Abstract
Background
Hypocalcemia is the most common complication of thyroid surgery. The aim of this study was to determine the early predictive factors of postoperative hypocalcemia and to analyze their efficiency.
Methods
We performed a retrospective study of 345 consecutive patients who underwent total thyroidectomy at the Endocrine Surgery Department (Policlinico G. Rodolico Hospital of Catania) between January 2011 and November 2013. We measured serum intact parathormone (iPTH) levels preoperatively and 4 h after surgery. The threshold values of hypocalcemia for iPTH levels and iPTH relative decline were obtained by receiver operating curves (ROC) analysis.
Results
The incidence of hypocalcemia was 32.2% (111 of 345 patients). Our statistical analysis revealed that hypocalcemia rate was strongly correlated with the lower iPTH values and greater iPTH decline (P < 0.001). The threshold enabling prediction of hypocalcemia were 12,5 pg/mL for iPTH and 55,7% for relative iPTH decline. Patients with iPTH <12,5 pg/mL developed hypocalcemia in 58.6% of cases while those with iPTH ≥12,5 pg/dl in 18.8%. Among 175 patients with iPTH relative decline greater than 55,7% hypocalcemia was diagnosed in 91 cases (52%), while other 170 patients with iPTH relative decline less than 55,7% developed hypocalcemia only in 20 cases (11,7%).
Conclusions
The decreased iPTH levels and increased iPTH relative decline resulted to be an accurate predictive factors of postoperative hypocalcemia. The early administration of Calcium and vitamin D in the high-risk patients should be put on in order to prevent the symptoms of hypocalcemia and to reduce the costs and duration of hospitalization.
Keywords: Thyroidectomy, Parathormone, Hypocalcemia
Highlights
-
•
Predictive factors of postoperative hypocalcemia.
-
•
Retrospective study of 345 patients.
-
•
The threshold were iPTH 12,5 ng/L and iPTH decline 55,7%.
1. Introduction
The main life-threatening complications of thyroid surgery include damage to the recurrent laryngeal nerve (RLN) and hypoparathyroidism. To avoid or reduce the incidence of these complications, the surgeon should identify and preserve the RLN and parathyroid glands during intervention. However, the dissection of parathyroid glands can lead to their lesion or accidental removal resulting in a temporary o permanent hypoparathyroidism [1,2]. The incidence of postoperative hypocalcemia varies significantly in the literature from 1,7%–68% [[1], [2], [3], [4]]. Hypocalcemia should be diagnosed early to prevent the appearance of clinical symptoms. Recently different studies have reported the reliability of serum intact parathormone (iPTH) measurements in predicting postoperative hypocalcemia [[5], [6], [7], [8]].
The aim of this study was to analyze the correlation between serum iPTH levels and total serum calcium (Ca) levels and to evaluate the accuracy of postoperative iPTH levels in predicting hypocalcemia in patients who undergo total thyroidectomy. Local ethics committee approved the study.
2. Materials and methods
We performed a cohort retrospective study of 345 consecutive patients who underwent total thyroidectomy at the Endocrine Surgery Department (Policlinico G. Rodolico Hospital of Catania) between January 2011 and November 2013. Surgical indications were benign (64%) and malignant (36%) thyroid pathology; patients affected by Graves' disease were excluded from this review. Demographic, clinical and laboratory data were obtained from hospital records.
Thyroidectomy in all patients was performed by the same team of surgeons; during the intervention we always identified and preserved the recurrent laryngeal nerves through their entire extension, without use of intraoperative neuromonitoring. Parathyroid glands were identified and accurately separated from the thyroid gland with preservation of their vascularization.
We measured iPTH levels preoperatively and 4 h after surgery. Calcemia was measured before surgery and 18 h after operation. iPTH was estimated by the CLIA method (normal range: 15–65 pg/mL). The absolute iPTH decline was defined as: Δ PTH = preoperative iPTH - postoperative 4 h iPTH. Relative iPTH decline was defined as: Δ PTH/pre-PTH = (preoperative iPTH - postoperative 4 h iPTH)/preoperative iPTH. Serum calcium normal values ranged from 8.4 to 10.2 mg/dl, though we considered hypocalcemia when the serum Ca concentration was <8.0 mg/dl.
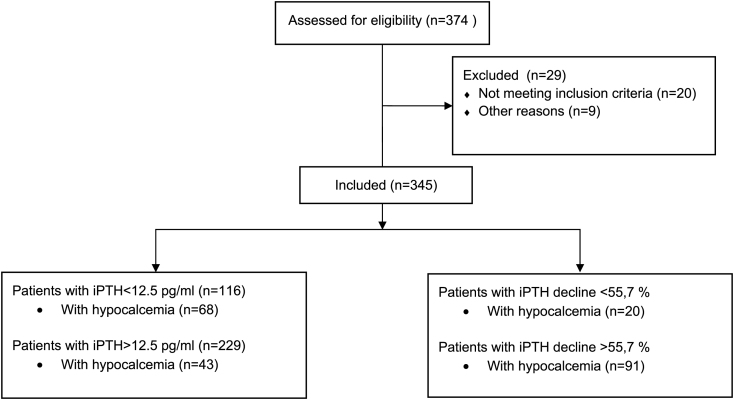
All patients with subnormal iPTH levels or patients who developed hypocalcemia received oral calcium and vitamin D supplements even if they didn't present any symptoms. Patients with hypocalcemia symptoms received intravenous infusion of calcium gluconate. (Flow Diagram).
Statistical analysis was performed using the Statistica version 10.0 and R software. Comparisons of data were obtained by Student-t and chi-squared tests. Results were considered statistically significant when p < 0,05. To identify the cut-off values for iPTH levels and iPTH decline and to analyze their diagnostic accuracy in predicting postoperative hypocalcemia we used the receiver operating characteristic (ROC) curve and we measured the area under the curve (AUC). The manuscript is compliant with the STROCSS criteria [9].
3. Results
The 345 patients included 267 females (77%) and 78 males (23%), the mean age was 51,2 years old (ranging from 11 to 85 years). Hypocalcemia, as defined by Ca levels lower than 8.0 mg/dl at 18 h after surgery, was observed in 111 (32.2%) of 345 patients. Of 111 patients with hypocalcemia, 70 (63.0%) patients were symptomatic and 41 (37.0%) were asymptomatic. In the majority of the cases hypocalcemia was transient, only two patients (0.005%) showed permanent hypocalcemia (evaluated 6 months after total thyroidectomy).
Of the preoperative iPTH estimates, all patients had normal levels of iPTH range from 14 to 105 pg/mL, with a mean value of 51.5 pg/mL. Postoperative measurements of iPTH revealed that the patients who developed postoperative hypocalcemia had a significant lower postoperative iPTH levels (mean iPTH = 13,9 pg/mL) than normocalcemic patients (mean iPTH = 30,4 pg/mL) and a significantly greater iPTH relative decline (70,9%). Table 1.
Table 1.
Mean preoperative and postoperative iPTH levels and iPTH relative decline in hypocalcemic and normocalcemic patients.
| All patients |
Hypocalcemic |
Normocalcemic |
P | |
|---|---|---|---|---|
| n = 345 | n = 111 | n = 234 | ||
| Mean preoperative PTH level,ng/L | 51,2 | 51,5 | 50,9 | <0.001 |
| Mean postoperative PTH level,ng/L | 25,1 | 13,9 | 30,4 | <0.001 |
| Mean PTH relative variation,% | 49,1 | 70,9 | 38,7 | <0.001 |
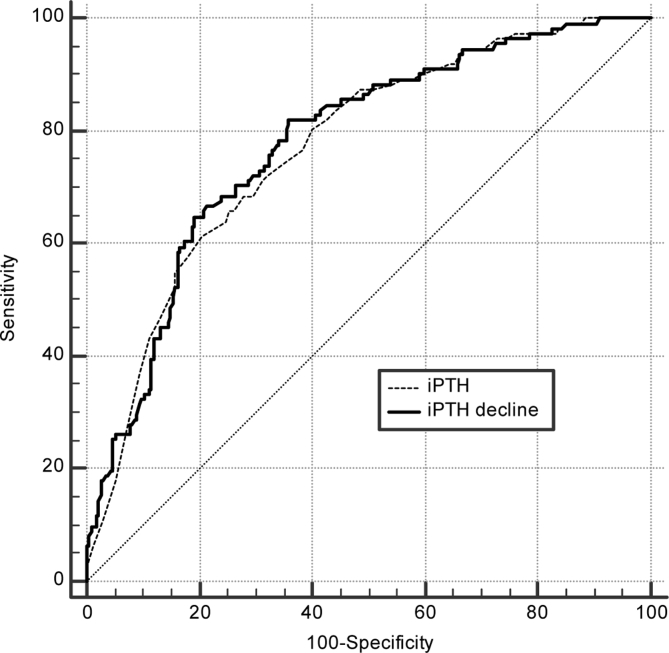
ROC analysis was performed. Fig. 1 showes the ROC curves corresponding to postoperative 4 h iPTH level and relative iPTH decline. From this analysis we obtained the optimal thresholds enabling prediction of hypocalcemia for iPTH (12,5 pg/mL) and relative iPTH decline (55,7%).
Fig. 1.
ROC analysis of postoperative 4 h iPTH and iPTH relative decline in predicting postoperative hypocalcemia.
Sensitivity, specificity, and positive and negative predictive values for iPTH with a threshold of 12,5 pg/mL were 61% (95% confidence interval [95%CI] 51,5–70,4), 79,5% (95% CI 73,7–84,5), 58,6% (95% CI 49,1–67,7) and 81,2% (95% CI 75,6–86,1). The curve had an area under the curve (AUC) of 0.77 (SE = 0.05, 95% CI = 0.72–0.81, P < 0.0001). Patients with iPTH levels <12,5 pg/mL developed hypocalcemia in 58.6% (68 of 116 patients) of cases while those with iPTH ≥12,5 pg/mL had hypocalcemia only in 18.8% (43 of 229 patients) of cases. These results are strongly significant (P < 0.001). Table 2.
Table 2.
Acurancy of postoperative iPTH level in predicting postoperative hypocalcemia.
| Patients with iPTH <12,5 pg/mL | Patients with iPTH ≥12,5 pg/mL | |
|---|---|---|
| Number of patients (total: 345) | 116 | 229 |
| Mean postoperative Ca level (mg/dl) | 7.8 | 8.4 |
| Hypocalcemia rate | 68 (58,6%) | 43 (18,8%) |
| P value iPTH vs Ca levels | p < 0,001 | p < 0,001 |
Sensitivity, specificity, and positive and negative predictive values for the relative iPTH decline with a threshold of 55,7% were 82,0% (95% 73,6–88,6), 64,1% (95% CI 57,6–70,2), 52,0% (95% CI 44,3–59,6) and 88,2% (95% CI 82,4–92,7). The curve had an AUC of 0.78 (SE = 0.05, 95% CI = 0.73–0.82, P < 0.0001). Among 175 patients with iPTH relative decline greater than 55,7% hypocalcemia was diagnosed in 91 cases (52%), while other 170 patients with iPTH relative decline less than 55,7% developed hypocalcemia only in 20 cases (11,7%). Table 3.
Table 3.
Acurancy of postoperative iPTH relative decline in predicting postoperative hypocalcemia.
| Patients with iPTH decline <55,7% | Patients with iPTH decline ≥55,7% | |
|---|---|---|
| Number of patients (total: 345) | 170 | 175 |
| Mean postoperative Ca level (mg/dl) | 8.5 | 7.9 |
| Hypocalcemia rate | 20 (11,7%) | 91 (52%) |
| P value iPTH decline vs Ca levels | p < 0,001 | p < 0,001 |
Hospital stay was significantly longer in symptomatic patients (mean hospital stay 3,4 days; range 2–7 days) compared with those asymptomatic (mean stay 2,2; range 2–3 days), (p < 0.001).
4. Discussion
Despite the accurate identification and preservation of parathyroid glands during thyroidectomy, postoperative hypocalcemia remains the most common complication after thyroid surgery. It frequently occurs due to the failure of parathyroid glands resulting in low PTH production and consequent reduction of serum calcium levels[[10], [11]].
Hypocalcemia is often asymptomatic, though it can present with different symptoms such as paresthesia, perioral or digital tingling, muscle cramps or tetany. When severe it can manifest with life threatening cardiovascular events including heart blocks, hypocalcemic cardiomyopathy, and requires intravenous therapy to relieve the symptoms[[12], [13]].
The functioning insufficiency of parathyroid tissue is caused by inadvertent removal of parathyroid glands or their damage during surgical manipulations such as devascularization, thermal or mechanical trauma, restraint of venous function [14,15]. Graves' disease, retrosternal goiter, central neck dissection, re-interventions, thyroid malignancies and parathyroid autotransplantation have all been shown to increase the risk of postoperative hypocalcemia [[16], [17], [18]].
The early monitoring of calcium levels in postoperative period is very important in the prevention of symptomatic hypocalcemia. However it was demonstrated that the appearance of postoperative hypocalcemia can be delayed up to 12–24 h after surgery. Delay in the diagnosis can lead to the retard in treatment and prolongation of hospitalization [6]. Different studies have revealed the correlation between the decrease of serum iPTH levels and Calcium levels [[19], [20], [21], [22]]. Intact PTH is characterized by a short half-life of 1–4 min [23], thus its decrease may be detected previously in the early postoperative period.
Lombardi et al. reported that iPTH levels <10 pg/mL at 4 and 6 h after thyroidectomy accurately predict the appearance of postoperative hypocalcemia and necessity of pharmacological therapy [6]. Carr et al. confirm that iPTH level of 10 pg/mL o less measured 4 h after surgery is an accurate predictor of postoperative hypocalcemia which allows the earlier identification of patients who need supplementary treatment with calcium and vitamin D [7]. Other studies suggested that a single measurement of iPTH levels 1 h after thyroid surgery is a strong predictor of postoperative hypocalcemia[[24], [25]]. Nevertheless, in several studies decrease in serum iPTH levels seemed not to be predictive of postoperative hypocalcemia[[26], [27]].
Recently some authors studied the role of iPTH decline in order to find a more accurate predictive factor of hypocalcemia. Lecerf et al. reported that the iPTH decline (iPTH decline > 68.5%) is more precise than the single measurement of postoperative iPTH levels and allows earlier identification of patients at a high risk of hypocalcemia[28]. Seo et al. suggested that iPTH level of <10.42 pg/mL and decrease of >70% of PTH levels 1 h after surgery were the reliable predictive factors of postoperative hypocalcemia[29].
In our review we observed that mean postoperative iPTH level and iPTH relative decline were predictive factors of postoperative hypocalcemia. By using the ROC analysis we found that both tests yield the same overall diagnostic performance. Consequently, the calculation of iPTH relative decline could be avoided, and only a single measurement of iPTH at 4 h after surgery may be used like a predictive factor of hypocalcemia. We found that a level of iPTH <12,5 pg/mL correctly identify the patients at high risk of postoperative hypocalcemia, though the level of iPTH ≥12,5 pg/mL does not exclude absolutely the appearance of hypocalcemia. In our series of patients the rate of hypocalcemia with a level of iPTH ≥12,5 pg/mL was 18.8%. Therefore, the monitoring of Ca levels in the postoperative period is recommended in all patients. Ca and vitamin D supplementation should be placed on in the high-risk patients, in the patients with the serum Ca concentration <8.0 mg/dl and in the patients with symptomatic hypocalcemia.
5. Conclusions
In this study we analyzed the predictive value of iPTH levels and iPTH relative decline and we found that a level of iPTH <12,5 pg/mL and iPTH relative decline ≥55,7% correctly predict the patients at high risk of postoperative hypocalcemia. The authors suggest that early administration of Calcium and vitamin D in these patients should be indicated in order to prevent the symptoms of hypocalcemia and to reduce the costs and duration of hospitalization.
Ethical approval
No ethical approval was required.
Sources of funding
No funding received.
Author contribution
Cannizzaro MA: study design.
Okatyeva V: data analysis, writing.
Lo Bianco S: data analysis, writing.
Caruso V: data collections.
Buffone A: study design.
Conflicts of interest
The authors declare that they have no conflict of interest.
Research registration unique identifying number (UIN)
Researchregistry2870.
Guarantor
Cannizzaro Matteo Angelo.
Footnotes
The authors declare that they have no conflict of interests.
Contributor Information
Matteo Angelo Cannizzaro, Email: cannizzaromatteoangelo@yahoo.it.
Valeriya Okatyeva, Email: okvaleria@hotmail.com.
Salvatore Lo Bianco, Email: salvo.lobianco@alice.it.
Valerio Caruso, Email: va.caruso@hotmail.it.
Antonino Buffone, Email: a.buffone@unict.it.
References
- 1.Pattou F., Combemale F., Fabre S. Hypocalcemia following thyroid surgery: incidence and prediction of outcome. World J. Surg. 1998;22:718–724. doi: 10.1007/s002689900459. [DOI] [PubMed] [Google Scholar]
- 2.Costanzo M., Marziani A., Condorelli F. Post-thyroidectomy hypocalcemic syndrome: predictive value of early PTH. Preliminary results. Ann. Ital. Chir. 2010;81:301–306. [PubMed] [Google Scholar]
- 3.Asari R., Passler C., Kaczirek K. Hypoparathyroidism after total thyroidectomy. A prospective study. Arch. Surg. 2008;143:132–137. doi: 10.1001/archsurg.2007.55. [DOI] [PubMed] [Google Scholar]
- 4.Bhattacharyya N., Fried M.P. Assessment of the morbidity and complications of total thyroidectomy. Arch. Otolaryngol. Head Neck Surg. 2002;128:389–392. doi: 10.1001/archotol.128.4.389. [DOI] [PubMed] [Google Scholar]
- 5.Tartaglia F, Giuliani A, Sgueglia M et al. (200%) Randomized study on oral administration of calcitriol to prevent symptomatic hypocalcemia after total thyroidectomy. Am. J. Surg. 190: 424–429. [DOI] [PubMed]
- 6.Lombardi C.P., Raffaelli M., Princi P. Early prediction of postthyroidectomy hypocalcemia by one single iPTH measurement. Surgery. 2004;136:1236–1241. doi: 10.1016/j.surg.2004.06.053. [DOI] [PubMed] [Google Scholar]
- 7.Carr A.A., Yen T.W., Fareau G.G., Cayo A.K., Misustin S.M., Evans D.B. A single parathyroid hormone level obtained 4 hours after total thyroidectomy predicts the need for postoperative calcium supplementation. J. Am. Coll. Surg. 2014;219(4):757–764. doi: 10.1016/j.jamcollsurg.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Baldassarre R.L., Chang D.C., Brumund K.T. 2012. Predictors of Hypocalcemia after Thyroidectomy: Results from the Nationwide Inpatient Sampl. ISRN Surgery 838614 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agha R.A., Borrelli M.R., Vella-Baldacchino M., Thavayogan R., Orgill D.P., for the STROCSS Group The STROCSS statement: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2017;46:198–202. doi: 10.1016/j.ijsu.2017.08.586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roh J.L., Park C. Intraoperative parathyroid hormone assay for management of patients undergoing total thyroidectomy. Head Neck. 2006;28:990–997. doi: 10.1002/hed.20444. [DOI] [PubMed] [Google Scholar]
- 11.Promberger R., Ott J., Kober F. Normal parathyroid hormone levels do not exclude permanent hypoparathyroidism after thyroidectomy. Thyroid. 2011;21:145–150. doi: 10.1089/thy.2010.0067. [DOI] [PubMed] [Google Scholar]
- 12.Reber P.M., Heath H., 3rd Hypocalcemic emergencies. Med. Clin. 1995;79:93–106. doi: 10.1016/s0025-7125(16)30086-4. [DOI] [PubMed] [Google Scholar]
- 13.Baldassarre R.L., Chang D.C., Brumund K.T. 2012. Predictors of Hypocalcemia after Thyroidectomy: Results from the Nationwide Inpatient Sampl. ISRN Surgery 838614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang J., Gu J., Han Q. Value of intraoperative parathyroid hormone monitoring in papillary thyroid cancer surgery: can it be used to guide the choice of operation methods? Int. J. Clin. Exp. Med. 2015;8:7778–7785. [PMC free article] [PubMed] [Google Scholar]
- 15.Lorente-Poch L., Sancho J.J., Muňoz-Nova J.L. Defining the syndromes of parathyroid failure after total thyroidectomy. Gland Surg. 2015;4:82–90. doi: 10.3978/j.issn.2227-684X.2014.12.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qasaimeh G.R., Al Nemri S., Al Omari A.K. Incidental Extirpation of the parathyroid glands at thyroid surgery: risk factors and post-operative hypocalcemia. Eur. Arch. Oto-Rhino-Laryngol. 2011;268:1047–1051. doi: 10.1007/s00405-010-1413-x. [DOI] [PubMed] [Google Scholar]
- 17.Rajinikanth J., Paul M.J., Deepak Abraham T. Surgical audit of inadvertent parathyroidectomy during total thyroidectomy: incidence, risk factors, and outcome. Medscape J Med. 2009;11:29. [PMC free article] [PubMed] [Google Scholar]
- 18.Paek S.H., Lee Y.M., Min S.Y. Risk factors of hypoparathyroidism following total thyroidectomy for thyroid cancer. World J. Surg. 2013;37:94–101. doi: 10.1007/s00268-012-1809-4. [DOI] [PubMed] [Google Scholar]
- 19.Jumaily J.S., Noordzij J.P., Dukas A.G. Prediction of hypocalcemia after using 1- to 6-hour postoperative parathyroid hormone and calcium levels: an analysis of pooled individual patient data from 3 observational studies. Head Neck. 2010;32:427–434. doi: 10.1002/hed.21199. [DOI] [PubMed] [Google Scholar]
- 20.Wang T.S., Cayo A.K., Wilson S.D. The value of postoperative parathyroid hormone levels in predicting the need for long-term vitamin D supplementation after total thyroidectomy. Ann. Surg Oncol. 2011;18:777–781. doi: 10.1245/s10434-010-1377-5. [DOI] [PubMed] [Google Scholar]
- 21.Cayo A.K., Yen T.W., Misustin S.M. Predicting the need for calcium and calcitriol supplementation after total thyroidectomy: results of a prospective, randomized study. Surgery. 2012;152:1059–1067. doi: 10.1016/j.surg.2012.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raffaelli M., De Crea C., Carrozza C. Combining early postoperative parathyroid hormone and serum calcium levels allows for an efficacious selective post-thyroidectomy supplementation treatment. World J. Surg. 2012;36:1307–1313. doi: 10.1007/s00268-012-1556-6. [DOI] [PubMed] [Google Scholar]
- 23.Sywak M.S., Palazzo F.F., Yeh M. Parathyroid hormone assay predicts hypocalcaemia after total thyroidectomy. ANZ J. Surg. 2007;77:667–670. doi: 10.1111/j.1445-2197.2007.04183.x. [DOI] [PubMed] [Google Scholar]
- 24.Lam A.1, Kerr P.D. Parathyroid hormone: an early predictor of postthyroidectomy hypocalcemia. Laryngoscope. 2003;113(12):2196–2200. doi: 10.1097/00005537-200312000-00029. [DOI] [PubMed] [Google Scholar]
- 25.AlQahtani Awad, Parsyan Armen, Payne Richard, Tabah Roger. Parathyroid hormone levels 1 hour after thyroidectomy: an early predictor of postoperative hypocalcemia. Can. J. Surg. 2014;57 doi: 10.1503/cjs.008013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Del Rio P., Arcuri M.F., Ferreri G. The utility of serum PTH assessment 24 hours after total thyroidectomy. Otolaryngol. Head Neck Surg. 2005;132:584–586. doi: 10.1016/j.otohns.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 27.Ghaheri B.A., Liebler S.L., Andersen P.E. Perioperative parathyroid hormone levels in thyroid surgery. Laryngoscope. 2006;116:518–521. doi: 10.1097/01.MLG.0000202617.63668.CC. [DOI] [PubMed] [Google Scholar]
- 28.Lecerf P., Orry D., Perrodeau E. Parathyroid hormone decline 4 hours after total thyroidectomy accurately predicts hypocalcemia. Surgery. 2012;152:863–868. doi: 10.1016/j.surg.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 29.Seo S.T., Chang J.W., Jin J., Lim Y.C., Rha K.S., Koo B.S. Transient and permanent hypocalcemia after total thyroidectomy: early predictive factors and long-term follow-up results. Surgery. 2015;158(6):1492–1499. doi: 10.1016/j.surg.2015.04.041. [DOI] [PubMed] [Google Scholar]