Abstract
Objective
Activity trackers are designed to support individuals in monitoring and increasing their physical activity. The use of activity trackers among individuals diagnosed with depression and anxiety has not yet been examined. This pilot study investigates how this target group engages with an activity tracker during a 10-week health intervention aimed to increase their physical activity level and improve their physical and mental health.
Methods
Two groups of 11 young adults (aged 18–29 years) diagnosed with depression or anxiety participated in the digital health intervention. The study used mixed methods to investigate the research question. Quantitative health data were used to assess the intervention’s influence on the participants’ health and qualitative data provided insights into the participants’ digital health experience.
Results
The study demonstrated an ambiguous influence from the use of an activity tracker with positive physical and mental health results, but a fading and even negative digital health engagement and counterproductive competition.
Conclusions
The ambiguous results identify a need for (1) developing strategies for health professionals to provide supervised use of activity trackers and support the target groups’ abilities to convert health information about physical activity into positive health strategies, and (2) designing alternatives for health promoting IT targeted users who face challenges and need motivation beyond self-tracking and competition.
Keywords: Activity tracker, health monitoring, anxiety disorders, depressive disorder, general practice
Introduction
Numerous types of monitoring technologies have migrated from clinical use into lay peoples’ lives in the form of consumer technologies for supporting everyday health. Relatively inexpensive consumer products such as blood pressure monitors, glucose meters, activity trackers and mobile applications (apps) for self-monitoring daily sleep, diet and exercise provide people with the technological ability to produce and manage their personal health data. Market developments predict that consumer technology for health management will continue to increase – it has been estimated that wearable health technology will become the eighth largest revenue driver within consumer and mobile devices in 2018.1 This increase shows strong indications of consumers’ interests in everyday health information management and it opens opportunities for healthcare providers to develop and implement digital health interventions.2,3 There are many prospects for self-tracking of everyday health.4,5 However, research is needed to investigate the use of tracking technology for various target groups and to contribute to an understanding of the scope of tracking technology and nuances related to digital health engagement.6 The research reported in this paper contributes to a growing body of research on the effect of tracking technology on people’s health engagement. The presented study contributes insights into the use of activity trackers among young adults who face challenges maintaining daily physical activity because of depression and anxiety. Recent research on mobile tracking demonstrates that people who self-track are typically young and educated7,8 or people (mostly men) with a high interest in technology.9 This supports a growing concern that most health information technology (IT) is designed for ‘people like us’, i.e. ‘people who believe to understand healthcare and health issues, take care of their own health, are literate, well to do, tech-savvy, and hold a tertiary qualification’.10 The use of tracking technologies among people diagnosed with anxiety and depression has not yet been investigated systematically. However, studies on this target group are important for understanding how to innovate existing and future health IT to provide functional support to people who face health challenges. People with mental disorders are considered vulnerable because they have a high risk of early death due to physical and medical conditions caused by a series of risk factors, including a low physical activity level.11 Common symptoms following the diagnoses of depression and anxiety include fatigue and difficulties organising and conducting daily activities, which hamper the ability to be physically active on a daily or regular basis.12 However, it is not known if using IT health tools is effective in supporting a healthier lifestyle in young people with mental health problems. The aim of the present study was to explore opportunities related to digital health interventions for a group of patients who were motivated but challenged in their attempts to increase their physical activity levels.
Activity trackers
Activity trackers exist in various forms of wearable accelerometers, e.g. bracelets, watches, pendants and clips that can be attached to shoes or clothing. Because many people carry smartphones, activity trackers are also found in mobile apps. These wearable and mobile technologies offer users an easy way to track daily activity, which is highlighted in the literature as central to their success.13 Additionally, activity trackers are considered a mature technology. A recent technical assessment of activity trackers’ accuracy has documented that affordable consumer trackers can compete with advanced medical products when it comes to accuracy.14
Activity trackers record the physical activity of their users by counting steps and distance via a mix of accelerometers, GPS and other sensors. Advanced activity trackers include heart-rate monitors. The earliest electronic activity trackers were developed with goals of 10,000 steps per day, based on Japanese walking culture. This goal has since been documented as a positive health goal that is now found in most activity trackers.15,16 The interface of activity trackers gives information about the daily activity status either within the 10,000 steps goal or a personal goal set by the user. Most activity trackers also give reminders for users to be active, e.g. red flashes if the user has been inactive for a certain period of time. Almost all activity trackers connect via Bluetooth to a mobile iOS and/or Android app, where users can find data about specific activities and developments in their activity level.
Health interventions with activity trackers
Potentials for activity trackers in health interventions are continuously explored within specific target groups such as men with prostate cancer,13 youths who are overweight or obese,17 older adults,9,18,19 patients in rehabilitation,20 patients with Parkinson’s disease21 and community-oriented walking interventions.22 Literature reviews analysing the effect of activity trackers across multiple studies show that trackers have a positive influence on users’ physical activity levels during digital health interventions and that the best results are found when focusing interventions on specific groups of patients.16,23 However, despite the growing body of studies, knowledge about the potential and drawbacks of activity tracking is incipient9 and research is dominated by studies focusing on the short-term effects on individuals who are already physically active.24 Recent research in digital health interventions is increasingly occupied with opportunities for healthcare professionals to make use of the large volume of personal health data generated by patients in their everyday lives via tracking technology. This includes studies on patient-generated data (PGD) in clinical practice3 with an interest in how PGD can support patient-provider collaboration.2
In addition to research on activity trackers’ influence on health effects, a minor but significant part of related work is occupied with understanding people’s motives and experience of using tracking technology and includes studies of why and how people use activity trackers,25–28 how people experience self-tracking,29 why people abandon activity trackers,30 digital health engagement strategies6 and broader studies of the appropriation of self-monitoring devices in everyday domestic environments.31 This research is characterised by critical examinations of technology use and emphasises that the health behaviour associated with activity trackers is interwoven in complex contextual factors and raises concerns that too simple assumptions are made about tracking technology’s influence on health behaviour.
Research questions
Against this background, we have investigated the health effect of the use of tracking technology among young adults diagnosed with depression and anxiety. To the best of our knowledge, no previous study has investigated the use of activity tracking among individuals who face challenges in their daily physical activity because of depression and anxiety with the aim of understanding opportunities for this technology in a health-professional setting. With this background, the pilot study presented herein explores opportunities for digital health interventions that reach beyond consultations and clinical treatment in general practice. This pilot study is a first step in the research and development of digital health interventions targeting individuals with depression and anxiety. The research is anchored in the theory on planned behaviour emphasising perceived behavioural control as a central component to investigations of behaviour.34 Thus, in addition to investigations of the quantitative physical health effects from activity tracking, this pilot study also investigates the qualitative perceived health effects from activity tracking among the participating young adults. On this basis, we have set up and examined the health effects related to the use of activity trackers with the following research questions:
How does activity tracking influence the engagement of young adults with depression and anxiety in own health identified through investigating the activity tracking’s influence on (1) the target group’s physical and mental health and (2) the target group’s digital health engagement?
Methods
The activity tracker
This study explored the use of the wearable activity tracker Garmin VivoFit and its mobile app (Figure 1). The activity tracker was chosen because of its high score in accuracy and because it had a battery life greater than one year and is waterproof, meaning the participants could wear the tracker during the whole health intervention without needing to take it off for battery charging or showers.
Figure 1.
The health intervention presented in this paper used the Garmin VivoFit activity tracker. (Images retrieved from vendor’s website: (https://buy.garmin.com/da-DK/DK/p/143405).
The activity tracker shows the users’ steps via a display on the bracelet (Figure 1). Steps are counted per day and the tracker resets each day at midnight. If the user has been inactive for two hours, a move bar flashes a red light in the display. There is one device key on the tracker. When the user clicks this key, they shift between the following types of information in the display: (1) the clock, (2) the date, (3) the accumulated number of steps on the current day, (4) the remaining number of steps for the user to reach the set goal of the day, (5) the accumulated activity of the day measured in miles or kilometres and (6) an estimation of calories burned during the day. The tracker stores data for up to three weeks. The user transfers data from the tracker to a personal account in a mobile app by holding the device key until ‘sync’ appears in the display. The user can also choose to measure sleep by holding the device key until ‘sleep’ appears in the display.
Via the mobile app the users access their tracking history and follow developments in activity level and hours of sleep per day, per week, per month and per year. When the user reaches a certain number of steps, they receive rewards in form of badges. In the mobile app, users can also create groups and see ranking lists of group members, which are updated when users synchronise their data. Figure 2 presents examples of the central features in the mobile app: visualisation of daily measures (left and middle) and group ranking (right).
Figure 2.
Main features in the mobile application for the activity tracker. Visualisation of daily measures (left and middle) and group ranking (right).
Participants
We recruited participants for the health intervention via a general practice, and we included young adults (aged 18–30) with depression and/or anxiety who had a low physical activity level (less than two hours per week). All participants were also recruited by postal code to support that activities in the health intervention were taking place in a manageable distance for all participants. The exclusion criteria were: no registered diagnoses of depression or anxiety in the electronic medical record (ICPC2 diagnosis codes P01, P03, P76, P74, P79 or corresponding ICD10 diagnoses), inability to communicate in Danish, significant abuse of alcohol or narcotics, inability to participate due to other diseases or physical impairment and no informed consent.
We conducted the health intervention in two iterations because most participants could only cope interacting with a low number of people. In total, 11 participants were recruited for an intervention in autumn 2015 and another 11 participants were recruited for an intervention in spring 2016. The local general practitioner (GP) informed all participants about the study, and they were scheduled for a first interview and health check at the general practice clinic prior to the health intervention. The health check included auscultation of the lungs and heart, measurement of blood pressure, electrocardiogram and overall assessment of health status to ensure eligibility for the study. All participants were recruited and participated on a volunteer basis and signed an informed consent form. All participants completed their participation in the project. Table 1 shows the baseline characteristics of the participants
Table 1.
Baseline characteristics of participants.
| Number | % | |
|---|---|---|
| Gender | ||
| Male | 3 | 13.6 |
| Female | 19 | 86.4 |
| Diagnoses (ICPC2 code) | ||
| Anxiety/nervousness (P01) | 3 | 13.6 |
| Sadness (P03) | 5 | 22.7 |
| Anxiety disorder (P74) | 4 | 18.2 |
| Depression (P76) | 10 | 45.5 |
| Mean (SD) | Range | |
| Age | 24.6 (3.8) | 19-30 |
The health intervention
The health intervention was assigned the title ‘PulseUp’ to signal the goal of increasing the physical activity level and to target a young audience. The intervention included several activities presented in an overview in Table 2. All exercise activities (weeks one to eight) were levelled in relation to the health results (baseline) from the participants.
Table 2.
Activities in the digital health intervention.
| Time | Activity |
|---|---|
| Two months prior to the intervention | Recruit 11 participants for intervention I and II |
| Week 0: baseline | Health tests and pre-interviews |
| Weeks 1-8: intervention | Two hours of exercise Tuesday and Thursday each week |
| Week 9: evaluation | Joint evaluation workshop |
| Week 10: assessment | Health tests and post interviews |
In addition to wearing an activity tracker, all participants were given a health check and participated in individual interviews prior to and after the intervention. All participants met with instructors for group exercise activities (fitness, walking tours, ball games etc.) twice a week. A closed Facebook group was set up to support communication among all parties in the health intervention. The Facebook group was open to all kinds of posts from the health professionals, researchers and the participating young adults.
Evaluation of physical and mental health effects
To evaluate their cardiovascular fitness, all participants performed a sub-maximal cycle ergometer test before and after the intervention. The participants started at a 50 W load, which was increased by 25 W every second minute until the target heart rate (pulse) level was reached. We aimed to reach 65% of the pulse reserve, which was calculated as resting pulse + 65%*(220 − age − resting pulse). When reaching the level of the target pulse, the participant cycled for six minutes and the pulse was recorded. The re-test used the same time intervals and loading used in the initial test. The participants’ heart rate, workload and gender provided a basis for calculating their fitness levels.32 A reduction in heart rate when working at a given workload signified an improved cardiovascular fitness.
To evaluate the participants’ experienced health effects, a quality of life test was conducted before and after the intervention using the World Health Organization Five Well-Being Index (WHO-5).33 The index assesses subjective psychological well-being by asking five questions regarding spirits, calmness, feeling active, feeling fresh when waking up and feeling as if life has been filled with things of interest.
Descriptive statistics include mean (SD) for age and number (%) for categorical variables. Changes over time were tested in Stata, IC version 12.0 (College Station, Texas, USA) using a paired two-sided t-test; a P value of < 0.05 was considered statistically significant.
Additionally, data from the participants’ activity trackers were extracted to an Excel file by the end of each week in the intervention. On this basis a total activity level per week was calculated for the participants.
Evaluation of digital health engagement
To investigate the participants’ digital health engagement, we conducted a semi-structured qualitative interview with each participant before and after the intervention. The interview guidelines and analysis were rooted in theory of planned behaviour.34 Following this theory, interview questions and data analysis focused on understanding the participants’ perceived behavioural control from engaging with the activity tracker. This included questions related to their expectations for activity tracking, their motivation to use the activity tracker and their perceived health behavioural control during activity tracking. The interviews were conducted in a meeting room at the general practice clinic in conjunction with the cycling test and quality of life/WHO-5 test. Each interview lasted approximately 30 minutes, and was audio recorded and transcribed. Data from the 44 qualitative interviews were coded following the procedure for inductive thematic analysis.35 This included a verbatim account of all interviews, a reading and coding process starting with the use of initial codes of semantic content in each interview followed by a search for and identification of key themes that appeared across the interviews. The results from the analysis were key themes related to the use and non-use of the activity tracking and themes about positive and negative digital health engagement. These key themes were synthesised into identified contradicting dimensions in their digital health engagement from activity tracking. The key themes and synthesis are presented below. All quotations have been translated from Danish.
Results
Activity tracking’s influence on physical and mental health
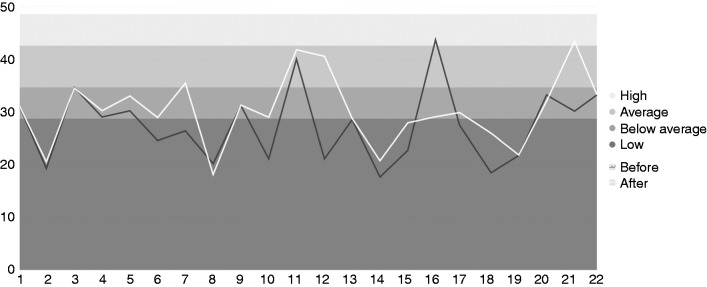
As Figure 3 shows, the fitness levels of seven participants improved after completing the health intervention, whereas those of 11 participants remained in the same interval. Four participants did not participate in the post-test. Overall, the fitness levels of all participants were significantly higher after the health intervention compared to before (lower pulse at submaximal work load).a
Figure 3.
Cardiovascular fitness level before and after the intervention.1,2 Participants are listed in the horizontal line, and the fitness level is listed in the vertical line. Results from the pre-test are visualised with the darker shaded line and the results from the post-test are visualised with the lighter shaded line.
1Fitness level was estimated from a sub-maximal cycle ergometer test.
2Four participants were not retested.
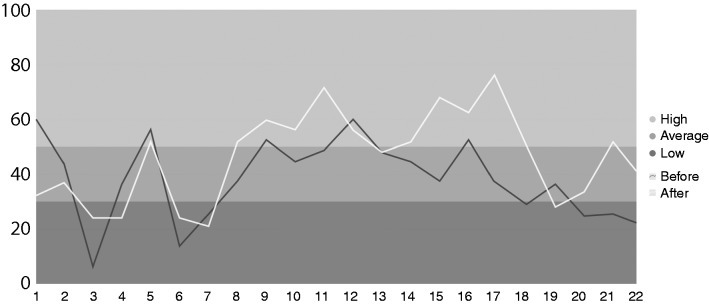
As shown in Figure 4, the WHO-5 scores for nine of the participants are in a higher interval after the health intervention compared to before, nine participants’ scores are in the same interval before and after the intervention and three participants’ scores are in a lower interval. One participant did not participate in the post-test. Overall, the WHO-5 scores for all participants are significantly higher after the health intervention compared to before.b
Figure 4.
WHO-5 scores – quality of life – for all participants before and after the intervention. Participants are listed in the horizontal line, and the WHO-5 scores are listed in the vertical line. Results from the pre-test are visualised with the dark-coloured line, and the results from the post-test are visualised with the light-coloured line.
WHO-5: World Health Organization Five Well-Being Index.
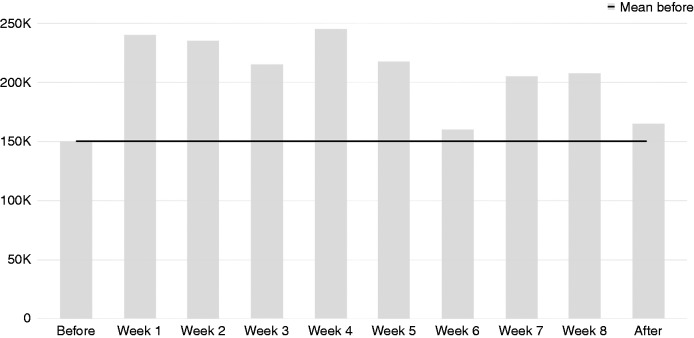
Data from the activity trackers showed that the activity level for all participants increased during the health intervention compared to the baseline measured in week 0 (see Table 2). Figure 5 communicates the collective number of steps for all participants during the interventions. For everyone there was an increase in the activity level during the intervention compared to the mean before the intervention and a fade in the activity level after the intervention.
Figure 5.
Activity level – data from the activity trackers – for all participants during the health intervention.
In sum, the health results support related research demonstrating that activity trackers have a positive effect on participants’ activity level and health during health interventions.16,23
Activity tracking’s influence on digital health engagement
The coding of the participants’ expectations for activity tracking identified a low experience with use of tracking technology and health apps in general. Table 3 lists exercise apps known and used by the participants before beginning the intervention. Apps known by some of the participants include pedometers (wearables and pedometers in mobile phones), apps for tracking exercise (the app Endomondo is used by four of the participants and two had tried the app once), apps for calorie counting (Lifesum, Foodlog, MyFitnessPal) and various websites were used to browse for information about healthy food, recipes and weight loss. Six participants had once used apps with exercise instructions (SevenMinutes and YouTube channels) and one participant was using an app with instructions for mindfulness.
Table 3.
Applications known by the participants before starting the intervention.
| Application | Know | Use |
|---|---|---|
| Pedometer | 1 | 2 |
| Apps for tracking exercise | 2 | 4 |
| Apps for calorie counting | 2 | 1 |
| Websites with information about weight loss and recipes | 3 | 2 |
| Apps with exercise instructions | 6 | 1 |
App, application.
One important finding is that the number of known apps (middle column in Table 3) exceeded the number of used apps (right column in Table 3). The majority of the participants reported the non-use of exercise apps when asked, ‘Do you know of or use apps for exercise or health in general?’. Examples of answers are: ‘I know that there are many apps, but I don't use them' and ‘My sister uses a lot of apps for health but I don't'. The analysis of the participants’ low use of health apps indicates a perceived low control over their behaviour when using tracking technology. For example: ‘I know that there are apps for calorie counting, but I don’t have the patience for them’ and ‘I don’t remember the name of the app, but I tried to set up a profile, but it was very confusing and then I dropped it and deleted the app’.
In contrast, the coding of the participants’ motivation for activity tracking during the intervention identified some level of perceived increased control over their behaviour and their ability to influence their health behaviour. At the post-interviews, most participants expressed that they had become more aware of their physical activity level by wearing the activity tracker. A positive experience with the tracker was presented as support to set, keep and accomplish goals. The ability to track the daily development in the physical activity level motivated participants to reach their goals. This motivation was especially presented as an engagement in reaching goals. For example: ‘This is about hyping yourself when knowing that you are getting close to 10,000, as you may as well continue to reach the goal’ and ‘It’s very motivating to wear this [the activity tracker]. You set your target and then you can intend to beat it. And I have tried to do that every day’.
In relation to motivation, the participants presented that they particularly used the activity tracker’s mobile app (see Figure 2) to compare their activity level with others in the health intervention and to compete with each other. The group feature’s ranking list was positive for four of the participants. Notably, these four participants were at the top of the ranking list and they all expressed how competing against others motivated them while their individual use was less interesting: ‘The ranking list for the group is the feature that I use most. If it were only me and my data, it would not interest me, but competing against others is great fun. Now when the project stops it will become less interesting’.
However, most (18) participants expressed a decrease in their enthusiasm for the activity tracker. The following quote is a typical example from the data material of a fading interest: ‘In the beginning, I was very focused on how much I had walked and I actually synchronised every evening. I looked at the app and compared data from the day before. That’s how it worked for the first two weeks. Then later I kind of forgot to look up data’.
The coding of the participants perceived behavioural control from engaging with the activity tracker also identified negative effects from activity tracking. Two participants presented a total disinterest in the activity tracker and the mobile app. One of these participants explained: ‘I haven’t used the activity tracker at all, or the application. Only when the intervention required me to synchronize data’.
Overall, 12 participants presented that they experienced tracking as ‘controlling’ and as a burden having to keep up with goals set by the tracker. For example: ‘All the time it has been a small personal fight having to reach those steps’.
Two participants explained that the tracker intensified obsessive-compulsive disorders (OCD): ‘I have OCD and it means that I have several number systems and the activity tracker influences this in a negative way’ and ‘I was very dependent on knowing how many steps I had walked and whether it was a good or bad day, and what the reason for that was (…) It almost became an obsession using the wrist band’.
The daily or weekly goal set by the activity tracker was experienced as particularly demanding and counterproductive when it was impossible for the participants to reach it. For example: ‘I haven’t used it much to see how many steps I have walked because it could make me a little sad, when I saw that I had not walked as much as I would have liked to walk. This stressed me’.
These (18) participants considered it demotivating to share tracking data and compete with others. Their disinterest was primarily related to their low performance and an experience of being a failure. For example: ‘I am so behind in the ranking list that my fighting spirit is completely gone’ and ‘I don't use the ranking list because I have the lowest score’.
In contrast to the fading and negative engagement with the activity tracker the participants presented the Facebook group as the best digital support for exercise during the intervention. The Facebook group was only set up to support communication among participants. However, the participants presented that Facebook allowed them to communicate with fewer constraints (compared to data sharing and ranking lists supported by the activity tracker). Following others' achievements was presented as a primary motivation by the 14 participants who did not appreciate the activity tracker's ranking list. The participants posted encouragement, accomplishments, appreciation and apologies in the Facebook group. For example: ‘Thanks for a great power walk. You made my day' and ‘Sorry, I missed it today. Fell asleep and just woke up'. The participants who were most challenged to participate presented the Facebook group as an ability to participate from home. For example: ‘It was so nice that I could see the photos from the walk last Thursday. I just could not go out but I could follow the activities and it made me happy to be part of the activities in that way'.
In sum, the participants entered the intervention with low digital health experience. The activity tracker had a positive influence on the participants’ awareness of the daily activity level and four of the participants’ digital health engagement was especially positive in relation to their engagement in competition supported by the activity trackers’ mobile app. However, most participants experienced a decrease in their digital health engagement during the intervention and several participants expressed a negative experience of low control over their health behaviour. These participants presented Facebook as the best digital support for exercise because it allowed them to communicate with fewer constraints.
Synthesis: Contradictions in the digital health engagement
The participants experienced improved physical and mental health, their activity levels increased and they expressed a positive increased awareness about their physical activity on an every-day basis. However, the majority of the participants expressed a feeling of failure when unable to meet the goals set by the activity tracker, a fading interest in tracking and especially competition was counterproductive to most participants. The results of this study indicate contradicting dimensions in digital health engagement from the use of an activity tracker in a health intervention. Table 4 summarises these conflicting types of influence.
Table 4.
Three contradicting dimensions in digital health engagement from use of an activity tracker.
| Positive dimensions | Negative dimensions |
|---|---|
| Improved physical health and quality of life measures | Negative digital health experience – feeling of failure |
| Increased physical activity levels | Fading interest towards low and even negative digital health engagement |
| Individual and group competition increases motivation to exercise | Counterproductive competition aggravates mental health problems |
As presented by Ajzen,34 ambiguous results are not uncommon for research on health behaviour. Several factors tend to overlap or are difficult to classify. For example, some digital health behaviour is related to internal factors such as perceived cognitive overload (e.g. ‘it was very confusing and then I dropped it and deleted the app’), other examples are related to external factors such as perceived lack of time (e.g. ‘I spend too much time getting started and need to ask people for help’ and so on). Similarly, some behaviour starts with a perceived positive digital health engagement (e.g. ‘in the beginning, I was very focused on how much I had walked, and I actually synchronised every evening’), which develops into a perceived negative digital health engagement (e.g. ‘I was very dependent on knowing how many steps I had walked and whether it was a good or bad day, and what the reason for that was… It almost became an obsession using the wrist band’). In this light, the synthesis of the results emphasise the complexity related to activity tracking and digital health engagement and identify mental illness as an element that brings further complexity and ambiguity to conclusions on the use of activity tracking in health interventions.
Discussion
The technical performance of activity trackers is considered to be high and, in this study, none of the participants reported any technical problems that prevented them from using the tracker. The conceptual model for activity trackers is a goal-oriented tracking of steps on a daily basis and related opportunities for accumulating data to monitor own activity levels and compete with peers in groups. Our study showed that this conceptual model works well for users who are motivated by competition, which in this study was a minority (four participants out of 22). Whether this result is related to the included target group is unclear because research is dominated by studies focusing on the short-term effects on individuals who are already physically active.24 However, related research on IT-enhanced health for vulnerable citizens presents low use of health technology caused by lack of resources36 and negative perceptions of the benefits from technology use.37 This finding questions the perspective that 10,000 steps per day is a positive health goal15,16 and suggests a need to include vulnerable and marginalised people in future research on the design and use of health IT to expand existing technology to a broader audience in need of health support.8,10,38
The quantitative monitoring of the participants through the cycling test and a quality of life test before and after the health intervention demonstrates a positive health effect from the intervention. Although the activity tracker is only one element in the intervention (see Table 2), these health results support related research demonstrating that activity trackers have a positive effect on participants’ activity levels and health during the health interventions.16,23 However, from the qualitative data, it is not possible to identify a positive link or correlation between the participants’ improved health condition and experienced digital health engagement. Hence, these findings support the theory emphasising that perceived behavioural control is a central component to investigations of behaviour.34 Overall, 18 participants presented a fading digital health interest and even counterproductive and negative experience from activity tracking. This finding indicates that activity trackers and mental vulnerability are not a good combination and thus call for future research to understand better how to develop and integrate tracking technology into the delivery of healthcare.39 Even though the participants all expressed a wish to increase their physical activity level prior to recruitment and were enthusiastic about wearing an activity tracker during the intervention, the activity tracker was not seen as a positive supporting technology for the majority of the participants’ everyday health management. Related work on the long-term use of fitness apps indicates that the motivation to exercise using fitness apps typically decreases over time25,40 and identify sustained engagement as a key challenge for design of tracking technology.41 In addition, related work on tracking technology and vulnerable patients indicates a general difficulty related to converting health information into health strategies in daily living.42
The contradictions in the results support related work highlighting the complexity of information practice for people living with and managing everyday health issues.43–45 The participants in this study entered the health intervention with no, ad-hoc or resistive digital health experience. All participants were challenged but motivated to participate and wear the activity tracker. The results must be understood on this basis, which to some extent brings perspective to the identified ambiguity of tracking among the participants. However, the findings highlight the complexity related to health tracking and the socio-technical challenges faced when combining mental illness, bodily experience, self-tracking technology and technology-mediated competition. Health IT, including activity trackers as explored in this study, is a node in a complex socio-technical system and the ambiguous results from this study indicate that research investigating activity trackers’ specific effects on health are too narrow and fail to understand important contextual aspects for digital health engagement.
Limitations and future research
Participation in the health intervention was facilitated by exercise activities twice a week in addition to using the activity tracker. Naturally, this influenced an increase in the participants’ activity levels, which was below two hours in total per week prior to the intervention (see recruitment section). For this reason, it cannot be concluded that the activity tracker alone caused an increase in the participants’ activity and fitness levels. Digital health interventions are intrusive, and the effect of the activity tracker is influenced by several other factors in the intervention, which are important to highlight as a context for understanding the results. A Hawthorne effect46 is observable in this study, where all participants found it positive to be included in a research project, to experiment with an activity tracker and to participate in exercise activities and receive special attention during health checks and the intervention. As most participants were lonely prior to the intervention, all activities and attention they received during the intervention is likely to have affected their quality of life, just as the interventions’ focus on health is likely (and intended) to have had a learning effect that made the participants adjust and improve their daily health. Consequently, our study supports related work emphasising that the health behaviour associated with activity trackers is interwoven in complex contextual factors and the results highlight the danger of making too simple assumptions related to the effect of tracking technology.20,27,28,30,31
Also, the number of participants in this pilot study (n = 22) is a limitation that calls for future research on a larger scale, including a control group to investigate further the complex factors related to vulnerable users and activity trackers.
Related research supports the identified contradicting dimensions related to self-tracking and stresses the importance of not understanding and using activity trackers as ‘rationalising forces’ but as ‘an ongoing negotiation of the boundaries and meanings of self within an anxious alliance of knowledge, bodies, devices, and data’.29 This evidence that our identified ambiguity of using an activity tracker is not specific for vulnerable people. It highlights the resources that self-tracking demands from its users for reflections and ‘ongoing negotiation’ and indicates why this digital demand was overwhelming and even negative for the most vulnerable participants in this study, because they were low on resources. In general, this study presents a need for future research and development of the use of activity trackers and health IT for vulnerable users. National studies from Denmark, where this study was conducted, shows that people with mental illness have a high interest in health improvement, but that a change in lifestyle is a major challenge.47 Consequently, policies are made for developing and investigating opportunities for supporting vulnerable people in improving their health, including exercise. However, there are no current policies or experiences with the use of technology that support vulnerable people in exercise. The findings from this study indicate that use of activity trackers in health interventions with vulnerable users require close supervision to overcome a fade in interest, but especially to prevent and counter negative health engagement. This outcome calls for further studies to understand and guide the development and use of tracking technology in healthcare delivery.39
Prospects for PGD – in this case, number of steps walked – could, if shared with the GP, be used during consultations to support patients’ psychological well-being. Future research on how to expand activity tracking from a rather personal technology to a technology supporting cooperation between health professionals and patients is worth pursuing, although this raises several issues related to data protection and consumer health technology. Several of the difficulties experienced by the participants in this study were related to their health and life challenges. Conversations with health professionals about activity data can expand the limited information window provided to health professionals today in clinic consultations and support conversations about how the patient is developing and coping with their health on a daily basis.
Also notable is that the participants enjoyed being in a group with peers during the intervention, although several found the competition feature in the tracker difficult to cope with. The Facebook group was presented as a positive digital health experience and future research could benefit from design alternatives to support health cooperation among patients and citizens in general. Recent research on collective health has presented interesting directions for such design alternatives, which bring attention to social health relations and opportunities for design of IT enhanced capacity building of health.48,49 The results from this study have pointed out a general problem related to the conceptual model of activity trackers and vulnerable users. In this light, design alternatives for health IT are worth pursuing in future research.
Conclusions
This pilot study on the influence of activity tracking has identified contradicting dimensions related to digital health engagement for the target group of young adults diagnosed with anxiety and depression disorders. The findings include positive improvement of physical and mental health during the digital health intervention but a fading digital health engagement and counterproductive negative experience especially from competition. The study indicates a potential for using activity trackers as part of treatment in general practice. However, the ambiguous results identify a need for (1) developing strategies for health professionals to provide supervised use of activity trackers and support the target groups’ abilities to convert health information about physical activity into positive health strategies; and (2) designing alternatives for health promoting IT targeted users who face challenges and need motivation beyond self-tracking and competition.
Acknowledgement
We thank all participants and partners in the study.
Notes
a. Paired two-sided t-test: t = 3.52, n = 18, P = 0.0026.
b. Paired two-sided t-test: t = −2.12, n = 21, P = 0.047.
Contributorship
All three authors have made substantial contributions to the study design, data analysis and drafting of this article.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
The study was approved by the Danish Data Protection Agency, under administration by the office for Grants and Contracts at Aalborg University (registration number: 2015-851/10-0061). All participants gave their oral and written consent. The study was also submitted to the Regional Research Ethics Committee in North Denmark, who found that according to Danish laws the study did not need their approval.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the Danish foundation TrygFonden.
Guarantor
Principal Investigator Anne Marie Kanstrup.
References
- 1.Walker S. Wearable Technology – Market Assessment. An IHS Whitepaper, London, UK: IHS Electronics & Media, 2015. [Google Scholar]
- 2.Chung CF, Dew K, Cole A, Zia J, Fogarty J, Kientz JA and Munson SA. Boundary negotiating artifacts in personal informatics: Patient-provider collaboration with patient-generated data. In: CSCW’16 Proceedings of the 19th ACM Conference on Computer-Supported Cooperative Work & Social Computing, San Francisco, California, USA, 27 February–2 March 2016. New York: ACM Press, 2016, pp. 770–786. [DOI] [PMC free article] [PubMed]
- 3.Zhu H, Colgan J, Reddy M, Choe EK. Sharing patient-generated data in clinical practices: An interview study. In: AMIA Annual Symposium Proceedings, 2016, pp. 1303–1312. [PMC free article] [PubMed]
- 4.Almalki M, Gray K, Sanchez FM. The use of self-quantification systems for personal health information: Big data management activities and prospects. Health Inform Sci Syst 2015; 3: 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Swan M. Sensor Mania! The Internet of things, wearable computing, objective metrics, and the quantified self 2.0. J Sens Actuator Netw 2012; 1: 217–253. [Google Scholar]
- 6.O’Connor S, Hanlon P, O’Donelle CA, Garcia S, Glanville J, Mair FS. Understanding factors affecting patient and public engagement and recruitment to digital health interventions: A systematic review of qualitative studies. BMC Med Inf Decis Making 2016; 16: 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abril EP. Tracking myself: Assessing the contribution of mobile technologies for self-trackers of weight, diet, or exercise. J Health Commun 2016; 21: 638–646. [DOI] [PubMed] [Google Scholar]
- 8.Petersen LS and Bertelsen P. Equality challenges in the use of eHealth – Selected results from a Danish Citizens survey. In: Medinfo2017 Proceedings of the 16th World Congress on Medical and Health Informatics, Hangzhou, China, 21–25 August 2017. Amsterdam: IOS Press. [PubMed]
- 9.Seifert A, Schlomann A, Rietz C, Schelling HR. The use of mobile devices for physical activity tracking in older adults’ everyday life. Digital Health 2017; 3: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Showel C, Turner P. The PLU problem: Are we designing personal eHealth for people like us? Stud Health Tech Informat 2013; 183: 276–280. [PubMed] [Google Scholar]
- 11.World Health Organization.. Information sheet: Premature death among people with severe mental disorders, Geneva, Switzerland: WHO, 2016. [Google Scholar]
- 12.MacKean PR, Stewart M, Maddocks HL. Psychosocial diagnoses occurring after patients present with fatigue. Can Fam Physician 2016; 62: e465–e472. [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenberg D, Kadokura EA, Bouldin ED, Miyawaki CE, Higano CS and Hartzler AL. Acceptability of Fitbit for physical activity tracking within clinical care among men with prostate cancer. In: AMIA Annual Symposium Proceedings, 2016, pp. 1050–1059. [PMC free article] [PubMed]
- 14.Riel H, Kalstrup PM, Madsen NK, Pederen ES, Rathleff CR, Pape-Haugaard LB, et al. Comparison between Mother, ActiGraph wGT3X-BT, and a hand tally for measuring steps at various walking speeds under controlled conditions. Peer J 2016; 4: e2799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tudor-Locke C, Hatano Y, Pangrazi R, Kang M. Re-visiting “how many steps are enough?”. Med Sci Sports Exerc 2018; 40: 537–543. [DOI] [PubMed] [Google Scholar]
- 16.Kang M, Marshall SJ, Barreira TV, Lee JO. Effects of pedometer-based physical activity interventions. Res Q Exerc Sport 2009; 80: 648–655. [DOI] [PubMed] [Google Scholar]
- 17.Kim KK, Logan HC, Young E, Sabee CM. Youth-centered design and usage results of the iN Touch mobile self-management program for overweight/obesity. Pers Ubiquit Comput 2015; 19: 59–68. [Google Scholar]
- 18.Fausset CB, Mitxner TL, Price CE, Jones BD, Fain WB and Rogers WA. Older adults’ use of and attitudes toward activity monitoring technology. In: Proceedings of the Human Factors and Ergonomic Society 57th Annual Meeting, 2013, pp. 1683–1687. [DOI] [PMC free article] [PubMed]
- 19.Mercer K, Li M, Giangregorio L, Burns C, Grindrod K. Behaviour change techniques present in wearable activity trackers: A critical analysis. JMIR Mhealth Uhealth 2016; 4: e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schwennesen N. When self-tracking enters physical rehabilitation: From ‘pushed’ self-tracking to ongoing affective encounters in arrangements of care. Digital Health 2017; 3: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones J, Wu H, Patel J, Kasthurirathne S, Thai N and Mukherjee S. An evaluation of activity trackers for monitoring Parkinson’s disease patient outcomes. In: AMIA Annual Symposium Proceedings, 2016, p. 1451.
- 22.Shaw R, Fenwich E, Baker G, McAdam C, Fitzsimons C, Mutrie N. Pedometers cost buttons: The feasibility of implementing a pedometer-based walking programme within the community. BMC Public Health 2011; 11: 200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brevata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R, et al. Using pedometers to increase physical activity and improve health: A systematic review. JAMA 2007; 298: 2296–2304. [DOI] [PubMed] [Google Scholar]
- 24.Dallinga JM, Mennes M, Alpay L, Bijwaard H, De la Faille-Deutekom MB. App use, physical activity and healthy lifestyle: A cross-sectional study. BMC Public Health 2015; 15: 833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hermann LK, Kim J. The fitness of apps: A theory-based examination of mobile fitness app usage over 5 months. mHealth 2017; 3(2): DOI: 10.21037/mhealth.2017.01.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meyer J, Wasmann M, Heuten W, Ali AE and Boll SCJ. Identification and classification of usage patterns in long-term activity tracking. In: CHI 2017 Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems. Denver, CO, USA, 6–11 May 2017. New York: ACM Press, 2017, pp. 667–678.
- 27.Patel M and O’Kane AA. Context influences on the use and non-use of digital technology while exercising at the gym. In: CHI’15 Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems, Seoul, Republic of Korea, 18–23 April 2015. New York: ACM Press, 2015, pp. 2923–2932.
- 28.Rooksby J, Rost M, Morrison A and Chalmers M. Personal tracking as lived informatics. In: CHI’14 Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Toronto, Ontario, Canada, 26 April–1 May 2014. New York: ACM Press, 2014, pp. 1163–1172.
- 29.Williams K. An anxious alliance. In: Proceedings of The Fifth Decennial Aarhus Conference on Critical Alternatives, 17–21 August 2015. Copenhagen, Denmark: AARHUS University, 2015, pp. 121–131.
- 30.Clawson J, Pater JA, Miller AD, Mynatt ED and Mamykina L. No longer wearing: Investigating the abandonment of personal health-tracking technologies on Craigslist. In: UbiComp’15 Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Osaka, Japan, 7–11 September 2015. New York: ACM Press, 2015, pp. 647–658.
- 31.Storni C. Multiple forms of appropriation in self-monitoring technology: Reflections on the role of evaluation in future self-care. Intl J Human-Comput Interact 2010; 26: 537–556. [Google Scholar]
- 32.Åstrand P. Ergometri konditionsprov. Monark Exercise AB. 1964.
- 33.Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 well-being index: A systematic review of the literature. Psychother Psychosom 2015; 84: 167–176. [DOI] [PubMed] [Google Scholar]
- 34.Ajzen I. Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. J Appl Soc Psychol 2002; 32: 665–683. [Google Scholar]
- 35.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 36.Atkinson NL, Billing AS, Desmond SM, Gold RS, Tournas-Hardt A. Assessment of the nutrition and physical activity education needs of low-income, rural mothers: Can technology play a role? J Community Health 2007; 32: 245–267. [DOI] [PubMed] [Google Scholar]
- 37.Jimison H, Gorman P, Woods S, Nygren P, Walker M, Norris S, et al. Barriers and drivers of health information technology use for the elderly, chronically ill, and undeserved. Evid Rep Technol Assess 2008; 175: Report No.: 09-E004. [PMC free article] [PubMed] [Google Scholar]
- 38.Kanstrup AM and Bertelsen P. Bringing new voices to design of exercise technology: Participatory design with vulnerable young adults. In: PDC’16 Proceedings of the 14th Participatory Design Conference Volume 1, Aarhus, Denmark, 15–19 August 2016. New York: ACM Press 2016, pp. 121–130.
- 39.Morgan H. ‘Pushed’ self-tracking using digital technologies for chronic health condition management: A critical interpretive synthesis. Digital Health 2016; 2: 1–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Harrison D, Marshall P, Bianchi-Berthouze N and Bird J. Activity tracking: Barriers, workarounds and customisation. In: UbiComp’15. Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Osaka, Japan, 7–11 September 2015. New York: ACM Press, 2015, pp. 617–621.
- 41.Gouveia R, Karapanos E and Hassenzahl M. How do we engage with activity trackers? A longitudinal study of habito. In: UbiComp’15. Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Osaka, Japan, 7–11 September 2015. New York: ACM Press, 2015, pp. 1305–1316.
- 42.Johansen SK and Kanstrup AM. Expanding the locus of control: Design of a mobile quantified self-tracking application for whiplash patients. In: NordiCHI’16 Proceedings of the 9th Nordic Conference on Human-Computer Interaction, Gothenburg, Sweden, 23–27 October 2016. New York: ACM Press, 2016, article no. 59.
- 43.Kanstrup AM, Rotger-Griful S, Laplante-Lévesque A and Nielsen AC. Designing connections for hearing rehabilitation: Exploring future client journeys with elderly hearing aid users, relatives and healthcare providers. In: DIS’17 Proceedings of the 2017 Conference on Designing Interactive Systems, Edinburgh, UK, 10–14 June 2017. New York: ACM Press, 2017, pp. 1153–1163.
- 44.Moen A, Brennan PF. Health@Home. The work of health information management in the household (HIMH): Implications for consumer health informatics (CHI) innovations. J Am Med Inform Assoc 2005; 12: 648–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.O’Kane A, Park SY, Mentis H, Blandford A, Chen Y. Turning to Peers. Integrating understanding of self, the condition, and others’ experiences in making sense of complex chronic conditions. CSCW 2016; 25: 477–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Parsons HM. What happened at Hawthorne? Science 1974; 183: 911–932. [DOI] [PubMed] [Google Scholar]
- 47.Sundhedsstyrelsen.. Struktur på sundheden – inspiration til sundhedsindsatser til borgere med psykiske lidelser, Copenhagen, Denmark: Sundhedsstyrelsen, 2014. [Google Scholar]
- 48.Parker AG, Grinter RE. Collectivistic health promotion tools: Accounting for the relationship between culture, food and nutrition. Int J Hum Comput Stud 2014; 72: 185–206. [Google Scholar]
- 49.Kanstrup AM, Bertelsen P, Nunez HC, Svarre T, Stage J. MOVE: a mobile app designed for social health relations in residential areas. Stud Health Technol Informat 2018; 247: 496–500. [PubMed] [Google Scholar]