Abstract
Background
Integrating physical therapy sessions and an online application (e-Exercise) might support people with hip osteoarthritis (OA), knee OA, or both (hip/knee OA) in taking an active role in the management of their chronic condition and may reduce the number of physical therapy sessions.
Objective
The objective of this study was to investigate the short- and long-term effectiveness of e-Exercise compared to usual physical therapy in people with hip/knee OA.
Design
The design was a prospective, single-blind, multicenter, superiority, cluster- randomized controlled trial.
Setting
The setting included 143 primary care physical therapist practices.
Participants
The participants were 208 people who had hip/knee OA and were 40 to 80 years of age.
Intervention
e-Exercise is a 3-month intervention in which about 5 face-to-face physical therapy sessions were integrated with an online application consisting of graded activity, exercise, and information modules. Usual physical therapy was conducted according to the Dutch physical therapy guidelines on hip and knee OA.
Measurements
Primary outcomes, measured at baseline after 3 and 12 months, were physical functioning and free-living physical activity. Secondary outcome measures were pain, tiredness, quality of life, self-efficacy, and the number of physical therapy sessions.
Results
The e-Exercise group (n = 109) received, on average, 5 face-to-face sessions; the usual physical therapy group (n = 99) received 12. No significant differences in primary outcomes between the e-Exercise group and the usual physical therapy group were found. Within-group analyses for both groups showed a significant improvement in physical functioning. After 3 months, participants in the e-Exercise group reported an increase in physical activity; however, no objectively measured differences in physical activity were found. With respect to secondary outcomes, after 12 months, sedentary behavior significantly increased in the e-Exercise group compared with the usual physical therapy group. In both groups, there were significant improvements for pain, tiredness, quality of life, and self-efficacy.
Limitations
The response rate at 12 months was 65%.
Conclusions
The blended intervention, e-Exercise, was not more effective than usual physical therapy in people with hip/knee OA.
Osteoarthritis (OA) is the most common chronic condition of the joints.1 Prevalence of this rheumatic disease increases with age and mostly affects the hip and knee. Based on radiographic diagnosis, 5% to 15% of people 55 years old and older are affected with hip OA2 and 10% to 30% with knee OA.3 Because of the aging population and the growing number of people with obesity, the prevalence of OA is expected to increase,1 with an extra demand on health services as a consequence. People with OA of the hip, OA of the knee, or both (hip/knee OA) experience pain, stiffness, crepitation, reduced range of motion, and sometimes inflammation.4 Daily activities become more problematic, and these, in combination with psychological factors, put people at risk for a negative spiral of inactivity, resulting in muscle weakness and even more limitations in daily activities.5
The most recommended nonsurgical and nonpharmacological treatment for patients with OA is physical therapy.6,7 Physical therapist intervention consisting of muscle strengthening exercises, aerobic exercises, and patient education has shown to be effective in reducing levels of pain and improving physical functioning.2,3 One of the approaches to increase activity levels among patients with OA is graded activity.8 However, the downside of face-to-face physical therapy sessions is that they are costly. With the increasing prevalence of OA, there is a need for effective and cost-effective interventions to manage hip and knee OA.
Technological developments provide new solutions for guiding patients to a physically active lifestyle. For example, internet-based interventions, which are accessible at any time and place, might be able to replace part of physical therapists’ face-to-face guidance. In literature, the integration of therapeutic guidance and online care is called “blended care.”9 One of the main advantages of blended care is that the online part can support patients 24/7 in exercise at home. Well-designed online applications can be used as a medium for many behavior change techniques, such as goal-setting assignments, monitoring of outcomes and behavior, instruction, and providing information.10,11 Next, patients’ online evaluations of home assignments can provide valuable information for physical therapists about patients’ individual needs for guidance. Whereas online self-guided interventions often struggle with high rates of nonusage, the combination with therapeutic guidance is seen as highly promising in terms of usage, effectiveness, and cost-effectiveness.12,13
Given the high potential of blended interventions for people with OA, we developed the intervention e-Exercise.14 In e-Exercise, physical therapy sessions are combined with an online application to improve free-living physical activity in patients with hip/knee OA. The integration of physical therapy sessions and an online application might replace part of the therapeutic guidance. In addition, we expect that the online application can support patients in taking an active role in the management of their chronic condition in daily living by providing access to a 24/7-available behavior-change application. Therefore, we hypothesize e-Exercise to be more effective than usual physical therapy. The aim of this multicenter superiority cluster-randomized controlled trial was to investigate the short- and long-term effectiveness on physical functioning and free-living physical activity of e-Exercise compared to usual physical therapy in people with hip/knee OA.
Methods
Design Overview
A prospective, single-blind, multicenter, superiority, cluster randomized controlled trial was conducted. From May 2014 to August 2014, 248 physical therapists working in 143 primary care physical therapist practices were recruited. Half of the physical therapists were instructed to treat people with hip/knee OA according to the e-Exercise protocol, and the other half of the physical therapists were instructed to treat people as usual. Enrollment of participants started in September 2014 and ended in March 2015. Study outcomes were assessed at baseline, 3 months, and 12 months. The study design and protocol were approved by the Medical Ethical Committee of St Elisabeth Hospital, Tilburg, the Netherlands (Dutch Trial Register ref. no. NTR4224). Because we wanted to prevent less accurate answers or nonresponding, we deleted some secondary outcome measures (ie, motivation, locus of control, depression and anxiety, self-reported adherence, and self-management) that are listed in the trial register and executed the study as described in the study protocol.15 The trial is reported according to the CONSORT Cluster Trial checklist (eAppendix 1, available at academic.oup.com/ptj).
Setting and Randomization
Physical therapists were recruited in 2 ways. First, an invitational letter was sent to a random sample of 800 physical therapist practices in 3 provinces of the Netherlands. Second, an advertisement was placed in the online newsletter of The Royal Dutch Society for Physiotherapy. Physical therapist practices could participate with 1 or 2 physical therapists. Inclusion criteria for physical therapists were (1) practicing in primary care and (2) treating at least 6 patients with OA of the hip and/or knee per year. Physical therapists were cluster-randomized on the level of physical therapist practice using a computer-generated sequence table. To avoid contamination across physical therapists working in the same practice, randomization of the 248 eligible physical therapists took place at the level of the physical therapist practice using a 1:1 allocation ratio. By email they were informed about their allocation. Physical therapists were not masked, since they had to treat according to the randomization. The main investigator (C.J.J.K.) was masked to group assignment until completion of statistical analyses. Participants were assigned to a unique trial code. Participant information was stored separately from outcome data.
All physical therapists were invited for a half-day training. Physical therapists allocated to the e-Exercise group (n = 123) were instructed about the study procedure and how to use the online application. Physical therapists allocated to the “usual physical therapy” group (n = 125) were also instructed on the study procedure and received a presentation about the Dutch OA guideline.16 Physical therapists who followed the training and recruited at least 2 participants received accreditation points for the Dutch physical therapy registration. Physical therapists allocated to the “usual physical therapy” group received e-Exercise log-in codes and an invitation for an instruction session after the study period.
Participants
People who had hip/knee OA and visited a participating physical therapist were invited to participate in the study. Also, recruitment advertisements were placed in local newspapers, and information brochures were sent to general practitioners. Physical therapists verified patient eligibility for study participation. Eligibility criteria were as follows: an age of 40 to 80 years and hip/knee OA according to the clinical criteria of the American College of Rheumatology.17 The 6 exclusion criteria were as follows: being on a waiting list for a hip or knee replacement surgery, contraindications for PA without supervision according to the Physical Activity Readiness Questionnaire (PAR-Q), sufficiently physically active according to the physical therapist, participation in a physical therapy and/or PA program in the past 6 months, no access to internet, and inability to understand the Dutch language. Eligible people were informed by their physical therapist about the study and received an information letter and informed consent form. Participants were masked to the study hypotheses but were not masked to the comparator intervention. After an informative phone call with the researcher (C.J.J.K.), participants were asked to return their informed consent form.
Participant characteristics (age, sex, height, weight, educational level, location of OA, duration of OA, and the presence of comorbidities) were assessed as part of the baseline questionnaire.
Intervention: e-Exercise
The development and pilot study of e-Exercise is described elsewhere.14 The overall aim of e-Exercise is to stimulate a physically active lifestyle regardless of OA-related sensations. The intervention e-Exercise takes 12 weeks and is a combination of about 5 face-to-face sessions with a physical therapist and an online application focusing on behavioral graded activity, exercises, and information. The e-Exercise protocol is based on the Dutch OA guideline.16 In a participant's first session (week 1), the therapist created an e-Exercise account and provided support in the selection of 1 type of PA—for example, walking or cycling—and 4 strength and stability exercises. The participant was informed about the first online assignment, which was a 3-day baseline test to assess physical load ability. The results were discussed during the second face-to-face session and used for the formulation of a short- and long-term goal. During the third session in week 6, participant progress was discussed using online progress reports (ie, a summary of website visits and patients’ experiences with the exercises). In the last session (week 12), the maintenance of PA was discussed and supported. Although physical therapists were recommended to treat according to the e-Exercise protocol, they were free to deviate from the protocol with respect to their clinical competence.
The online part of e-Exercise consisted of 3 modules:
Graded activity—the duration of a participant's chosen PA was gradually increased until the individual short-term goal was met.
Strength and stability—each week the participant was asked to perform 2 video-supported exercises on 3 different days, and the number of repetitions was increased gradually every 4 weeks.
Information—each week a new video was generated about OA etiology, pain management, weight management, motivation, medication, and social influences on pain.
Weekly automatic emails informed and reminded patients about new assignments and content, and, at the end of the week, patients were asked to evaluate the execution of their assignments. Depending on their answer to the question “Were you able to execute the graded activity assignment, or did you do less or more?” automatic tailored feedback was generated. (The online application of e-Exercise can be seen at https://www.e-exercise.nl [in Dutch]; a promotional video with English subtitles is available at https://www.youtube.com/watch?v=4l9GoQWWy58.)
Intervention: Usual Physical Therapy
Usual physical therapy in the current study was defined as any treatment provided by the physical therapist. Physical therapists were encouraged to practice according to the Dutch OA guideline, which recommends the same 3 elements as e-Exercise: information, physical exercise, and strength and stability exercises.16 No restrictions were given with regard to the number of face-to-face sessions.
Outcomes and Follow-up
Participants received an online questionnaire and an accelerometer at baseline, after 12 weeks, and after 12 months. The physical therapist measured physical functioning objectively at baseline and after treatment. No financial incentives were offered to complete the measurements. In case of an unfilled questionnaire, a first reminder was sent after 10 days and a second reminder or a phone call after 15 days. A detailed description of outcome measures and interpretation are given in eAppendix 2 (available at academic.oup.com/ptj).
Primary outcome measures
Physical functioning was assessed subjectively with the subscale “function in daily living” of the Hip OA Outcome Score (HOOS) and/or the Knee Injury and OA Outcome Score (KOOS).18,19 A lower score on the sum score (0-100) indicates problems in physical functioning. Physical functioning was assessed by the physical therapists using the Timed “Up & Go” (TUG) test.20
Free-living PA was assessed subjectively with the Short QUestionnaire to Assess Health-Enhancing Physical Activity (SQUASH), a questionnaire that measures habitual PA during the preceding week.21 PA was objectively assessed using ActiGraph GT3x (ActiGraph, Pensacola, Florida) triaxial accelerometers. Participants were instructed to wear the accelerometer on a belt around their waist for 5 consecutive days, except during the night or when showering or swimming. Accelerometer data were eligible if patients had worn the meter at least 3 days, for 8 hours or more.22 PA thresholds of Freedson et al23 were used to distinguish sedentary activity and light, moderate, and vigorous PA. Moderate activity and vigorous activity were summed and divided by the number of wearing days to calculate a PA score in minutes per day.
Secondary outcome measures
Other symptoms and functional limitations were assessed with the HOOS and the KOOS, using 4 other subscales: pain, symptoms, sport/recreation function, and quality of life.18,19
Self-perceived effect was assessed by a single question about the degree of change in OA symptoms. Scores ranged from 1 (much better) to 6 (much worse).
Pain and tiredness were assessed using a numeric rating scale ranging from 0 (no pain/not tired) to 10 (worst possible pain/very tired).
Self-efficacy was assessed by the Arthritis Self-efficacy Scale (ASES), using the subscale “pain and symptoms.”24 Scores ranged from 1 to 5; a higher score indicates greater self-efficacy.
Other measures
Quantitative data about website usage, stored on the backend of the website, were used to analyze adherence to the online application. Usability was assessed using the System Usability Scale (SUS).25 A higher SUS score (range = 0–100) indicates better usability. For interpretation, a grading system introduced by Sauro and Lews26 was used. Physical therapists were asked to fill out a registration form about the number and content of face-to-face sessions.
Data Analysis
Descriptive statistics were used to describe patients’ general characteristics and the number and content of the physical therapy sessions. Frequencies, t tests, and chi-square tests were used to explore differences in demographics between both groups. Primary analysis was performed according to the intention-to-treat principle. Per-protocol analyses were performed for participants who adhered to the e-Exercise intervention and for all participants who received usual physical therapy. They were considered to be adhering to the intervention if they completed at least 8 of 12 modules.27
Multilevel repeated measures analyses were used to determine the short-term (3-month) and long-term (12-month) effectiveness of e-Exercise compared to usual physical therapy on primary and secondary outcome measures. The 3-level hierarchy consisted of repeated measurements (level 1), nested within participants (level 2), and nested within physical therapists (level 3). Analyses were controlled for the physical therapist, baseline values, sex, body mass index, level of education, and location of OA. Between-group effect sizes were calculated according to the Cohen d using the pooled standard deviation. Effect sizes of 0.2, 0.5, and 0.8 or larger were considered to represent small, medium, and large effects, respectively.28 According to the recommendations of Twisk et al29,30 about handling missing data in longitudinal mixed-model analyses, no imputation techniques were used. In order to investigate selective attrition, a nonresponse analysis with t tests and chi-square tests was performed by comparing general characteristics and primary baseline variables of responders and nonresponders at 3 and 12 months. For per-protocol analyses, participants who were adherent and completed ≥8 modules were compared with participants in the usual physical therapy group. Per-protocol analyses consisted of multilevel analyses controlling for the same variables as the primary analysis.
Sample size. The power calculation was based on a previous multicenter cluster-randomized controlled trial among patients with hip/knee OA8 and was performed for the primary outcome measure physical functioning (power = 0.8; alpha = .05). A target sample size of 200 participants was chosen to detect a small to medium effect size (0.2–0.4) in physical functioning at a 2-sided significance level of .05, anticipating a maximum loss to follow-up of 20% over the study period of 12 months. Because we had 4 primary outcome measures, we applied a Bonferroni correction. A 2-tailed significance level of .05/4 = .0125 was considered as statistically significant. Analyses were carried out using SPSS Statistics 23.0 (IBM SPSS, Chicago, Illinois).
Role of the Funding Source
This study was funded by ZonMw (ZonMw Research Program Sport, ref. no. 525001007), the Dutch Rheumatoid Arthritis Foundation, and the Royal Dutch Society for Physiotherapy. The funders played no role in the conduct of this study.
Results
Participants
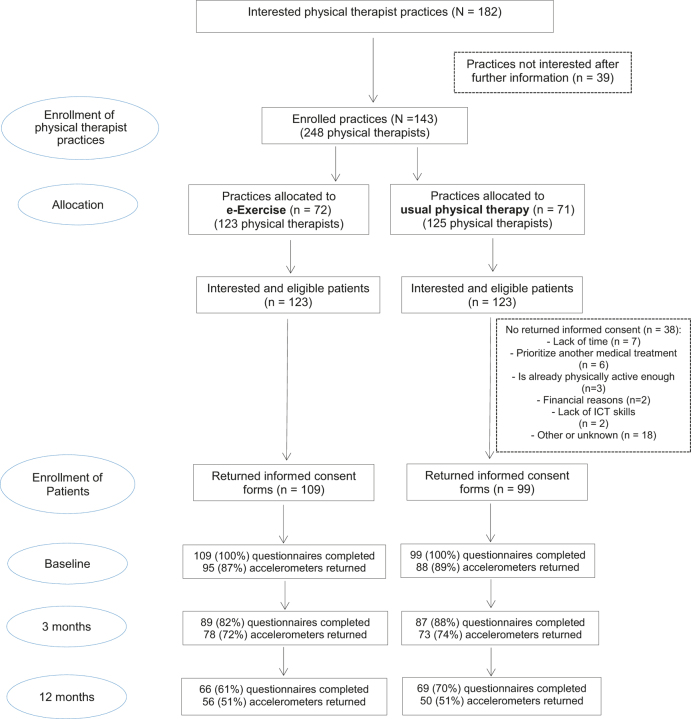
In total, 246 eligible people were included (Fig. 1). Thirty-eight people did not return informed consent after reading the participant information letter because of lack of time (n = 7), priority for another medical treatment (n = 6), a physically active lifestyle (n = 3), financial reasons (n = 2), a lack of information communication technology skills (n = 2), or other/unknown reasons (n = 18). From the physical therapist practices allocated to e-Exercise, 109 participants filled out the first questionnaire. From the physical therapist practices allocated to usual physical therapy, 99 participants completed the first questionnaire. The response rates for the follow-up questionnaire was 85% at 3 months (e-Exercise, n = 89; usual physical therapy, n = 87) and 65% at 12 months (e-Exercise, n = 66; usual physical therapy, n = 69). Eligible accelerometer data at baseline and after 3 months and 12 months were available for 88%, 73%, and 51% of the 208 participants, respectively. Demographics are shown in Table 1. The e-Exercise group consisted of more people with a low level of education (e-Exercise, 24.8%; usual physical therapy, 12.1%; P = .04) at baseline. No other differences in demographics were seen between groups. After 3 months, responders differed from nonresponders in body mass index (responders, 27.4 [SD = 4.4]; nonresponders, 29.0 [4.1]; P = .02). No statistical differences were seen between participants who wore the accelerometer and those who did not.
Figure 1.
Flow chart. ICT = information communication technology.
Table 1.
Demographics and Unadjusted Primary Outcome Measures for Participants at Baseline, 3 Months, and 12 Monthsa
| Baseline | 3 mo | 12 mo | ||||
|---|---|---|---|---|---|---|
| Measurement | e-Exercise | Usual Physical Therapy | e-Exercise | Usual Physical Therapy | e-Exercise | Usual Physical Therapy |
| No. of respondents | 109 | 99 | 89 | 87 | 66 | 69 |
| Sex | ||||||
| Women | 74 (67.9) | 67 (67.7) | 60 (67.4) | 57 (65.5) | 44 (66.7) | 44 (63.8) |
| Men | 35 (32.1) | 32 (32.3) | 29 (32.6) | 30 (34.5) | 22 (33.3) | 25 (36.2) |
| Age, y, mean (SD) | 63.8 (8.5) | 62.3 (8.9) | 63.6 (8.1) | 62.6 (9.1) | 64.1 (7.7) | 61.7 (8.8) |
| BMI, kg/m2, mean (SD) | 27.8 (4.2) | 27.9 (4.9) | 27.4 (4.4) | 27.7 (4.8) | 26.9 (4.2) | 27.7 (4.9) |
| Location of OA | ||||||
| Knee | 71 (65.1) | 67 (67.6) | 59 (66.3) | 58 (66.7) | 45 (68.2) | 48 (69.6) |
| Hip | 21 (19.3) | 17 (17.2) | 19 (21.3) | 16 (18.4) | 16 (24.2) | 12 (17.4) |
| Both | 17 (15.6) | 15 (15.2) | 11 (12.4) | 13 (14.9) | 5 (7.6) | 9 (13.0) |
| Duration of symptoms | ||||||
| <1 y | 21 (19.3) | 20 (20.2) | 14 (15.7) | 19 (21.8) | 11 (16.7) | 14 (20.3) |
| 1–5 y | 42 (38.5) | 38 (38.4) | 38 (42.7) | 33 (37.9) | 31 (47.0) | 31 (44.9) |
| ≥5 y | 46 (42.2) | 41 (41.4) | 37 (41.6) | 35 (40.2) | 24 (36.4) | 24 (34.8) |
| Education | ||||||
| Low | 27 (24.8) | 12 (12.1) | 23 (25.8) | 9 (10.3) | 17 (25.8) | 8 (11.6) |
| Middle | 41 (37.6) | 51 (51.5) | 35 (39.3) | 46 (52.9) | 26 (39.4) | 34 (49.3) |
| High | 41 (37.6) | 36 (36.4) | 31 (34.8) | 32 (36.8) | 23 (34.8) | 27 (39.1) |
| No. of comorbidities | ||||||
| 0 | 62 (56.9) | 62 (62.6) | 47 (52.8) | 53 (60.9) | 37 (56.1) | 40 (58.0) |
| 1 | 20 (18.3) | 20 (20.2) | 16 (18.0) | 18 (20.7) | 11 (16.7) | 15 (21.7) |
| ≥2 | 27 (24.8) | 17 (17.2) | 26 (29.2) | 16 (18.4) | 18 (27.3) | 14 (20.3) |
| Physical functioning, scores of 0–100, mean (SD) | 61.3 (18.3) | 55.5 (21.4) | 66.7 (18.2) | 62.2 (20.4) | 69.3 (18.7) | 65.3 (22.8) |
| Timed “Up & Go” test, s, mean (SD) | 8.4 (2.1) | 8.6 (5.8) | 7.3 (1.7) | 7.3 (2.4) | ||
| Physical activity, subjective, min/d, mean (SD) | 98.4 (118.4) | 107.0 (103.3) | 120.4 (111.0) | 131.4 (122.2) | 105.6 (97.2) | 125.8 (123.0) |
| Physical activity, objective, min/d, mean (SD) | 25.2 (23.1) | 22.5 (21.8) | 25.5 (17.7) | 25.5 (23.7) | 23.5 (19.9) | 25.3 (22.8) |
aData are reported as number (percentage) of participants unless otherwise indicated. BMI = body mass index, OA = osteoarthritis.
Content and Number of Physical Therapy Sessions
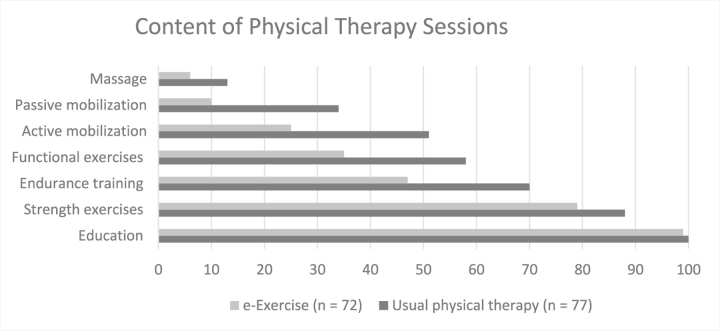
In total, 149 physical therapist registration forms were returned, 77 about participants who received usual physical therapy and 72 about participants who received e-Exercise. Figure 2 shows the content of physical therapy sessions of usual physical therapy and e-Exercise. Overall, physical therapists who applied usual physical therapy provided active and passive mobilizations, endurance training, and functional and strength exercises more often. Participants in the usual physical therapy group received 12 sessions (range = 2–29); participants in the e-Exercise group received, on average, 5 sessions (range = 2–16).
Figure 2.
Applied physical therapist interventions (percentages of participants who received the given interventions as part of their physical therapist treatment for osteoarthritis). e-Exercise = combination of physical therapist sessions with an online application.
Usability and Adherence
At 3 months, the average System Usability Score of 85 responders was 73.1 (SD = 18.6), which corresponds with a grade B usability. For 90 of 109 participants, adherence data were available. Of these participants, 73 (81.1%) completed at least 8 of 12 modules and were classified as “adherent.” A detailed overview of adherence to e-Exercise and related factors is published elsewhere.27
Short-Term Effectiveness
After 3 months, no statistically significant differences were seen between e-Exercise and usual physical therapy for the primary outcome measures of physical functioning and physical activity (Tab. 2) and the secondary outcome measures (Tab. 3). Within the usual physical therapy group, significant improvements were seen for physical functioning, the Timed “Up & Go” Test, subscales of the HOOS and the KOOS (pain, sport, and quality of life), the Numeric Rating Scale (NRS) for pain, and self-efficacy (subscales pain and symptoms). Within the e-Exercise group, significant improvements were seen for physical functioning, subjective PA, pain (NRS and HOOS/KOOS), tiredness, and self-efficacy (subscales pain and symptoms). The self-perceived effect of participants in the e-Exercise group was 3.1 (SD = 1.2), and that of participants in the usual physical therapy group was 3.1 (SD = 1.3); a score of 3 means “a little bit better.” The results of the per-protocol analyses showed that there were no statistically significant differences between the participants who were adherent in the e-Exercise group and those who were adherent in the usual physical therapy group (results not shown).
Table 2.
Adjusted Primary Outcome Measures: Improvements and Differences Within and Between Groups
| Outcome Measure | No. of Participants | e-Exercise, Mean (95% CI) | Within-Group Difference (P)a | No. of Participants | Usual Physical Therapy, Mean (95% CI) | Within-Group Difference (P)a | Difference in Difference, Mean (95% CI)b | Between-Group Difference (P)a | Between-Group Effect Size |
|---|---|---|---|---|---|---|---|---|---|
| Physical Functioning, Scores of 0–100 | |||||||||
| Baseline | 109 | 52.7 (47.3 to 58.0) | 99 | 50.7 (45.1 to 56.4) | |||||
| 3 mo | 87 | 56.8 (51.0 to 62.7) | <.01 | 87 | 56.3 (50.2 to 62.4) | <.01 | −1.4 (−5.6 to 2.8) | .52 | 0.01 |
| 12 mo | 65 | 59.8 (51.4 to 68.1) | <.01 | 69 | 58.0 (49.6 to 66.5) | <.01 | −0.2 (−6.4 to 6.0) | .95 | 0.04 |
| Timed “Up & Go” Test, s | |||||||||
| Baseline | 72 | 9.6 (8.1 to 11.1) | 74 | 9.8 (8.3 to 11.3) | |||||
| 3 mo | 68 | 8.5 (7.3 to 9.7) | .01 | 66 | 8.4 (7.1 to 9.7) | <.01 | 0.3 (−0.8 to 1.5) | .58 | 0.02 |
| Physical Activity,c Subjective, min/d | |||||||||
| Baseline | 109 | 126.7 (73.7 to 179.6) | 99 | 129.8 (73.8 to 185.9) | |||||
| 3 mo | 87 | 154.2 (100.2 to 208.1) | <.01 | 87 | 141.7 (85.0 to 198.4) | .26 | 15.7 (−13.4 to 44.7) | .26 | 0.04 |
| 12 mo | 65 | 193.1 (122.5 to 263.8) | .41 | 69 | 200.9 (129.5 to 272.4) | .22 | 4.6 (−27.9 to 37.2) | .78 | −0.02 |
| Physical Activity,c Objective, min/d | |||||||||
| Baseline | 95 | 35.4 (25.3 to 45.5) | 88 | 33.7 (23.1 to 44.3) | |||||
| 3 mo | 79 | 34.9 (24.7 to 45.1) | .78 | 72 | 35.0 (24.3 to 45.6) | .52 | −1.8 (−7.2 to 3.6) | .51 | 0.00 |
| 12 mo | 56 | 43.4 (30.1 to 56.8) | .28 | 50 | 44.6 (30.8 to 57.6) | .89 | 3.0 (−3.9 to 10.0) | .39 | −0.02 |
aAdjusted for baseline, sex, body mass index, level of education, pain, type of osteoarthritis, and physical therapist.
bDifference between baseline and 3 months in e-Exercise vs. usual physical therapy; difference between baseline and 12 months in e-Exercise vs. usual physical therapy. Baseline and 3-month data were extracted from short-term analyses; 12-month data were extracted from long-term analysis.
cModerate and vigorous intensities.
Table 3.
Adjusted Secondary Outcome Measures: Improvements and Differences Within and Between Groups
| Outcome Measure | No. of Participants | e-Exercise, Mean (95% CI) | Within-Group Difference (P)a | No. of Participants | Usual Physical Therapy, Mean (95% CI) | Within-Group Difference (P)a | Difference in Difference, Mean (95% CI)b | Between-Group Difference (P)a | Between-Group Effect Size |
|---|---|---|---|---|---|---|---|---|---|
| Pain, Scores of 0–100 | |||||||||
| Baseline | 109 | 50.4 (42.1 to 58.8) | 99 | 43.9 (35.2 to 52.7) | |||||
| 3 mo | 87 | 55.8 (47.3 to 64.3) | <.01 | 87 | 48.8 (39.9 to 57.7) | <.01 | 0.5 (−4.1 to 5.0) | .84 | 0.14 |
| 12 mo | 65 | 65.9 (54.3 to 77.5) | <.01 | 69 | 61.6 (49.9 to 73.4) | <.01 | −2.0 (−8.9 to 4.8) | .56 | 0.07 |
| Symptoms, Scores of 0–100 | |||||||||
| Baseline | 109 | 53.1 (45.9 to 60.4) | 99 | 51.2 (43.5 to 58.8) | |||||
| 3 mo | 87 | 54.2 (46.7 to 61.7) | .50 | 87 | 54.4 (46.5 to 62.3) | .05 | −2.1 (−6.6 to 2.4) | .35 | 0.00 |
| 12 mo | 65 | 56.7 (46.3 to 67.1) | <.01 | 69 | 62.1 (51.6 to 72.6) | .03 | −7.4 (−13.8 to −1.0) | .73 | −0.10 |
| Sport, Scores of 0–100 | |||||||||
| Baseline | 109 | 36.3 (39.2 to 50.8) | 99 | 39.7 (29.8 to 49.6) | |||||
| 3 mo | 87 | 39.3 (42.7 to 55.4) | .23 | 87 | 46.6 (36.1 to 57.1) | <.01 | −3.9 (−11.0 to 3.1) | .27 | −0.16 |
| 12 mo | 65 | 45.9 (32.5 to 59.3) | .05 | 69 | 49.1 (35.5 to 62.6) | .04 | 0 (−8.3 to 8.3) | .99 | −0.05 |
| Quality of Life, Scores from 0–100 | |||||||||
| Baseline | 109 | 45.0 (39.2 to 50.8) | 99 | 44.2 (38.1 to 50.4) | |||||
| 3 mo | 87 | 49.1 (42.7 to 55.4) | .02 | 87 | 53.0 (46.3 to 59.7) | <.01 | −4.7 (−9.5 to 0.2) | .06 | −0.10 |
| 12 mo | 65 | 52.5 (43.6 to 61.4) | <.01 | 69 | 56.1 (47.0 to 65.1) | <.01 | −4.3 (−10.3 to 1.8) | .16 | −0.08 |
| Sedentary Behavior, Objective, min/d | |||||||||
| Baseline | 95 | 495.5 (457.3 to 533.6) | 88 | 514.0 (474.1 to 553.9) | |||||
| 3 mo | 79 | 505.8 (466.5 to 545.0) | .19 | 72 | 498.3 (457.4 to 539.3) | .05 | 26.0 (3.9 to 48.1) | .02 | 0.03 |
| 12 mo | 56 | 521.0 (467.5 to 574.6) | .37 | 50 | 501.3 (447.0 to 555.7) | <.01 | 29.4 (10.3 to 48.6) | <.01 | 0.08 |
| Pain, Scores of 0–10 | |||||||||
| Baseline | 109 | 5.4 (4.3 to 6.4) | 99 | 6.1 (4.9 to 7.2) | |||||
| 3 mo | 87 | 4.1 (3.0 to 5.2) | <.01 | 87 | 5.3 (4.1 to 6.4) | <.01 | −0.5 (−1.1 to 0.2) | .16 | −0.18 |
| 12 mo | 65 | 3.8 (2.4 to 5.2) | <.01 | 69 | 4.0 (2.6 to 5.5) | <.01 | 0.4 (−0.5 to 1.3) | .40 | −0.03 |
| Tiredness, Scores of 0–10 | |||||||||
| Baseline | 109 | 6.1 (5.1 to 7.2) | 99 | 6.1 (5.1 to 7.2) | |||||
| 3 mo | 87 | 4.8 (3.8 to 5.8) | <.01 | 87 | 5.6 (4.5 to 6.7) | .02 | −0.8 (−1.4 to −0.1) | .02 | −0.13 |
| 12 mo | 65 | 5.6 (4.2 to 7.0) | <.01 | 69 | 5.6 (4.2 to 7.1) | <.01 | −0.1 (−0.9 to 0.8) | .84 | 0 |
| Self-efficacy for Pain, Scores of 1–5 | |||||||||
| Baseline | 109 | 3.6 (3.3 to 4.0) | 99 | 3.5 (3.2 to 3.9) | |||||
| 3 mo | 87 | 3.9 (3.6 to 4.3) | <.01 | 87 | 4.0 (3.6 to 4.4) | <.01 | −0.1 (−0.4 to 0.1) | .33 | −0.05 |
| 12 mo | 65 | 4.1 (3.6 to 4.6) | <.01 | 69 | 4.0 (3.5 to 4.5) | <.01 | 0 (−0.3 to 0.3) | .99 | 0.04 |
| Self-efficacy for Symptoms, Scores of 1–5 | |||||||||
| Baseline | 109 | 3.5 (3.1 to 3.8) | 99 | 3.4 (3.0 to 3.7) | |||||
| 3 mo | 87 | 3.7 (3.4 to 4.1) | <.01 | 87 | 3.8 (3.4 to 4.2) | <.01 | −0.2 (−0.4 to 0.1) | .20 | −0.05 |
| 12 mo | 65 | 3.7 (3.2 to 4.2) | <.01 | 69 | 3.7 (3.2 to 4.3) | <.01 | −0.1 (−0.4 to 0.1) | .29 | 0 |
| Pain Reported by Physical Therapist, Scores of 0–10 | |||||||||
| Baseline | 72 | 6.4 (5.5 to 7.3) | 74 | 6.6 (5.7 to 7.5) | |||||
| 3 mo | 69 | 4.2 (3.2 to 5.1) | <.01 | 73 | 4.5 3.6 to 5.5) | <.01 | −0.2 (−0.9 to 0.6) | .64 | −0.06 |
aAdjusted for baseline, sex, body mass index, level of education, pain, type of osteoarthritis, and physical therapist.
bDifference between baseline and 3 months in e-Exercise vs. usual physical therapy; difference between baseline and 12 months in e-Exercise vs. usual physical therapy. Baseline and 3-month data were extracted from short-term analyses; 12-month data were extracted from long-term analysis.
Long-Term Effectiveness
At the 12-month follow-up, no statistically significant differences were seen between groups for the primary outcome measures. For secondary outcome measures, a significant difference was seen on changes in sedentary behavior (usual physical therapy group, 29.4 min/d; e-Exercise, +8.3 min/d; P ≤ .01; effect size = 0.73). Within the usual physical therapy group, statistical significant improvements were seen on physical functioning, subscales of the HOOS and the KOOS (pain and quality of life), NRS pain, and NRS tiredness and self-efficacy (subscales pain and quality of life). Within the e-Exercise group, statistically significant improvements were seen on physical functioning, subscales of the HOOS and the KOOS (pain, symptoms, and quality of life), NRS pain, and NRS tiredness and self-efficacy (subscales pain and quality of life). The results are shown in Tables 2 and 3. The self-perceived effect of participants in the e-Exercise group was 3.4 (SD = 1.4), and that of participants in the usual physical therapy group was 3.1 (SD = 1.6). Long-term results of the per-protocol analyses showed that there were no statistically significant differences between the participants who were adherent in the e-Exercise group and those who were adherent in the usual physical therapy group (results not shown). The intraclass correlation coefficient (ICC) ranged from 0.0% to 1.4%.
Discussion
The aim of this multicenter superiority cluster-randomized controlled trial study was to investigate the short- and long-term effectiveness of e-Exercise compared to usual physical therapy in people with hip/knee OA. Because online applications can support people in exercise at home,13,31 we expected that e-Exercise would be more effective than usual physical therapy. The results of this randomized controlled study showed that there were no significant differences between the e-Exercise group and the usual physical therapy group with respect to physical functioning and free-living PA. However, within-group differences showed that both interventions were significantly effective with respect to physical functioning and most secondary outcomes soon after treatment and after 12 months. Notably, participants in the e-Exercise group visited the physical therapist 5 times, whereas the usual physical therapy group received, on average, 12 sessions. This reduction of face-to-face sessions might lead to a reduction in health care costs, which will be investigated in a future cost-effectiveness study.
Integrating face-to-face physical therapy with online applications is an upcoming field and, to our knowledge, this is the first randomized controlled trial evaluating the effectiveness of blended care in patients with hip/knee OA compared to usual physical therapy. The comparison of the average change in both treatment groups showed minimal differences, with small effect sizes in all primary and secondary outcome measures. To illustrate, participants improved, on average, 7.2 points for physical functioning (e-Exercise, +7.1; usual physical therapy, +7.3; effect size = 0.04; P = .95) and 16.1 points for pain (e-Exercise, +15.5; usual physical therapy, +17.7; effect size = 0.07; P = .56) as measured with the HOOS and the KOOS (on a 0–100 scale). If we would have used a noninferiority design, we probably would have specified a noninferiority margin of 0.5 × 0.3 = 0.15.2,3,32 Because all of our between-group effect sizes were below this value, e-Exercise and usual physical therapy are likely to be equally effective. These within-group effects are comparable to those found in other studies of exercise therapy for patients with hip/knee OA2,3 and underline the potential of blended care.
Although participants in the e-Exercise group reported a significant increase in PA after 3 months, in both groups, no significant improvements in objective PA were found. This result is in accordance with a recent meta-analysis that found no consistent evidence for improvement of objective PA in lower limb OA.33 Next to the difficulty of measuring free-living PA,34 an explanation in our trial might be participants’ high level of PA at baseline. Whereas PA was set as an inclusion criterion (administered during physical therapists’ anamnesis), baseline data show that participants already met the global recommendations for PA.35 Physical therapists might have underestimated participants’ level of PA, leading to a physically active study population with less room for improvement. In addition, a significant increase in sedentary behavior within the e-Exercise group compared to the usual physical therapy group was determined. Because sedentary behavior increases morbidity and mortality risk,36 we will include an information module about this topic within a future e-Exercise intervention. Taking into account the difficulty of changing PA and sedentary behavior, we also recommend combining e-Exercise with wrist-worn activity trackers for self-monitoring. At the same time, these trackers can be used for continuous measurement of intervention adherence.37,38
A remarkable difference between e-Exercise and usual physical therapy is the content of the physical therapy sessions. Physical therapists who applied e-Exercise provided, for a smaller proportion of participants, active and passive mobilizations, endurance training, and functional and strength exercises. A possible explanation is that participants in the e-Exercise group were extensively encouraged to take an active role in their treatment. A detailed description of patients’ and physical therapists’ experiences with e-Exercise is published elsewhere27 and also is provided in other data (C.J.J.K., D.B., H.J.d.V., D.H.d.B., et al, unpublished data, 2017).
Strengths and Limitations
The strength of this study is that we compared e-Exercise with usual physical therapy. This design made it possible to set up conclusions about the additional value of a blended delivery mode compared to face-to-face physical therapy. Unfortunately, we had to deal with high dropout rates: 15% after 3 months and 35% after 12 months. Percentages of missing data in our accelerometer data were even higher. We might have overloaded the participants with too many measurements. Although we did not find clinically relevant differences in baseline demographics between responders and nonresponders, results should be interpreted with caution. It is known that dropout rates in eHealth studies are accompanied with nonusage attrition.39 For future studies, we recommend the use of in-person survey visits because doing so might increase response rates and would also allow the measurement of objective physical functioning by an independent researcher.40 The final limitation is the discrepancy between our intended study population and the actual study population. Selection of patients was done by the physical therapists, and the clinical diagnosis of OA was not confirmed by an independent caregiver. Next, physical therapists assessed participants’ level of physical activity during anamneses with a single question. After analyses of the baseline data, it turned out that participants were already sufficiently physically active at baseline. On the one hand, it is a limitation that our inclusion strategy resulted in a physically active population that had less room for improvement on this outcome measurement during the intervention. On the other hand, our inclusion strategy has the advantage that it reflects physical therapists’ clinical reasoning process in daily practice. In the future, physical therapists will select patients for e-Exercise in the same way.
Clinical Implications and Future Directions
We recommend further elaboration of an instrument to determine patients’ suitability for a (partly) online intervention. In line with a stepped care strategy that promotes starting with relatively simple treatment modalities,41 patients could start with an unguided internet-delivered intervention like Join2Move.12 If this simple treatment modality appears to be inadequate, physical therapist guidance can be added (e-Exercise). In case of deterioration of symptoms or unsatisfying results, the frequency of face-to-face contact can be increased.41 In a future study we will describe the cost-effectiveness of e-Exercise compared to usual physical therapy from a societal perspective.
Conclusions
The blended intervention e-Exercise was not more effective than usual physical therapy in patients with hip/knee OA. Both interventions led to clinical improvements.
Supplementary Material
Author Contributions and Acknowledgments
Concept/idea/research design: C.J.J. Kloek, D. Bossen, J. Dekker, D.H. de Bakker, C. Veenhof
Writing: C.J.J. Kloek, D. Bossen, P.M. Spreeuwenberg, J. Dekker, C. Veenhof
Data collection: C.J.J. Kloek
Data analysis: C.J.J. Kloek, D. Bossen, P.M. Spreeuwenberg, C. Veenhof
Project management: C.J.J. Kloek, D. Bossen, D.H. de Bakker, C. Veenhof
Fund procurement: J. Dekker, D.H. de Bakker, C. Veenhof
Providing facilities/equipment: C. Veenhof
Consultation (including review of manuscript before submitting): D. Bossen, J. Dekker, P.M. Spreeuwenberg, C. Veenhof
The authors thank Prof Dr Jos W.R. Twisk for his advice in the statistical analysis.
Ethics Approval
The study design and protocol were approved by the Medical Ethical Committee of the St Elisabeth Hospital Tilburg, the Netherlands (Dutch Trial Register ref no. NTR4224).
Funding
The study is funded by ZonMw (ZonMw Research Program Sport, ref. no. 525001007), the Dutch Rheumatoid Arthritis Foundation, and the Royal Dutch Society for Physiotherapy.
Disclosures
The authors completed the ICJME Form for Disclosure of Potential Conflicts of Interest. The authors report no competing interests.
References
- 1. Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010; 26:355–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fransen M, McConnell S, Hernandez-Molina G, Reichenbach S. Exercise for osteoarthritis of the hip. Cochrane Database Syst Rev. 2014;CD007912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2015;1:CD004376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bijlsma JW, Berenbaum F, Lafeber FP. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377:2115–2126. [DOI] [PubMed] [Google Scholar]
- 5. Dekker J, ed. Exercise and Physical Functioning in Osteoarthritis: Medical, Neuromuscular and Behavioral Perspectives. New York: Spinger-Verlag; 2013. [Google Scholar]
- 6. McAlindon TE, Bannuru RR, Sullivan MC et al. . OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22:363–388. [DOI] [PubMed] [Google Scholar]
- 7. Nelson AE, Allen KD, Golightly YM, Goode AP, Jordan JM. A systematic review of recommendations and guidelines for the management of osteoarthritis: The chronic osteoarthritis management initiative of the U.S. bone and joint initiative. Semin Arthritis Rheum. 2014;43:701–712. [DOI] [PubMed] [Google Scholar]
- 8. Veenhof C, Koke AJ, Dekker J et al. . Effectiveness of behavioral graded activity in patients with osteoarthritis of the hip and/or knee: A randomized clinical trial. Arthritis Rheum. 2006;55:925–934. [DOI] [PubMed] [Google Scholar]
- 9. Wentzel J, van der Vaart R, Bohlmeijer ET, van Gemert-Pijnen JE. Mixing online and face-to-face therapy: How to benefit from blended care in mental health care. JMIR Ment Health. 2016;3:e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010;12:e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wood CE, Richardson M, Johnston M et al. . Applying the behaviour change technique (BCT) taxonomy v1: a study of coder training. Transl Behav Med. 2015;5:134–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bossen D, Veenhof C, Van Beek KE et al. . Effectiveness of a web-based physical activity intervention in patients with knee and/or hip osteoarthritis: randomized controlled trial. J Med Internet Res. 2013;15:e257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kelders SM, Kok RN, Ossebaard HC, Van Gemert-Pijnen JE. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J Med Internet Res. 2012;14:e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bossen D, Kloek C, Snippe HW, Dekker J, de Bakker D, Veenhof C. A blended intervention for patients with knee and hip osteoarthritis in the physical therapy practice: development and a pilot study. JMIR Res Protoc. 2016;5:e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kloek CJ, Bossen D, Veenhof C, van Dongen JM, Dekker J, de Bakker DH. Effectiveness and cost-effectiveness of a blended exercise intervention for patients with hip and/or knee osteoarthritis: study protocol of a randomized controlled trial. BMC Musculoskelet Disord. 2014;15:269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Peter WFH JM, Bloo H, Dekker-Bakker LMMCJ, Dilling RG, Hilberdink WK, Kersten-Smit C, de Rooij M, Veenhof C, Vermeulen HM, de Vos I, Vlieland TP. 2010 KNGF-richtlijn Artrose heup-knie. Ned Tijdschr voor Fysiotherapie 2010. [Google Scholar]
- 17. Altman R, Asch E, Bloch D et al. . Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29:1039–1049. [DOI] [PubMed] [Google Scholar]
- 18. de Groot IB, Favejee MM, Reijman M, Verhaar JA, Terwee CB. The Dutch version of the Knee Injury and Osteoarthritis Outcome Score: a validation study. Health Qual Life Outcomes. 2008;6:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. de Groot IB Reijman M, Terwee CB et al. . Validation of the Dutch version of the Hip disability and Osteoarthritis Outcome Score. Osteoarthritis Cartilage. 2007;15:104–109. [DOI] [PubMed] [Google Scholar]
- 20. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. [DOI] [PubMed] [Google Scholar]
- 21. Wendel-Vos GC, Schuit AJ, Saris WH, Kromhout D. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity. J Clin Epidemiol. 2003;56:1163–1169. [DOI] [PubMed] [Google Scholar]
- 22. Hart TL, Swartz AM, Cashin SE, Strath SJ. How many days of monitoring predict physical activity and sedentary behaviour in older adults? Int J Behav Nutr Phys Act. 2011;8:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30:777–781. [DOI] [PubMed] [Google Scholar]
- 24. Taal E, Riemsma RP, Brus HL, Seydel ER, Rasker JJ, Wiegman O. Group education for patients with rheumatoid arthritis. Patient Educ Couns. 1993;20:177–187. [DOI] [PubMed] [Google Scholar]
- 25. Brooke J. Sus—a quick and dirty usability scale. Usability Evaluation in industry 1996. [Google Scholar]
- 26. Sauro JL, Lewis J. Quantifying the User Experience: Practical Statistics for User Research. San Francisco, California; 2012. [Google Scholar]
- 27. De Vries HJ, Kloek CJJ, de Bakker DH, Dekker J, Bossen D, Veenhof C. Determinants of adherence to the online component of a blended intervention for patients with hip and/or knee osteoarthritis: a mixed methods study embedded in the e-Exercise trial. Telemed J E Health. 2017;23:1002–1010. [DOI] [PubMed] [Google Scholar]
- 28. Cohen J. Statistical Power Analysis for the Behavioral sciences. Hillsdale, NJ: L Erlbaum Associates; 1988. [Google Scholar]
- 29. Twisk J, de Vente W. Attrition in longitudinal studies. How to deal with missing data. J Clin Epidemiol. 2002;55:329–337. [DOI] [PubMed] [Google Scholar]
- 30. Twisk J, de Boer M, de Vente W, Heymans M. Multiple imputation of missing values was not necessary before performing a longitudinal mixed-model analysis. J Clin Epidemiol. 2013;66:1022–1028. [DOI] [PubMed] [Google Scholar]
- 31. Pietrzak E, Cotea C, Pullman S, Nasveld P. Self-management and rehabilitation in osteoarthritis: is there a place for internet-based interventions? Telemed J E Health. 2013;19:800–805. [DOI] [PubMed] [Google Scholar]
- 32. Greene CJ, Morland LA, Durkalski VL, Frueh BC. Noninferiority and equivalence designs: issues and implications for mental health research. J Trauma Stress. 2008;21:433–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Williamson W, Kluzek S, Roberts N et al. . Behavioural physical activity interventions in participants with lower-limb osteoarthritis: a systematic review with meta-analysis. BMJ Open. 2015;5:e007642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kelly P, Fitzsimons C, Baker G. Should we reframe how we think about physical activity and sedentary behaviour measurement? Validity and reliability reconsidered. Int J Behav Nutr Phys Act. 2016;13:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Organization WH Global recommendations on physical activity for health. 2010. [PubMed] [Google Scholar]
- 36. Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38:105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cadmus-Bertram L. Using Fitness Trackers in Clinical Research: What Nurse Practitioners Need to Know. J Nurse Pract. 2017;13:34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Mercer K, Li M, Giangregorio L, Burns C, Grindrod K. Behavior change techniques present in wearable activity trackers: a critical analysis. JMIR Mhealth Uhealth. 2016;4:e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Eysenbach G. The law of attrition. J Med Internet Res. 2005;7:e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Christensen AI, Ekholm O, Glumer C, Juel K. Effect of survey mode on response patterns: comparison of face-to-face and self-administered modes in health surveys. Eur J Public Health. 2014;24:327–332. [DOI] [PubMed] [Google Scholar]
- 41. Smink AJ, van den Ende CH, Vliet Vlieland TP et al. . “Beating osteoARThritis”: development of a stepped care strategy to optimize utilization and timing of non-surgical treatment modalities for patients with hip or knee osteoarthritis. Clin Rheumatol. 2011;30:1623–1629. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.