Abstract
We herein present a surgically treated case of huge adrenal myelolipoma. A 62-year-old woman presented to our surgical outpatient clinic with a retroperitoneal tumor. A clinical examination revealed an elastic soft, smooth-surfaced, painless, child-head-sized tumor with poor mobility, which was located in the left upper abdomen. Computed tomography (CT) and magnetic resonance imaging (MRI) of the abdomen revealed an uneven tumor surrounding the stomach, spleen, pancreas, and left kidney, which was 20 × 18 × 10 cm in size. The retroperitoneal tumor was resected. The tumor was attached to the surrounding organs, including the pancreas, spleen, and left kidney, but had not directly invaded these organs. The tumor was yellow and elastic soft and covered with a thin film. The origin of the tumor was suggested to be the left adrenal gland. The weight of the excised tumor was 1500 g. The histopathological diagnosis was adrenal myelolipoma. The patient had an uneventful recovery and was discharged from the hospital on the thirteenth day after the operation. She has been followed up in our outpatient clinic.
1. Introduction
Adrenal myelolipoma (AML) is a relatively rare benign tumor composed of mature adipose tissues and a variable amount of hematopoietic elements. The male-to-female ratio is 1 : 1. The incidence of AML is reported to be 0.08–0.4% at autopsy [1]. AMLs are nonfunctional tumors that are usually asymptomatic; however, they have been known to coexist with other endocrine disorders, such as Cushing's syndrome, congenital adrenal hyperplasia (CAH), Conn's syndrome, and pheochromocytoma [2–4]. Recently, AMLs have been reported in patients with CAH with increasing frequency. One study indicated that myelolipoma was detected in 4% of patients with CAH [5].
The largest AML (size, 31 × 24.5 × 11.5 cm; weight, 6000 g) in a patient without endocrine disorder was described by Akamatsu et al. [6], while the largest AML in a patient with CAH (size, 34 × 24 × 10.5 cm; weight, 5900 g) was described by Boudreaux et al. [7].
We herein report a relatively rare case of a giant AML of 1500 g in weight in a patient without endocrine disorder and discuss our analysis of the literature.
2. Case Report
A 62-year-old Japanese female patient presented with a left abdominal mass. She was referred to our surgical outpatient clinic to undergo a detailed examination and treatment for the left abdominal mass. A clinical examination revealed an elastic soft, smooth-surfaced, painless, child-head-sized tumor with poor mobility, which was located in the left upper abdomen. Abdominal computed tomography (CT) demonstrated a child-head-sized mass with heterogeneous contrast at the left upper abdomen around the stomach, spleen, pancreas, and left kidney on a horizontal image (Figure 1(a)) and coronal image (Figure 1(b)).
Figure 1.

Abdominal computed tomography (CT) demonstrated a child-head-sized mass with heterogeneous contrast located in the left upper abdomen around the stomach, spleen, pancreas, and left kidney on the horizontal (a) and coronal (b) images.
Magnetic resonance imaging (MRI) revealed a heterogeneously hyperintense mass on T1-weighted imaging (Figure 2(a)), a relatively uniform and hyperintense mass on T2-weighted imaging (Figure 2(b)), and a hypointense mass with an enhanced border on gadolinium- (Gd-) enhanced imaging (Figure 2(c)). A retroperitoneal tumor was diagnosed. Her laboratory data were white blood cell count, 4600/mm3; hemoglobin, 12.8 g/dl; hematocrit, 36.5%; and platelet count, 182,000/mm3, with normal electrolytes, as well as normal blood urea nitrogen levels, but slight liver dysfunction. Her serum levels of corticosteroid and/or androgen were 13.3 ng/ml (10.4–35.0 in female) and 173 pg/dl (35.7–240.0), respectively, which are within the normal ranges; however, her serum level of ACTH was elevated at 138.70 pg/ml (7.2–63.3).
Figure 2.

Magnetic resonance imaging (MRI) revealed a heterogeneously hyperintense mass on T1-weighted imaging (a), a relatively uniform and hyperintense mass on T2-weighted imaging (b), and a hypointense mass with an enhanced border on Gd-enhanced imaging (c).
The retroperitoneal tumor was resected (Figure 3). The tumor was located at the left side of the stomach, posteriorly to the transverse mesocolon and pancreas, on the cranial side of the left kidney (Figures 1 and 2), but has not invaded the surrounding organs (Figures 1 and 2). The right adrenal gland was normal in size. The resected tumor was 20 × 18 × 10 cm in diameter and weighted 1500 g. An examination of the cut surface of the tumor revealed a multilobular yellow mass with bleeding in places (Figure 4).
Figure 3.
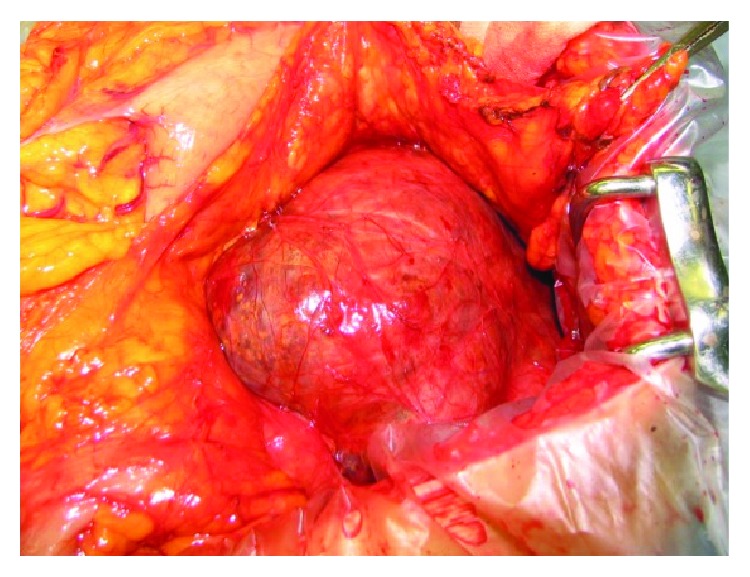
The operative findings revealed a yellow mass covered with a thin layer that was located at the left side of the stomach, posteriorly to the transverse mesocolon and pancreas, on the cranial side of the left kidney.
Figure 4.

An examination of the cut surface of this tumor revealed a multilobular yellow mass with bleeding in places.
A histopathological examination with hematoxylin and eosin staining revealed that the tumor was composed of a proliferation of mature and variable-sized adipocytes admixed with aggregates of hematopoietic elements, associated with adrenal gland tissue in the peripheral region within the tumor (Figure 5). These findings were compatible with AML.
Figure 5.

A histopathological examination (×200) with hematoxylin and eosin staining revealed that tumor was composed of a proliferation of mature and variable-sized adipocytes admixed with aggregates of hematopoietic elements.
The patient had an uneventful recovery and was discharged from the hospital on the 6th day after the operation. She has been followed up in our outpatient clinic without recurrence for approximately 12 years since undergoing the operation.
3. Discussion
The etiology of AML remains unclear. Some of the hypothesized etiologies include extramedullary hematopoiesis due to the autonomous proliferation of bone marrow cells transferred during embryogenesis, degeneration of epithelial tissues of the adrenal cortex, and adrenocortical cell metaplasia of the reticuloendothelial cells of the blood capillaries in response to stimuli such as necrosis, infection, or stress [1, 8–10]. The most widely accepted theory is that myelolipomas arise due to metaplasia of the reticuloendothelial cells of the blood capillaries in the adrenal gland in response to stimuli such as chronic stress, infection, necrosis, or inflammation [11, 12].
Although the diameter of AMLs ranges from less than 1 cm to more than 30 cm, they are usually less than 5 cm in diameter [13, 14]. AML is often asymptomatic, sometimes leading to very large adrenal masses (≧10 cm in diameter). These are often called “giant AML” [15]. Lawler et al. proposed a definition of the often quoted term “giant” AML [16]. We propose that giant AMLs of ≧1, 500 g should be called “real giant AMLs.” According to this criterion, we found the 21 cases involving giant AMLs in patients without endocrine disorders (Table 1) and the 6 cases involving giant AMLs in patients with CAH (Table 2).
Table 1.
Giant myelolipoma more than 1500 g without endocrine disorder.
| Number | Author | Year | Gender | Age | Site | Size (cm) | Weight (g) | Symptoms | Ref. number |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Akamatsu | 2004 | Male | 51 | Right | 31 × 24.5 × 11.5 | 6000 | Abd. mass, abd. pain | [6] |
| 2 | Wilhelmus | 1981 | Female | 70 | Left | 30 × 22 × 16 | 5500 | Abd. mass, abd. pain | [21] |
| 3 | Mukherjee | 2010 | Male | 56 | Right | 28 × 26 × 17 | 5500 | Abd. mass, weight loss | [22] |
| 4 | Kumar | 2015 | Male | 40 | Right | 38 × 20 × 16 | 5200 | Abd. pain, dyspnea, dizziness | [23] |
| 5 | Brogna | 2011 | Male | 52 | Left | 25 × 20 × 20 | 4400 | No | [24] |
| 6 | O'Daniel-Pierce | 1996 | Male | 67 | Right | 30 × 20 × 11 | 4370 | Abd. pain, abd. mass | [25] |
| 7 | Reshi | 2007 | Male | 45 | Right | 25 × 14 × 11 | >4000 | Abd. mass | [26] |
| 8 | Gautam | 2013 | Male | 52 | Right | 28 × 18 × 12 | 3850 | Abd. pain, headache | [27] |
| 9 | Tanaka | 1998 | Male | 50 | Right | 30 × 25 × 23 | 3500 | Abd. mass | [28] |
| 10 | Dell'Avanzato | 2009 | Male | 43 | Right | 22 × 18 × 9 | 3500 | ND | [29] |
| 11 | Saha | 2015 | Female | 59 | Left | 23 × 16 × 9 | 3300 | Abd. distension, dragging sensation | [30] |
| 12 | Kumaresan | 2011 | Female | 24 | Right | 30 × 20 × 18 | 3000 | Abd. pain, abd. mass | [31] |
| 13 | Gerson | 2015 | Female | 62 | Right | 21 × 18 × 9 | 2468 | Abd. pain, nausea | [32] |
| 14 | Takahashi | 2005 | Male | 48 | Right | 20 × 18 × 16 | 2400 | Abd. distension, fever, diarrhea | [33] |
| 15 | Fernandes | 2010 | Male | 48 | Right | 28 × 20 × 15 | 2200 | Abd. pain, abd. mass | [34] |
| 16 | Chand | 2017 | Male | 35 | Right | 24 × 15 × 12 | 2000 | Pain in the right thigh | [35] |
| 17 | Répássy | 2001 | Female | 50 | Right | 20 × 14 | 1650 | Abd. pain, abd. discomfort | [36] |
| 18 | Andersom | 2010 | Man | 35 | Right | 23.8 × 11.6 × 7.5 | 1575 | Right-sided abd. discomfort | [37] |
| 19 | Goldman | 1996 | Male | 42 | Right | 20.5 × 15 × 8.5 | 1550 | Right frank pain, dizziness, vomiting | [38] |
| 20 | Ersoy | 2006 | Male | 67 | Right | 12 × 10 | 1500 | Abd. pain, fever | [39] |
| 21 | Chakrabarti | 2012 | Female | 40 | Right | 15 × 10 × 8 | 1500 | Abd. pain | [40] |
| 22 | Our case | 2018 | Female | 62 | Left | 20 × 18 × 10 | 1500 | Abd. mass |
ND: not described in abstract.
Table 2.
Giant adrenal myelolipoma more than 1500 g with CAH.
| Number | Author | Year | Gender | Age | Site | Size (cm) | Weight (g) | Symptoms | Ref. number |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Boudreaux | 1979 | Male | 56 | 34 × 24 × 10.5 | 5900 | Dyspnea, low thoracic pain | [7] | |
| 2 | McGeoch | 2012 | Male | 34 | Left | 23 × 19 × 11 | 5800 | Adb. mass | [41] |
| 3 | Kale | 2015 | Male | 51 | Left | 34 × 20 × 13 | 4700 | Back pain | [42] |
| 4 | Alvarez | 2014 | Female | 44 | Left | 26 × 24 × 9.5 | 5090 | Abd. pain, nausea, bilious emesis | [43] |
| 5 | Al-Bahri | 2014 | Male | 39 | Left, right | 30 × 25 × 20 25 × 20 × 13 | 4100, 2700 | Abd. distension, fatigue | [44] |
| 6 | German-Mena | 2011 | Male | 45 | Left | 24.4 × 19.0 × 9.5 | 2557 | Abd. distension, abd. pain | [45] |
CAH: congenital adrenal hyperplasia.
Ultrasonography (US), computed tomography (CT), and magnetic resonance imaging (MRI) are effective for diagnosing AML in ≧90% of cases [4, 17]. Recently, with the widespread use of imaging studies such as US, CT, and MRI, the incidental detection of AML has been more common, and they now represent up to 10–15% of incidentally detected adrenal masses [18]. US shows myelolipoma as a well-defined tumor with varying degrees of hyperechoic (fatty tissue) and hypoechoic (myeloid tissue) components. CT shows myelolipoma as a well-delineated mass with heterogeneous attenuation and low-density fat tissue with more dense areas of myeloid tissue. MRI demonstrates myelolipoma as an area of high signal intensity on T1-weighted and T2-weighted sequences with reduced signal intensity on fat suppression and opposite phase imaging [18, 19].
Management of AML should be individualized. Small lesions, which are asymptomatic and measure less than 5 cm, should be monitored over a period of 1-2 years with imaging controls [20]. On the other hand, surgery is indicated when the patient is symptomatic, when the lesion is more than 5 cm in size due to rupture—which is a rare event—or when malignancy is suspected [20]. The most recognized complication of AML is spontaneous retroperitoneal hemorrhage [14, 16]. Daneshmand et al. suggested that symptomatic tumors or myelolipomas of ≧7 cm in size should be removed because they are associated with an increased risk of spontaneous rupture with retroperitoneal hemorrhage [4].
4. Conclusion
We reported a relatively rare case of a real giant AML that weighted 1500 g in a patient without an endocrine disorder. It is very important to provide suitable management on an individual basis.
Conflicts of Interest
Yoshifumi Nakayama and the other coauthors have no conflicts of interest to declare.
Authors' Contributions
Yoshifumi Nakayama contributed to drafting and editing of the paper. Masaki Akiyama and Yusuke Sawatsubashi contributed to obtaining the clinical details. Jun Nagata contributed to literature search. Nobutaka Matayoshi helped in drafting the paper. Masanori Hisaoka and Keiji Hirata helped in editing the paper.
References
- 1.Olsson C. A., Krane R. J., Klugo R. C., Selikowitz S. M. Adrenal myelolipoma. Surgery. 1973;73(5):665–670. [PubMed] [Google Scholar]
- 2.Wagnerová H., Lazúrová I., Bober J., Sokol L., Zachar M. Adrenal myelolipoma. 6 cases and a review of the literature. Neoplasma. 2004;51(4):300–305. [PubMed] [Google Scholar]
- 3.Yildiz L., Akpolat I., Erzurumlu K., Aydin O., Kandemir B. Giant adrenal myelolipoma: case report and review of the literature. Pathology International. 2000;50(6):502–504. doi: 10.1046/j.1440-1827.2000.01071.x. [DOI] [PubMed] [Google Scholar]
- 4.Daneshmand S., Quek M. L. Adrenal myelolipoma: diagnosis and management. Urology Journal. 2006;3(2):71–74. [PubMed] [Google Scholar]
- 5.Nermoen I., Rørvik J., Holmedal S. H., et al. High frequency of adrenal myelolipomas and testicular adrenal rest tumours in adult Norwegian patients with classical congenital adrenal hyperplasia because of 21-hydroxylase deficiency. Clinical Endocrinology. 2011;75(6):753–759. doi: 10.1111/j.1365-2265.2011.04151.x. [DOI] [PubMed] [Google Scholar]
- 6.Akamatsu H., Koseki M., Nakaba H., et al. Giant adrenal myelolipoma: report of a case. Surgery Today. 2004;34(3):283–285. doi: 10.1007/s00595-003-2682-4. [DOI] [PubMed] [Google Scholar]
- 7.Boudreaux D., Waisman J., Skinner D. G., Low R. Giant adrenal myelolipoma and testicular interstitial cell tumor in a man with congenital 21-hydroxylase deficiency. The American Journal of Surgical Pathology. 1979;3(2):109–123. doi: 10.1097/00000478-197904000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Collins D. C. Formation of bone marrow in the suprarenal gland. The American Journal of Pathology. 1932;8(1):97–106.1. [PMC free article] [PubMed] [Google Scholar]
- 9.Plaut A. Myelolipoma in the adrenal cortex; myeloadipose structures. The American Journal of Pathology. 1958;34(3):487–515. [PMC free article] [PubMed] [Google Scholar]
- 10.Rubin H. B., Hirose F., Benfield J. R. Myelolipoma of the adrenal gland: angiographic findings and review of the literature. The American Journal of Surgery. 1975;130(3):354–358. doi: 10.1016/0002-9610(75)90401-8. [DOI] [PubMed] [Google Scholar]
- 11.Lam K. Y., Lo C. Y. Adrenal lipomatous tumours: a 30 year clinicopathological experience at a single institution. Journal of Clinical Pathology. 2001;54(9):707–712. doi: 10.1136/jcp.54.9.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meyer A., Behrend M. Presentation and therapy of myelolipoma. International Journal of Urology. 2005;12(3):239–243. doi: 10.1111/j.1442-2042.2005.01034.x. [DOI] [PubMed] [Google Scholar]
- 13.Enzinger F. M., Sharen W. W. Benign lipomatous tumors. In: Enzinger F. M., Sharen W. W., editors. Soft Tissue Tumors. 3rd. St Louis: Mosby; 1995. pp. 409–410. [Google Scholar]
- 14.Meaglia J. P., Schmidt J. D. Natural history of an adrenal myelolipoma. The Journal of Urology. 1992;147(4):1089–1090. doi: 10.1016/S0022-5347(17)37482-7. [DOI] [PubMed] [Google Scholar]
- 15.Iorio B., Gravante G., Pietrasanta D., et al. Description of a case of giant adrenal myelolipoma and survey of the literature. Minerva Chirurgica. 2003;58(4):595–600. [PubMed] [Google Scholar]
- 16.Lawler L. P., Pickhardt P. J. Giant adrenal myelolipoma presenting with spontaneous hemorrhage. CT, MR and pathology correlation. Irish Medical Journal. 2001;94(8):231–233. [PubMed] [Google Scholar]
- 17.Kenney P. J., Wagner B. J., Rao P., Heffess C. S. Myelolipoma: CT and pathologic features. Radiology. 1998;208(1):87–95. doi: 10.1148/radiology.208.1.9646797. [DOI] [PubMed] [Google Scholar]
- 18.Wani N. A., Kosar T., Rawa I. A., Qayum A. Giant adrenal myelolipoma: incidentaloma with a rare incidental association. Urology Annals. 2010;2(3):130–133. doi: 10.4103/0974-7796.68865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cyran K. M., Kenney P. J., Memel D. S., Yacoub I. Adrenal myelolipoma. AJR. American Journal of Roentgenology. 1996;166(2):395–400. doi: 10.2214/ajr.166.2.8553954. [DOI] [PubMed] [Google Scholar]
- 20.Tyritzis S. I., Adamakis I., Migdalis V., Vlachodimitropoulos D., Constantinides C. A. Giant adrenal myelolipoma, a rare urological issue with increasing incidence: a case report. Cases Journal. 2009;2(1):p. 8863. doi: 10.4076/1757-1626-2-8863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilhelmus J. L., Schrodt G. R., Alberhasky M. T., Alcorn M. O. Giant adrenal myelolipoma: case report and review of the literature. Archives of Pathology & Laboratory Medicine. 1981;105(10):532–535. [PubMed] [Google Scholar]
- 22.Mukherjee S., Pericleous S., Hutchins R. R., Freedman P. S. Asymptomatic giant adrenal myelolipoma. Urology Journal. 2010;7(1):66–68. [PubMed] [Google Scholar]
- 23.Kumar S., Jayant K., Prasad S., et al. Rare adrenal gland emergencies: a case series of giant myelolipoma presenting with massive hemorrhage and abscess. Nephro-Urology Monthly. 2015;7(1, article e22671) doi: 10.5812/numonthly.22671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brogna A., Scalisi G., Ferrara R., Bucceri A. M. Giant secreting adrenal myelolipoma in a man: a case report. Journal of Medical Case Reports. 2011;5(1, article 298) doi: 10.1186/1752-1947-5-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.O’Daniel-Pierce M. E., Weeks J. A., Mcgrath P. C. Giant adrenal myelolipoma. Southern Medical Journal. 1996;89(11):1116–1118. doi: 10.1097/00007611-199611000-00022. [DOI] [PubMed] [Google Scholar]
- 26.Reshi R., Bhat M. L., Kadri S. M., et al. Giant myelolipoma of the adrenal gland with adenocarcinoma of the colon: a rare surgico-pathological presentation. Laboratory Medicine. 2007;38(8):491–492. doi: 10.1309/CB9AGFWNDMBJ4QV9. [DOI] [Google Scholar]
- 27.Gautam S. C., Raafat H., Sriganesh S., et al. Giant adrenal myelolipoma. Qatar Medical Journal. 2013;2013(1):2–11. doi: 10.5339/qmj.2013.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tanaka D., Oyama T., Niwatsukino H., Nakajo M. A case of asymptomatic giant myelolipoma of the adrenal gland. Radiation Medicine. 1998;16(3):213–216. [PubMed] [Google Scholar]
- 29.Dell'Avanzato R., Castaldi F., Giovannini C., Mercadante E., Cianciulli P., Carlini M. Giant symptomatic myelolipoma of the right adrenal gland: a case report. Chirurgia Italiana. 2009;61(2):231–236. [PubMed] [Google Scholar]
- 30.Saha M., Dasgupta S., Chakrabarti S., Chakraborty J. Giant myelolipoma of left adrenal gland simulating a retroperitoneal sarcoma. International Journal of Advanced Medical and Health Research. 2015;2(2):p. 122. doi: 10.4103/2349-4220.172896. [DOI] [Google Scholar]
- 31.Gupta K., Kalra N., Das R., Kumaresan K. A rare association of giant adrenal myelolipoma in a young female double heterozygous for HbD Punjab and β-thalassemia trait. Indian Journal of Pathology and Microbiology. 2011;54(3):p. 635. doi: 10.4103/0377-4929.85126. [DOI] [PubMed] [Google Scholar]
- 32.Gerson G., Bêco M. P. F. G., Hirth C. G., et al. Giant retroperitoneal myelolipoma: case report and literature review. Jornal Brasileiro de Patologia e Medicina Laboratorial. 2015;51(1) doi: 10.5935/1676-2444.20150010. [DOI] [Google Scholar]
- 33.Takahashi H., Yamaguchi T., Takeda R., Sakata S., Yamamoto M. A case of giant adrenal myelolipoma. Nihon Rinsho Geka Gakkai Zasshi (Journal of Japan Surgical Association) 2005;66(1):197–201. doi: 10.3919/jjsa.66.197. [DOI] [Google Scholar]
- 34.Fernandes G. C., Gupta R. K., Kandalkar B. M. Giant adrenal myelolipoma. Indian Journal of Pathology & Microbiology. 2010;53(2):325–326. doi: 10.4103/0377-4929.64314. [DOI] [PubMed] [Google Scholar]
- 35.Chand G. Giant adrenal myelolipoma presenting as an incidentaloma: a case report and review of literature. Journal of Investigative Genomics. 2017;4(2) doi: 10.15406/jig.2017.04.00061. [DOI] [Google Scholar]
- 36.Répássy D. L., Csata S., Sterlik G., Iványi A. Giant adrenal myelolipoma. Pathology Oncology Research. 2001;7(1):72–73. doi: 10.1007/BF03032610. [DOI] [PubMed] [Google Scholar]
- 37.Anderson B. B., Hampton L. J., Johnson C. M., Guruli G. E. Symptomatic giant adrenal myelolipoma. World Journal of Endocrine Surgery. 2010;2(3):143–144. doi: 10.5005/jp-journals-10002-1040. [DOI] [Google Scholar]
- 38.Goldman H. B., Howard R. C., Patterson A. L. Spontaneous retroperitoneal hemorrhage from a giant adrenal myelolipoma. The Journal of Urology. 1996;155(2):p. 639. doi: 10.1016/S0022-5347(01)66474-7. [DOI] [PubMed] [Google Scholar]
- 39.Ersoy E., Ozdoğan M., Demirağ A., et al. Giant adrenal myelolipoma associated with small bowel leiomyosarcoma: a case report. The Turkish Journal of Gastroenterology. 2006;17(2):126–129. [PubMed] [Google Scholar]
- 40.Chakrabarti I., Ghosh N., Das V. Giant adrenal myelolipoma with hemorrhage masquerading as retroperitoneal sarcoma. Journal of Mid-life Health. 2012;3(1):42–44. doi: 10.4103/0976-7800.98818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McGeoch S. C., Olson S., Krukowski Z. H., Bevan J. S. Giant bilateral myelolipomas in a man with congenital adrenal hyperplasia. The Journal of Clinical Endocrinology & Metabolism. 2012;97(2):343–344. doi: 10.1210/jc.2011-2373. [DOI] [PubMed] [Google Scholar]
- 42.Kale G., Pelley E. M., Davis D. B. Giant myelolipomas and inadvertent bilateral adrenalectomy in classic congenital adrenal hyperplasia. Endocrinology, Diabetes & Metabolism Case Reports. 2015;2015, article 150079 doi: 10.1530/EDM-15-0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alvarez J. F., Goldstein L., Samreen N., et al. Giant adrenal myelolipoma. Journal of Gastrointestinal Surgery. 2014;18(9):1716–1718. doi: 10.1007/s11605-014-2553-x. [DOI] [PubMed] [Google Scholar]
- 44.al-Bahri S., Tariq A., Lowentritt B., Nasrallah D. V. Giant bilateral adrenal myelolipoma with congenital adrenal hyperplasia. Case Reports in Surgery. 2014;2014:5. doi: 10.1155/2014/728198.728198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.German-Mena E., Zibari G. B., Levine S. N. Adrenal myelolipomas in patients with congenital adrenal hyperplasia: review of the literature and a case report. Endocrine Practice. 2011;17(3):441–447. doi: 10.4158/EP10340.RA. [DOI] [PubMed] [Google Scholar]


