Abstract
One complication of an autogenous arteriovenous fistula (AVF) for hemodialysis is the formation of a venous aneurysm. The treatment of a massive aneurysmal AVF generally involves ligation or resection with the use of prosthetic interposition. We present the case of a 46-year-old man in whom an AVF aneurysm was successfully treated by placating the excess free wall of the aneurysm with sutures. This method is a simple and effective intervention for managing aneurysm-associated complications. In addition, this approach helps to maintain the benefits of autogenous access while conserving future dialysis sites.
Keywords: arteriovenous fistula aneurysm, hemodialysis, vascular access
An autogenous arteriovenous fistula (AVF) is a widely accepted approach to obtaining vascular access for patients with end-stage renal disease on chronic hemodialysis. This approach is associated with a low complication and high patency rate. However, even though AVFs are superior to catheters and grafts, nearly one-third of all AVFs develop complications, including thrombosis, stenosis, venous aneurysm formation, and infection. The incidence of aneurysm formation is approximately 5% to 6%.1 Expansion of the venous aneurysm not only reduces the available sites for cannulation but can also lead to thrombosis and rupture with fatal hemorrhage. The treatment of a massive aneurysmal AVF generally involves ligation or resection with the use of prosthetic interposition. However, these procedures usually need to sacrifice the AVF or, at least, the benefit of an autogenous AVF. We present a case in which an uncomplicated giant AVF aneurysm was successfully treated using a method that involved narrowing the aneurysmal segment to salvage autogenous dialysis access.
PATIENT REPORT
A 46-year-old man began hemodialysis for his end-stage renal failure due to renal sclerosis 5 years prior to his visit. He had an AVF created in his left forearm. He experienced no blood flow problems through his AVF, but enlargement of the AVF had gradually developed (Fig. 1). An echogram indicated an aneurysm that was 5.5 cm in maximum diameter; there was no indication of stenosis within the anastomosis or the aneurysm. Because the patient was young, we chose a technique to salvage autogenous dialysis access in order to maintain the benefits while conserving future dialysis sites. The procedure was done under general anesthesia. An incision over the aneurysm was made longitudinally and the dilated venous aneurysm was completely skeletonized. Heparin was given intravenously. Proximal and distal control of the fistula was obtained using vascular clamps (Fig. 2). The aneurysmal fistula was then opened longitudinally along its entire length (Fig. 3A). The excess length secondary to the tortuosity of the aneurysmal fistula was resected. A back wall anastomosis was constructed using a 5-0 polypropylene suture in a running fashion (Fig. 3B). To reconstruct a fistula 8-10 mm in diameter, a clear plastic tube of the appropriate size was inserted into the fistula (Fig. 3C). Using the tube as a guide, the excess wall of the fistula was resected. The fistula was then closed over the tube using a 5-0 polypropylene running suture and the tube was removed just before finishing the suture (Fig. 3D). The excess skin over the fistula was then resected. Finally, the skin was closed in two layers using absorbable sutures (Fig. 4). The operation time was 171 min, and the patient experienced some bleeding (355 mL). He was discharged the following day. We were able to cannulate the site 2 weeks after the operation. This AVF is still highly functional and no aneurysm recurrence has been observed during the 4 year follow-up period.
Fig. 1.
The picture of the AVF aneurysm of this patient. A: An AVF aneurysm in the left forearm. B: Magnified view of the AVF aneurysm. The extent of the aneurysm is marked. AVF, autogenous arteriovenous fistula.
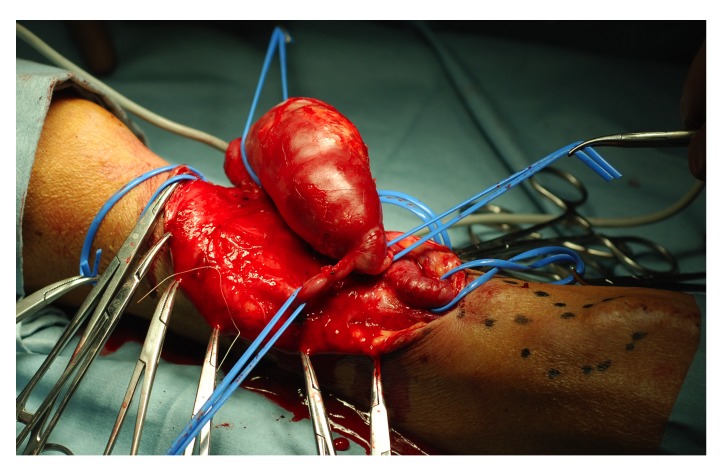
Fig. 2.
The surgical view of the AVF aneurysm. The proximal and distal portions of the AVF were encircled with the vessel tape. A couple of side branches were also encircled. AVF, autogenous arteriovenous fistula.
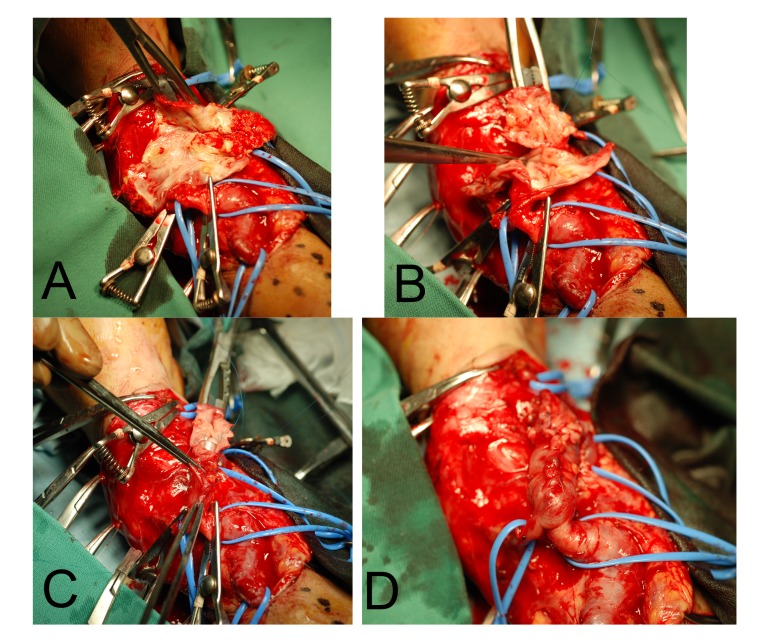
Fig. 3.
The picture of the surgical procedure. A: The proximal and distal portions of the AVF were clamped and the aneurysm was opened. B: The aneurysm was resected, and the back wall was approximated partially with a polypropylene suture. C: A plastic tube was placed inside the AVF and the AVF was closed with polypropylene sutures after the resection of redundant side wall. D: Completion of the remodeling. AVF, autogenous arteriovenous fistula.
Fig. 4.
After the skin closure, the AVF aneurysm completely disappeared. AVF, autogenous arteriovenous fistula.
DISCUSSION
An AVF aneurysm occurs due to collagen matrix degeneration of the vein wall. Repeated puncture on the same site may weaken the venous wall and could be one of the causes for the formation of an AVF aneurysm. An AVF aneurysm is commonly seen as a complication of autogenous AVF, while the incidence of rupture is reported to be 0.8% to 5.2%.2, 3 Since an AVF aneurysm can limit the available areas for needling in dialysis and could possibly rupture causing fatal hemorrhage, its potential danger cannot be ignored.
Ligation of the AVF is an effective method to prevent rupture. However, with this procedure, the functional vascular access must be sacrificed, and the patient needs to have a new AVF created at another site. Aneurysm resection using a prosthetic interposition is another effective method, which can salvage the AVF without sacrificing the areas of cannulation. However, the long-term patency of a prosthetic graft is less than that of the native AVF. Another method involves endovascular treatments using covered stents, which can prevent further aneurysmal dilatation.4, 5 However, the drawback of this method is the increased risk of infection with the artificial material inside the AVF. In addition, the needling for dialysis with this method is usually difficult over the covered stents.
With our procedure, the AVF aneurysm could be remodeled to an appropriate size with a tube as a guide. The native fistula was salvaged and the distal portion of the remodeled fistula was used for the cannulation of the dialysis even on the day after the procedure. Thus, the placement of a temporary catheter can be avoided. Furthermore, long-term patency seems to be satisfactory without aneurysm recurrence. Hong-Yee et al. reported a similar surgical treatment for an AVF aneurysm, in which they only plicated the aneurysm.6 Since the plication method is not necessary to resect the aneurysm, the operation time can be shorter if it is not included in the procedure. However, with the plication only approach, the reduction of the aneurysm size could be inappropriate, and recurrence of the aneurysm is anticipated. Bachleda et al introduced a similar surgical remodeling method for an AVF aneurysm.7 Hossny reported the midterm results of 14 patients remodeled with this method; all of the remodeled AVFs maintained adequate function, providing vascular access for dialysis during the mean follow-up period of 30.4 months.8 Although favorable results were reported, only a limited number of patients with AVF aneurysms have been treated with this remodeling approach. Technically, this procedure can be performed almost all the AVF aneurysms, but the drawbacks of this method are as follows: 1. The duration of the operation is longer than that of other methods. 2. General anesthesia is necessary in most of the cases. 3. The amount of blood loss could be more than other methods because the area of dissection needs to be more extensive. For our 46-year-old male patient, the remodeled AVF is functioning adequately, providing vascular access 4 years after the operation, which is consistent with other reports. The patient has not experienced aneurysm recurrence. In a successful AVF, the vein receiving the increased blood flow becomes arterialized (lumen enlargement and wall thickening). These morphologic changes can allow for repeated punctures. Our procedure preserves and utilizes the already thickened vein wall, while removing the aneurysm. That could be the reason the recurrence of the AVF aneurysm is rare by this procedure. Irrespective of the above-mentioned drawbacks, surgical remodeling of an AVF is useful, especially for young patients in whom the preservation of a functioning native AVF is of great benefit.
In conclusion, surgical remodeling of an AVF aneurysm is a safe and effective procedure to treat an aneurysm and salvage the native AVF. The long-term results are also satisfactory since aneurysm recurrence is unlikely.
The authors declare no conflict of interest.
REFERENCES
- 1. Diskin CJ, Stokes TJ, Dansby LM, Radcliff L, Carter TB, et al. Understanding the pathophysiology of hemodialysis access problems as a prelude to developing innovative therapies. Nat Clin Pract Nephrol. 2008;4:628-38. doi: 10.1038/ncpneph0947 [DOI] [PubMed] [Google Scholar]
- 2. Haimov M, Baez A, Neff M, Slifkin R. Complications of arteriovenous fistulas for hemodialysis. Arch Surg. 1975;110:708-12. [DOI] [PubMed] [Google Scholar]
- 3. Zibari GB, Rohr MS, Landreneau MD, Bridges RM, DeVault GA, Petty FH, et al. Complications from permanent hemodialysis vascular access. Surgery. 1988;104:681-6. [PubMed] [Google Scholar]
- 4. Grauhan O, Zurbrügg HR, Hetzer R. Management of aneurysmal arteriovenous fistula by a perivascular metal mesh. Eur J Vasc Endovasc Surg. 2001;21:274-5. doi: 10.1053/ejvs.2001.1265 [DOI] [PubMed] [Google Scholar]
- 5. Kershen LM, Marichal DA. Endovascular treatment of stent fracture and pseudoaneurysm formation in arteriovenous fistula dialysis access. Proc Bayl Univ Med Cent. 2013;26:47-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lo HY, Tan SG. Arteriovenous fistula aneurysm-plicate, not ligate. Ann Acad Med Singapore. 2007;36:851-3. [PubMed] [Google Scholar]
- 7. Bachleda P, Utíkal P, Kalinová L, Váchalová M. Surgical remodelling of haemodialysis fistula aneurysms. Ann Acad Med Singapore. 2011;40:136-9. [PubMed] [Google Scholar]
- 8. Hossny A. Partial aneurysmectomy for salvage of autogenous arteriovenous fistula with complicated venous aneurysms. J Vasc Surg. 2014;59:1073-7. doi: 10.1016/j.jvs.2013.10.083 [DOI] [PubMed] [Google Scholar]