Abstract
Background
The impact of employee health on productivity in the workplace is generally evidenced through absenteeism and presenteeism. Multicomponent worksite health programmes, with significant online elements, have gained in popularity over the last two decades, due in part to their scalability and low cost of implementation. However, little is known about the impact of digital-only interventions on health-related outcomes in employee groups. The aim of this systematic review was to assess the impact of pure digital health interventions in the workplace on health-related outcomes.
Methods
Multiple databases, including MEDLINE, EMBASE, PubMed and PsycINFO, were used to review the literature using PRISMA guidelines.
Results
Of 1345 records screened, 22 randomized controlled trial studies were found to be eligible. Although there was a high level of heterogeneity across these studies, significant improvements were found for a broad range of outcomes such as sleep, mental health, sedentary behaviours and physical activity levels. Standardized measures were not always used to quantify intervention impact. All but one study resulted in at least one significantly improved health-related outcome, but attrition rates ranged widely, suggesting sustaining engagement was an issue. Risk of bias assessment was low for one-third of the studies and unclear for the remaining ones.
Conclusions
This review found modest evidence that digital-only interventions have a positive impact on health-related outcomes in the workplace. High heterogeneity impacted the ability to confirm what interventions might work best for which health outcomes, although less complex health outcomes appeared to be more likely to be impacted. A focus on engagement along with the use of standardized measures and reporting of active intervention components would be helpful in future evaluations.
Keywords: Digital health, workplace interventions, internet-based interventions, occupational health, systematic review, e-health, health promotion, workplace well-being
Introduction
Over the past two decades, the understanding of how employee health impacts productivity has advanced substantially.1–4 There is now a large body of evidence linking financial costs to employee health risks. This relationship is mainly defined by a loss of productivity driven by absenteeism and presenteeism. Absenteeism, defined as time away from work due to illness or disability, is a simple debt to calculate and has long been associated with lowered productivity.5–7 Presenteeism is slightly more complex in that it refers to time spent at work with decreased levels of productivity, which is often harder to measure. This lack of workplace performance can be due to mental or physical health issues, and it is often underestimated by organizations.8 Both absenteeism and presenteeism are strongly correlated with unhealthy employee behaviours and status. Examples of these can include poor management of health conditions, obesity, insomnia, lack of physical activity or depression, all of which have been shown to have a detrimental economic impact on organizations.3,9–12
In addition, research has shown that many of the unhealthy lifestyle behaviours linked to reduced productivity are highly modifiable. Studies implementing interventions in the workplace designed specifically to address these behaviours have frequently shown health status improvements and consequent reductions in absenteeism and presenteeism in participants.13–17 The greater understanding of the causal link between employee health status and work performance metrics has resulted in a steady and sustained growth in employee focused health and well-being programmes. Once considered a ‘nice to have’ benefit, these programmes are now key to many organizations’ global investment and people management strategies. It has become commonplace for large organizations to conduct regular employee health risk assessments (HRAs) and to offer health promotion programmes to employees to address identified health issues. These programmes vary in length, composition and intensity, but are all designed to assess and promote an increase in healthy lifestyle behaviours, such as proactive stress management, better nutrition and greater physical activity.
The research literature suggests that the most successful approach to addressing employee health issues is through a multicomponent design.13–15,17–19 Multicomponent health interventions combine support from various sources such as health professionals, employee support groups, telephonic coaching programmes and most recently, web and mobile device-delivered applications. The advancement of digital technology over the last 20 years has penetrated almost every aspect of modern life, and health management is no exception. Digital health interventions have become increasingly popular within the health industry due to the ease with which they can be implemented and scaled to large and often dispersed populations. In addition, such an approach may be more cost effective compared with more traditional personnel-dependent programmes. Accessible through any internet-connected device, many organizations are using digital interventions to leverage support for the health and well-being of their employees.20
Despite their popularity, one aspect that is not well understood about workplace health promotion programmes in the digital age is how much the digital element can itself, or as part of a multicomponent intervention, contribute to the overall programme efficacy and improved health outcomes. To address this question and the gap in the literature we conducted a systematic review of current peer-reviewed research of workplace-based ‘digital only’ interventions, which we hope will be a valuable resource for researchers and programme developers alike.
The main objective of this review was to assess the impact of digital health interventions in the workplace on health-related outcomes. This review implemented a conservative definition of digital interventions to exclude studies that included any form of employee support that was non-digital.
Methods
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement21 and is registered with PROSPERO (registration: CRD42017059621).22
Eligibility criteria
Studies that were randomized controlled trials (RCTs), including pilots, reported in English, assessing the impact of digital health interventions in the workplace, with at least one primary outcome being health related were included. Participants recruited were eligible if they were aged 18 years or above and were employees. Digital interventions were considered eligible if they delivered through the use of a computer, tablet, smartphone or email, either as a website, app or downloadable software.
Digital interventions, which included further support such as meetings, health counselling or direct feedback from a health professional or coach (even those delivered digitally), were considered not purely digital and therefore were not included, as it was not possible to discern the impact of the digital component. The exception to this was the introduction of the intervention to participants or follow-up reminder for data collection, which were often conducted with human support for research purposes. Finally, interventions incorporating the use of wearable technology were not considered eligible as self-monitoring wearable devices can be considered a separate intervention on their own.
There was no limit to length or duration of interventions included within this review and outcomes were any health-related measure, including those quantifying physical or mental health, illness symptoms and health-related lifestyle behaviours.
Search strategy
Electronic databases including MEDLINE, EMBASE, PubMed, PsycINFO and CINAHL were searched for studies published up to and including December 2017. The search strategy was based on the PICO (population, intervention, comparison and outcome) strategy,23 with the language restriction of English. Reference lists of eligible studies were screened for further papers meeting the inclusion criteria. Databases were searched using a combination of the key words such as: ‘work*’, ‘occupational’, ‘digital’, ‘web’, ‘internet’, ‘apps’, ‘well-being’, ‘health’, ‘intervention’ and ‘treatment’. Terms were based on MeSH indexing as well as free text terms (see supplementary File 1 for a full list of search terms and combinations).
Data collection and extraction
Using the predefined criteria, all searches were conducted by the first author (AH) based on abstract and title. Results were then screened independently by two authors (AH and PM) who rated the eligibility of the records to confirm relevant papers. Full texts for papers rated as relevant or potentially relevant were then retrieved and reviewed by two authors (AH and PM) to determine final eligibility. Any studies that were disagreed upon were discussed, and a consensus was reached for all articles included.
A data extraction of the following fields was then used to summarize the key points of the eligible studies: first author name, publication date, country, design and aim, participant characteristics (including age, gender and employment detail), type of intervention, type of comparison, main outcome measures and results (i.e. effects of interventions on outcomes). The extraction was conducted by AH and verified by SJ, JC and PM.
Assessment of quality
Methodological quality of the included studies was assessed for those with an RCT design using the Cochrane Handbook for Systematic Reviews of Interventions.24 The handbook recommends using the Cochrane risk of bias tool25 to allocate a risk of bias classification for each study. Grading with this approach was dependent on certain issues affecting bias such as reporting of randomization, blinding and allocation concealment and whether outcome measures were fully reported. Each study was reviewed by two authors (AH and PM), given an overall risk of bias grade of low, unclear or high and then discussed for consensus if there was disagreement in grading.
Analysis
Meta-analysis was not considered a feasible option based on the included studies, as there was a lack of the required homogeneity across outcome measures.24 A narrative approach was therefore used to summarize findings.
Results
Selection of studies
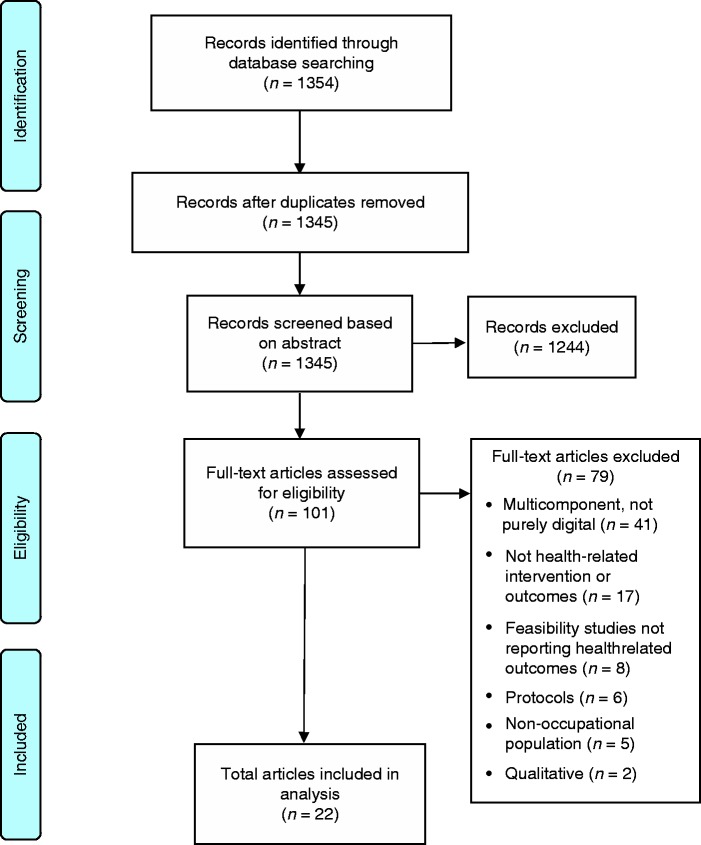
The search identified 1354 papers and these articles were then screened using the inclusion criteria as illustrated by the PRISMA flow diagram21 below (see Figure 1) by two authors (AH and PM). Duplicates were removed, and initial screening based on title and abstract resulted in 101 articles deemed eligible. Full-text articles for these records were then obtained and reviewed by two authors (AH and PM). From this process, a further 79 articles were excluded. The majority (n = 41) were excluded because they were multicomponent in nature; 17 studies were found not to be evaluating health-related outcomes or interventions. Eight were feasibility studies that did not report on health-related outcomes, six were protocol articles, five studies did not use an occupational population and two studies were qualitative. No additional studies were found by hand searches and the final total of eligible studies was 22.
Figure 1.
PRISMA flow diagram illustrating screening of studies.
Study characteristics
A total of 22 studies were included in this review up to and including December 2017. A summary of study characteristics can be seen in Table 1 and a summary of intervention characteristics can be seen in Table 2.
Table 1.
Overview of included studies.
| First author, date (ref) country | Design/aim | Participants | Intervention and comparator/control | Outcome measures | Findings | Risk of biasc |
|---|---|---|---|---|---|---|
| Bolier, 2014 (26) Netherlands | RCTa To examine the effectiveness of an online health module targeting positive mental health | 366 nurses, allied health professionals Mean age 40.0 yrs ± 11.9 yrs 80% female | (a) Online health screening and personalized feedback module with access to online self-help interventions (b) Online health screening as waitlist control | Mental Health Continuum – Short Form, Utrecht Work Engagement Scale, WHO-5 Well-being Indexb, Brief Symptom Inventory (anxiety and depression sub-scales) | Positive mental health was significantly enhanced in the intervention group compared with the control group There was also a small but significant effect for work engagement in the intervention group | L |
| Bostock, 2016 (27) UK | RCT To evaluate a digital cognitive behavioural therapy intervention for insomnia | 270 self-reported insomniacs from a global ‘Fortune 500’ company Mean age 33.6 yrs ± 6.0 yrs 33% female | (a) dCBT (digital cognitive behavioural therapy) for insomnia including assessment, tailored feedback and online support (b) Online assessment as waitlist control | Sleep Condition Indicator, Work Productivity and Activity Impairment questionnaire | The dCBT group had significantly higher Sleep Condition Indicator scores than the control Before and after analysis of the dCBT group found significant improvements in presenteeism | L |
| Brendryen, 2017 (28) Norway | Pilot RCT To pilot the effectiveness of a previously established internet-based alcohol intervention, within a workplace setting | 80 employees from four organizations: a group of public hospitals, a county, a municipality department, a consulting company Mean age 43.0 yrs ± 11.0 yrs 52% female | (a) Web-based, intensive self-help alcohol programme with SMS support (b) e-booklet with general alcohol-related educational information and advice | Total weekly alcohol consumption as reported using a scale ranging from 0 to 10 drinks per day | Findings were inconclusive regarding the effectiveness of the intensive intervention in comparison to the brief due to recruitment issues but of survey responders, the intensive intervention group drank 5–6 less drinks a week than the brief intervention group | L |
| Cook, 2007 (29) USA | RCT To evaluate the effectiveness of a web-based health programme designed to improve diet, stress and physical activity | 419 employees from a human resources company 40.0 yrs ± 11.9 yrs 80% female | (a) Web-based health programme with substantial information and guidance on the major health promotion and wellness topics (b) Printed materials consisting of five commercially available booklets on eating, weight management, stress, fitness and alcohol | 21 online health questionnaires covering diet, weight, stress, coping, exercise and motivation assessment | The web-based group scored significantly higher than the printed materials group in areas of diet and nutrition although both groups showed improvements on most dietary measures No significant differences were found between the two groups on measures of stress or physical activity although both groups showed improvements | U |
| Cook, 2015 (30) USA | RCT To evaluate the effectiveness of a web-based health programme aimed specifically at workers 50 years and older | 278 employees from a large global IT company 67% were aged 50–68 yrs 33% female | (a) Web-based health programme with major health promotion topics of healthy ageing, diet, physical activity, stress management and tobacco use (b) Waitlist control | 16 online health questionnaires assessing diet, weight, stress, coping, exercise, motivation, tobacco use and beliefs about ageing | The programme group scored significantly better than the control group on diet, healthy eating and exercise There were no significant programme effects found on measures of stress or ageing beliefs | U |
| Deitz, 2014 (31) USA | RCT To examine whether a web-based programme reduces cardiovascular (CV) risk behaviours | 210 hospital employees with at least one known CV risk factor Range 21–72 yrs 86% female | (a) Web-based, interactive, Heart Healthy programme with tailored feedback designed to reduce cardiovascular risk reduction behaviour (b) Waitlist control | 13 online questionnaires and surveys covering CV risk attitudes and behaviour, blood pressure, heart rate, BMId | The intervention group showed significant improvements in diet, exercise, self-efficacy, stress and mood measures | U |
| Doumas, 2007 (32) USA | RCT To evaluate the efficacy of a web-based programme aimed at reducing high-risk alcohol behaviour in young adults | 124 human resources employees, aged 18–24 yrs 73% female | (a) Web-based programme with personalized drinking feedback designed to reduce high-risk drinking (b) Web-based programme with personalized drinking feedback designed to reduce high-risk drinking with 15-min motivational interview in person (c) Waitlist control | Measures of alcohol consumption: drinking quantity, peak consumption, frequency of drinking to intoxication and binge drinking, Modified Daily Drinking Questionnaire | When both interventions were combined and compared with the control group, significantly lower levels of drinking were found in the intervention group, especially in high-risk individuals The web-based alone intervention also had significantly lower drinking levels compared with the control group but there was no difference found between the web-based with interview intervention when compared with the control | U |
| Griffiths, 2016 (33) Australia | RCT To assess the effectiveness of an online mental health programme | 507 government employees Mean age 44.5 yrs ± 11.4 yrs 74% female | (a) Online educational programme focusing on depression and anxiety (b) Waitlist control | Depression Literacy Scale, Generalized Anxiety Literacy Scale, Depression Stigma Scale – Personal subscale, Generalized Anxiety Stigma scale – Personal subscale, Generalized Help-Seeking Questionnaire, Attitudes Towards Seeking Professional Psychological Help Scale-Short Form, help-seeking behaviour | The intervention group showed significantly greater improvements in depression and anxiety literacy, and a greater reduction of depression and anxiety personal stigma, compared with the control | U |
| Irvine, 2011 (34) USA | RCT To test a web-based intervention designed to improve physical activity of sedentary workers | 221 employees from a large manufacturing plant Mean age 45.0 yrs ± 9.7 yrs 42% female | (a) Web-based tool for health promotion and stress management including classical stress management exercises and a chat (b) Web-based tool for health promotion and stress management with no extra exercises or chat | Current Exercise Status Scale, study specific measures of depression, anxiety, stage of change, attitudes and perceived knowledge, behavioural self-efficacy and intention, barriers to PA and PA motivation | The intervention group differed significantly from the control group on 11 outcomes Large effect sizes were found for PA status and knowledge, attitudes and behavioural intention Medium effect sizes were found for perceived barriers, depressive symptoms, motivation and self-efficacy | U |
| Ketelaar, 2014 (35) Netherlands | RCT To evaluate an e-mental health (EMH) programme aimed at improving work function and mental health | 128 nurses and allied health professionals Mean age 49.0 yrs ± 12.0 yrs 77% female | (a) Website designed to offer tailored education, support and guidance for PA (b) Waitlist control | Nurses Work Functioning Questionnaire, Four-Dimensional Symptoms Questionnaire, Dutch Questionnaire on the Experience and Evaluation of Work | Significant improvements were found on work functioning and work-related fatigue for the intervention group Work functioning improved in 30% of participants with a small effect on stress found in the participants who had logged onto the EMH intervention | U |
| Khadjesar, 2014 (36) UK | RCT To determine the effectiveness of an online alcohol reduction programme as part of an online employee health check | 1066 employees in a large organization Median age 48.0 yrs 25% female | (a) Online health check with feedback on all health behaviours including specific risk advice regarding alcohol (b) Waitlist control group which received the same feedback minus alcohol advice | Online health check including health behaviours (e.g. smoking status, fruit and vegetable consumption), Alcohol Use Disorders Identification Test, EQ-5De | There was no significant difference in past week alcohol consumption between groups or on the scores of the Alcohol Use Disorders Identification Test or EQ-5D at follow-up | U |
| Mainsbridge, 2014 (37) Australia | RCT To evaluate the effect of an e-health intervention on mean arterial pressure (MAP) through reducing prolonged sitting | 29 desk-based employees from a government agency Mean age 39.5 yrs ± 11.0 yrs 83% female | (a) Interactive e-health programme designed to encourage breaks in long bouts of sitting by standing up to engage in brief physical activity with screen prompts every 45 min (b) Waitlist control | Blood pressure, stages of change questionnaire, Short Form-36 | The intervention group had a significantly decreased mean MAP after a 13-week period compared with the control group | L |
| Matano, 2006 (38) USA | Pilot RCT To pilot a web-based intervention for alcohol consumption reduction | 145 employees from a Silicon Valley work site identified as low or moderate risk for alcohol abuse Mean age 39.9 yrs ± 11.3 yrs 78% female | (a) Website providing general information about alcohol use and its effects along with full individualized feedback based on individual risk for alcohol abuse (b) Website providing general information about alcohol use and its effects with no individualized feedback | CAGE questionnaire, Alcohol Use Disorders Identification Test | Those who were classified moderate-risk in the intervention group had a significant reduction in frequency of beer bingeing Those who were classified low-risk in the intervention group had a significant reduction in frequency of beer binges and hard liquor binges | U |
| Pedersen, 2014 (39) Australia | RCT To examine the effectiveness of an e-health intervention designed to improve workday energy expenditure for desk-based employees | 34 desk-based police employees from several sectors Mean age 39.7 yrs ± 11.0 yrs 76% female | (a) e-health software program designed to reduce sitting time by prompting user on their computer to be active (stand, move, stretch) every 45 min (b) Waitlist control | Study-specific questionnaire based on the Occupational Sitting and Physical Activity Questionnaire and the Occupational Physical Activity Questionnaire | The intervention group significantly increased calories expended during the work day compared with the control group, which decreased | U |
| Querstret, 2016 (40) UK | RCT To investigate how an online mindfulness course influences occupational health | 118 employees from various organizations Mean age 40.7 yrs ± 10.5 yrs 81% female | (a) Online mindfulness course based on traditional mindfulness based stress reduction course (b) Waitlist control | The Work-Related Rumination Questionnaire, Occupational Fatigue Exhaustion Recovery scale, The Pittsburgh Sleep Quality Index, Five Facet Mindfulness Questionnaire Short form | The intervention group reported significantly improved levels of rumination, problem solving, pondering, fatigue and sleep quality compared with the control group | L |
| Schell, 2008 (41) Sweden | RCT To evaluate the effect of a web-based stress programme on back, neck and shoulder pain and pain-related stress | 226 news media employees Mean age 44.0 yrs Age range 23–61 yrs 45% female | (a) Web-based tool for health promotion and stress management including classical stress management exercises and a chat (intervention group) (b) Web-based tool for health promotion and stress management with no extra exercises or chat (reference group) (c) Control with no intervention | Study-specific self-reported pain and pain-related stress questionnaire | There were no significant differences between groups at any point Some significant differences were found within groups, but they were inconsistent and varied according to pain localization | L |
| Shimazu, 2005 (42) Japan | RCT To examine the effects of a web-based programme on self-efficacy, problem-solving behaviour, stress responses and job satisfaction | 212 white collar employees Mean age 43.0 yrs ± 11.4 yrs 28% female | (a) Online self-paced employee programme aimed at enhancing coping abilities (b) Waitlist control | The Self-efficacy scale, study-specific problem-solving behaviour measure, Brief Job Stress Questionnaire, Single item job satisfaction measure | Job satisfaction changes pre to post intervention were marginal but significant compared with the control group | U |
| Solenhill, 2016 (43) Sweden | RCT To evaluate the effect of a web-based health programme with or without the option of telephone coaching | 981 transport employees Mean age 44.0 yrs ± 10.2 yrs 23% female | (a) Health risk assessment and tailored feedback (b) Health risk assessment and tailored feedback and telephone coaching option (c) Health assessment with no feedback | BMI, Alcohol Use Disorders Identification Test, Karolinska Sleep Questionnaire, self-reported activity levels, usage of telephone helplines, healthy eating behaviours, self-perceived health, motivation to change ratings | No significant differences were found between any groups in relation to reported health behaviours At baseline, the intervention groups reported significantly higher motivation to improve dietary and physical activity behaviour compared with the control | U |
| Umanodan, 2014 (44) Japan | Cluster RCT To evaluate the effectiveness of a computer-based stress management training programme | 263 employees from a manufacturing company Mean age 38.9 yrs ± 11.4 yrs 7% female | (a) Online stress management training consisting of behavioural, communication and cognitive techniques (b) Waitlist control | Brief Job Stress Questionnaire, Utrecht Work Engagement Scale, World Health Organization Health and Work Performance Questionnaire, Brief Scales for Coping Profile | There was a significant effect found for increase in ‘knowledge about stress management’ in the intervention group | L |
| Van den Heuvel, 2003 (45) Netherlands | RCT To evaluate the effects of a software program that promotes extra activity for workers with neck and upper-limb complaints | 268 computer worker employees Age range 18–50 yrs | (a) Software program that prompts a 5-min break on screen for every 35 min of computer use with physical exercise recommendations (b) Software program that prompts a 5-min break on screen for every 35 min of computer use with no physical exercise recommendations (c) Control | Recovery rate from complaints questionnaire, frequency and severity of complaints, self-reported sick leave, productivity by the mean number of key strokes a day | There were no differences between pre and post intervention score comparisons between groups Self-reported recovery was significantly higher in the intervention groups compared with the control | U |
| Westrup, 2003 (46) USA | RCT To assess the impact of a website-based intervention aimed at reducing high-risk drinking | 187 employees Mean age 40.9 yrs ± 11.5 yrs 77% female | (a) Website for alcohol and coping behaviour with limited individualized feedback (b) Website for alcohol and coping behaviour with full individualized feedback | Social Readjustment Rating Scale, modified version of Brief COPEf Inventory, daily website usage in minutes | There was no significant difference between groups for average daily minutes of website use Significant differences were found in average daily use related to alcohol dependence risk level with those at the high-risk level using the website more than those in the moderate or low-risk group | U |
| Zhang, 2017 (47) Singapore | Pilot RCT To pilot Smartphone-Based Coronary Heart Disease (CHD) Prevention programme aimed at improving awareness and knowledge of CHD, perceived stress and cardiac-related lifestyle behaviours | 80 employees without CHD not working in heart-related organizations or institutes Age range 21–40 yrs65% female | (a) Smartphone app with heart-related educational programme (b) Health promotion website access | Awareness of CHD, Heart Disease Fact Questionnaire, Perceived Stress Scale, Behavioural Risk Factor Surveillance System questionnaire | The intervention group had higher CHD awareness and knowledge than the control group as well as one better coronary behaviour (i.e. blood cholesterol control) | U |
Randomized controlled trial (RCT).
WHO-5 Well-being Index (World Health Organization 5-item well-being index).
L: low risk of bias; U: unclear risk of bias.
BMI (body mass index).
EQ-5D (European Quality of Life-5 Dimensions).
COPE (Coping Inventory).
Table 2.
Summary of intervention characteristics of included studies.
| First author, date (ref) | Label and content | Mode of delivery | Duration of intervention |
|---|---|---|---|
| Bolier, 2014 (26) | Workers’ health surveillance module with established self-help programmes: Psyfit, Colour Your Life, Strong at Work, Don't Panic Online, Drinking Less: screening with automated individual feedback and offer of online interventions targeting well-being and mental health | Multiple websites | 12 wks |
| Bostock, 2016 (27) | Digital cognitive behavioural therapy (dCBT) for insomnia: assessment, tailored feedback and online support delivered using established programme (www.sleepio.com). Included automatic email/SMSa prompts support | Website, SMS, email | 8 wks |
| Brendryen, 2017 (28) | Intensive online alcohol self-help programme with SMS and email reminders – programme designed to address risky alcohol behaviour through self-regulation with four key aspects: goal setting and tracking of alcohol consumption, relapse prevention, emotion regulation and alcohol education | Website, SMS, email | 24 wks |
| Cook, 2007 (29) | Health Connection: multimedia health promotion programme offering education/guidance for stress, weight management and fitness. Rooted in models of health behaviour change and designed to improve lifestyle behaviours and attitudes of working adults | Website | 12 wks |
| Cook, 2015 (30) | HealthyPast50: Web-based multimedia programme containing education/guidance on the major health topics relevant to older adults including assessments and educational modules | Website | 12 wks |
| Deitz 2014 (31) | Heart Healthy: Your Guide for Life!: web-based, healthy heart promotion programme with tailored feedback and five interactive modules. Email reminders every 2 weeks | Website, email | 6 wks |
| Doumas, 2007 (32) | www.CheckYourDrinking.net: web-based programme with personalized drinking feedback in relation to national norms, financial costs, negative effects and risk status | Website | 4 wks |
| Griffiths, 2016 (33) | Mental Health Guru (MH-Guru): two-module online mental health workplace induction programme focused on depression and anxiety. Modules take 30 min to complete, once a week | Website | 2 wks |
| Irvine, 2011 (34) | Get Moving: online web-based intervention accessible on company-specified computer included tailored feedback, education, support and guidance for physical activity. Participants were encouraged to visit a location once a week to log on | Website, SMS | 4 wks |
| Ketelaar, 2014 (35) | e-mental health (EMH): online programme consisting of screening, tailored feedback and online advice through access to self-help internet interventions | Website, email | 4 wks |
| Khadjesar, 2014 (36) | Online health check with personalized feedback including Down Your Drink (DYD): online programme consisting of screening, tailored feedback and access to an extended online alcohol intervention. Email reminder to complete final questionnaire | Website, email | 12 wks |
| Mainsbridge, 2014 (37) | Exertime: e-health software program designed to reduce sitting time with personal computer prompts to stand and undertake physical activity (e.g. walking to the photocopier, taking the stairs), which then had to be logged as completed to return to work screen | Downloaded software | 13 wks |
| Matano, 2006 (38) | CopingMatters: website providing fully tailored feedback, recommendations, mini-workshops, activities and links to further online resources to better manage risk for alcohol-related problems | Website | 12 wks |
| Pedersen, 2014 (39) | Exertime: e-health software program designed to reduce sitting time with personal computer prompts to stand and undertake physical activity (e.g. walking to the photocopier, taking the stairs), which then had to be logged as completed to return to work screen | Downloaded software | 13 wks |
| Querstret, 2016 (40) | www.bemindfulonline.com: online mindfulness programme with 10 interactive sessions through which participants learn to use both formal meditation skills and informal mindfulness techniques. Shortened version of traditional 8-week mindfulness programme | Website | 4 wks |
| Schell, 2008 (41) | Web-based stress management and health promotion programme: online programme for assessing, monitoring and managing stress levels and health including online diaries | Website | 24 wks |
| Shimazu, 2005 (42) | Web-based programme for stress management, problem solving and coping enhancement: online self-paced programme with three phases aimed at improving stress knowledge, problem solving in the workplace and application of acquired skills in the workplace. Email reminders or prompts were sent when learning did not initiate or was incomplete | Website, email | 5 wks |
| Solenhill, 2016 (43) | Web-based lifestyle health intervention: online health programme aimed at improving lifestyle factors including BMIb, perceived health and motivation to change along with tailored feedback | Website | 36 wks |
| Umanodan, 2014 (44) | Computer-based stress management training: online self-paced programme with a two-phased approach consisting of skill acquisition followed by application. Weekly email reminders and prompts throughout | Website, email | 8 wks |
| Van den Heuvel, 2003 (45) | Programme stimulating regular breaks in the work place for physical activity: software installed onto workplace computers prompts a 5-min break on screen for every 35 min of computer use with recommendation to partake in physical exercise | Website | 8 wks |
| Westrup, 2003 (46) | CopingMatters: website providing tailored feedback, recommendations, mini-workshops, activities and links to further online resources to better manage risk for alcohol-related problems | Website | 12 wks |
| Zhang, 2017 (47) | Care4Heart: app with SMS support developed specifically for working adults with four learning modules, covering coronary heart disease education (CHD), risk factors for CHD, healthy lifestyles related to CHD and stress management in relation to CHD. Relaxation video clips and the ability to track health information such as daily calorie intake were included in the app | Smart phone app, SMS | 4 wks |
Short messaging service (SM).
Body mass index (BMI).
Participant characteristics
The mean age of participants was 42 years (SD = 6.5 years) with over 90% being less than 50 years old and more than two-thirds being between 40 and 50 years of age. As the review inclusion criteria was a workplace setting, all participants were employees. Ethnicity was generally not specified with instead the location of the study being the only indication of participant nationality. Of the 22 studies, the gender ratios were tipped towards female participants with the average proportion of females in studies being 69%.
Participants were recruited from a variety of workplaces including public and private offices, academic or hospital settings and manufacturing plants. The majority of studies (n = 11) recruited employees who were identified as desk-based or office workers,32,37–39,41–43,45,46,48,49 three studies included nurse or health professionals26,31,35 and the remaining eight studies recruited employees from a government department,33 large unnamed organizations,27,36 manufacturing plant employees34,44 or a mix of businesses and organizations combined together.28,40,47
Over a quarter of the studies (n = 7) were conducted in the USA29–32,34,38,50 with the next most common locations being Australia (n = 3),26,35,45 the Netherlands (n = 3)27,36,40 and the UK (n = 3).27,36,40 The last six studies were conducted in Sweden,41,43 Japan,42,44 Norway28 and Singapore.47
Attrition rates
Using available data reported within each study, attrition rates were calculated based on numbers at baseline compared with those included in the final analysis. Attrition rates ranged from 0 to 60%, with a median rate of 21%, but two studies stood out with no participants withdrawing,37,39 both of which included interventions aimed at reducing sitting time for desk-based employees. In contrast, the two studies35,44 with the highest attrition rate (i.e. 56% and 60%) were aimed at improving mental health and stress management.
Intervention characteristics
The contents of the interventions varied considerably (see Table 2) but most (n = 17) were formatted much the same way in that they included an assessment (e.g. screening) and individualized feedback based on the results of the assessment.26,28–33,35,36,38,41–47 The feedback component within these interventions usually consisted of a website with health and education information and/or interactive sessions to improve the targeted behaviour or outcome. The remaining interventions were specific software programs aimed at reducing sedentary behaviour in the work place (n = 3),34,37,39 an online digital CBT (cognitive behavioural therapy) programme27 and an online mindfulness course for employees.40 Despite the large volume of health applications available for smart phones, only one study had an intervention that was delivered primarily by a smart phone application,47 but four in total used SMS (short message services).
While some interventions were introduced with human (e.g. researcher) contact, all participation with the actual intervention was digital, usually accessed with a private code or password once the employee consented to participate. Tailored feedback generated ranged from generic information related to response options chosen by participants during health or well-being screenings to fully individualized recommendations, homework, personal challenges or online diaries. Push notifications and encouraging emails automatically sent at certain stages throughout interventions were included within 50% of studies.
Just over half of the reviewed studies (n = 12) included interventions that used an already existing online intervention, usually in combination with a health assessment.26,27,31–33,35,37–40,46 A further seven28,34,41–45 included interventions that were study specific (i.e. programmes that had not been used or evaluated previously) and three studies assessed interventions that had been previously developed by the authors themselves.29,30,47
Duration of interventions
The average length of the interventions in the studies included was 3 months (median = 12 weeks) with nine being exactly 12 weeks in length26,29,30,36–39,42,46 and 10 studies running from 2 to 8 weeks.27,31–35,40,44,45,47 Of the three studies that had interventions that ran for longer, two ran for 6 months28,41 and one study had a general health behaviour intervention that was available to participants for 9 months.43
Control and comparisons
There were a variety of control and comparison types used for the studies reviewed, all of which were time matched in length. More than half of the reviewed studies (n = 12) used a waitlist control,26,27,31,33–35,37,39,40,42,44,49 where the control groups were administered the same baseline assessment and then upon completion of the study, were given the opportunity to try the intervention as well. Studies that had a comparison group instead of a waitlist control included five studies36,38,45–47 that offered a reduced version of the intervention (e.g. website access without tailored feedback), two studies that offered text material only (i.e. brief educational e-booklet or printed material)28,29 and three studies that included comparison groups that were not purely digital32,41,43 and involved human support such as a motivational interview or telephone support. Only two of these studies41,43 included a waitlist control and a comparison group.
Outcome measures
Most studies used a mix of different outcome measures including physical, psychological, biological, behavioural or work measures. There were 30 instances where standardized measures were used, which are detailed in Table 1, but many measures were study specific to adapt to the digital nature of the intervention.
Physical measures
Physical health measures were both self-reported and biometric with 19 instances in total (see Table 1). The outcomes included self-reported measures of sleep, physical activity levels and healthy lifestyle rating as well as biological measures of heart rate, blood pressure and body mass index (BMI).
Psychological measures
The total number of instances of mental or well-being related measures was 25. These measures (see Table 1) ranged from perceived motivation ratings to self-efficacy scales with the most common being measures of anxiety and depression (n = 6). Examples of more novel measures were mindfulness and help-seeking attitude questionnaires.
Other health-related measures
As per Table 1, most studies used a combination of health measures, which largely reflected the variety of study aims undertaken. This included health-related measures focused on alcohol and eating behaviours, website usage, logged activity counts and even productivity by daily mean number of keystrokes on a work computer keyboard. The total instances of occupational measures related to health was 17 with standardized measures such as the Brief Job Stress Questionnaire,50 the Utrecht Work Engagement Scale51 and the Work Productivity and Activity Impairment52 questionnaire being common examples.
Design and aims of studies
All studies included in the review were RCTs, three of which were pilot RCTs28,38,47 and three clustered RCTs.26,44,45 Across the studies, the combined number of participants randomized was 6168. Sample sizes ranged from 29 to 1066 participants, with a median of 216. Less than one-fifth of studies randomized under 100 participants28,37,39,47 and two of these were pilots, which therefore aimed to recruit a smaller sample.46,47 Almost half (n = 9) of the studies had samples consisting of 200–500 randomized participants26,27,29,31,34,41,44,45,49 with only three studies over 500.33,36,43
Most of the studies (n = 19) aimed to improve or change a specific health-related outcome. Of these, five were an alcohol improvement intervention,28,32,38,46,53 another five aimed to improve a mental health outcome,26,33,35,42,44 three studies aimed to improve sedentary behaviour for desk-based employees,34,37,39 two focused on improving musculoskeletal symptoms,41,45 another two on heart health improvement,31,47 one for insomnia27 and one for a mix of work-related rumination, fatigue and sleep.40 The final three studies aimed to improve a combination of outcomes such as general health, stress, coping abilities and diet.29,30,43
Intervention effects
Out of the 22 studies reviewed, almost half (n = 9) had positive significant findings for a primary outcome measure. The most common type of intervention with a significant effect (n = 3) was an intervention aimed at improvement of sedentary behaviour among computer-based employees reported in three studies using an e-health software program.34,37,39 The remaining studies found significant improvements with mental health,26,33 job satisfaction,42 healthy heart-related behaviours (e.g. diet, exercise, self-efficacy)31 and insomnia,27 and in one study the intervention was found to improve work-related levels of rumination, problem solving, pondering, fatigue and sleep quality.40
Mixed and negative findings
The studies reviewed (n = 13) that had mixed results and in one instance a negative outcome did not vary appreciably with regard to type of interventions or mode of delivery when compared with those that found positive significant effects. The most common aim of the studies in this group was alcohol behaviour related (n = 5), and while there were significant improvements for all but one, each had a caveat attached. One study found improvements but the high attrition rate rendered the results inconclusive,28 another found improvement but only when the two intervention groups were combined and compared with the control,38 another found differences but only between high- versus low-risk drinkers and not between intervention groups,26 and another found differences between groups but only when sub-analysis was conducted and only with specific types of binge-drinking behaviours.36 The last of the alcohol-focused studies was the only study that did not result in any significant outcomes,36 and in this study the intervention group reported a 5.6% increase in weekly alcohol consumption.
The remaining studies with mixed results (n = 8) included interventions aimed at improving a group of health behaviours, psychological well-being and stress-related musculoskeletal complaints. The majority of these studies (n = 6) found a significant improvement in only one or some of the health-related measures29,30,35,44,45,47 included. The two remaining studies were less clear in that one found improvement for the intervention group but only at baseline compared with the control (i.e. the difference was short term)43 and another found differences within groups but not between and were inconsistent in regard to symptom localization.41
Risk of bias
Of the 22 studies, seven were classified as having a low risk of bias26–28,37,40,41,44 based on qualities such as clearly defined randomization process reporting, appropriate blinding of group allocation where possible and complete reporting of all outcomes stated in the methods. The remaining studies (n = 15) did not report or clarify measures taken to avoid bias, so they were given an unclear risk status. A summary of the risk of bias assessment can be found in Table 3 in supplementary File 2.
Excluded studies
Throughout the study selection process, a total of 11 studies were found to be highly relevant but not eligible due to the inclusion criteria. Six of these studies included human input supplied in the form of health care professionals, such as physicians or counsellors, who were accessible in person or by phone, text or email.16,19,54–57 Another four studies did not report health-related outcomes and instead reported engagement and acceptability outcomes.53,58–60 One study was a cost analysis study that reported health care cost results with no data on specific health-related outcomes.61
Discussion
The purpose of this systematic review was to assess the impact of digital health interventions in the workplace on health-related outcomes of employee participants. A key eligibility factor for study inclusion was the use of digital-only interventions so as to better discern the effect of the digital component. The final selection of articles was 22 RCTs covering a broad range of interventions and measured outcomes. Significant improvements were found in all studies but one, for at least one health-related outcome, although more than half of the studies had a mix of both positive and negative findings. The interventions varied in content, but most were formatted as a combination of an initial assessment followed by access to a website. Three of the studies differed slightly in approach; two used specific software programs downloaded on to work computers and one used a smart phone app. Although the study designs were all RCTs, three were pilot RCTs and three were cluster RCTs. These were considered eligible as they were randomized and included at least one primary health-related outcome. The quality of the studies included was adequate based on risk of bias assessment using the Cochrane risk of bias tool.
A high level of heterogeneity across the studies in terms of intervention aims, content, measures and overall outcomes made it difficult to compare or discern patterns of impact among the 22 included studies. However, from the group of nine studies that reported positive significant improvements for a primary health-related outcome, it would appear interventions that targeted specific health behaviours, such as being sedentary in the workplace, were especially engaging and effective. The two studies that exemplify this both used an intervention labelled ‘Exertime’.37,39 Both articles reported a 0% attrition rate, unmatched in this respect by any other intervention reviewed. It is worth noting that the ‘Exertime’ studies had substantially smaller samples sizes (ranging from 29 to 34 participants) compared with most of the other studies and it is therefore not clear whether this observed impact would be replicated in larger, more dispersed populations. It is clear, however, that the combination of intervention design and implementation garnered impressive engagement over the 12- to 13-week study period. This was potentially due to the ease with which the intervention, consisting of short and simple tasks, was integrated into participants’ daily workflow creating a high opportunity, low demand situation for the behaviour change to occur. Further supporting this type of approach was another study using a programme called ‘Get Moving’.34 This intervention also aimed to improve sedentary work behaviour and reported significant findings and a low attrition rate of only 5%.
The concept of targeting a specific area of health to drive efficacy and outcomes was evidenced by two other studies with positive significant findings. These studies were aimed at improving insomnia in one instance27 and heart healthy behaviour in the other.31 Both were successful with sample sizes of over 200 participants and attrition rates lower than 25%, closer to the average rate for digital health interventions in general.62
In contrast, studies targeting complex, and sometimes multifactorial, health-related behaviours did not appear to be as efficacious. An example of this was a collection of five studies that included interventions aimed at improving alcohol-related behaviours. Of these studies, four had significant findings but only within certain contexts. The first two studies38,46 found improvements for specific groups (e.g. moderate or high-risk alcohol groups) and for specific types of drinking behaviours (e.g. bingeing). As one of these studies46 used website usage as an outcome measure, it is difficult to tell if this translated into actual behaviour change. The third study32 had a significant result but only when two intervention arms were combined and compared with the waitlist control group, and the fourth study28 found a significant difference between groups, but this effect disappeared when a sensitivity analysis was conducted to account for missing data. This highlights a major issue with evaluating any intervention that has a high attrition rate. The final study36 had non-significant findings even though it utilized an intervention much the same as the previous four studies (i.e. online screening and tailored feedback specific to drinking) and resulted in the intervention group having an increased weekly average alcohol consumption of 5.6%.
Based on the studies within this review, it would appear that purely digital interventions are most beneficial when firmly embedded into the work environment (e.g. downloaded as software directly onto a work computer) and are restricted to targeting specific health behaviours that are routinely conducted during working hours (e.g. physical activity, eating). In the case of more complex health issues, especially ones where the health behaviours extend outside the workplace environment, a purely digital intervention may not be adequate and a multicomponent intervention, including human support, may be a better approach.63
Limitations and future directions
Although the included studies were of robust design (i.e. RCTs), the frequent use of non-standardized outcome measures made attempts to draw comparisons between outwardly similar studies difficult, which is a limitation of the review overall. The results from the alcohol studies demonstrate the difficulties of assessing the impact of digital interventions in the workplace, especially when targeting complex health behaviours. Perhaps mirroring some of the same issues, many of the studies within this review reported both positive and negative results, making it difficult in particular to formulate conclusions in relation to which type of intervention is effective for which outcome. In addition, attrition rates (ranging from 0 to 60%) raise questions as to whether engagement or the measures used for quantifying outcomes were influencing results. An in-depth focus on engagement together with the use of standardized measures and better reporting of ‘active’ intervention components would strongly enhance future evaluations and perhaps allow for meta-analysis.
Conclusions
Existing evidence suggests that workplace digital health interventions show promise as a method for improving various aspects of employee health. This review systematically assessed current available research investigating purely digital interventions in the workplace. It is clear that more research is needed as a strong foundation of evidence is currently lacking. Many recently developed health interventions have begun to use the behaviour change taxonomy developed by Michie et al. (2013)64 and future research should include the reporting of the ‘active’ components of interventions to help clarify how programmes are working. This together with the use of standardized measures will make it easier to demonstrate the type of interventions that are most efficacious for different health-related behaviours.
In addition, further investigation of intervention engagement is necessary. Investigators should address engagement early on in programme design as well as throughout implementation and evaluation. This approach, alongside the inclusion of measures that more clearly translate into return on investment (ROI) metrics, may be beneficial to many employers looking to quantify the value of workplace digital health interventions.
Finally, this review highlights the scalability of digital workplace interventions for improving health-related outcomes. Although there is evidence suggesting multicomponent interventions are superior in supporting employee health and well-being enhancement, further investigation of the digital components of these programmes is necessary. With smartphone internet access now surpassing traditional computer-based access, it would be advantageous for new studies to explore the efficacy of this particular medium. As mentioned earlier, only one study47 in this review included a smartphone app as part of the intervention. Considering that the number of health apps available worldwide exceeded 318,000 last year,65 it may be that evaluating existing smartphone apps in an employee population could be the next step in establishing the impact of digital health interventions within the workplace.
Supplemental Material
Supplemental material for The impact of digital health interventions on health-related outcomes in the workplace: A systematic review by Ana Howarth, Jose Quesada, Jessica Silva, Stephanie Judycki and Peter R Mills in Digital Health
Contributorship
JQ, PM and AH conceived and designed the study. AH with the assistance of PM, SJ, JS and JQ, contributed to data extraction, conducted the analyses, and drafted and revised the manuscript. All authors read and approved the final manuscript.
Conflict of interest
All authors are either directly employed or contracted by Cigna Corporation, or one of its subsidiaries, which develops and markets a variety of health interventions. The authors declare that they have no conflicting interests.
Ethical approval
Not applicable.
Funding
This work was supported by Cigna Global Wellbeing Solutions Ltd, UK.
Guarantor
AH was the guarantor.
Peer review
This manuscript was reviewed by two reviewers who have both chosen to remain anonymous.
Supplementary Material
Supplementary material is available for this article online.
References
- 1.Rizzo JA, Zyczynski TM, Chen J, Mallow PJ, Trudel GC, Penrod JR. Lost labor productivity costs of prostate cancer to patients and their spouses. J Occup Environ Med 2016; 58(4): 351–358. [DOI] [PubMed] [Google Scholar]
- 2.Henke RM, Carls GS, Short ME, Pei X, Wang S, Moley S, et al. The relationship between health risks and health and productivity costs among employees at Pepsi Bottling Group. J Occup Environ Med 2010; 52(5): 519–527. [DOI] [PubMed] [Google Scholar]
- 3.Durden ED, Huse D, Ben-Joseph R, Chu B-C. Economic costs of obesity to self-insured employers. J Occup Environ Med 2008; 50(9): 991–997. [DOI] [PubMed] [Google Scholar]
- 4.Ozminkowski RJ, Wang S, Walsh JK. The direct and indirect costs of untreated insomnia in adults in the United States. Sleep 2007; 30(3): 263–273. [DOI] [PubMed] [Google Scholar]
- 5.Tsai SP, Ahmed FS, Wendt JK, Bhojani F, Donnelly RP. The impact of obesity on illness absence and productivity in an industrial population of petrochemical workers. Ann Epidemiol 2008; 18(1): 8–14. [DOI] [PubMed] [Google Scholar]
- 6.Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D. Cost of Lost Productive Work Time Among US Workers With Depression. JAMA 2003; 289(23): 3135. [DOI] [PubMed] [Google Scholar]
- 7.Kirsten W. Making the link between health and productivity at the workplace–a global perspective. Ind Health 2010; 48(3): 251–255. [DOI] [PubMed] [Google Scholar]
- 8.Kigozi J, Jowett S, Lewis M, Barton P, Coast J. The estimation and inclusion of presenteeism costs in applied economic evaluation: a systematic review. Value Heal 2017; 20(3): 496–506. [DOI] [PubMed] [Google Scholar]
- 9.Kannan H, Thompson S, Bolge SC. Economic and humanistic outcomes associated with comorbid type-2 diabetes, high cholesterol, and hypertension among individuals who are overweight or obese. J Occup Environ Med 2008; 50(5): 542–549. [DOI] [PubMed] [Google Scholar]
- 10.Darkow T, Chastek BJ, Shah H, Phillips AL. Health care costs among individuals with chronic obstructive pulmonary disease within several large, multi-state employers. J Occup Environ Med 2008; 50(10): 1130–1138. [DOI] [PubMed] [Google Scholar]
- 11.Ozminkowski RJ, Burton WN, Goetzel RZ, Maclean R, Wang S. The impact of rheumatoid arthritis on medical expenditures, absenteeism, and short-term disability benefits. J Occup Environ Med 2006; 48(2): 135–148. [DOI] [PubMed] [Google Scholar]
- 12.Wang F, McDonald T, Champagne L. Relationship of body mass index and physical activity to health care costs among employees. Occup … 2004. [DOI] [PubMed]
- 13.Merrill RM, Aldana SG, Garrett J, Ross C. Effectiveness of a workplace wellness program for maintaining health and promoting healthy behaviors. J Occup Environ Med 2011; 53(7): 782–787. [DOI] [PubMed] [Google Scholar]
- 14.Patel DN, Lambert EV, da Silva R, Greyling M, Nossel C, Noach A, et al. The association between medical costs and participation in the vitality health promotion program among 948,974 members of a South African health insurance company. Am J Health Promot 2010; 24(3): 199–204. [DOI] [PubMed] [Google Scholar]
- 15.Baicker K, Cutler D, Song Z. Workplace wellness programs can generate savings. Health Aff (Millwood) 2010; 29(2): 304–311. [DOI] [PubMed] [Google Scholar]
- 16.Widmer RJ, Allison TG, Keane B, Dallas A, Bailey KR, Lerman LO, et al. Workplace digital health is associated with improved cardiovascular risk factors in a frequency-dependent fashion: A large prospective observational cohort study. PLoS One 2016; 11(4): e0152657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beiwinkel T, Eissing T, Telle N-T, Siegmund-Schultze E, Rossler W. Effectiveness of a web-based intervention in reducing depression and sickness absence: randomized controlled trial. J Med Internet Res 2017; 19(6): e213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mills PR, Kessler RC, Cooper J, Sullivan S. Impact of a health promotion program on employee health risks and work productivity. Am J Health Promot 2007; 22(1): 45–53. [DOI] [PubMed] [Google Scholar]
- 19.van Wier MF, Dekkers J, Bosmans JE, Heymans MW, Hendriksen IJ, Pronk NP, et al. Economic evaluation of a weight control program with e-mail and telephone counseling among overweight employees: a randomized controlled trial. Int J Behav Nutr Phys Act 2012; 9(1): 112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aneni EC, Roberson LL, Maziak W, Agatston AS, Feldman T, Rouseff M, et al. A Systematic review of internet-based worksite wellness approaches for cardiovascular disease risk management: outcomes, challenges & opportunities. PLoS One 2014; 9(1): e83594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group TP. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6(7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Howarth A, Mills PR. Systematic review of the impact of digital health interventions in the workplace. Prospero. 2017. Available at: www.crd.york.ac.uk/prospero (accessed 23 March 2018).
- 23.Counsell C. Formulating questions and locating primary studies for inclusion in systematic reviews. Ann Intern Med 1997; 127(5): 380–387. [DOI] [PubMed] [Google Scholar]
- 24.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated march 2011]. In: Higgins JP, Green S. (eds). Cochrane Handbook for Systematic Reviews of Interventions, Chichester, UK: John Wiley & Sons, Ltd, 2008, pp. 1–649. [Google Scholar]
- 25.Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011; 343 doi: https://doi.org/10.1136/bmj.d5928 (accessed 18 October 2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bolier L, Ketelaar SM, Nieuwenhuijsen K, Smeets O, Gortner FR, Sluiter JK. Workplace mental health promotion online to enhance well-being of nurses and allied health professionals: A cluster-randomized controlled trial. Internet Interv 2014; 1(4): 196–204. [Google Scholar]
- 27.Bostock S, Luik AI, Espie CA. Sleep and productivity benefits of digital cognitive behavioral therapy for insomnia. J Occup Environ Med 2016; 58(7): 683–689. [DOI] [PubMed] [Google Scholar]
- 28.Brendryen H, Johansen A, Duckert F, Nesvåg S. A Pilot randomized controlled trial of an internet-based alcohol intervention in a workplace setting. Int J Behav Med 2017; 24(5): 768–777. [DOI] [PubMed] [Google Scholar]
- 29.Cook RF, Billings DW, Hersch RK, Back AS, Hendrickson A. A field test of a web-based workplace health promotion program to improve dietary practices, reduce stress, and increase physical activity: randomized controlled trial. J Med Internet Res 2007; 9(2): e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cook RF, Hersch RK, Schlossberg D, Leaf SL. A Web-based health promotion program for older workers: randomized controlled trial. J Med Internet Res 2015; 17(3): e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deitz D, Cook RF, Hersch RK, Leaf S. Heart healthy online. J Occup Environ Med 2014; 56(5): 547–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Doumas DM, Hannah E. Preventing high-risk drinking in youth in the workplace: A web-based normative feedback program. J Subst Abuse Treat 2008; 34(3): 263–271. [DOI] [PubMed] [Google Scholar]
- 33.Griffiths KM, Bennett K, Walker J, Goldsmid S, Bennett A. Effectiveness of MH-Guru, a brief online mental health program for the workplace: A randomised controlled trial. Internet Interv 2016; 6: 29–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Irvine AB, Philips L, Seeley J, Wyant S, Duncan S, Moore RW. Get moving: a web site that increases physical activity of sedentary employees. Am J Heal Promot 2011; 25(3): 199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ketelaar SM, Nieuwenhuijsen K, Bolier L, Smeets O, Sluiter JK. Improving work functioning and mental health of health care employees using an e-mental health approach to workers' health surveillance: pretest-posttest study. Saf Health Work 2014; 5(4): 216–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khadjesari Z, Freemantle N, Linke S, Hunter R, Murray E, Force U. Health on the web: randomised controlled trial of online screening and brief alcohol intervention delivered in a workplace setting. PLoS One 2014; 9(11): e112553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mainsbridge CP, Cooley PD, Fraser SP, Pedersen SJ. The effect of an e-health intervention designed to reduce prolonged occupational sitting on mean arterial pressure. J Occup Environ Med 2014; 56(11): 1189–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Matano RA, Koopman C, Wanat SF, Winzelberg AJ, Whitsell SD, Westrup D, et al. A pilot study of an interactive web site in the workplace for reducing alcohol consumption. J Subst Abuse Treat 2007; 32(1): 71–80. [DOI] [PubMed] [Google Scholar]
- 39.Pedersen SJ, Cooley PD, Mainsbridge C. An e-health intervention designed to increase workday energy expenditure by reducing prolonged occupational sitting habits. Work 2014; 49(2): 289–295. [DOI] [PubMed] [Google Scholar]
- 40.Querstret D, Cropley M, Fife-Schaw C. Internet-based instructor-led mindfulness for work-related rumination, fatigue, and sleep: Assessing facets of mindfulness as mechanisms of change. A randomized waitlist control trial. J Occup Health Psychol 2017; 22(2): 153–169. [DOI] [PubMed] [Google Scholar]
- 41.Schell E, Theorell T, Hasson D, Arnetz B, Saraste H. Impact of a web-based stress management and health promotion program on neck-shoulder-back pain in knowledge workers? 12 month prospective controlled follow-up. J Occup Environ Med 2008; 50(6): 667–676. [DOI] [PubMed] [Google Scholar]
- 42.Shimazu A, Kawakami N, Irimajiri H, Sakamoto M, Amano S. Effects of web-based psychoeducation on self-efficacy, problem solving behavior, stress responses and job satisfaction among workers: a controlled clinical trial. J Occup Health 2005; 47(5): 405–413. [DOI] [PubMed] [Google Scholar]
- 43.Solenhill M, Grotta A, Pasquali E, Bakkman L, Bellocco R, Trolle Lagerros Y. The effect of tailored web-based feedback and optional telephone coaching on health improvements: a randomized intervention among employees in the transport service industry. J Med Internet Res 2016; 18(8): e158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Umanodan R, Shimazu A, Minami M, Kawakami N. Effects of computer-based stress management training on psychological well-being and work performance in japanese employees: a cluster randomized controlled trial. Ind Health 2014; 52(6): 480–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.van den Heuvel SG, de Looze MP, Hildebrandt VH, Thé KH. Effects of software programs stimulating regular breaks and exercises on work-related neck and upper-limb disorders. Scand J Work Environ Health 2003; 29(2): 10616. [DOI] [PubMed] [Google Scholar]
- 46.Westrup D, Futa KT, Whitsell S, Mussman L, Wanat SF, Koopman C, et al. Employees' reactions to an interactive website assessing alcohol use and risk for alcohol dependence, stress level and coping. J Subst Use 2003; 8(2): 104–111. [Google Scholar]
- 47.Zhang H, Jiang Y, Nguyen HD, Poo DCC, Wang W. The effect of a smartphone-based coronary heart disease prevention (SBCHDP) programme on awareness and knowledge of CHD, stress, and cardiac-related lifestyle behaviours among the working population in Singapore: a pilot randomised controlled trial. Health Qual Life Outcomes 2017; 15(1): 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cook RF, Billings DW, Hersch RK, Back AS, Hendrickson A. A field test of a web-based workplace health promotion program to improve dietary practices, reduce stress, and increase physical activity: Randomized controlled trial. J Med Internet Res 2007; 9(2): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cook RF, Hersch RK, Schlossberg D, Leaf SL. A Web-based health promotion program for older workers: Randomized controlled trial. J Med Internet Res 2015; 17(3): 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shimomitsu T, Haratani T, Nakamura K, Kawakami N, Hayashi T, Hiro H, et al. Final development of Brief Job Stress Questionnaire mainly used for assessment of the individuals. The Ministry of Labor sponsored grant for prevention of work-related illness, FY1999 report. Tokyo; 2000.
- 51.Schaufeli WB, Salanova M, González-romá V, Bakker AB. The measurement of engagement and burnout: a two sample confirmatory factor analytic approach. J Happiness Stud 2002; 3(1): 71–92. [Google Scholar]
- 52.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics 1993; 4(5): 353–365. [DOI] [PubMed] [Google Scholar]
- 53.Khadjesari Z, Newbury-Birch D, Murray E, Shenker D, Marston L, Kaner E. Online health check for reducing alcohol intake among employees: A feasibility study in six workplaces across england. PLoS One 2015; 10(3): 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Petersen R, Sill S, Lu C, Young J, Edington DW. Effectiveness of employee internet-based weight management program. J Occup Environ Med 2008; 50(2): 163–171. [DOI] [PubMed] [Google Scholar]
- 55.Phillips R, Schneider J, Molosankwe I, Leese M, Foroushani PS, Grime P, et al. Randomized controlled trial of computerized cognitive behavioural therapy for depressive symptoms: effectiveness and costs of a workplace intervention. Psychol Med 2014; 44(4): 741–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pratt DS, Jandzio M, Tomlinson D, Kang X, Smith E. The 5-10-25 Challenge: An Observational Study of a Web-Based Wellness Intervention for a Global Workforce. Dis Manag 2006; 9(5): 284–290. [DOI] [PubMed] [Google Scholar]
- 57.Watson AJ, Singh K, Myint-U K, Grant RW, Jethwani K, Murachver E, et al. Evaluating a web-based self-management program for employees with hypertension and prehypertension: A randomized clinical trial. Am Heart J 2012; 164(4): 625–631. [DOI] [PubMed] [Google Scholar]
- 58.Cousineau T, Houle B, Bromberg J, Fernandez KC, Kling WC. A pilot study of an online workplace nutrition program: the value of participant input in program development. J Nutr Educ Behav 2008; 40(3): 160–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cowdery JE, Suggs LS, Parker S. Application of a web-based tailored health risk assessment in a work-site population. Health Promot Pract 2007; 8(1): 88–95. [DOI] [PubMed] [Google Scholar]
- 60.Lucini D, Zanuso S, Solaro N, Vigo C, Malacarne M, Pagani M. Reducing the risk of metabolic syndrome at the worksite: preliminary experience with an ecological approach. Acta Diabetol 2016; 53(1): 63–71. [DOI] [PubMed] [Google Scholar]
- 61.Sacks N, Cabral H, Kazis LE, Jarrett KM, Vetter D, Richmond R, et al. A web-based nutrition program reduces health care costs in employees with cardiac risk factors: Before and after cost analysis. J Med Internet Res 2009; 11(4): 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Eysenbach G. The law of attrition. J Med Internet Res [Internet]. 2005 [cited 2016 Sep 30];7(1):e11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15829473. [DOI] [PMC free article] [PubMed]
- 63.Newman MG, Szkodny LE, Llera SJ, Przeworski A. A review of technology-assisted self-help and minimal contact therapies for drug and alcohol abuse and smoking addiction: Is human contact necessary for therapeutic efficacy? Clin Psychol Rev 2011; 31(1): 178–186. [DOI] [PubMed] [Google Scholar]
- 64.Michie S, Richardson M, Marie J, Abraham C, Frances J, hardemann W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013; 46(1): 81–95. [DOI] [PubMed] [Google Scholar]
- 65.IQVIA Institute. The growing value of digital health - evidence on human health and the healthcare system [Internet]. 2017. Available from: https://www.iqvia.com/institute/reports/the-growing-value-of-digital-health (accessed 15 Feb 2018).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material for The impact of digital health interventions on health-related outcomes in the workplace: A systematic review by Ana Howarth, Jose Quesada, Jessica Silva, Stephanie Judycki and Peter R Mills in Digital Health