond that point [3]. However, it should be indicated that the quality of the images obtained with the fiber optic device he used is very limited which can lead to misleading assessment of these images. Endoscopic ear surgery with rigid scopes allows the high-resolution evaluation and instrumentation of the protympanic segment of the tube [7]. We had earlier reproduced Linstrom study using high resolution rigid scopes and Valsalva CT and confirmed his findings in our patient population: namely that the distal tube is patent and the proximal part is the site of the obstruction in chronic ear disease [4]. This area contains the isthmus, the narrowest segment of the cartilaginous tube and is in close proximity to the tympanic cavity and any recurrent inflammatory process within it during childhood years. However, it stand to reason that there is a degree of variability in the site of obstruction and that some of our patients do have obstruction in other more distal locations in the Eustachian tube.
Recently, balloon dilatation of the Eustachian tube has been described with significant degree of success. The procedure is designed to address obstruction located in the distal segment of the cartilaginous segment in proximity to the nasopharyngeal opening of the Eustachian tube [1, 2]. The procedure is performed by introducing a balloon dilatation catheter through the nasopharyngeal opening of the tube with a design features that prevent its introduction to the area in proximity of the carotid artery canal. The procedure and the catheters are designed to stay well clear of the proximal cartilaginous segment of the tube, an area that in our opinion represent the most common site of anatomic obstruction of the Eustachian tube.
The safety of the carotid and its canal can be ascertained due to the consistency of the identification of the carotid canal in the medial wall of the protympanum that was observed here and the introduction of the balloon catheter beyond that point as well as the different steps in the technique that we outlined earlier to confirm the catheter location within the Eustachian tube.
The anatomy of the protympanic segment of the Eustachian tube is variable and clear understanding that anatomy and full visualization is a precondition to safe instrumentation of the proximal end of the Eustachian tube. In about 30% of the ears examined, there was a pneumatization of an area anterior to the carotid which resulted in ridge of bone that separated the protympanic opening of the Eustachian tube into a lateral opening for the Eustachian tube and a medial false passage (Fig. 5) [12]. This requires the surgeon to introduce a small scope far enough anteriorly to determine the exact anatomy of that area (Figs. 6, 7). If the false passage is cannulated, and if the surgeon fails to clearly identify the carotid canal and to ascertain the intubation of the Eustachian tube anterior to the canal, one can see the possibility of doing damage to the carotid canal (Fig. 5).
Fig. 5.
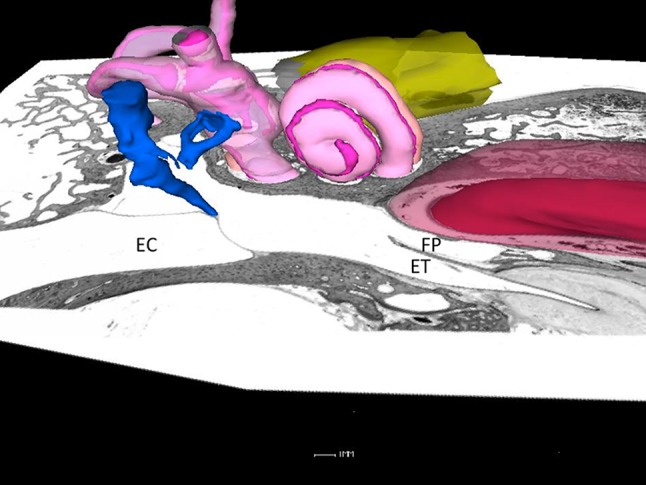
Axial histologic section of the temporal bone with the cochlea and malleus simulated for orientation. Note the pneumatization and formation of a medial false passage. ET Eustachian tube, FP false passage
Fig. 6.
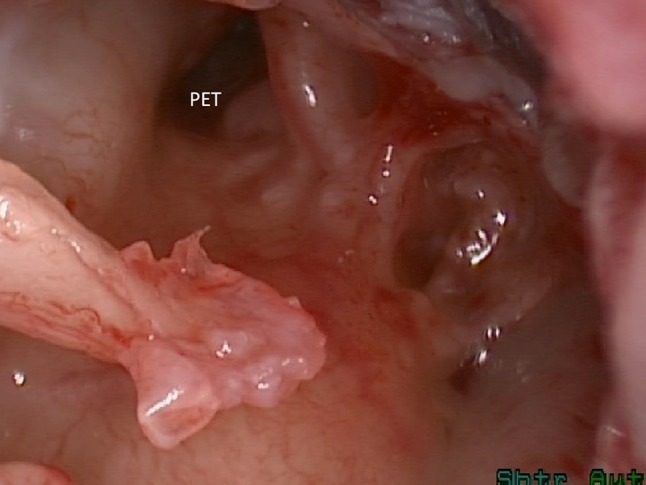
Right ear the protympanum is visualized after lifting of the tympanic membrane off the handle of the malleus. An apparent opening of the Eustachian tube is visualized. PET protympanic Eustachian tube
Fig. 7.
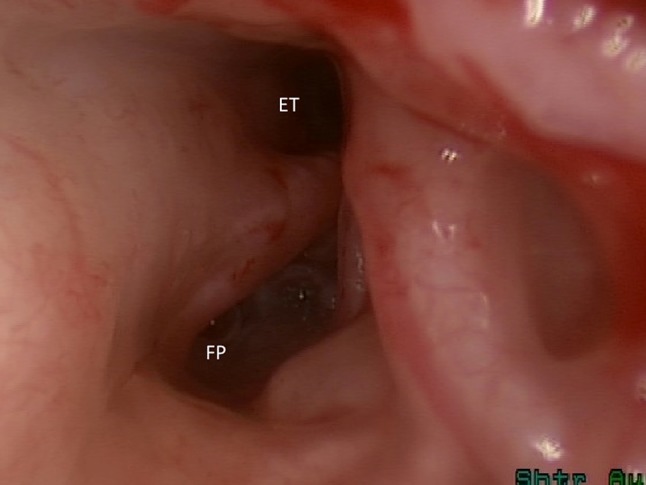
Further introduction of the scope shows the true opening of the Eustachian tube laterally to a false passage that was initially thought to be the opening of the tube. ET Eustachian tube, FP false passage
There are two cadaver studies to investigate the safety and feasibility of Transtympanic Balloon Catheter dilatation of Eustachian tube with contradictory conclusions. The first study by Kepchar et al. [5] found serious safety concerns with the technique, which is in direct opposition to the findings of Nicholas et al. [6] study. Kepchar used the microscope to help in introducing the balloon catheter into place and it resulted in successful intubation of the Eustachian tube in 6 out of ten ears. In three ears, there was false passage creation with trauma to the carotid canal. Overall this experiment revealed serious safety issues with Transtympanic Eustachian tube dilatation using microscopic straight line access.
The other study by Nicholas et al. [6], showed 100% success rate in 10 cadaver heads with no adverse effect and trauma to the adjacent structures. All 10 cadaver heads successfully underwent unilateral Balloon dilatation (five left and five right) using 3 mm diameter, 20 mm length Sterling Monorail Balloon Dilatation Catheter with attached Encore 26 Inflator (Boston Scientific Corp., Marlborough, MA, USA). Visual confirmation of successful Eustachian tube catheter insertion was appreciated in all cadaveric specimens. Dilatation was confirmed by pre and post procedure CT scan and manometric study. No obvious complications occurred during the procedure, such as damage to the ossicles and carotid canal, or overt bony fracture. The major difference between this study and the one reported by Kepchar et al. study is that, it used endoscopic guidance for catheter placement and dilatation.
Despite similar methodology based on the use of endoscopic guidance there were three major differences between our study and Nicholas et al. study;
In our study we used a different Eustachian tube balloon dilatation catheter (Spiggle & Theis, Overath Germany).
As described above, we used a different technique for catheter placement and used the “Catheter pull in” to the nasopharynx to confirm the location of the catheter.
The catheterization and dilatations were performed by multiple mature otolaryngologists who were instructed on the technique and then supervised and assisted by the first author during hands-on training course on endoscopic ear surgery. This would better assess the safety of the technique during the early phases of the learning curve.
Given the limited microscopic access to the protympanum, it has been the common wisdom in the otology community to stay away from any interventions involving the Eustachian tube given its proximity to the carotid artery. Further confirmation of that close relationship is found on the axial plane CT images, the carotid is very prominent and appears in close proximity to the whole length of the Eustachian tube (Fig. 8). Multiplanar reconstruction of high resolution CT images of the temporal bone has allowed the orientation of the sections in the plane of the ET tube as it turns downward bringing it into view. Therefore producing a more realistic assessment of the anatomical relationship between Carotid artery and the Eustachian tube (Fig. 9). In reality, all of the cartilaginous tube is well away from the carotid artery as it turns downward toward the nasopharynx (Fig. 9). Figure 10 is Parasagittal multiplanar reconstruction of the CT taken in the plane of the Eustachian tube defining the downward slope of the cartilaginous tube. Figure 11 is the same image as Fig. 10 but with an overlay of the carotid artery course obtained from a parallel section just medial to Fig. 10. It confirms that the carotid artery takes a very different direction and intersects with only a limited segment of the medial aspect of the protympanic bony segment of the tube. If that segment is visualized endoscopically and instrumentation is directed anterior to it, carotid artery safety should be assured. There are two main safety concerns in Transtympanic Eustachian tube dilatation, Ossicular chain dislocation/displacement and Carotid canal trauma. More specifically the possible coiling of the catheter in the middle ear and the medial displacement/dislocation of the handle of malleus. This can be avoided by continuous monitoring endoscopically of the advancing catheter. One should always consider aborting the procedure if the catheter is meeting too much resistance. Maintaining the introducer in position while advancing the catheter over it would also prevent coiling in the middle ear. Damage to the stapes would be avoided by correctly introducing the catheter from the superior posterior aspect of the ear canal rather than more inferiorly. This also serves to align the catheter with the anatomy and orientation of the Eustachian tube. Inspection of the protympanum for the carotid canal anatomy and any dehiscence is important first step in assuring the safety of this procedure. Directing the catheter anterior to the carotid and inferiorly away from it is essential to be able to intubate the tube with the catheter. Atraumatic insertion with measured application of pressure is the third requirement. The procedure discussed earlier allows the surgeon to confirm the presence of the catheter in the right position before inflating the balloon.
Fig. 8.
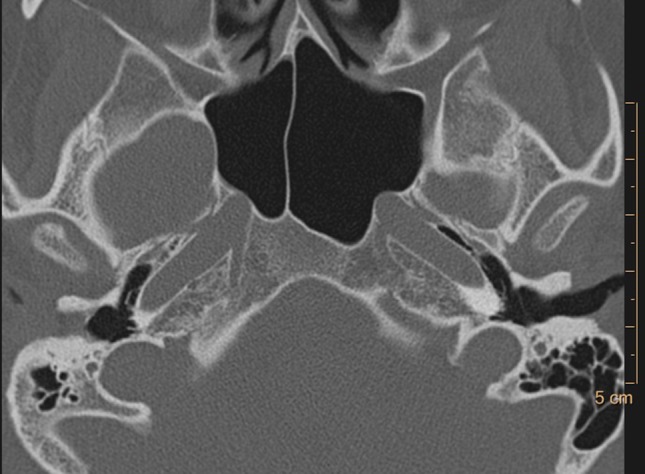
Axial CT of the protympanum depicting that much of the medial wall of the tube is occupied by the carotid artery
Fig. 9.
Reconstructed images in the plane of the Eustachian tube showing visualization of the whole length of the tube on both sides. Note as well that the whole cartilaginous tube and part of the bony segment is well clear of carotid (green line) and the carotid proximity to the Eustachian tube is limited to a certain area within the bony part (red line)
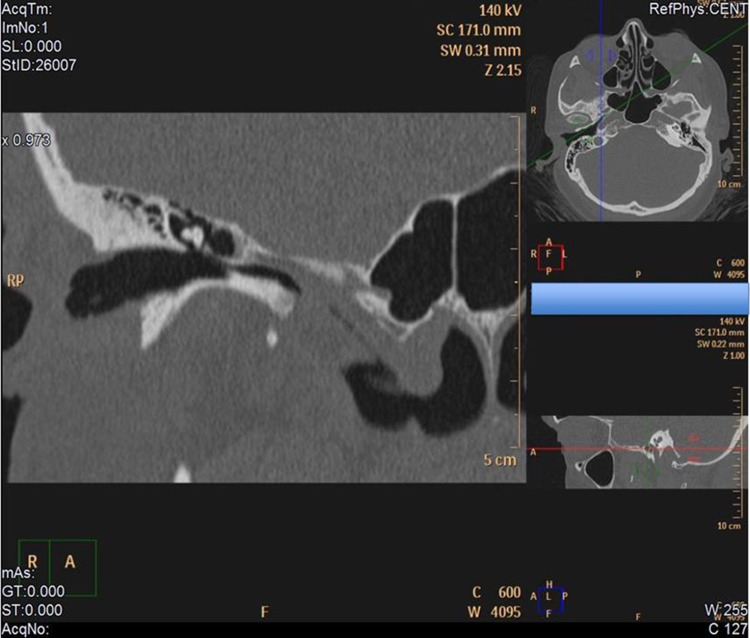
Fig. 10.
Parasagittal multiplanar reconstruction in the axis of the tube showing the downward orientation of the cartilaginous tube
Fig. 11.
The same plane as in Fig. 10, but with an overlay of the carotid artery course obtained from another image parallel to the one showed in 10 but more medial to show the carotid
Conclusion
This study demonstrated that balloon dilatation of the cartilaginous portion of the Eustachian tube was feasible and without significant adverse effects. Endoscopic guidance assures exact placement of the balloon catheter and safety of carotid artery canal in Transtympanic balloon dilatation. Endoscopic examination after balloon dilatation showed significant increase in the aperture of the proximal cartilaginous tube.
Compliance with Ethical Standards
Conflict of interest
All of the authors have read and approved the manuscript. The authors have no funding, financial relationships, or conflicts of interest to disclose.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
References
- 1.Poe DS, Juha S, Ilmari P. Balloon dilation of the cartilaginous eustachian tube. Otolaryngol Head Neck Surg. 2011;144:563–569. doi: 10.1177/0194599811399866. [DOI] [PubMed] [Google Scholar]
- 2.Ockermann T, Ulf R, Tahwinder U, Jörg E, Holger HS. Balloon dilatation eustachian tuboplasty: a clinical study. Laryngoscope. 2010;120:1411–1416. doi: 10.1002/lary.20950. [DOI] [PubMed] [Google Scholar]
- 3.Linstrom CJ, Carol AS, Arie R, Lawrence ZM. Eustachian tube endoscopy in patients with chronic ear disease. Laryngoscope. 2000;110:1884–1889. doi: 10.1097/00005537-200011000-00022. [DOI] [PubMed] [Google Scholar]
- 4.Tarabichi M, Najmi M. Site of Eustachian tube obstruction in chronic ear disease. Laryngoscope. 2015;125:2572–2575. doi: 10.1002/lary.25330. [DOI] [PubMed] [Google Scholar]
- 5.Kepchar J, Acevedo J, Schroeder J, Littlefield P. Transtympanic balloon dilatation of Eustachian tube: a human cadaver pilot study. J Laryngol Otol. 2012;126:1102–1107. doi: 10.1017/S0022215112001983. [DOI] [PubMed] [Google Scholar]
- 6.Nicholas J, Alexander T, Allison N, Nirmal P. Endoscopically guided transtympanic balloon catheter dilatation of the eustachian tube: a cadaveric pilot study. Otol Neurotol. 2016;37:350–355. doi: 10.1097/MAO.0000000000000975. [DOI] [PubMed] [Google Scholar]
- 7.Tarabichi M. Transcanal endoscopic management of cholesteatoma. Otol Neurotol. 2010;31:580–588. doi: 10.1097/MAO.0b013e3181db72f8. [DOI] [PubMed] [Google Scholar]
- 8.Sato H, Hajime N, Iwao H, Masahiko H. Eustachian tube function in tympanoplasty. Acta Otolaryngol. 1990;110:9–12. doi: 10.3109/00016489009124803. [DOI] [PubMed] [Google Scholar]
- 9.Takahashi H, Fujita A, Honjo I. Site of eustachian tube dysfunction in patients with otitis media with effusion. Am J Otolaryngol. 1987;8:361–363. doi: 10.1016/S0196-0709(87)80021-2. [DOI] [PubMed] [Google Scholar]
- 10.Edelstein DR, Magnan J, Parisier C. Microfiberoptic evaluation of the middle ear cavity. Am J Otol. 1994;15:50–55. [PubMed] [Google Scholar]
- 11.Takahashi H, Honjo I, Fujita A. Endoscopic findings at the pharyngeal orifice of the eustachian tube in otitis media with effusion. Eur Arch Otorhinolaryngol. 1996;253:42–47. doi: 10.1007/BF00176702. [DOI] [PubMed] [Google Scholar]
- 12.Tarabichi M, Najmi M. Transtympanic dilatation of the eustachian tube during chronic ear surgery. Acta Otolaryngol. 2015;135:640–644. doi: 10.3109/00016489.2015.1009640. [DOI] [PubMed] [Google Scholar]