Abstract
There is conflicting evidence as to whether repeat syphilis is more likely to present asymptomatically than initial syphilis. If it is, then this would motivate more frequent and long-term syphilis screening in persons with a history of multiple episodes of syphilis. We conducted detailed folder reviews of all individuals with 4 or more diagnoses of syphilis between 2000 and 2017 at the Institute of Tropical Medicine, Antwerp, and assessed if there was a difference in the proportion presenting with symptomatic (primary and secondary) vs asymptomatic (latent) syphilis in initial vs repeat syphilis. Forty-five clients with 4 or more episodes of syphilis were included in the study. All were HIV-infected. Repeat episodes of syphilis were less likely to be symptomatic than initial episodes (35/160 [21.9%] vs 28/45 [62.2%]; P < .001). Frequent screening in those with HIV infection may be the only way to diagnose repeat episodes of syphilis. Care providers can use this information to motivate persons with multiple episodes of syphilis to be screened every 3 to 6 months.
Keywords: HIV, immunity, MSM, repeat infection, screening, syphilis
Individuals with repeat syphilis are considered by some to be playing an increasingly important role in the epidemics of syphilis in Europe and elsewhere [1–3]. At our sexually transmitted infection (STI) clinic in Antwerp, Belgium, we have noted that close to half of all syphilis cases are repeat syphilis [3]. It is crucial to establish if cases of repeat syphilis are more likely to be asymptomatic than initial cases. If they are more likely to be asymptomatic, then the timely detection of these cases will depend on frequent serological screening.
Studies comparing the clinical findings in initial and repeat syphilis have reached different conclusions. Three studies found that persons with initial syphilis were more likely than those with repeat syphilis to present with symptomatic disease [4–6], whereas another 3 found no difference [1, 2, 7].
Given this uncertainty, we conducted a retrospective case review of all clients with 4 or more episodes of syphilis to assess if repeat syphilis patients were more likely to be asymptomatic.
METHODS
We conducted detailed folder reviews for all clients attending our HIV/STI clinic at the Institute of Tropical Medicine (ITM), Antwerp, Belgium, who had had 4 or more episodes of syphilis recorded between January 1, 2000, and July 30, 2017. We chose 4 episodes as this provided a sufficient number of episodes of syphilis while remaining a manageable number of folders to review. Patients in the HIV cohort are typically followed up at 6-monthly intervals and have their RPR and Treponema pallidum Particle Agglutination (TPA) tests assessed every 6 months [8]. The data extracted included demographics, HIV diagnosis, clinical stage of syphilis at the time of diagnosis, and therapy administered. An adequate response to syphilis therapy was defined as a ≥2-titer decrease in RPR and a disappearance of symptoms of syphilis. Stages of syphilis were determined by an infectious disease specialist according to US Centers for Disease Control and Prevention (CDC) surveillance definitions [9]. A repeat episode of syphilis (repeat syphilis) was defined as an episode of syphilis that met the CDC definition of syphilis, such as a 2-titer increase in RPR plus a positive TPA, or a positive T. pallidum polymerase chain reaction, that followed a previous episode of syphilis.
The chi-square test and chi-square test for trend were used to assess the associations between initial/repeat syphilis and symptomatic syphilis. Analyses were conducted in Stata 13.0 (StataCorp, College Station, TX). Ethical approval for this study was provided by the Institutional Review Board of the ITM.
RESULTS
Forty-five clients with 4 or more episodes of syphilis were included in the study. Twenty-two clients had 4 episodes, 16 had 5 episodes, 5 had 6 episodes, and 2 clients had 7 episodes of syphilis. The median age at first episode of syphilis (interquartile range [IQR]) was 44.4 (38.6–48) years. All clients were men who have sex with men (MSM), and all were HIV-infected. The diagnosis of HIV preceded the first diagnosis of syphilis in 41 individuals. They were commenced on antiretroviral therapy at various intervals following the diagnosis of HIV. The median CD4+ T-cell count at the time of the initial syphilis infection (IQR) was 416 (270–602) cells/uL. For 42/45 individuals, we had evidence of a negative TPPA test preceding their first episode of syphilis. Each episode of syphilis was followed by stage-appropriate therapy and an appropriate ≥2-titer reduction in RPR during post-treatment follow-up.
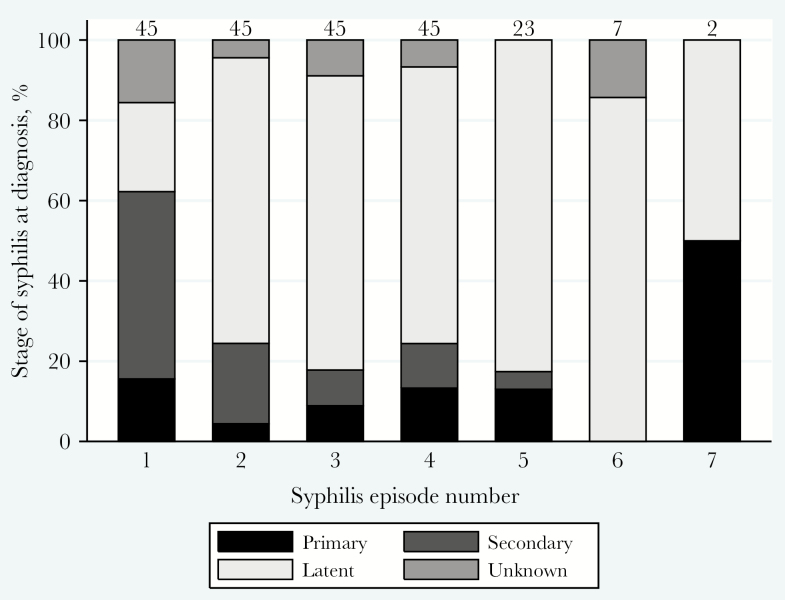
Repeat episodes of syphilis were less likely to be symptomatic than initial episodes (35/167 [21.0%] vs 28/45 [62.2%]; P < .001, chi-square test). The proportion of patients with symptomatic (primary and secondary) syphilis declined from 28/45 (62.2%) at initial syphilis to 11/45 (24.4%) [second episode], 8/45 (17.8%) [third episode], 11/45 (24.4%) [fourth episode], 4/23 (17.4%) [fifth episode], 0/7 (0%) [sixth episode], and 1/2 (50.0%) [seventh episode] (P < .001; chi-square test for trend) (Figure 1). Repeating the analyses without the episodes where the syphilis stage was unknown did not alter the results (data not shown). The breakdown of syphilis stage by number of episodes of syphilis is depicted in Figure 1.
Figure 1.
Percentage of clients presenting with primary, secondary, and latent syphilis by syphilis episode number in a group of 45 clients who had 4 or more diagnoses of syphilis between 2000 and 2017 at the STI clinic of the Institute of Tropical Medicine in Antwerp, Belgium (No. above each bar = No. of episodes of syphilis included in this category).
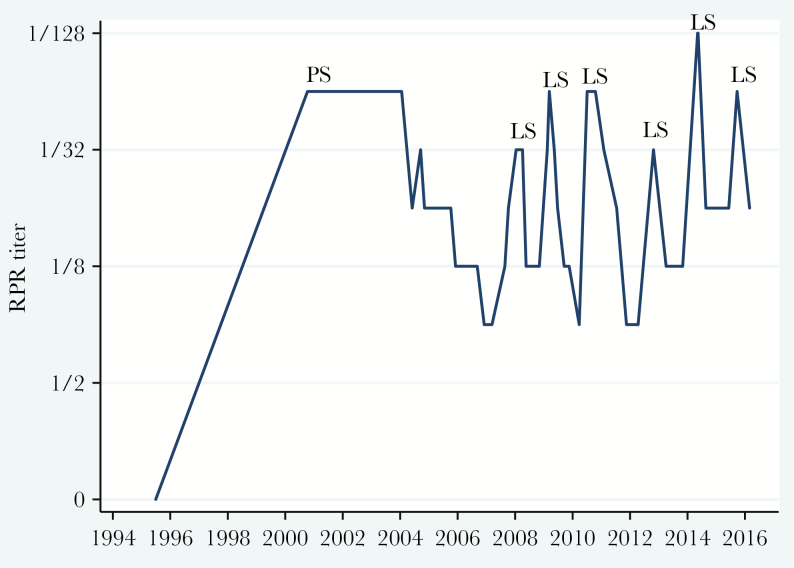
Results of the RPR titer over time are shown for 1 of the patients with 7 episodes of syphilis in Figure 2. After an initial episode of primary syphilis in 2000, he had 6 subsequent episodes of latent syphilis diagnosed over the subsequent 16 years. Of interest, his second and third episodes of syphilis were preceded by an asymptomatic 1-titer rise in his RPR titer from 10 and 4 months previously, respectively.
Figure 2.
Rapid plasma reagin (RPR) titer over time for an individual with 7 episodes of syphilis diagnosed between 2000 and 2017. His first presentation was with primary syphilis (PS), and his subsequent 6 episodes were with latent syphilis (LS).
The proportion with symptomatic syphilis in noninitial episodes of syphilis did not vary according to the stage of syphilis at the initial episode of syphilis. For those with primary, secondary, and latent syphilis at their initial episodes of syphilis, the proportions with symptomatic syphilis at subsequent episodes of syphilis were 4/35 (11.4%), 19/95 (20%), and 5/44 (11.4%), respectively.
DISCUSSION
In our setting, repeat syphilis in HIV-infected individuals is more likely to present asymptomatically. There are 2 compelling explanations for this finding [3]. First, lead time bias, where the frequent screening in clients with a history of syphilis leads to their syphilis being diagnosed before they develop symptoms of syphilis. Second, partial immunity: it is known that T. pallidum infection induces partial immunity to reinfection in humans and rabbits [10–12]. A human inoculation experiment conducted 64 years ago, for example, found that previous syphilis considerably attenuated the response to a T. pallidum challenge [11]. A more recent study found that the plasma cytokine and RPR titer responses differed between initial and repeat syphilis [6]. Partial immunity would predict that repeat syphilis would less likely be symptomatic and/or that if symptomatic, these symptoms would be milder. This was indeed the finding of the only study whose design enabled it to compare the severity of clinical manifestations of syphilis in an intra-individual way. In a review of syphilis infections in an HIV-infected, single-center cohort in France over an 8-year period, detailed clinical notes including photographs were kept from each syphilis diagnosis, which enabled a more detailed and intra-individual comparison than the other studies could perform [5]. The study found that 78% of repeat infections were scored as less symptomatic than initial infections.
The RPR titer trajectory presented in Figure 2 suggests that lead time bias is an implausible explanation for the fact that this client’s second and third episodes of syphilis were asymptomatic. This lead time bias explanation posits that enhanced screening would detect cases of syphilis before they had time to develop symptoms. This explanation is, however, implausible in these 2 episodes of syphilis as the RPR was climbing over 10- and 4-month periods, which are longer than the incubation period for primary syphilis (10–91 days) [13]. We consider it likely that a combination of lead time bias and partial immunity are responsible for repeat syphilis being less symptomatic.
The decline in the proportion symptomatic in repeat syphilis appeared to be mainly driven by a decline in those with secondary and not primary syphilis. Our sample size was too small to justify testing this association statistically, but a larger study of syphilis reinfections noted the following: Although there were no differences in syphilis stage between initial and repeat syphilis overall, in the HIV-infected MSM subgroup, repeaters were less likely than those with initial syphilis to present as secondary syphilis [1]. Further studies in larger cohorts would be useful to better characterize this association.
Our study is limited by its small size, retrospective design, and the fact that we could not ascertain the stage of syphilis for all episodes. The immunological response to infection with Treponema pallidum has been shown to differ between HIV-infected and -uninfected individuals [14]. The fact that all our study participants were HIV-infected therefore means that we cannot extrapolate to HIV-uninfected individuals with syphilis. It is also possible that the immune dysregulation associated with HIV may result in a slower decline and greater fluctuation in RPR titers than in HIV-uninfected individuals [14, 15]. This could result in an increased probability of false-positive diagnoses of repeat syphilis. A systematic review on the topic, however, found little support for this [15]. Only 2 out of 9 studies found that HIV-infected individuals with syphilis were less likely to achieve serological cure. The other 7 studies found no differences in serological response to therapy [15]. Our findings are, however, strengthened by (1) the study taking place in a single center, where the same nontreponemal test has been in use for the past 20 years [16], and (2) the fact that it compares the same group of individuals at initial and repeat episodes of syphilis.
We conclude that this study contributes to a growing body of evidence that suggests that, at least in those with HIV infection, repeat syphilis is more likely to present asymptomatically. This is an important finding as it suggests a clear public health message for patients with syphilis and particularly those with multiple episodes: “If you acquire syphilis again, it is more likely to be asymptomatic. The only way we can assuredly diagnose repeat syphilis in a timely manner is if we check your syphilis tests frequently, such as every 3 to 6 months.” It may also be relevant to understanding the decline in the proportion of syphilis that is symptomatic over the past 8 years in Australia and elsewhere [17]. Chow et al. attributed this decline to the efficacy of enhanced syphilis screening in detecting syphilis before it becomes [17]. A re-analysis of their data revealed that an alternative explanation for the decline in the proportion of syphilis-that-is-symptomatic is that contemporary syphilis outbreaks are characterized by an increasing proportion of cases that are repeat syphilis and therefore asymptomatic [18].
Acknowledgments
Financial support. No funding was received for this study.
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Brewer TH, Peterman TA, Newman DR, Schmitt K. Reinfections during the Florida syphilis epidemic, 2000-2008. Sex Transm Dis 2011; 38:12–7. [DOI] [PubMed] [Google Scholar]
- 2. Katz KA, Lee MA, Gray T, et al. Repeat syphilis among men who have sex with men–San Diego County, 2004-2009. Sex Transm Dis 2011; 38:349–52. [DOI] [PubMed] [Google Scholar]
- 3. Kenyon C, Lynen L, Florence E, et al. Syphilis reinfections pose problems for syphilis diagnosis in Antwerp, Belgium—1992 to 2012. Euro Surveill 2014; 19:20958. [DOI] [PubMed] [Google Scholar]
- 4. Kerani R, Lukehart S, Stenger M, et al. Is early latent syphilis more likely in patients with a prior syphilis infection?British Society for Sexual Health and HIV. Paper presented at: 18th International Society for STD Research, June 28–July 1, 2009; London, UK. [Google Scholar]
- 5. Courjon J, Hubiche T, Dupin N, et al. Clinical aspects of syphilis reinfection in HIV-infected patients. Dermatology 2015; 230:302–7. [DOI] [PubMed] [Google Scholar]
- 6. Kenyon C, Tsoumanis A, Osbak K, et al. Repeat syphilis has a different immune response compared to initial syphilis: an analysis of biomarker kinetics in two cohorts. Sex Transm Infect 2018; 94(3):180–186. [DOI] [PubMed] [Google Scholar]
- 7. Hutchinson CM, Rompalo AM, Reichart CA, Hook EW 3rd. Characteristics of patients with syphilis attending Baltimore STD clinics. Multiple high-risk subgroups and interactions with human immunodeficiency virus infection. Arch Intern Med 1991; 151:511–6. [PubMed] [Google Scholar]
- 8. Van den Bossche D, Florence E, Kenyon C, Van Esbroeck M. Vitros 5600 Syphilis TPA assay: evaluation of an automated chemiluminescence assay for detection of Treponema pallidum antibodies in a high prevalence setting. Sex Transm Dis 2014; 41:680–3. [DOI] [PubMed] [Google Scholar]
- 9. Case definitions for infectious conditions under public health surveillance. Centers for Disease Control and Prevention. MMWR Recomm Rep 1997; 46:1–55. [PubMed] [Google Scholar]
- 10. Morgan CA, Lukehart SA, Van Voorhis WC. Protection against syphilis correlates with specificity of antibodies to the variable regions of Treponema pallidum repeat protein K. Infect Immun 2003; 71:5605–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Magnuson HJ, Thomas EW, Olansky S, et al. Inoculation syphilis in human volunteers. Medicine (Baltimore) 1956; 35:33–82. [DOI] [PubMed] [Google Scholar]
- 12. Sell S, Salman J, Norris SJ. Reinfection of chancre-immune rabbits with Treponema pallidum. I. Light and immunofluorescence studies. Am J Pathol 1985; 118:248–55. [PMC free article] [PubMed] [Google Scholar]
- 13. Tramont E. Syphilis. In: Mandell GL, Bennett JE, Dolin R. Principles and Practice of Infectious Diseases. 8th ed. Philadelphia: Churchill Livingstone Inc; 2015. [Google Scholar]
- 14. Kenyon C, Osbak KK, Crucitti T, Kestens L. The immunological response to syphilis differs by HIV status; a prospective observational cohort study. BMC Infect Dis 2017; 17:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Seña AC, Zhang XH, Li T, et al. A systematic review of syphilis serological treatment outcomes in HIV-infected and HIV-uninfected persons: rethinking the significance of serological non-responsiveness and the serofast state after therapy. BMC Infect Dis 2015; 15:479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kenyon CR, Osbak KK, Van Esbroek M, et al. What is the role of paired rapid plasma reagin testing (simultaneous testing of acute and convalescent samples) in the diagnosis of repeat syphilis and the follow-up of syphilis?Sex Transm Dis 2017; 45:35–8. [DOI] [PubMed] [Google Scholar]
- 17. Chow EPF, Callander D, Fairley CK, et al. ; ACCESS collaboration Increased syphilis testing of men who have sex with men: greater detection of asymptomatic early syphilis and relative reduction in secondary syphilis. Clin Infect Dis 2017; 65:389–95. [DOI] [PubMed] [Google Scholar]
- 18. Kenyon C. Increases in asymptomatic early syphilis may be due to increases in repeat syphilis and not enhanced screening. Clin Infect Dis 2018; 66(5):811–2. [DOI] [PubMed] [Google Scholar]