Abstract
Purpose
To make a comparative evaluation, by means of the finite element method, of the stress generated on supporting tissues and prosthetic system components, using zygomatic implants with the exteriorized and extramaxillary techniques, and different placement positions, associated either with inclined anterior implants, or those without inclination.
Materials and methods
Eight (8) tridimensional models were created to represent the clinical situations being researched, using the dataset of scanned images of an edentulous model. The implants and prosthetic components were photographed on millimeter paper and inserted into Rhinoceros 3D modeling computer software. From the measurements made on the image, the virtual models were made. The application force was distributed on the occlusal surface of the working side of the left maxillary first molar, first and second premolars, and incisal regions of the central incisor, simulating the occlusal load during mastication, in a total of 150 N.
Results
The extramaxillary technique presented considerable variation in increased tension on the prosthesis screws and bone tissue. In the exteriorized technique, the highest tension values occurred in the region of the ridge, and the lowest, on the zygomatic process; the absence of cantilever reduced the stress on bone tissue in almost all regions.
Conclusion
The exteriorized technique was shown to be more favorable to the distribution of stresses on the micro-unit screws and bone tissue, with the model with zygomatic implant placed in the region of the first molar and inclined anterior implant presenting the best results.
Keywords: Zygomatic implants, Atrophic maxilla, Finite element analysis, Cantilever, Inclined implant
Highlights
-
•
The extramaxillary technique showed considerable variation in stress increase.
-
•
In the exteriorized technique, the highest stress occurred in the alveolar ridge region.
-
•
The alveolar bone support for zygomatic implants reduced the internal stress generated by the vertical force.
1. Introduction
In implant dentistry, the major challenge is to rehabilitate individuals with loss of bone support, especially in the maxillary arch, due to the natural physiological process that occurs after tooth loss. Remarkable changes will occur in the height and width of the alveolar ridge after the extraction of one or several teeth [1]. For rehabilitating these areas, one of the options is to use bone grafts, either with autogenous, homogenous, heterogenous, or alloplastic bone and growth factors [2,3].
The technique of using zygomatic implants has also been as a possibility for the more rapid treatment of atrophic areas, with less morbidity when compared with the use of bone grafts [4]. When well indicated, zygomatic implants have a high success rate [[5], [6], [7]], and immediate loading may be used, optimizing the final time for delivery of the dental prosthesis and presenting a high level of patient satisfaction [[8], [9], [10]].
Four types of zygomatic implant placement techniques have been described, with the most up-to-date being the exteriorized and extramaxillary types [11]. The advantages of these two types are that the zygomatic implants, differently form the other techniques, are placed external to the maxillary sinus, prevent possible conditions of sinusitis, the main complication in this type of therapy [6].
Inclined implants are also indicated for the treatment of atrophic maxillae. In the surgical technique denominated M − 4 only 4 inclined conventional implants are used, and it is possible to rehabilitate individuals without the need for grafts in the maxilla [12].
Atrophic maxillary rehabilitation with zygomatic implants requires the combination of a minimum of 4 implants; 2 may be straight, conventional implants and 2, unilateral zygomatic implants; or 2 zygomatic implants on each side. Selecting the approach will depend on the degree of bone resorption of the maxilla. In daily clinical practice, this resorption may have occurred to such an extent that in some cases, inclination of the anterior implants may be combined with the apex directed 30° towards the lateral paranasal bone of the pyriform aperture [13], with placement of posterior zygomatic implants, which is a technique that has not yet been evaluated.
Thus, the aim of this study was to verify, by means of the Finite Element Method, which type of surgical approach could provide better distribution of the stresses and implant stability in the maxilla, and on the zygomatic bone; and compare the exteriorized technique with the extramaxillary type, associated with inclination of the conventional anterior implants.
2. Materials and methods
In the posterior region, was used internal hexagon zygomatic implant of 4.0 × 42.5 mm (Titanium Cortical Screw Master Zigomax 4.0 × 42.5 mm - Conexão Sistemas de Prótese Ltda, São Paulo, Brazil).
In the anterior region, a morse cone implant 3,5 × 10 mm was used (Flash HI Porous NP 3.5 × 10 mm - Conexão Sistema de Prótese Ltda, São Paulo, Brazil).
With the aid of a universal analog pachymeter with 0.05 mm precision (Mitutoyo, São Paulo, Brazil), the implant measurements were obtained. The implants were photographed on millimeter paper, and by means of the Rhinoceros 3D modeling computer software (Robert MCNell & Associados, USA, Seattle, WA), the virtual models were created.
The same steps were used for fabricating the prosthetic components.
For the straight anterior implants, straight micro-unit abutments with 2.5 mm collar; and for the inclined implants, micro-unit abutments angled at 17° with 3.5 mm collar (Conexão Sistema de Prótese Ltda, São Paulo, Brazil) were used. For the zygomatic implants, micro-unit abutments angled at 30° with 3 mm collar (Conexão Sistema de Prótese Ltda, São Paulo, Brazil) were used.
For an assembly with the correct relations of the components on the implants, wear on the implant was performed with a mandril disc, and the relationship of the position between the parts within the implants was studied (Fig. 1).
Fig. 1.
A: Straight micro-unit abutment with 2.5 mm collar, screw-retained on morse cone implant, B: Micro-unit abutment angled at 30° with 3 mm collar, screw-retained on zygomatic implant.
To make the virtual model of the maxilla, an edentulous model of the middle third of the face with bilaterally pneumatized maxillary sinuses was used, obtained by means of prototyping (Nacional Ossos, São Paulo, Brazil). This was scanned with a 3D laser scanner (Nextengine HD, Santa Monica, USA).
The models were saved in STL (Stereolithography, 3D Systems, Rock Hill, USA) format, for later processing. The use of 3D scanners for obtaining geometric models in Dentistry has previously been documented [[14], [15], [16], [17]].
After this, the images were imported into the Solidworks 2014 software (Dassault Systems, Solidworks Corps, USA), for editing and preparing the virtual models.
The 3D scanner software reconstructed the model with a network of polygonal surfaces. These polygons were exclusively triangular and flat, and to define a model with adequate precision, dozens or hundreds of thousands of polygons are sometimes necessary. However, the majority of CAD type software programs for editing models, such as Solidworks, do not accept the importation of hundreds of thousands of surfaces. Simply diminishing the number of polygons would result in great distortion of the model. To resolve this problem, an importation supplement of Solidworks called “Scanto 3D” was used. With this, it was possible to transform the polygons into surfaces of the NURBS (Non Uniform Rational Basis Splines) type, for generating solid models, so that these surfaces had the capacity to be curves and register geometrical details on the face itself, thus allowing drastic reduction in the number of surfaces necessary, without compromising the precision of the model.
Eight (8) model were created to represent the clinical situations to be researched. Table 1 describes the zygomatic implants in position; technique used, and the morse cone implants with inclination. Table 2 indicates the properties used of each component of the models.
Table 1.
Models with the position of the zygomatic implants and the technique used, and angulation of implants.
| Model | Anterior Region |
Posterior Region |
|||||
|---|---|---|---|---|---|---|---|
| Implant | Region | Abutment | Implant | Technique | Region | Abutment | |
| 1 | 3.5 × 10 (Straight) |
12 and 22 | Microunit 2.5 |
Zygomatic | Exteriorized | 14 and 24 | Microunit 30° × 3 |
| 2 | 3.5 × 10 (Straight) |
12 and 22 | Microunit 2.5 |
Zygomatic | Exteriorized | 16 and 26 | Microunit 30° × 3 |
| 3 | 3.5 × 10 (Angled) |
12 and 22 | Microunit 17° × 3.5 |
Zygomatic | Exteriorized | 14 and 24 | Microunit 30° × 3 |
| 4 | 3.5 × 10 (Angled) |
12 and 22 | Microunit 17° × 3.5 |
Zygomatic | Exteriorized | 16 and 26 | Microunit 30° × 3 |
| 5 | 3.5 × 10 (Straight) |
12 and 22 | Microunit 2.5 |
Zygomatic | Extramaxillary | 14 and 24 | Microunit 30° × 3 |
| 6 | 3.5 × 10 (Straight) |
12 and 22 | Microunit 2.5 |
Zygomatic | Extramaxillary | 16 and 26 | Microunit 30° × 3 |
| 7 | 3.5 × 10 (Angled) |
12 and 22 | Microunit 17° × 3.5 |
Zygomatic | Extramaxillary | 14 and 24 | Microunit 30° × 3 |
| 8 | 3.5 × 10 (Angled) |
12 and 22 | Microunit 17° × 3.5 |
Zygomatic | Extramaxillary | 16 and 26 | Microunit 30° × 3 |
Table 2.
Properties of materials used in the models.
| Structure | Modulus of Elasticity (MPa) | Poisson | References |
|---|---|---|---|
| Infrastructure (Ni-Cr) | 203000 | 0.30 | Suansuwan (2001) [18] |
| Implant (Ti cp IV) | 110000 | 0.33 | Matweb |
| Screw (Ti6Al4V) | 105000 | 0.36 | Neodent |
| Mini-abutment (Ti6Al4V) | 105000 | 0.36 | Neodent |
| Cortical bone | 13400 | 0.30 | Carter & Hayes (1977) [19] |
| Cancellous bone | 1370 | 0.31 | Carter & Hayes (1977) [19] |
| Resin | 21000 | 0.24 |
The quality of the mesh and consequently the number of elements has a great influence on the result. In this sense, a large quantity of elements was used in order to seek a well refined mesh. Moreover, to minimize possible numerical errors, a similar mesh was used in the 8 models. The mean number of nodes in each model was 10, 605, 420 and the mean number of elements, 7,612,999. The same could be said of the loading and displacement conditions. Table 3 indicates the quantity of nodes and elements in each model.
Table 3.
Quantity of nodes and elements in each model.
| Model | M1 | M2 | M3 | M4 | M5 | M6 | M7 | M8 |
|---|---|---|---|---|---|---|---|---|
| Nodes | 10607699 | 10602899 | 10604637 | 10605784 | 10601897 | 10606933 | 10605311 | 10608201 |
| Elements | 7614943 | 7610589 | 7612879 | 7613129 | 7610425 | 7613899 | 7612237 | 7615892 |
After discretization into finite elements, the contour conditions were inserted (restriction of movement and occlusal load).
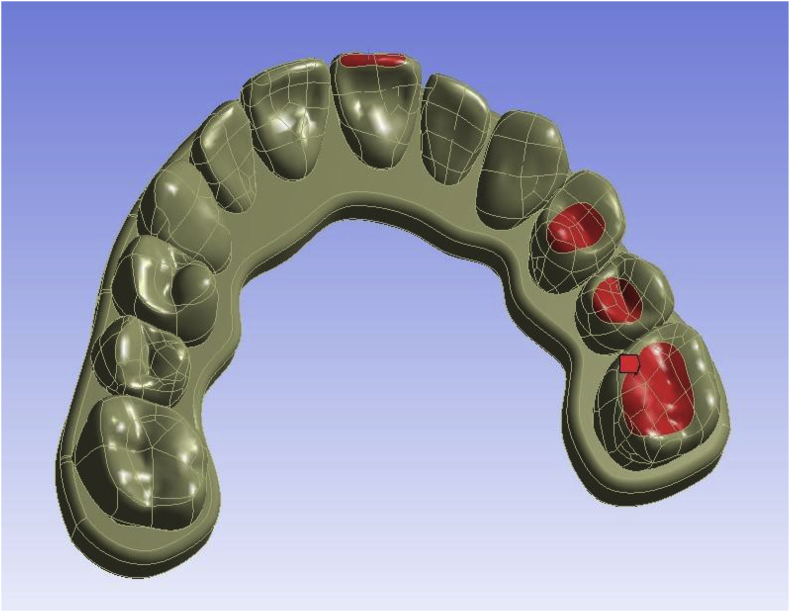
Fig. 2 illustrates the restrictions of movements on the bone ridge of the model. The application force was distributed on the occlusal surface of the working side of the left maxillary first molar, left first premolar, left and second premolar and incisal regions of the central incisor, simulating the occlusal load during mastication, in a total of 150 N (Fig. 3).
Fig. 2.
Restrictions of movements on the bone ridge of the model (in blue). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 3.
Occlusal load on the occlusal surface of teeth 26, 25, 24 and on incisal surface of 21 (in red). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
The simplifications adopted in this study were: plane state of stress, behavior of material considered linearly elastic, isotropic, loading distributed on surface of dental prosthesis/crown and restriction of displacement at the base of the cortical bone in directions x, y and z.
For pre-processing, processing and readout of results, the software Ansys (Ansys Inc, USA, Canonsburg, PA) was used. For stress distribution analysis, the Von Mises criterion of equivalent stresses was used.
3. Results
3.1. Von Mises analysis of stress on screws
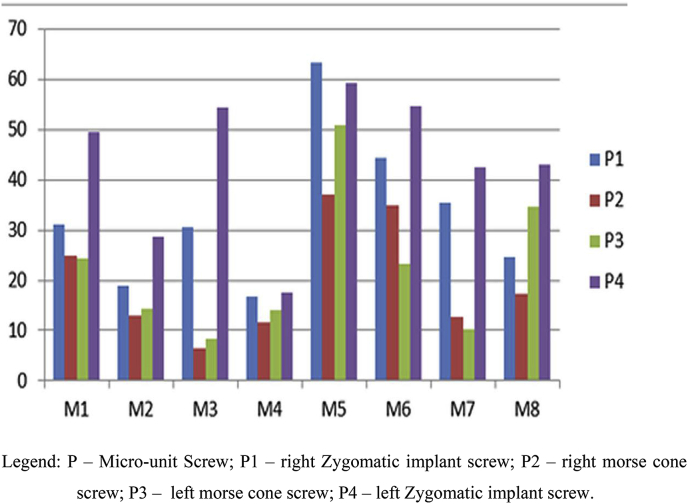
Table 4 and Fig. 4 demonstrate the values of stress on fixation mini-screws of dental prostheses in the different models. M5 was observed to present the highest stress on the screws, and M4 presented the lowest stress.
Table 4.
Von Mises stress generated in the screws (values in megapascals [MPa]).
| Model | P1 | P2 | P3 | P4 |
|---|---|---|---|---|
| M1 | 31.167 | 25.022 | 24.449 | 49.543 |
| M2 | 19.067 | 12.947 | 14.256 | 28.72 |
| M3 | 30.681 | 6.3498 | 8.4646 | 54.37 |
| M4 | 16.648 | 11.531 | 14.085 | 17.549 |
| M5 | 63.451 | 37.132 | 50.777 | 59.198 |
| M6 | 44.48 | 34.905 | 23.172 | 54.639 |
| M7 | 35.514 | 12.751 | 10.355 | 42.604 |
| M8 | 24.628 | 17.343 | 34.703 | 43.167 |
Legend: P – Micro-unit Screw; P1 – right Zygomatic implant screw; P2 – right morse cone screw; P3 – left morse cone screw; P4 – left Zygomatic implant screw.
Fig. 4.
Von Mises Stresses generated on the screws (Values in MPa - Mega Pascal).
3.2. Von Mises analysis of stress on bone tissue
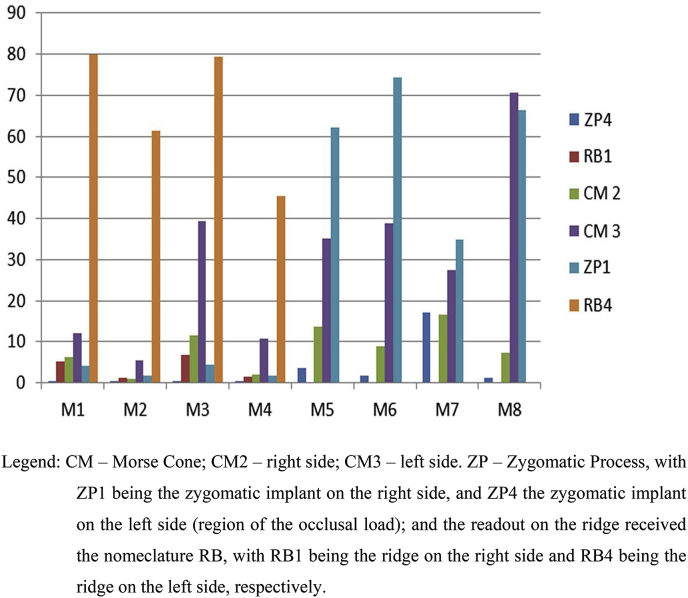
Table 5 and Fig. 5 demonstrate the values of stress on bone tissue in the different models. Readout of the stresses that occurred on the zygomatic process and bone ridge in Models M1, M2, M3 e M4 (exteriorized technique for zygomatic positioning) and only in the zygomatic process of models M5, M6, M7 and M8 (extramaxillary technique for zygomatic positioning), because, in this second technique there is no bone at the head of the implant in the region of the ridge. For analysis of this graph, in general, there was greater stress on the occlusal side, with concentration in the region of the ridge in models M1, M2, M3 and M4; and higher concentration on the zygomatic process in models M5, M6, M7 and M8.
Table 5.
Values of stresses on bone tissues in the differents models (values in megapascals [MPa]).
| ZYGOMATIC 1 |
CM 2 |
CM 3 |
ZYGOMATIC 4 |
|||
|---|---|---|---|---|---|---|
| ZP1 | RB1 | CM2 | CM3 | ZP4 | RB4 | |
| M1 | 0.22338 | 5.1107 | 6.2446 | 12.002 | 4.2004 | 79.864 |
| M2 | 0.07247 | 1.1735 | 1.0367 | 5.577 | 1.8061 | 61.316 |
| M3 | 0.26582 | 6.6994 | 11.62 | 39.433 | 4.2953 | 79.45 |
| M4 | 0.09099 | 1.516 | 2.1025 | 10.709 | 1.7316 | 45.489 |
| M5 | 3.6124 | 13.606 | 35.252 | 62.245 | ||
| M6 | 1.6541 | 8.8062 | 38.809 | 74.39 | ||
| M7 | 17.092 | 16.488 | 27.539 | 34.808 | ||
| M8 | 1.2066 | 7.4078 | 70.695 | 66.4 | ||
Legend: CM – Morse Cone; CM2 – right side; CM3 – left side. ZP – Zygomatic Process, with ZP1 being the zygomatic implant on the right side, and ZP4 the zygomatic implant on the left side (region of the occlusal load); and the readout on the ridge received the nomenclature RB, with RB1 being the ridge on the right side and RB4 being the ridge on the left side, respectively.
Fig. 5.
Values of stresses on bone tissues in the different models (Values in MPa - Mega Pascal).
3.3. Von Mises analysis of stress on zygomatic implants
Table 6 describes the Von Mises stresses generated on the zygomatic implants. It may be observed that M2 and M4 (exteriorized technique without cantilever) and M7 (extramaxillary technique with cantilever) received the lowest stress values on the left zygomatic (side of occlusal load).
Table 6.
Von Mises Stresses generated in the zygomatic implants (Values in MPa - Mega Pascal).
| M1 | M2 | M3 | M4 | M5 | M6 | M7 | M8 | |
|---|---|---|---|---|---|---|---|---|
| ZYGO E | 410.68 | 140.23 | 417.62 | 147.51 | 537.96 | 399.05 | 288.16 | 356.7 |
| ZYGO D | 23.085 | 3.6706 | 28.335 | 3.8387 | 33.335 | 17.232 | 112.16 | 14.146 |
Legend: ZYGO E = zygomatic implant on the side of the load; ZYGO D = zygomatic implant on the opposite side of the load.
4. Discussion
The lowest stress values on the bone tissue with the micro-unit screws were found in the exteriorized technique. Whereas, the extramaxillary technique presented the highest stress values. The lack of bone support in the coronal portion of the implant for resisting the loads in the vestibular direction was different from the pattern of displacement in the exteriorized approach, in which the head of the implant is highly restricted by the alveolar bone in the vestibular-lingual and mesio-distal directions, which in compatible with the highest peaks of stress found in the extramaxillary technique in this research. A similar situation was found in a research in which the intrasinus technique was compared with the extramaxillary technique [20]. In another study, when the original, exteriorized and extramaxillary techniques were compare, the lowest deformations of bone around the zygomatic dental implants were observed in the exteriorized technique and group with the original technique [11].
The stress on the maxillary bone that surrounded the zygomatic implants was much higher than that on the bone that surrounded dental implants, however, below the values of static force of the bone, which was approximately 150 MPa in stress and 250 MPa in compression [11]. Rehabilitation of atrophic maxillae with zygomatic and conventional implants must not involve risk of overloading the surrounding bone. In this technique, Model M4 presented the best stress distribution results. The feature observed in this model was that inclination of the anterior implant with the zygomatic implant placed in the region of the first molar favored the low Von Mises stress values found, showing that the inclination of anterior implants was beneficial only in the absence of the cantilever [20]. What occurred was that the maximum stress inducted by the more posterior loading without the presence of cantilever was initially transferred to the alveolar bone, and then dispersed by the zygomatic implant. Inclination of the anterior implants in this situation allowed greater stress dispersion, considering that if they had been straight, they would have had limited space for dispersing the stress in the region of the anterior nasal spine [21]. The cantilever effect is one of the questions that cannot be compromised in implant-supported fixed dental prostheses, which led to model M4 presenting the best results in stress distribution on the micro-unit screws and bone tissue. One author reported that the increase in stress on implants was proportional to the increase in length of the cantilever [20]. A similar result was found in a study that compared 3 zygomatic implant placement techniques, however, with the use of straight anterior implants, and concluded that to minimize the stress on the zygomatic implant structures, and when the stress and deformation of the bones that surrounded the zygomatic implants were considered, the best model was the one that had 2 straight anterior implants in the lateral incisor region, and one zygomatic implant on each side positioned in the first molar region, in the exteriorized technique. Thus, the exteriorized technique could increase the long term success rate of zygomatic implants, from the biomechanical point of view [11].
In this research, the authors observed that the lack of bone tissue at the head of the zygomatic implant resulted in the highest peaks of stress on the zygomatic implants ZI4, on the anterior implants and micro-unit screws, as well as on the zygomatic process, in the extramaxillary technique. This was in agreement with the findings of a study in which the authors concluded alveolar bone support for zygomatic implants reduced the internal stresses generated by the occlusal and lateral forces, when compared with implants not supported by alveolar bone [22].
However, zygomatic bone offers predictable anchorage for fixed dental prostheses in patients who have a severely resorbed maxilla [23], favoring the receipt and displacement of stress, in addition to emergence of the implant head being more prosthetically correct in the extramaxillary technique [20,24]. The highest value of stress on the zygomatic implant in this research was found in the extramaxillary technique, in Model M5, on the implant that received the vertical load, with a value of 537. 96 MPa, however, below the 900 N/mm2 tolerated by Titanium alloys [11]. A similar situation was found for the head of the most distal zygomatic implant in the model without alveolar support, in a recent research [22]. Differently from the exteriorized technique, in this study the authors observed that the highest stress values occurred on the zygomatic process ZP4 and micro-unit screws P4, in models M5, M6, M7 and M8. Inclination of anterior implants was shown to be more favorable for stress received on the micro-unit screws in models M7 and M8, generating fewer stresses on the anterior screws of model M7. Whereas, relative to stress on bone tissue, model M7 presented the best result, showing that implant inclination diminished the stress on bone tissue only in the presence of a cantilever.
As there is no bone tissue at the head of the zygomatic implant to receive the vertical occlusal load, approximation of the anterior implant to the posterior zygomatic implant generated less stress on the system, whereas the greater antero-posterior distance between the anterior implant and the posterior zygomatic implant increased the values of stress on bone tissue, as shown in Models M6 and M8. Different results were found in a study in which the authors suggested that the cantilever effect contributed to increasing the stress distribution and displacement in the extramaxillary approach, which could be reduced by the use of a support system that uses a short implant and ball type abutment as additional retention for the distal extension of the dental prosthesis cantilever [20]. In another research, the authors also reported that in the extramaxillary technique, the length of the distal cantilever was almost 2× longer than it was in the intrasinus technique [25]. Another author related that with the use of the extramaxillary technique, not only was there less contact of bone tissue with the zygomatic implant in comparison with the Branemark and exteriorized techniques, but there was a long cantilever, which was a risk factor for failure [11].
Bearing in mind the results found in this research, the authors supposed that it would be ideal, whenever bone anatomy allowed this, to use the exteriorized technique, because it presented less stress on the systems studied in this research. Considering that over the years, bone support would be lost at the head of the zygomatic implant BR4 that received the vertical load, the stress would be transmitted to the zygomatic bone ZP4, providing these implants with a longer time of life, and consequently for the prosthetic rehabilitation as well. In a systematic review, after 36 months of follow-up, the successful survival rate of zygomatic implants was 97.86%, showing that this treatment was feasible, and must form part of the implant dentists' treatment options for rehabilitating patients with severely resorbed maxillae [7], in addition to promoting their quality of life [26].
5. Conclusion
The authors concluded that the exteriorized technique was shown to be more favorable to stress distribution on the micro-screws and bone tissues. The model with inclined anterior implants associated with the zygomatic implant in the molar regions in the exteriorized technique presented lower tension values for the screws and bone tissues. Alveolar bone support for zygomatic implants reduced the internal stresses generated by vertical force when compared with implants not supported by alveolar bone. Inclination of the anterior implant was shown to be more favorable without the presence of the cantilever in the exteriorized technique, and with the presence of cantilever in the extramaxillary technique.
Ethical approval
Waived to be submitted to analysis, being exclusively laboratory research, without involving patients or materials.
Research Ethics Committee (REC) of the São Leopoldo Mandic Dental School, protocol number 2014/0272.
Funding
None.
Author contribution
Study design: Paulo H. T. Almeida, Fabiana M. G. França. Data collection: Paulo H. T. Almeida. Data analysis: Paulo H. T. Almeida, Fabiana M. G. França. Manuscript preparation: Paulo H. T. Almeida. Critical revision: Paulo H. T. Almeida, Sergio H. Cacciacane, Fabiana M. G. França.
Conflicts of interest
None declared.
Research registration unique identifying number (UIN)
Research registry 3640.
Guarantor
Paulo Henrique Teles de Almeida.
References
- 1.Araújo M.G., Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J. Clin. Periodontol. 2005 Feb;32(2):212–218. doi: 10.1111/j.1600-051X.2005.00642.x. [DOI] [PubMed] [Google Scholar]
- 2.Vidote R.M., Guastaldi F.P.S., Klüppel L.E., Spagnoli D.B., Mazzonetto R. Uso da proteína morfogenética óssea recombinante humana-2 em levantamento de assoalho de seio maxilar. Implant News. 2009;6(1):27–31. [Google Scholar]
- 3.Costa A.L.C.C., Ramos Neto A.S., Neves D.M., Silva F.G.O., Simão G.M.L. Características dos agregados plaquetários e indicações da L-PRF na cirurgia oral. Implant News. 2012;9(4):519–526. [Google Scholar]
- 4.Ferreira E.J., Kuabara M.R., Gulinelli J.L. All-on-four" concept and immediate loading for simultaneous rehabilitation of the atrophic maxilla and mandible with conventional and zygomatic implants. Br. J. Oral Maxillofac. Surg. 2010 Apr;48(3):218–220. doi: 10.1016/j.bjoms.2009.08.017. [DOI] [PubMed] [Google Scholar]
- 5.Bedrossian E. Rehabilitation of the edentulous maxilla with the zygoma concept: a 7-year prospective study. Int. J. Oral Maxillofac. Implants. 2010 Nov-Dec;25(6):1213–1221. [PubMed] [Google Scholar]
- 6.Candel-Martí E., Carrillo-García C., Peñarrocha-Oltra D., Peñarrocha-Diago M. Rehabilitation of atrophic posterior maxilla with zygomatic implants: review. J. Oral Implantol. 2012 Oct;38(5):653–657. doi: 10.1563/AAID-JOI-D-10-00126. [DOI] [PubMed] [Google Scholar]
- 7.Goiato M.C., Pellizzer E.P., Moreno A., Gennari-Filho H., dos Santos D.M., Santiago J.F. Implants in the zygomatic bone for maxillary prosthetic rehabilitation: a systematic review. Int. J. Oral Maxillofac. Surg. 2014 Jun;43(6):748–757. doi: 10.1016/j.ijom.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 8.Bedrossian E., Rangert B., Stumpel L., Indresano T. Immediate function with the zygomatic implant: a graftless solution for the patient with mild to advanced atrophy of the maxilla. Int. J. Oral Maxillofac. Implants. 2006 Nov-Dec;21(6):937–942. [PubMed] [Google Scholar]
- 9.Davo R., Malevez C., Rojas J. Immediate function in the atrophic maxilla using zygoma implants: a preliminary study. J. Prosthet. Dent. 2007 Jun;97(6 Suppl):S44–S51. doi: 10.1016/S0022-3913(07)60007-9. [DOI] [PubMed] [Google Scholar]
- 10.Sartori E.M., Padovan L.E., de Mattias Sartori I.A., Ribeiro P.D., Jr., Gomes de Souza Carvalho A.C. Evaluation of satisfaction of patients rehabilitated with zygomatic fixtures. J. Oral Maxillofac. Surg. 2012 Feb;70(2):314–319. doi: 10.1016/j.joms.2011.03.044. [DOI] [PubMed] [Google Scholar]
- 11.Wen H., Guo W., Liang R., Xiang L., Long G., Wang T., Deng M., Tian W. Finite elemento analysis of three zygomatic implant techniques for the severely atrophic edentulous maxilla. J. Prosthet. Dent. 2014 Mar;111(3):203–215. doi: 10.1016/j.prosdent.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 12.Jensen O.T., Adams M.W. The maxillary M-4: a technical and biomechanical note for all-on-4 management of severe maxillary atrophy–report of 3 cases. J. Oral Maxillofac. Surg. 2009 Aug;67(8):1739–1744. doi: 10.1016/j.joms.2009.03.067. [DOI] [PubMed] [Google Scholar]
- 13.Jensen O.T., Adams M.W., Smith E. Paranasal bone: the prime factor affecting the decision to use transsinus vs zygomatic implants for biomechanical support for immediate function in maxillary dental implant reconstruction. Int. J. Oral Maxillofac. Implants. 2014 Jan-Feb;29(1):e130–e138. doi: 10.11607/jomi.te52. [DOI] [PubMed] [Google Scholar]
- 14.Aoun M., Mesnard M., Monède-Hocquard L., Ramos A. Stress analysis of temporomandibular joint disc during maintained clenching using a viscohyperelastic finite element model. J. Oral Maxillofac. Surg. 2014 Jun;72(6):1070–1077. doi: 10.1016/j.joms.2013.11.031. [DOI] [PubMed] [Google Scholar]
- 15.Da Silveira A.C., Daw J.L., Jr., Kusnoto B., Evans C., Cohen M. Craniofacial applications of three-dimensional laser surface scanning. J. Craniofac. Surg. 2003 Jul;14(4):449–456. doi: 10.1097/00001665-200307000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Fuster-Torres M.A., Albalat-Estela S., Alcañiz-Raya M., Peñarrocha-Diago M. CAD/CAM dental systems in implant dentistry: update. Med. Oral Patol. Oral Cir. Bucal. 2009 Mar 1;14(3):E141–E145. [PubMed] [Google Scholar]
- 17.Wu T., Liao W., Dai N., Tang C. Design of a custom angled abutment for dental implants using computer-aided design and nonlinear finite element analysis. J. Biomech. 2010 Jul 20;43(10):1941–1946. doi: 10.1016/j.jbiomech.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 18.Suansuwan N., Swain M.V. Determination of elastic properties of metal alloys and dental porcelains. J. Oral Rehabil. 2001 Feb;28(2):133–139. doi: 10.1046/j.1365-2842.2001.00642.x. [DOI] [PubMed] [Google Scholar]
- 19.Carter D.R., Hayes W.C. The compressive behavior of bone as a two-phase porous structure. J Bone Joint Surg Am. 1977 Oct;59(7):954–962. [PubMed] [Google Scholar]
- 20.Ishak M.I., Kadir M.R., Sulaiman E., Kasim N.H. Finite element analysis of different surgical approaches in various occlusal loading locations for zygomatic implant placement for the treatment of atrofhic maxillae. Int. J. Oral Maxillofac. Surg. 2012;41:1077–1089. doi: 10.1016/j.ijom.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 21.Maló P., Rangert B., Nobre M. All-on-4 immediate-function concept with Branemark system implants for completely edentulous maxillae: a 1-year retrospective clinical study. Clin. Implant Dent. Relat. Res. 2005;7(1):88–94. doi: 10.1111/j.1708-8208.2005.tb00080.x. [DOI] [PubMed] [Google Scholar]
- 22.Freedman M., Ring M., Stassen L.F. Effect of alveolar bone support on zygomatic implants: a finite element analysis study. Int. J. Oral Maxillofac. Surg. 2013 May;42(5):671–676. doi: 10.1016/j.ijom.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 23.Fernández H., Delgado A., Saldarriaga S. Zygomatic implants for the management of the severely atrophied maxila: a retrospective analysis of 244 implants. J. Oral Maxillofac. Surg. 2014;72:887–891. doi: 10.1016/j.joms.2013.12.029. [DOI] [PubMed] [Google Scholar]
- 24.Aparicio C., Manresa C., Francisco K., Claros P., Alández J. Zygomatic implant: indications, techniques and outcomes, and the zygomatic success code. Periodontology. 2000;2014(66):41–58. doi: 10.1111/prd.12038. [DOI] [PubMed] [Google Scholar]
- 25.Ishak M.I., Kadir M.R., Sulaiman E., Kasim N.H. Finite element analysis of zygomatic implants in intrasinus and extramaxillary approaches for prosthetic rehabilitation in severely atrophic maxillae. Int. J. Oral Maxillofac. Implants. 2013 May-Jun;28(3):e151–e160. doi: 10.11607/jomi.2304. [DOI] [PubMed] [Google Scholar]
- 26.Almeida P.H.T., Salvoni A.D.A., França F.M.G. Evaluation of satisfaction of individuals rehabilitated with zygomatic implants as regards anesthetic and sedative procedure: a prospective cohort study. Ann Med Surg. (Lond) 2017;22:22–29. doi: 10.1016/j.amsu.2017.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]