Abstract
Aims
Examine 30-day readmissions for recurrent hypoglycemia and hyperglycemia in a national cohort of adults with diabetes.
Methods
Retrospective analysis of data from OptumLabs Data Warehouse for all adults with diabetes hospitalized January 1, 2009 to December 31, 2014 with a principal diagnosis of hypoglycemia or hyperglycemia. We examined the rates and risk factors of 30-day readmissions for hypoglycemia and hyperglycemia.
Results
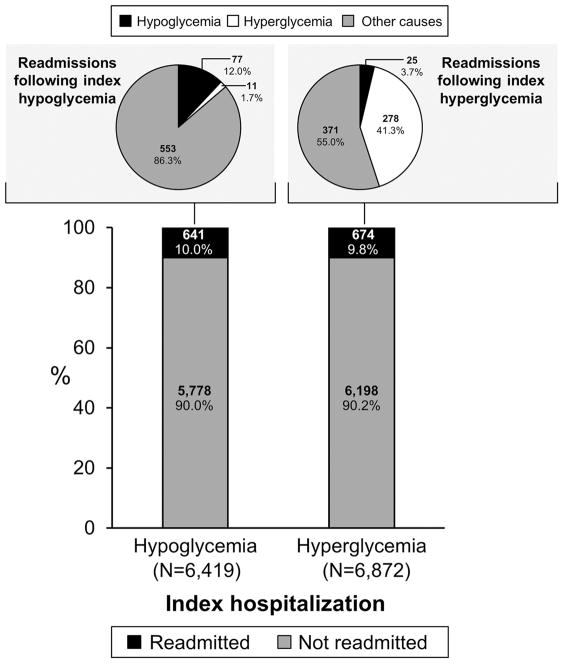
After 6419 index hypoglycemia hospitalizations, 1.2% were readmitted for recurrent hypoglycemia, 0.2% for hyperglycemia, and 8.6% for other causes. Multimorbidity was the strongest predictor of recurrent hypoglycemia. After 6872 index hyperglycemia hospitalizations, 4.0% were readmitted for recurrent hyperglycemia, 0.4% for hypoglycemia, and 5.4% for other causes. Recurrent hyperglycemia was less likely in older patients (OR 0.6, 95% CI 0.5–0.9 for 45–64 vs. <45 years) and with the addition of a new glucose-lowering medication at index discharge (OR 0.40; 95% CI 0.2–0.7). New hypoglycemia readmissions were most likely among patients ≥75 years (OR 13.3, 95% CI 2.4–73.4, vs. <45 years).
Conclusions
Patients hospitalized for hyperglycemia are often readmitted for recurrent hyperglycemia, while patients hospitalized for hypoglycemia are generally readmitted for unrelated causes. Early recognition of high risk patients may identify opportunities to improve post-discharge management and reduce these events.
Keywords: Hypoglycemia, ketoacidosis (DKA), hyperglycemic hyperosmolar state (HHS), hospitalization, readmission, health services research, epidemiology, diabetes
1. Introduction
Patients with diabetes who experience severe hypoglycemia or hyperglycemia incur potentially preventable morbidity,1,2 mortality,3 high costs,4–7 and impaired quality of life,4,7,8 particularly when the events are so severe as to require hospitalization. Despite being potentially preventable with optimal ambulatory care, rates of hospitalization for hypoglycemia9–11 and hyperglycemia9,10 remain high. In a recent study of hospitalizations and readmissions among patients with diabetes, admissions for severe dysglycemia accounted for 2.6% of all hospitalizations and 2.5% of all 30-day readmissions.9 Such hospitalizations may reflect underlying deficiencies in patient care and diabetes management, particularly if patients need to be readmitted for hypoglycemia or hyperglycemia shortly after hospitalization for a similar event.
Preventing hospitalizations and readmissions is key to improving care quality and lowering costs of care. To promote high quality care for people with diabetes, the Centers for Medicare & Medicaid Services (CMS) uses rates of 30-day all-cause unplanned readmissions among all patients12 and of all-cause unplanned admissions among patients with diabetes13 for public reporting and payment adjustment. Identifying patients at highest risk for readmission specifically for severe hypoglycemic or hyperglycemic events is an important first step toward their prevention.
Prior studies identified several risk factors for hypoglycemia including prior hypoglycemia,14,15 intensive glucose-lowering therapy,16,17 insulin and sulfonylurea use,11,15–19 older age,11,15,19–21 multimorbidity,11,16 and cognitive impairment.22 Severe hyperglycemia is more common among younger patients21 and patients with depression or substance use.24,45 Elevated hemoglobin A1c (HbA1c) 11,23,24 and socioeconomic disadvantage 23,25–29 are associated with both hypoglycemia and hyperglycemia. However, there is little information about recurrent hospitalizations for severe dysglycemia among adults with diabetes. Because patients may be experiencing both types of events, concurrently examining severe hypoglycemia and hyperglycemia would present a more complete and holistic representation of diabetes care, and potentially identify clinically meaningful trends and risk factors. To address this knowledge gap, we examine hospital readmissions for severe hypoglycemia and hyperglycemia that occur within 30 days of hospital discharge for another hypoglycemic or hyperglycemic event in a national cohort of adults with established diabetes.
2. Materials and methods
2.1. Study design and data source
We conducted a retrospective analysis of patients with medical and pharmacy claims data from OptumLabs Data Warehouse (OLDW), an administrative database of more than 100 million privately insured and Medicare Advantage enrollees throughout the U.S. (Appendix A.1)30,31 This national dataset encompasses a wide range of ages and racial/ethnic groups. All study data were accessed after the data were de-identified, consistent with Health Insurance Portability and Accountability Act expert de-identification determination and with appropriate legal, regulatory, and contractual permissions. Because this study involved analysis of pre-existing, de-identified data, it was deemed exempt from further review by the Mayo Clinic Institutional Review Board.
2.2. Study population
The study sample was comprised of index hospitalizations with the principal diagnosis of either severe hypoglycemia or severe hyperglycemia among adults, age ≥18 years, with a diagnosis of diabetes prior to the date of hospitalization (e.g. diabetes was not diagnosed in the context of the index hospitalization). Eligible hospitalizations lasted ≥1 night and occurred in non-federal acute care hospitals between January 1, 2009 and December 31, 2014. Hospitalizations, rather than individual patients, were the unit of analysis to allow for comprehensive assessment of risk factors for recurrent events which can vary at each admission. Patients were excluded if they had less than 12 months of continuous medical and pharmacy insurance enrollment prior to the index admission date or less than 120 days of enrollment after the index discharge date.
Principal diagnoses were identified using the first/primary discharge diagnosis ICD-9- CM code from the hospitalization claim and categorized as hypoglycemic or hyperglycemic based on validated algorithms: (1) Hypoglycemia: ICD-9-CM 251.x; 962.3, E858.0, E932.3, E950.4, E962.0, E980.4, 250.8x (unless concurrent 259.8, 272.7, 681, 682, 686.9, 707.1, 707.8, 707.9, 709.3, 730.0, 730.1, 730.2, 731.8);32 and (2) Hyperglycemia: ICD-9-CM 250.1x, 250.2x, 250.3x.33 Preexisting diagnosis of diabetes was established using Healthcare Effectiveness Data and Information Set claims-computable criteria, excluding gestational diabetes (ICD-9-CM 648.0x),34 applied to the 12 months preceding the date of index admission. In accordance with the CMS HWR Measure and National Committee for Quality Assurance criteria,35,36 hospitalizations and readmissions for medical treatment of cancer, primary psychiatric disease, and pregnancy were excluded. We excluded admissions with length of stay (LOS) >365 days and readmissions within one day of discharge, which were counted as part of the original admission.
2.3. Explanatory variables
Baseline patient demographic characteristics were obtained from enrollment data and included age at the index hospitalization, sex, race/ethnicity, and median annual household income of their residence zip code in US$. For each index hospitalization we determined the LOS (categorized as 1, 2–4, 5–7, 8–14, and ≥15 days), discharge year, and history of another hospitalization during the prior 12 months. Rather than assume a linear or monotone relationship between LOS and risk of readmission, we categorized this risk factor based on inspection of the distribution in our cohort. To identify comorbidities, we used the Diabetes Complications Severity Index (DCSI) adapted for claims data,37 and the Charlson Comorbidity Index (CCI),38 all from 12 months prior to the index admission.
Diabetes medications were ascertained from pharmacy claims comprised of medications filled through the health insurance pharmacy benefits. Medications obtained outside of health insurance coverage, including metformin, sulfonylurea, or human insulin agents purchased through low cost generic drug programs,39 cannot be identified but are estimated to comprise <5% of fills. Each medication class (Table A.2) was noted as being present at baseline (i.e. filled between the index admission date and the 120 days prior), after discharge (i.e. filled between the index admission date and the 120 days afterwards), or both (Figure A.3).
To examine the relationship between glucose-lowering treatment regimens and subsequent risk of hypoglycemia or hyperglycemia readmission, we considered all medications likely used by patients during the “immediate post-discharge” period, i.e. the interval between index hospital discharge and the day of readmission (for patients who were readmitted) or 30 days (for patients who were not readmitted). These medications were identified as drugs filled during this immediate-post discharge period in addition to those used at baseline and refilled during the 120-day following the index hospitalization (Figure A.3).
The disposition of baseline medications that were not refilled during the 120 days following index discharge, however, is uncertain, as these medications were discontinued during the 120-day period and the precise timing of discontinuation relative to the readmission (or lack thereof) cannot be determined. In our primary analysis, we considered all medications filled during the baseline 120-day period as being potentially used during the immediate post-discharge period, irrespective of whether these medications were ultimately refilled. This conservative approach results in misclassification of some discontinued medications as still being used prior to readmission, thereby overestimating number of medications used and underestimating prevalence of treatment de-intensification following index hospital discharge. We then performed a sensitivity analysis that took the opposite approach, classifying all baseline medications not refilled during the 120-day post-discharge period as being discontinued. This approach results in misclassification of medications discontinued later on as being discontinued prior to the potential readmission, thereby underestimating the number of medications used and overestimating the prevalence of treatment de-intensification upon index hospital discharge.
For both primary and sensitivity analyses, medication changes were categorized as additions (≥1 medication class started during the immediate post-discharge period spanning index hospital discharge and either readmission or day 30, whichever came first), discontinuations (≥1 medication class not refilled during the 120-day post-discharge period), and/or switches ((≥1 medication class changed for another when comparing medications filled in the 120 days before to 120 days after the index admission date). Because insulin doses cannot be reliably ascertained using claims data, intensification and de-intensification of insulin could not be measured. We nonetheless included insulin-treated patients in order to assess impacts of insulin use, start, and discontinuation (albeit not dose change) on readmission risk.
For the purposes of determining whether a hospitalization was planned, we applied version 3 of the CMS HWR planned readmission algorithm, which categorizes admissions as planned according to procedures performed during the hospitalization irrespective of the principle diagnosis upon admission.35,40
2.4. Outcomes
The primary outcome was unplanned readmission for either severe hypoglycemia or hyperglycemia within 30 days of discharge. Planned readmissions 35,40 were excluded.
2.5. Statistical analysis
We summarized patient and hospitalization characteristics for each hypoglycemia and hyperglycemia index hospitalization, and tested for differences in outcomes using chi-square tests of independence.
In order to identify independent risk factors for hypoglycemia and hyperglycemia readmissions, we estimated four mixed effects logistic regression models, two for each cohort, using the primary outcomes of hypoglycemia or hyperglycemia readmission as the dependent variables. Covariates included in the models were selected based on prior literature and clinical relevance. Each model included a random hospital effect to account for correlation of outcomes by hospital. To account for missing income data (8.1% of total sample), we used multiple imputations with 20 imputations.41
As a sensitivity analyses, we replicated the main analyses using an alternative treatment change classification, wherein medications not filled within 120 days post discharge were assumed to be discontinued at time of index admission (see above).
All analyses were conducted using Stata 14.1 (Stata Corp 2015, College Station, TX). P-values <0.05 were considered to be statistically significant.
3. Results
3.1 Study Population and 30-day Readmissions
Between January 1, 2009 and December 31, 2014, 11161 patients experienced 13291 index hospitalizations, including 6419 index hospitalizations for hypoglycemia among 5911 patients and 6872 index hospitalizations for hyperglycemia among 5250 patients. Overall, 1338 patients (12%) had more than one index hospitalization during the 5-year study period. Baseline patient characteristics at the time of index admission are shown in Table 1. Patients hospitalized for hypoglycemia were significantly older (68.0 vs. 48.6 years; p<0.001); more likely to be insulin-treated (65.5% vs. 48.6%; p<0.001); and had more diabetes complications (as measured by the DCSI) and more chronic conditions overall (as measured by the CCI) compared to patients hospitalized for hyperglycemia. At the time of index hospitalization, patients hospitalized for hypoglycemia were more likely to be taking two (8.4% vs. 6.0%), three (20.0% vs. 9.8%), four (9.4% vs. 3.9%), or five or more (1.8% vs. 0.8%) drugs compared to patients hospitalized for hyperglycemia; P<0.001.
Table 1.
Patient characteristics upon index hospital discharge.
| Hypoglycemia (n = 6419) | Hyperglycemia (n = 6872) | p-value | |
|---|---|---|---|
| Patient Demographics | |||
| Age, years, mean (SD) | 68.0 (13.2) | 48.6 (18.6) | <0.001 |
| Age category, years, N (%) | |||
| <45 | 340 (5.3) | 2819 (41.0) | |
| 45 – 64 | 1994 (31.1) | 2548 (37.1) | |
| 65 – 74 | 1708 (26.6) | 847 (12.3) | |
| ≥75 | 2377 (37.0) | 658 (9.6) | |
| Female sex, N (%) | 3143 (49.0) | 3637 (52.9) | <0.001 |
| Race/ethnicity, N (%) | <0.001 | ||
| Non-Hispanic white | 4088 (63.7) | 4523 (65.8) | |
| Black | 1608 (25.1) | 1674 (24.4) | |
| Asian | 163 (2.5) | 106 (1.5) | |
| Hispanic | 560 (8.7) | 569 (8.3) | |
| Annual household income, $US, N (%) | <0.001 | ||
| <$40,000 | 2823 (44.0) | 2164 (31.5) | |
| $40,000 – $49,999 | 645 (10.0) | 632 (9.2) | |
| $50,000 – $59,999 | 520 (8.1) | 597 (8.7) | |
| $60,000 – $74,999 | 595 (9.3) | 789 (11.5) | |
| $75,000 – $99,999 | 637 (9.9) | 899 (13.1) | |
| ≥$100,000 | 730 (11.4) | 1224 (17.8) | |
| Unknown | 469 (7.3) | 567 (8.3) | |
| Patient Clinical Information | |||
| Charlson comorbidity index, N (%) | <0.001 | ||
| 0–1 | 662 (10.3) | 2470 (35.9) | |
| 2–3 | 2801 (43.6) | 3057 (44.5) | |
| ≥4 | 2956 (46.1) | 1345 (19.6) | |
| Diabetes complications severity index, N (%) | <0.001 | ||
| 0 | 943 (14.7) | 999 (14.5) | |
| 1–2 | 1385 (21.6) | 2440 (35.5) | |
| 3–6 | 2309 (36.0) | 2351 (34.2) | |
| ≥7 | 1782 (27.8) | 1082 (15.7) | |
| Diabetes complications, N (%) | |||
| Retinopathy | 1197 (18.6) | 1004 (14.6) | <0.001 |
| Nephropathy | 1973 (30.7) | 1471 (21.4) | <0.001 |
| Neuropathy | 3134 (48.8) | 2343 (34.1) | <0.001 |
| Heart failure | 1852 (28.9) | 696 (10.1) | <0.001 |
| Cerebrovascular disease | 2836 (44.2) | 1253 (18.2) | <0.001 |
| Peripheral vascular disease | 2288 (35.6) | 712 (10.4) | <0.001 |
| Hyperglycemia | 274 (4.3) | 4610 (67.1) | <0.001 |
| Unknown | 469 (7.3) | 567 (8.3) | |
| Index Hospitalization Characteristics | |||
| Planned index admission, N (%) | 1142 (17.8) | 91 (1.3) | <0.001 |
| Length of stay, days, median (IQR) | 3 (2–5) | 3 (2–4) | |
| Length of stay category, days, N (%) | <0.001 | ||
| 1 | 1128 (17.6) | 1136 (16.5) | |
| 2–4 | 3281 (51.1) | 4344 (63.2) | |
| 5–7 | 1149 (17.9) | 969 (14.1) | |
| 8–14 | 674 (10.5) | 351 (5.1) | |
| ≥15 | 187 (2.9) | 72 (1.0) | |
| Prior hospitalization history, N (%) | 2786 (43.4) | 2907 (42.3) | 0.20 |
| Diabetes Treatment Regimen | |||
| Number of diabetes medications on index admission, N (%) | <0.001 | ||
| 0 | 1258 (19.6) | 1540 (22.4) | |
| 1 | 2626 (40.9) | 3917 (57.0) | |
| 2 | 537 (8.4) | 415 (6.0) | |
| 3 | 1281 (20.0) | 675 (9.8) | |
| 4 | 601 (9.4) | 270 (3.9) | |
| ≥5 | 116 (1.8) | 55 (0.8) | |
| Regimen change after index discharge, N (%) | <0.001 | ||
| No change | 4110 (64.0) | 4589 (66.8) | |
| Discontinue ≥1 drug(s) | 1559 (24.3) | 733 (10.7) | |
| Start ≥1 drug(s) | 500 (7.8) | 1202 (17.5) | |
| Switch ≥1 drug(s) | 170 (2.6) | 218 (3.2) | |
| Discontinue & switch | 62 (1.0) | 102 (1.5) | |
| Start & switch | 18 (0.3) | 28 (0.4) | |
| Number of diabetes medications following index discharge, N (%) | <0.001 | ||
| 0 | 1414 (22.0) | 754 (11.0) | |
| 1 | 2591 (40.4) | 4634 (67.4) | |
| 2 | 697 (10.9) | 221 (3.2) | |
| 3 | 1173 (18.3) | 821 (11.9) | |
| 4 | 452 (7.0) | 365 (5.3) | |
| ≥5 | 92 (1.4) | 77 (1.1) | |
Index hospitalizations for hypoglycemia were more likely to be considered planned by the CMS HWR planned readmission algorithm, which categorizes admissions as planned according to diagnostic and procedure codes,35,40 than index hospitalizations for hyperglycemia (17.8% vs. 1.3%; p<0.001). Among patients hospitalized with the principal diagnosis of hypoglycemia, these planned hospitalizations were most commonly for amputation (44%) or debridement (34%). In contrast, among patients hospitalized for the principal diagnosis of hyperglycemia, the planned index admissions were for most often for coronary angioplasty (21%) or debridement (20%). Remaining hospitalizations were considered planned because they involved surgical or non-surgical procedures (most often gastrointestinal, cardiovascular, or genitourinary), biopsies, diagnostic or imaging studies, intravenous medication administration, or dialysis. Hospitalizations for hypoglycemia were also longer and more likely to last ≥5 days (31.1% vs. 20.2%; p<0.001).
While the all-cause unplanned readmission rates after index hypoglycemic and hyperglycemic hospitalizations were similar (9.8% vs. 10.0%, respectively; p = 0.83), the probabilities of recurrent dysglycemia were very different (Figure 1). Patients hospitalized for hypoglycemia were most likely to be readmitted for other primary causes (553 [86.3%] of the 641 readmissions); 12.0% were readmitted for recurrent hypoglycemia (77/641 readmissions) and 1.7% were readmitted for hyperglycemia (11/641 readmissions). In contrast, patients hospitalized for hyperglycemia were almost as likely to be readmitted for recurrent hyperglycemia (278 [41.3%] of the 674 readmissions) as for unrelated causes (371 [55.0%] of the 674 readmissions); only 3.7% were readmitted for hypoglycemia (25/674).
Figure 1.
Patient readmission status following index hospitalization for severe hyperglycemia and severe hypoglycemia.
3.2. Medication Changes after Discharge
Diabetes treatment regimens were generally unchanged after both hypoglycemia (64.0%) and hyperglycemia (66.8%) index hospitalizations (Table 1), though we were not able to ascertain changes in medication dose. At least one drug was discontinued (e.g. not refilled within 120 days) by 25.3% of patients hospitalized for hypoglycemia (24.3% discontinued and 1% both discontinued and switched class) and 12.2% of those hospitalized for hyperglycemia (10.7% discontinued and 1.5% both discontinued and switched class). Conversely, at least one new drug was started at or after index hospital discharge and before readmission (or 30 days, whichever came first) in 17.9% of patients hospitalized for hyperglycemia (17.5% added and 0.4% both added and switched class) and 8.1% of those hospitalized for hypoglycemia (7.8% added and 0.3% both added and switched class).
Subsequent to hospital discharge for index hypoglycemia, 54.7% of patients were taking insulin, 30.5% metformin, 36.3% sulfonylureas, 2.0% GLP-1 receptor agonist, 8.9% DPP4 inhibitors, 9.7% other glucose-lowering drugs, and 0.2% SGLT2 inhibitors; 15.3% were not taking any glucose lowering medications. (Table 2) In the sensitivity analysis that considered medications not filled within 120 days of index hospitalizations as being discontinued, 47.7% were taking insulin, 21.9% sulfonylurea, 22.9% metformin, 1.4% GLP-1 receptor agonist, 6.5% DPP4 inhibitor, and 6.1% other glucose-lowering drugs; 26.0% filled no glucose-lowering medications and there were too few SGLT2 inhibitors to capture. This suggests that within 120 days of hospital discharge, 6.9% of patients discontinued insulin, 7.6% metformin, 14.3% sulfonylurea, 0.6% GLP-1 receptor agonist, 2.4% DPP4 inhibitor, and 3.6% another glucose-lowering medication.
Table 2.
Medication use following index hospital discharge stratified by primary reason for the index hospitalization. Primary analysis assumes that post-discharge medications are those that the patient was using at the time of index hospital admission plus those that were added between index hospital discharge and readmission (or 30 days, which ever came first). The sensitivity analysis subtracts medications not refilled during 120 days following the index hospitalization.
| Primary Analysis | Sensitivity Analysis | |||||
|---|---|---|---|---|---|---|
| Hypoglycemia N (%) | Hyperglycemia N (%) | p-value | Hypoglycemia N (%) | Hyperglycemia N (%) | p-value | |
| Insulin | 3509 (54.7) | 5835 (84.9) | <0.001 | 3065 (47.7) | 5524 (80.4) | <0.001 |
| Metformin | 1959 (30.5) | 1347 (19.6) | <0.001 | 1470 (22.9) | 903 (13.1) | <0.001 |
| Sulfonylurea | 2328 (36.3) | 777 (11.3) | <0.001 | 1408 (21.9) | 489 (7.1) | <0.001 |
| GLP-1 receptor agonist | 129 (2.0) | 104 (1.5) | 0.03 | 90 (1.4) | 51 (0.7) | <0.001 |
| DPP-4 inhibitor | 569 (8.9) | 317 (4.6) | <0.001 | 416 (6.5) | 198 (2.9) | <0.001 |
| SGLT2 inhibitor | 13 (0.2) | 32 (0.5) | 0.009 | <11* | 14 (0.2) | 0.52 |
| Other | 620 (9.7) | 303 (4.4) | <0.001 | 391 (6.1) | 166 (2.4) | <0.001 |
| No medications | 984 (15.3) | 706 (10.3) | <0.001 | 1671 (26.0) | 1052 (15.3) | <0.001 |
Data with cells containing ≤11 patients is suppressed in order to maintain strict patient deidentification.
After hospital discharge for index hyperglycemia, 84.9% were treated with insulin, 19.6% metformin, 11.3% sulfonylurea, 1.5% GLP-1 receptor agonist, 4.6% DPP4 inhibitor, 0.5% SGLT2 inhibitor, and 4.4% other glucose lowering drugs; 10.3% indications did not have any glucose lowering medications. (Table 2) In the sensitivity analysis, 80.4% were treated with insulin, 13.1% metformin, 7.1% sulfonylurea, 0.7% GLP-1 receptor agonist, 2.9% DPP4 inhibitor, 0.2% as SGLT2 inhibitor, and 2.4% other glucose-lowering drugs; 15.3% did not have any glucose lowering medications. This suggests that within 120 days of hospital discharge, 4.5% of patients discontinued insulin, 6.5% metformin, 4.2% sulfonylurea, 0.8% GLP-1 receptor agonist, 1.7% DPP4 inhibitor, 0.3% SGLT2 inhibitor, and 2.0% another glucose-lowering medication.
3.3. Readmissions after Index Hyperglycemia
In multivariate analysis, the risk of readmission for recurrent hyperglycemia within 30 days of discharge for hyperglycemia decreased progressively with age (p =0.02); Table 3. Patients 65–74 years old and ≥75 years had more than 40% lower rate of such events compared to patients <45 years. Patients with prior history of hyperglycemia (OR 1.60; 95% CI, 1.05–2.44) or prior hospitalizations for any cause (OR 3.77; 95% CI, 2.73–5.21) also had a significantly higher risk for recurrent hyperglycemia. Other diabetes complications and the overall comorbidity burden (measured by the CCI) were not significantly associated with recurrent hospitalization for hyperglycemia.
Table 3.
Risk factors for recurrent hospitalizations for severe hyperglycemia and hypoglycemia.
| Hyper → Hyper | Hyper → Hypo | Hypo → Hypo | ||||
|---|---|---|---|---|---|---|
| OR (CI) | P | OR (CI) | P | OR (CI) | P | |
| Age category | 0.03 | 0.01 | 0.77 | |||
| <45 | ref | ref | ref | |||
| 45–64 | 0.63 (0.46, 0.87) | 3.64 (0.89, 14.89) | 0.69 (0.22, 2.12) | |||
| 65–74 | 0.60 (0.36, 0.98) | 10.20 (2.13, 48.82) | 0.61 (0.19, 1.93) | |||
| ≥75 | 0.57 (0.31, 1.02) | 13.30 (2.41, 73.35) | 0.56 (0.18, 1.76) | |||
| Female (vs. male) | 1.10 (0.85, 1.42) | 0.65 | 1.05 (0.44, 2.49) | 0.91 | 0.60 (0.38, 0.97) | 0.04 |
| Race (vs. white) | 1.00 | 0.88 | 0.10 | |||
| Black | 1.00 (0.74, 1.35) | 1.30 (0.52, 3.30) | 1.87 (1.12, 3.13) | |||
| Asian | 1.00 (0.35, 2.85) | 2.03 (0.21, 19.65) | 1.96 (0.57, 6.71) | |||
| Hispanic | 1.03 (0.64, 1.66) | 0.90 (0.11, 7.40) | 1.24 (0.54, 2.85) | |||
| Planned (vs. no) | 1.91 (0.78, 4.66) | 0.16 | 2.88 (0.32, 26.22) | 0.35 | 0.37 (0.14, 1.01) | 0.05 |
| Length of stay | 0.54 | 0.22 | 0.71 | |||
| 1 day | 0.93 (0.65, 1.32) | 1.37 (0.37, 5.12) | 0.66 (0.34, 1.30) | |||
| 2–4 days | ref | ref | ref | |||
| 5–7 days | 0.75 (0.51, 1.11) | 1.22 (0.37, 3.98) | 0.87 (0.45, 1.68) | |||
| 8–14 days | 0.70 (0.37, 1.34) | 3.21 (1.06, 9.70) | 1.10 (0.50, 2.44) | |||
| DCSI category | 0.43 | 0.93 | 0.88 | |||
| 0 | ref | ref | ref | |||
| 1–2 | 0.81 (0.41, 1.59) | 1.26 (0.15, 10.82) | 0.69 (0.27, 1.78) | |||
| 3–6 | 1.08 (0.47, 2.45) | 0.97 (0.26, 3.69) | 0.80 (0.27, 2.41) | |||
| ≥7 | 1.37 (0.48, 3.95) | --* | 0.82 (0.19, 3.60) | |||
| Diabetes complications | ||||||
| Retinopathy | 0.71 (0.49, 1.04) | 0.08 | 1.17 (0.37, 3.65) | 0.79 | 0.56 (0.27, 1.17) | 0.12 |
| Nephropathy | 1.37 (0.97, 1.92) | 0.07 | 2.07 (0.71, 6.03) | 0.18 | 1.20 (0.68, 2.11) | 0.53 |
| Neuropathy | 1.31 (0.90, 1.88) | 0.15 | 1.33 (0.45, 3.93) | 0.61 | 0.72 (0.41, 1.26) | 0.25 |
| Heart failure | 0.63 (0.39, 1.01) | 0.06 | 0.39 (0.10, 1.53) | 0.18 | 0.47 (0.26, 0.86) | 0.01 |
| Cerebrovascular disease | 1.27 (0.86, 1.87) | 0.23 | 0.36 (0.11, 1.20) | 0.10 | 0.90 (0.50, 1.65) | 0.74 |
| Peripheral vascular disease | 0.89 (0.59, 1.35) | 0.59 | --* | 0.78 (0.42, 1.45) | 0.44 | |
| Hyperglycemia | 1.60 (1.05, 2.44) | 0.03 | 1.11 (0.36, 3.41) | 0.86 | 1.41 (0.57, 3.47) | 0.46 |
| Charlson category | 0.91 | 0.44 | 0.002 | |||
| 0–1 | ref | ref | ref | |||
| 2–3 | 1.09 (0.74, 1.60) | 0.96 (0.22, 4.23) | 0.93 (0.32, 2.71) | |||
| ≥4 | 1.10 (0.65, 1.86) | 1.89 (0.34, 10.45) | 2.93 (0.94, 9.12) | |||
| Prior hospitalization history | 3.77 (2.73, 5.21) | <0.001 | 3.63 (1.27, 10.36) | 0.02 | 2.28 (1.34, 3.88) | 0.002 |
| Treatment change | 0.04 | 0.01 | 0.31 | |||
| No change | ref | ref | ref | |||
| Stopped | 0.98 (0.65, 1.49) | 4.49 (1.69, 11.90) | 1.59 (0.95, 2.68) | |||
| Added | 0.40 (0.22, 0.72) | 0.35 (0.04, 2.85) | 0.53 (0.16, 1.80) | |||
| Switch | 0.42 (0.06, 3.16) | --* | 0.87 (0.11, 6.92) | |||
| Stopped + switch | --* | --* | --* | |||
| Added + switch | --* | --* | --* | |||
| Post-discharge medication(s) | ||||||
| Insulin | 0.80 (0.28, 2.34) | 0.69 | --* | 0.75 (0.36, 1.59) | 0.46 | |
| Sulfonylurea | 0.28 (0.08, 0.95) | 0.04 | 1.08 (0.12, 9.83) | 0.95 | 1.28 (0.63, 2.59) | 0.49 |
| GLP-1 receptor agonist | 1.42 (0.32, 6.29) | 0.65 | --* | 3.08 (0.69,13.84) | 0.14 | |
| DPP4 inhibitor | 0.28 (0.04, 2.06) | 0.21 | --* | 1.25 (0.49, 3.17) | 0.64 | |
| SGLT2 inhibitor | --* | --* | --* | . | ||
| Metformin | 1.09 (0.61, 1.96) | 0.77 | --* | 0.49 (0.23, 1.03) | 0.06 | |
| Other | 0.28 (0.04, 2.10) | 0.22 | --* | 1.50 (0.64, 3.52) | 0.35 | |
| No medications | 0.81 (0.27, 2.43) | 0.70 | --* | 0.53 (0.22, 1.29) | 0.16 | |
| Annual household income, $US | 0.53 | 0.62 | 0.51 | |||
| <$40,000 | ref | ref | ref | |||
| $40,000 – $49,999 | 1.23 (0.80, 1.88) | 1.88 (0.47, 7.58) | 0.56 (0.22, 1.43) | |||
| $50,000 – $59,999 | 1.22 (0.78, 1.91) | 2.42 (0.67, 8.75) | 1.11 (0.51, 2.43) | |||
| $60,000 – $74,999 | 0.95 (0.62, 1.48) | 1.51 (0.37, 6.15) | 0.81 (0.33, 1.98) | |||
| $75,000 – $99,999 | 0.86 (0.56, 1.33) | 1.94 (0.45, 8.30) | 0.59 (0.22, 1.57) | |||
| ≥$100,000 | 0.82 (0.54, 1.25) | 0.46 (0.05, 3.97) | 0.42 (0.13, 1.39) | |||
| Year of discharge | 0.30 | 0.43 | 0.89 | |||
| 2009 | ref | ref | ref | |||
| 2010 | 0.95 (0.59, 1.52) | 5.54 (0.58, 53.05) | 1.20 (0.52, 2.76) | |||
| 2011 | 0.63 (0.38, 1.04) | 4.08 (0.41, 40.95) | 1.01 (0.43, 2.40) | |||
| 2012 | 0.78 (0.49, 1.23) | 3.27 (0.34, 31.22) | 0.85 (0.35, 2.05) | |||
| 2013 | 1.02 (0.66, 1.56) | 5.88 (0.63, 54.58) | 1.25 (0.56, 2.77) | |||
| 2014 | 0.96 (0.62, 1.49) | 1.81 (0.17, 19.47) | 0.86 (0.36, 2.05) | |||
Data with cells containing ≤11 patients is suppressed in order to maintain strict patient deidentification.
Patients treated with sulfonylurea drugs subsequent to index hospital discharge had a lower risk of recurrent hyperglycemia hospitalizations (OR 0.28; 95% CI, 0.08–0.95). Furthermore, adding a medication at the time of the index discharge significantly lowered the risk of recurrent hyperglycemia (OR 0.40; 95% CI, 0.22–0.72); Table 3. Results were largely unchanged in the sensitivity analysis that considered medications not refilled within 120 days of discharge as being discontinued, though the association with sulfonylurea therapy was no longer statistically significant (Table A.3).
In contrast, the risk of being readmitted for severe hypoglycemia after index discharge for hyperglycemia increased progressively with age (p=0.02); Table 3. Patients ≥75 years of age had an over 13-fold higher risk of hypoglycemia rehospitalization compared with patients <45 years of age (OR 13.30; 95% CI, 2.41–73.35). No individual medication class changed the probability of hypoglycemia readmissions, both in the primary (Table 3) and sensitivity (Table A.3) analyses. The absence of continued fills of at least one previously used glucose-lowering drug during 120 days after the index hyperglycemia admission was associated with hyperglycemia-followed- by-hypoglycemia hospitalizations (OR 4.49; 95% CI, 1.69–11.90); however, because the precise time at which the medication was actually stopped cannot be determined from the data we cannot infer any causal relationship from this association.
3.4. Readmissions after Index Hypoglycemia
In contrast to readmissions following index hyperglycemia hospitalizations, there was no association between the risk of recurrent hypoglycemic events and patient age. Of the individual diabetes complications, heart failure was independently associated with lower risk of recurrent hypoglycemia (OR 0.46; 95% CI, 0.26–0.86). However, a higher overall comorbidity burden as measured by the CCI significantly increased the risk for recurrent hypoglycemia; OR 2.93 (95% CI 0.94–9.12) for CCI≥4 compared to CCI 0-1. History of prior hospitalizations also increased the risk for recurrent hypoglycemia admissions (OR 2.28; 95% CI, 1.34–3.88). No particular medication class or treatment change was associated with recurrent hypoglycemia in either the primary (Table 3) or sensitivity (Table A.3) analyses.
Because there were only 11 episodes of severe hyperglycemia following index hospitalization for hypoglycemia, we were unable to model this outcome.
4. Discussion
Severe hypoglycemia and hyperglycemia, particularly when requiring hospitalization, are common, harmful, yet potentially avoidable with optimal diabetes care. Patients experiencing severe hypoglycemia or hyperglycemia are at risk for recurrent events, particularly if risk factors for these events are not identified and addressed. In this study, we examined 6419 hospitalizations for the primary diagnosis of severe hypoglycemia and 6872 for severe hyperglycemia (ketoacidosis and hyperglycemic hyperosmolar state) among commercially insured U.S. adults with established diabetes between 2009 and 2014. We focused on patients with established diabetes to exclude hospitalizations for severe hyperglycemia as the presenting feature of newly diagnosed diabetes. The all-cause 30-day unplanned readmission rates among patients hospitalized for hypoglycemia and hyperglycemia were similar at approximately 10%. This is comparable to the 10.8% all-cause 30-day readmission rate in this patient population reported previously.9 However, patients hospitalized with severe hyperglycemia were almost as likely to be readmitted for recurrent dysglycemia (41.2% of their readmissions were for recurrent hyperglycemia and 3.7% were for new hypoglycemia) as for other causes (55.0%). In contrast, most readmissions among patients who had been hospitalized for hypoglycemia were for unrelated causes (86.3%) with only 12.0% of readmissions being for recurrent hypoglycemia and 1.7% for new hyperglycemia. The overall readmission rates were lower than in a prior study of hypoglycemia and hyperglycemia hospitalizations between 1999 and 2010, where readmission rates (in 2010) were 18.1% and 16.4%, respectively.10 However, that study was conducted among older Medicare beneficiaries whose risk of any readmission is higher. Ultimately, the fact that patients are more likely to experience the same type of dysglycemic event as their index hospitalization underscores the importance of timely intervention, particularly during or immediately after the index hospitalization, to prevent their recurrence.
A common scenario among patients hospitalized for severe hyperglycemia was readmission for a recurrent hyperglycemic event. Although claims data cannot be used to reliably ascertain diabetes type, we expect that many of these patients have type 1 diabetes as they were generally young, insulin-treated, with fewer diabetes complications and other comorbidities, but with higher prevalence of prior severe hyperglycemic events. Because diabetes was often their primary chronic health problem (36% had CCI≤1), it is not unexpected that 45% of their readmissions were for severe dysglycemia. The high rate of rehospitalization for recurrent hyperglycemia raises the possibility of unmitigated risk factors such as inadequate self-management education or resources, medication non-adherence or inability to obtain them, and socioeconomic barriers to diabetes- and self-care.42 Social services, medication management, care coordination, and diabetes self-management education may therefore benefit patients experiencing recurrent hyperglycemic events.
Lack of treatment intensification following the index hyperglycemia hospitalization may also increase the risk of hyperglycemia readmissions. Only 18% of patients had one or more glucose-lowering medications added subsequent to index hospital discharge, yet doing so decreased the risk of hyperglycemia readmissions by 60%. A similar observation was made by Wei et al, who found that diabetes treatment intensification during hospitalization for any cause was associated with a lower rate of all-cause 30-day readmission.43 It is possible that the true rate of treatment intensification was higher than presented here, as 85% of patients hospitalized for hyperglycemia were treated with insulin, and insulin dose changes (in this case, dose increases) cannot be captured in claims data. However, misclassification of treatment intensification as “no change” would artificially lower the association between treatment intensification and hyperglycemia readmission toward the null, suggesting that the real effect of treatment intensification on the probability of hyperglycemia-related readmissions is even higher than measured in our analysis. This finding underscores the potential harms of the lack of treatment intensification or patient inability to fill prescribed medications in the face of severe hyperglycemia.
Patients hospitalized with severe hypoglycemia were most likely to be readmitted for other primary causes. Only a small fraction (1.7%) experienced recurrent severe hypoglycemia and almost none returned with severe hyperglycemia that would have resulted from potential overreaction to the index hypoglycemic event and discontinuation of glucose-lowering therapies. Consistent with prior studies, patients hospitalized for severe hypoglycemia were older,15,21 had a greater comorbidity burden (46% of patients had CCI ≥4), more diabetes complications, and were more often treated with sulfonylureas. Notably, heart failure was the only chronic health condition associated with a lower probability of recurrent hypoglycemia hospitalizations (and possibly other readmissions as well, though those did not reach statistical significance). This may reflect widespread efforts to improve heart failure care and to reduce hospitalizations and readmissions among patients with heart failure as motivated by the CMS Readmission Reduction Program and other heart failure focused performance metrics. Higher rates of hypoglycemia hospitalizations among older patients may reflect an impaired ability to successfully manage hypoglycemia at home, whether it is because older patients are more likely to live alone (do not have a caregiver to detect and/or treat hypoglycemia), be frail, or have other health problems that predispose them to hypoglycemia. Older and clinically complex patients may also be more likely to be transported to the hospital by concerned caregivers or emergency medical services, and be more likely to be hospitalized for it. As such, younger and healthier patients may still be experiencing severe hypoglycemia, but are not hospitalized and thus not captured in this study.
We also found that only 25% of patients hospitalized for hypoglycemia had one or more of their glucose-lowering medications discontinued (i.e. not refilled) within 120 days of index hospital discharge. Treatment de-intensification among elderly insulin-treated patients with type 2 diabetes who experienced hypoglycemia has been shown to significantly lower the risk of recurrent events.44 Such low prevalence of treatment de-intensification among high risk individuals is consistent with prior studies,45,46 though none focused specifically on patients hospitalized for hypoglycemic events. We acknowledge that use of claims data to identify short-term treatment changes has limitations. Patients treated with insulin (nearly 55% of those hospitalized for hypoglycemia) may have had their dose lowered, yet this is not captured in claims. Conversely, some patients who did not refill their medication during the 120 days following their index hospitalization may have discontinued it after the 30-day period during which readmissions were ascertained. Nonetheless, rates of treatment de-intensification among patients hospitalized for hypoglycemia remain low and concerning.
We found that patients first hospitalized for hyperglycemia and then readmitted for hypoglycemia were more than 4-fold more likely to discontinue a medication during the 120-day period following their index (hyperglycemia) stay. It would make most sense for this medication discontinuation to occur following the hypoglycemia-related readmission rather than the hyperglycemia-related index hospitalization, but as discussed earlier this cannot be determined from the data. Conversely, it is possible that patients who experience hyperglycemia followed by hypoglycemia hospitalizations face significant socioeconomic challenges, whereby they do not refill their medications due to financial hardship (also a contributor to hyperglycemia) and their hypoglycemia occurs as a result of food insecurity. The potential role of food insecurity as a contributing factor to hypoglycemia risk is reinforced by the greater prevalence of lower income patients among those experiencing hypoglycemia and is consistent with prior studies.25,47 While the association of income with recurrent events failed to reach statistical significance, this may be because lower income is a risk factor for both hypoglycemic and hyperglycemic events,47 or because our measure of income was based on geographic residence and not the individual household. Nonetheless, addressing challenges with medication adherence and food insecurity may help improve patient care and health outcomes.
Though this is the largest study of readmissions specifically for recurrent severe dysglycemia following index hospitalizations for severe dysglycemia, there are several limitations to our findings. First, as with any observational study, causal inferences cannot be made. However we have included a wide range of demographic, clinical, and treatment factors, making the existence of an unobserved confounder less likely. Second, limited information about medication dose, time of discontinuation, and whether discontinuation was initiated by a healthcare provider or the patient precludes us from drawing definitive conclusions regarding the effects of individual drug classes and changes to the treatment regimen. Furthermore, while 12% of patients had more than one index admission, this was not accounted for in the analysis, primarily because these multiple observations were not nested within hospitals, which we did account for, making a model with the correct error structure difficult to estimate. Because most patients had just one observation, we would not expect the standard errors to be more than marginally contracted relative to those from a model which accounted for the repeated measures; still, marginal P-values (i.e. those close to significance) should be interpreted with some caution.
We also could not identify the precipitating factors for either the index or the recurrent severe hypoglycemic and hyperglycemic events. The understanding of severe dysglycemia in the real-world setting would be markedly enhanced by systematic assessment and documentation of hypoglycemic and hyperglycemic events, risk factors, and triggers. We could not capture the duration of diabetes (though presence of multiple diabetes complications ascertained using the DCSI may be a surrogate for longer duration of disease) as well as important social determinants of health and mental health conditions, which impact the likelihood of hypoglycemia23,25–27 and hyperglycemia hospitalizations.23,28,29 Our study relied on claims data of commercially-insured and Medicare Advantage beneficiaries, and patients with other or no healthcare coverage may face different medical, social, and economic challenges affecting their dysglycemia and readmission risks. Finally, while we could not assess the impact of glycemic control on readmission risk, HbA1c was not previously shown to be a reliable discriminating risk factor between hypoglycemic and hyperglycemic events.11,23,24 Nonetheless, our findings are consistent with prior literature, build upon existing knowledge, and identify key areas for further evaluation, intervention, and practice improvement Importantly, it reinforces the importance of reevaluating glucose-lowering therapy particularly among patients hospitalized for hyperglycemia; improving ambulatory diabetes care, including sick day management; and not neglecting the patients’ other comorbidities particularly when hospitalized for hypoglycemia.
5. Conclusions
Hospitalizations for severe hypoglycemia and hyperglycemia continue to be common and 10% result in 30-day readmission. Patients hospitalized for severe hyperglycemia are likely to be readmitted for recurrent hyperglycemia, while patients hospitalized for hypoglycemia are generally readmitted for unrelated causes. Importantly, these data represent only a fraction of severe hypoglycemic and hyperglycemic events experienced by patients with diabetes, as most episodes do not result in hospitalization particularly among patients with the knowledge, resources, and capacity to manage such events at home. Our findings underscore the importance of individualized discharge planning for patients hospitalized with severe hypoglycemia and hyperglycemia, recognizing the high rate of potentially preventable readmissions for glycemic crises particularly among patients hospitalized for hyperglycemia.
Supplementary Material
Acknowledgments
Author contributions: Dr. McCoy had full access to all the data in the study and serves as the guarantors for this work, taking responsibility for the integrity of the data and the accuracy of the data analysis. Study conception and design: McCoy, Shah. Acquisition of data: Herrin, Shah. Interpretation of data: McCoy, Herrin, Shah. Drafting of the manuscript: McCoy. Critical revision of the manuscript for important intellectual content: McCoy, Lipska, Herrin, Shah. Statistical analysis: Herrin. Obtained funding: McCoy, Shah. Administrative, technical, and material support: N/A. Study supervision: Shah.
Funding: RGM is supported by the National Institute Of Diabetes And Digestive And Kidney Diseases of the National Institutes of Health under Award Number K23DK114497. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. KJL receives support from the National Institute on Aging and the American Federation of Aging Research through the Paul Beeson Career Development Award (K23AG048359) and the Yale Claude D. Pepper Older Americans Independence Center (P30AG021342). She also receives support from CMS to develop and maintain publicly reported quality measures.
Declarations of interest: None
References
- 1.Khunti K, Davies M, Majeed A, Thorsted BL, Wolden ML, Paul SK. Hypoglycemia and risk of cardiovascular disease and all-cause mortality in insulin-treated people with type 1 and type 2 diabetes: a cohort study. Diabetes Care. 2015;38(2):316–322. doi: 10.2337/dc14-0920. [DOI] [PubMed] [Google Scholar]
- 2.Goto A, Arah OA, Goto M, Terauchi Y, Noda M. Severe hypoglycaemia and cardiovascular disease: systematic review and meta-analysis with bias analysis. BMJ. 2013;347:f4533. doi: 10.1136/bmj.f4533. [DOI] [PubMed] [Google Scholar]
- 3.Gibb FW, Teoh WL, Graham J, Lockman KA. Risk of death following admission to a UK hospital with diabetic ketoacidosis. Diabetologia. 2016;59(10):2082–2087. doi: 10.1007/s00125-016-4034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams SA, Shi L, Brenneman SK, Johnson JC, Wegner JC, Fonseca V. The burden of hypoglycemia on healthcare utilization, costs, and quality of life among type 2 diabetes mellitus patients. J Diabetes Complications. 2012;26(5):399–406. doi: 10.1016/j.jdiacomp.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 5.Veronese G, Marchesini G, Forlani G, et al. Costs associated with emergency care and hospitalization for severe hypoglycemia. Nutr Metab Cardiovasc Dis. 2016;26(4):345–351. doi: 10.1016/j.numecd.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Foos V, Varol N, Curtis BH, et al. Economic impact of severe and non-severe hypoglycemia in patients with Type 1 and Type 2 diabetes in the United States. J Med Econ. 2015;18(6):420–432. doi: 10.3111/13696998.2015.1006730. [DOI] [PubMed] [Google Scholar]
- 7.Willis WD, Diago-Cabezudo JI, Madec-Hily A, Aslam A. Medical resource use, disturbance of daily life and burden of hypoglycemia in insulin-treated patients with diabetes: results from a European online survey. Expert Rev Pharmacoecon Outcomes Res. 2013;13(1):123–130. doi: 10.1586/erp.12.80. [DOI] [PubMed] [Google Scholar]
- 8.McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA. Self-Report of Hypoglycemia and Health-Related Quality of Life in Patients with Type 1 and Type 2 Diabetes. Endocrine Practice. 2013:1–28. doi: 10.4158/EP12382.OR. [DOI] [PubMed] [Google Scholar]
- 9.McCoy RG, Lipska KJ, Herrin J, Jeffery MM, Krumholz HM, Shah ND. Hospital Readmissions among Commercially Insured and Medicare Advantage Beneficiaries with Diabetes and the Impact of Severe Hypoglycemic and Hyperglycemic Events. J Gen Intern Med. 2017 Oct;32(10):1097–1105. doi: 10.1007/s11606-017-4095-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lipska KJ, Ross JS, Wang Y, et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, 1999 to 2011. JAMA Intern Med. 2014;174(7):1116–1124. doi: 10.1001/jamainternmed.2014.1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pathak RD, Schroeder EB, Seaquist ER, et al. Severe Hypoglycemia Requiring Medical Intervention in a Large Cohort of Adults With Diabetes Receiving Care in U.S. Integrated Health Care Delivery Systems: 2005–2011. Diabetes Care. 2016;39(3):363–370. doi: 10.2337/dc15-0858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.CMS. [Accessed March 14, 2018];2015 Measure Information about the 30-Day All-Cause Hospital Readmission Measure, Calculated for the Value-Based Payment Modifier Program. 2017 https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeedbackProgram/Downloads/2015-ACR-MIF.pdf.
- 13.CMS. Accountable Care Organization 2017 Quality Measure Narrative Specifications. Waltham, MA, USA: RTI International; 2017. Prepared for the Next Generation ACO Model, Division of Accountable Care Organization Populations Seamless Care Models Group, Center for Medicare and Medicaid Innovation & the Medicare Shared Savings Program, Division of Shared Savings Program, Performance-Based Policy Group, Center for Medicare, Centers for Medicare and Medicaid Services. [Google Scholar]
- 14.Mays JA, Jackson KL, Derby TA, et al. An Evaluation of Recurrent Diabetic Ketoacidosis, Fragmentation of Care, and Mortality Across Chicago, Illinois. Diabetes Care. 2016;39(10):1671–1676. doi: 10.2337/dc16-0668. [DOI] [PubMed] [Google Scholar]
- 15.Fu H, Xie W, Curtis B, Schuster D. Identifying factors associated with hypoglycemia-related hospitalizations among elderly patients with T2DM in the US: a novel approach using influential variable analysis. Curr Med Res Opin. 2014;30(9):1787–1793. doi: 10.1185/03007995.2014.922944. [DOI] [PubMed] [Google Scholar]
- 16.McCoy RG, Lipska KJ, Yao X, Ross JS, Montori VM, Shah ND. Intensive Treatment and Severe Hypoglycemia Among Adults With Type 2 Diabetes. JAMA Intern Med. 2016;176(7):969–978. doi: 10.1001/jamainternmed.2016.2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. New England Journal of Medicine. 2008;358(24):2545–2559. doi: 10.1056/NEJMoa0802743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837–853. [PubMed] [Google Scholar]
- 19.Huang ES, Laiteerapong N, Liu JY, John PM, Moffet HH, Karter AJ. Rates of complications and mortality in older patients with diabetes mellitus: the diabetes and aging study. JAMA Intern Med. 2014;174(2):251–258. doi: 10.1001/jamainternmed.2013.12956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Predictors of nonsevere and severe hypoglycemia during glucose-lowering treatment with insulin glargine or standard drugs in the ORIGIN trial. Diabetes Care. 2015;38(1):22–28. doi: 10.2337/dc14-1329. [DOI] [PubMed] [Google Scholar]
- 21.Wang J, Geiss LS, Williams DE, Gregg EW. Trends in Emergency Department Visit Rates for Hypoglycemia and Hyperglycemic Crisis among Adults with Diabetes, United States, 2006–2011. PLoS One. 2015;10(8):e0134917. doi: 10.1371/journal.pone.0134917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bruderer SG, Bodmer M, Jick SS, Bader G, Schlienger RG, Meier CR. Incidence of and risk factors for severe hypoglycaemia in treated type 2 diabetes mellitus patients in the UK--a nested case-control analysis. Diabetes Obes Metab. 2014;16(9):801–811. doi: 10.1111/dom.12282. [DOI] [PubMed] [Google Scholar]
- 23.Weinstock RS, Xing D, Maahs DM, et al. Severe hypoglycemia and diabetic ketoacidosis in adults with type 1 diabetes: results from the T1D Exchange clinic registry. J Clin Endocrinol Metab. 2013;98(8):3411–3419. doi: 10.1210/jc.2013-1589. [DOI] [PubMed] [Google Scholar]
- 24.Lipska KJ, Warton EM, Huang ES, et al. HbA1c and risk of severe hypoglycemia in type 2 diabetes: the Diabetes and Aging Study. Diabetes Care. 2013;36(11):3535–3542. doi: 10.2337/dc13-0610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seligman HK, Bolger AF, Guzman D, Lopez A, Bibbins-Domingo K. Exhaustion of food budgets at month's end and hospital admissions for hypoglycemia. Health Aff (Millwood) 2014;33(1):116–123. doi: 10.1377/hlthaff.2013.0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berkowitz SA, Karter AJ, Lyles CR, et al. Low socioeconomic status is associated with increased risk for hypoglycemia in diabetes patients: the Diabetes Study of Northern California (DISTANCE) J Health Care Poor Underserved. 2014;25(2):478–490. doi: 10.1353/hpu.2014.0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bradford AL, Crider CC, Xu X, Naqvi SH. Predictors of Recurrent Hospital Admission for Patients Presenting With Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State. J Clin Med Res. 2017;9(1):35–39. doi: 10.14740/jocmr2792w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lohiya S, Kreisberg R, Lohiya V. Recurrent diabetic ketoacidosis in two community teaching hospitals. Endocr Pract. 2013;19(5):829–833. doi: 10.4158/EP13057.RA. [DOI] [PubMed] [Google Scholar]
- 29.Simmons D, Hartnell S, Davenport K, Jenaway A. Risk factors for recurrent admissions with diabetic ketoacidosis: importance of mental health. Diabet Med. 2017;34(3):451. doi: 10.1111/dme.13202. [DOI] [PubMed] [Google Scholar]
- 30.Optum. [Accessed March 14, 2018];Optum Research Data Assets. 2015 Jun;2015 https://www.optum.com/content/dam/optum/resources/productSheets/5302_Data_Assets_Chart_Sheet_ISPOR.pdf. [Google Scholar]
- 31.Wallace PJ, Shah ND, Dennen T, Bleicher PA, Crown WH. Optum Labs: Building A Novel Node In The Learning Health Care System. Health Aff (Millwood) 2014;33(7):1187–1194. doi: 10.1377/hlthaff.2014.0038. [DOI] [PubMed] [Google Scholar]
- 32.Ginde AA, Blanc PG, Lieberman RM, Camargo CA., Jr Validation of ICD-9-CM coding algorithm for improved identification of hypoglycemia visits. BMC Endocr Disord. 2008;8:4. doi: 10.1186/1472-6823-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.AHRQ. AHRQ QITM Research Version 5.0, Prevention Quality Indicators (PQI) #1, Technical Specifications. [Accessed March 16, 2018];Diabetes Short-Term Complications Admission Rate. 2015 http://www.qualityindicators.ahrq.gov/
- 34.National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS) Comprehensive Diabetes Care. Washington, D.C: National Committee for Quality Assurance; 2015. pp. 74–98. [Google Scholar]
- 35.Horwitz LI, Grady JN, Dorsey KB, et al. 2014 Measures Updates and Specifications Report: Hospital-Wide All-Cause Unplanned Readmission (Version 3.0) 2014 Submitted by Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE). Prepared for Centers for Medicare & Medicaid Services (CMS). Available at file: ///C:/Users/m070233/Downloads/Hosp-Wide_Rdmsn_Msr_Updts_032114.pdf.
- 36.National Quality Measures Clearinghouse. All-cause readmissions: the number of acute inpatient stays during the measurement year that were followed by an acute readmission for any diagnosis within 30 days and the predicted probability of an acute readmission, for patients 18 years of age and older. [Accessed 6/29/2016];2015 http://www.qualitymeasures.ahrq.gov/content.aspx?id=48857.
- 37.Chang HY, Weiner JP, Richards TM, Bleich SN, Segal JB. Validating the adapted Diabetes Complications Severity Index in claims data. American Journal of Managed Care. 2012;18(11):721–726. [PubMed] [Google Scholar]
- 38.Charlson ME, Pompei P, Ales KA, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 39.Pauly NJ, Brown JD. Prevalence of Low-Cost Generic Program Use in a Nationally Representative Cohort of Privately Insured Adults. J Manag Care Spec Pharm. 2015;21(12):1162–1170. doi: 10.18553/jmcp.2015.21.12.1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. [Accessed April 29, 2015];2015 Measure Updates and Specifications Report Hospital-Wide All-Cause Unplanned Readmission Measure – Version 4.0. 2015 Mar;2015 Submitted by Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE). Prepared for Centers for Medicare & Medicaid Services (CMS) http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. [Google Scholar]
- 41.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: J. Wiley & Sons; 1987. [Google Scholar]
- 42.Umpierrez G, Korytkowski M. Diabetic emergencies - ketoacidosis, hyperglycaemic hyperosmolar state and hypoglycaemia. Nat Rev Endocrinol. 2016;12(4):222–232. doi: 10.1038/nrendo.2016.15. [DOI] [PubMed] [Google Scholar]
- 43.Wei NJ, Wexler DJ, Nathan DM, Grant RW. Intensification of diabetes medication and risk for 30-day readmission. Diabet Med. 2013;30(2):e56–62. doi: 10.1111/dme.12061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Munshi MN, Slyne C, Segal AR, Saul N, Lyons C, Weinger K. Simplification of Insulin Regimen in Older Adults and Risk of Hypoglycemia. JAMA Intern Med. 2016;176(7):1023–1025. doi: 10.1001/jamainternmed.2016.2288. [DOI] [PubMed] [Google Scholar]
- 45.McCoy RG, Van Houten HK, Ross JS, Montori VM, Shah ND. HbA1c overtesting and overtreatment among US adults with controlled type 2 diabetes, 2001–13: observational population based study. BMJ. 2015;351:h6138. doi: 10.1136/bmj.h6138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sussman JB, Kerr EA, Saini SD, et al. Rates of Deintensification of Blood Pressure and Glycemic Medication Treatment Based on Levels of Control and Life Expectancy in Older Patients With Diabetes Mellitus. JAMA Intern Med. 2015:1–8. doi: 10.1001/jamainternmed.2015.5110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Seligman HK, Davis TC, Schillinger D, Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved. 2010;21(4):1227–1233. doi: 10.1353/hpu.2010.0921. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.