Ongoing alcohol, drug and psychiatric problems after completing treatment were associated with increased odds of low social status (unemployment, unstable housing and/or living in high-poverty neighborhood) over 7 years. The impact of drug problems declined over time, and there were small, delayed benefits of AA attendance on social status.
Abstract
Purpose
We examined whether alcohol-dependent individuals with sustained substance use or psychiatric problems after completing treatment were more likely to experience low social status and whether continued help-seeking would improve outcomes.
Short summary
Ongoing alcohol, drug and psychiatric problems after completing treatment were associated with increased odds of low social status (unemployment, unstable housing and/or living in high-poverty neighborhood) over 7 years. The impact of drug problems declined over time, and there were small, delayed benefits of AA attendance on social status.
Method
Alcohol-dependent individuals sampled from public and private treatment programs (N = 491; 62% male) in Northern California were interviewed at treatment entry and 1, 3, 5 and 7 years later. Random effects models tested relationships between problem severity (alcohol, drug and psychiatric problems) and help-seeking (attending specialty alcohol/drug treatment and Alcoholics Anonymous, AA) with low social status (unemployment, unstable housing and/or living in a high-poverty neighborhood) over time.
Results
The proportion of participants experiencing none of the indicators of low social status increased between baseline and the 1-year follow-up and remained stable thereafter. Higher alcohol problem scores and having any drug and/or psychiatric problems in the years after treatment were associated with increased odds of low social status over time. An interaction of drug problems with time indicated the impact of drug problems on social status declined over the 7-year period. Both treatment-seeking and AA attendance were associated with increased odds of low social status, although lagged models suggested there were small, delayed benefits of AA attendance on improved social status over time.
Conclusion
Specialty addiction treatment alone was not sufficient to have positive long-term impacts on social status and social integration of most alcohol-dependent people.
INTRODUCTION
Long-term consequences of alcohol use disorders (AUD) and drug use disorders (DUD) can include downward social migration and loss of social status, also known as ‘downward drift’. Indicators of low social status that may be consequences of AUD and DUD include unemployment (Braun et al., 2000; Compton et al., 2014; French et al., 2011), incarceration (Tsai et al., 2013), poverty (Buu et al., 2007) and homelessness (Johnson et al., 1997; McVicar et al., 2015). Some studies suggest the drift phenomenon may be more acute for heavy users of illicit drugs than for heavy drinkers (Compton et al., 2014; Johnson et al., 1997). In this study, we examine effects of both alcohol and drug problems on social status over time.
Prior research suggests many negative sequelae of untreated or ongoing substance use disorders (SUD). In cross-sectional analyses using data from the US National Surveys on Drug Use and Health, Compton and colleagues (2014) found robust associations of alcohol and other drug use with unemployment. They also used retrospective data to assess whether drug use was associated with future unemployment and found cannabis use predicted subsequent job loss. Using data from people ages 25–60 who responded to both Wave I and Wave II of the National Epidemiologic Survey on Alcohol and Related Conditions, French and colleagues (2011) employed fixed effects regression models to examine impacts of alcohol use and AUD on job loss and sustained unemployment over a 3-year period. They found weekly heavy drinking (4+ drinks for women/5+ drinks for men per episode) was associated with women’s job loss and AUD was associated with sustained unemployment for both women and men.
Associations with SUD are similar for other indicators of low social status. In comparisons of incarcerated and general-population veterans, Tsai and colleagues (2013) noted that incarcerated veterans were more likely to have SUD than the general population of veterans, and this was particularly acute for African American and Hispanic veterans. Regarding associations of AUD and poverty, Buu et al. (2007) found that after conviction for driving under the influence, men with ‘active’ AUD were more likely to either stay in or move to a disadvantaged neighborhood over a 12-year period than their DUI-convicted peers who never had AUD or who were in remission from AUD. Finally, two studies of homelessness provide strong evidence that SUD is associated with subsequent homelessness (Johnson et al., 1997; McVicar et al., 2015), and that current homelessness also contributes to SUD (Johnson et al., 1997). Johnson and colleagues (1997) noted that DUD was more strongly associated with homelessness in their sample from Chicago, IL USA, than was AUD, but the findings of McVicar and colleagues (2015) suggest more prominent effects of AUD, rather than DUD, on subsequent homelessness in their Australian sample.
For people with SUD, treatment can significantly improve substance use outcomes (Gerstein and Lewin, 1990; Moos and Moos, 2003). Because relapse after treatment is common, repeated treatment episodes can help promote long-term recovery (Hser et al., 1997; Mertens et al., 2005). Involvement with self- and mutual-help groups such as Alcoholics Anonymous (AA) also can significantly improve substance use outcomes over time (Gossop et al., 2008; Kaskutas, 2009; Moos and Moos, 2006), particularly in combination with formal treatment (Fiorentine and Hillhouse, 2000; Moos and Moos, 2006; Witbrodt et al., 2014). Less is known about the benefits of addiction treatment or mutual-help groups for social integration and social status, particularly in the absence of specialized support services (or wraparound services) to assist with employment, housing, education, psychiatric and other client needs. These problems may be particularly long-lasting and resistant to change: an analysis of the Combining Medications and Behavioral Interventions (COMBINE) Study documented long-term (up to 52 weeks) improvements in mental health and quality of life but the proportion of days paid for working did not show similar improvement in the year after completing treatment (LoCastro et al., 2009). Unfortunately, many treatment agencies do not effectively incorporate these essential support services in their programs (Paino et al., 2016; Polcin, 2016) and those programs which do address ancillary issues such as homelessness often only provide temporary support (Kertesz et al., 2009). An additional limitation of the existing literature is that many studies do not assess secondary treatment outcomes such as social status over a long time period.
To build on prior work, in the present study we examine longitudinal effects of alcohol, drug and psychiatric problems on low social status in a sample of alcohol-dependent individuals followed for 7 years after they completed AUD treatment. Based on extant literature, we hypothesized that, after completing treatment, individuals with sustained substance use or psychiatric problems would be more likely to experience low social status over time. We also expected individuals who continued to receive help (either from formal treatment or from AA) would experience better social status outcomes.
METHOD
This secondary analysis uses data from a sample of alcohol-dependent individuals recruited when entering public and private alcohol treatment programs in a Northern California County (USA). Original data collection and the subsequent study which added information on the neighborhood context over the longitudinal study period both received approval from the Institutional Review Board of the Public Health Institute, Oakland, CA. All respondents gave their informed consent prior to their inclusion in the longitudinal interview study, and the study was conducted in accordance with the ethical standards established in the 1964 Declaration of Helsinki and its later amendments.
Sample
Programs included ten first-line programs focused on treating AUD (i.e. stand-alone aftercare and methadone programs were excluded) and that had a least one intake per week. During the study period, the county represented a socially and culturally diverse population (~900,000 county residents at time of recruitment) with a mix of urban, suburban and rural areas that reflected national patterns in the relationship of substance use to other health and social problems (Weisner and Schmidt, 1995). A total of 926 clients agreed to be in the study (80% participation rate) and provided informed consent. One-, 3-, 5- and 7-year follow-ups were conducted using computer-assisted-telephone interviews. Response rates (based on the baseline sample) were 78%, 75%, 72% and 67% at respective follow-ups. More details on initial study recruitment procedures are provided elsewhere (Weisner and Schmidt, 1995).
For this paper, we included all clients who were alcohol dependent at baseline (N = 491). The Diagnostic Interview Schedule for Psychoactive Substance Dependence, which operationalizes the seven DSM-IV dependence criteria (American Psychiatric Association, 2000), was used to determine baseline dependence (Robins et al., 1991).
Measures
Outcome variable (time-varying)
Social status was measured at the time of each interview. Unstable housing was defined as living in a rooming house, hotel, jail, prison, other institutional setting or being homeless. Unemployment was defined as having no part- or full-time employment. Neighborhood disadvantage was defined as living in a neighborhood where 15% or more of the residents had annual incomes below national poverty standards. This variable was based on national tract-level data from the 2000 US Decennial Census. A composite variable was created to capture whether an individual met one or more of the three conditions at each interview (coded as low social status versus none of the conditions).
Predictor variables (time-varying)
Addiction Severity Index (ASI) was used to assess past-30-day problem severity for each follow-up period in three domains: alcohol, drug and psychiatric problems (McLellan et al., 1992). The ASI uses key items to produce a continuous composite score for each problem domain (range 0–1, with higher scores designating greater severity). Most studies have shown the ASI to be a reliable and valid instrument (Mäkelä, 2004; McLellan et al., 1992). For these analyses of alcohol-dependent treatment clients, we used the continuous ASI alcohol problem score for each follow-up period. Due to a high number of zeroes and highly skewed data, we used dichotomous indicators to capture co-morbid drug and psychiatric problems (coded as ASI score = 0 versus any indication of problems = 1).
Help-seeking included the number of AA meetings attended during the prior 12 months (range 0–365, capped to signify at most one meeting per day) and any substance use treatment (versus none) in the prior 12 months. At baseline, treatment referred to lifetime treatment received prior to the index (recruitment) episode, and at the 1-year follow-up, treatment only included additional treatment not received as part of the index treatment episode. Treatment could include services received at inpatient care, recovery/residential homes, detoxification or outpatient programs.
Control variables (time-invariant)
Multivariate models were used to control for several demographic characteristics. Gender (female as the reference group), education (less than a high school diploma compared with high school diploma or higher as the reference), marital status (single—including divorced or widowed with never married—compared with married or partnered as the reference), and ethnicity (minority race/ethnicity compared with Caucasian as the reference) were included in all adjusted models.
A nominal variable was used to denote the type of treatment program from which each individual was recruited. Outpatient programs included two sites in a Health Maintenance Organization offering long-term outpatient treatment (used as the reference group) and two public outpatient programs. Inpatient programs included two fee-for-service private hospital programs offering short-term detoxification and inpatient care, as well as two public, gender-specific and long-term residential programs. There also were two public detoxification sites.
Analysis
Longitudinal, logistic random intercept models (Twisk, 2013) that specified both linear and quadratic effects for time were used to estimate the effects of problem severity and help-seeking on social status over time. Random effects models were chosen for these longitudinal data because they efficiently account for correlation between observations of repeated measures (Hu et al., 1998), they work well for balanced designs with limited follow-up points, and they allow for data missing at follow-up points (Twisk, 2013). Compared with general estimating equation models, allowing for random effects also provides more appropriate modeling of individual development over time (Twisk, 2013). Interactions of a focal predictor with the time variables were used to assess changes in the impact of the predictor on the outcome over the 7-year study period. In this context, the main effect can be interpreted as an effect of the predictor on the intercept of the trajectory of social status over time and the interactions represent effects of the predictor on the linear or quadratic slope of the outcome trajectories.
A stepwise approach was taken to estimate a final and most parsimonious model. First, the effects of time (linear and quadratic terms) were included in unadjusted models. Then, models adjusted for the background control variables. Next, main effects and interactions of time and quadratic time with alcohol, drug and psychiatric problems and with the help-seeking variables were added to the adjusted model (results not shown). In the final reduced model, all non-significant (P>0.10) interactions with time were excluded. In sensitivity analyses, the final reduced model was estimated separately for each of the three variables used to create the composite outcome. Then, despite the spacing of the follow-up interviews (2 years between assessments after the 1-year follow-up), we also ran models using lagged predictor variables; these models excluded cases with missing data and did not include interactions with time. All analyses were conducted in Stata, Version 14 (StataCorp., 2015).
RESULTS
Descriptive Analysis
The sample (N = 491) was 38% female and 20% had less than a high school degree, 43% reported minority race/ethnicity race/ethnicity and 33% were married/partnered at baseline. Mean baseline alcohol, drug and psychiatric problem severity scores (and standard deviations) were 0.588 (0.246), 0.112 (0.131) and 0.451 (0.234), respectively. A high proportion (43%) met criteria for both drug and alcohol dependence at baseline.
More than half of the sample (56%) was interviewed at all four follow-up waves (75% at two or more waves, with an average of 3.8 interviews per person). Compared with those interviewed at all four waves, those not interviewed at all waves were significantly (P < 0.05) more likely to be male, unemployed, single, without a high school diploma and in unstable living situations at the baseline interview. Greater baseline alcohol problem severity, but not drug or psychiatric problem severity, also was associated with loss-to-follow-up.
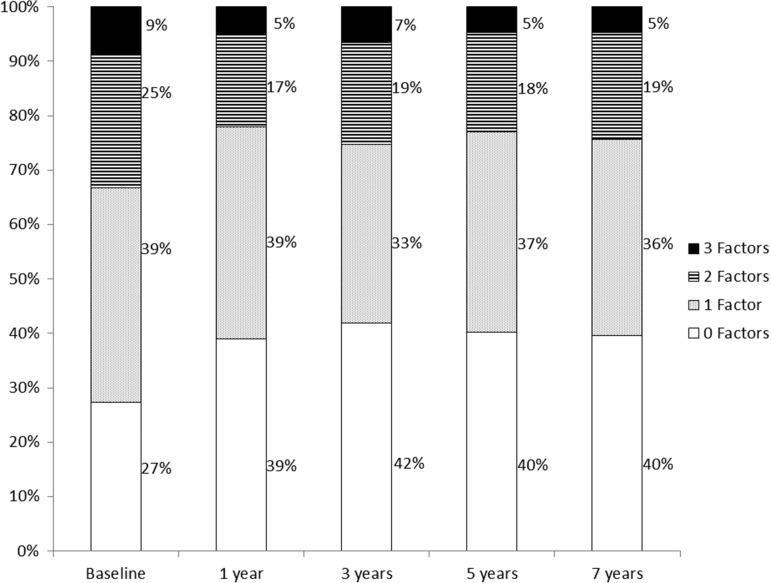
Figure 1 displays the number of participants who experienced zero (bottom portion of bars), one, two or three (top portion of bars) of the social status factors (i.e. being unstably housed, being unemployed and/or living in a disadvantaged neighborhood) at each wave. The proportion of those experiencing none of these factors increased between baseline and the 1-year follow-up and remained fairly stable thereafter; the proportions experiencing two or three factors appeared to decrease at this same point in the study. The proportion of those experiencing one factor remained stable after the 1-year follow-up. Odds of low social status decreased over time primarily due to changes in unemployment and unstable living conditions, rather than to changes in neighborhood poverty (with the latter being more stable over time).
Fig. 1.
Prevalence of low social status over time.
Table 1 shows predictor and control variables included in the longitudinal models across levels of the dependent variable (low social status) at each interview period. Problem severity (especially drug and psychiatric problems) and treatment attendance were strongly associated with the outcome at every wave, as were the demographic control variables (excluding gender). In addition, post-baseline alcohol problem severity was higher for those meeting at least one criterion for low social status (P < 0.05 at three waves). Prior AA attendance was associated with social status at baseline but attendance differences were not significantly different at subsequent waves. Correlations among key study variables are presented in Table 2.
Table 1.
Problem severity, help-seeking and demographics by social status over time
| Low social statusa | Baseline | 1-Year follow-up | 3-Year follow-up | 5-Year follow-up | 7-Year follow-up | |
|---|---|---|---|---|---|---|
| Sample size (%) | 0 | 127 (26) | 149 (39) | 153 (42) | 137 (40) | 124 (39) |
| 1+ | 364 (74) | 235 (61) | 214 (58) | 207 (60) | 190 (61) | |
| ASI alcohol, mean (SD) | 0 | 0.578 (0.252) | 0.131 (0.187) | 0.110 (0.170) | 0.106 (0.175) | 0.076 (0.133) |
| 1+ | 0.590 (0.246) | 0.203 (0.251)** | 0.136 (0.213) | 0.152 (0.223)* | 0.139 (0.211)** | |
| ASI drug, mean (SD) | 0 | 0.051 (0.091) | 0.026 (0.051) | 0.026 (0.051) | 0.024 (0.048) | 0.029 (0.055) |
| 1+ | 0.137 (0.136)*** | 0.064 (0.096)*** | 0.048 (0.087)** | 0.054 (0.090)** | 0.052 (0.085)** | |
| % Any drug problem | 0 | 44.9 | 39.6 | 41.8 | 37.2 | 47.6 |
| 1+ | 70.9*** | 49.8* | 43.0 | 49.8* | 54.2 | |
| ASI psychiatric, mean (SD) | 0 | 0.415 (0.215) | 0.155 (0.216) | 0.164 (0.190) | 0.176 (0.184) | 0.126 (0.171) |
| 1+ | 0.466 (0.237)* | 0.263 (0.238)*** | 0.275 (0.247)*** | 0.271 (0.229)*** | 0.272 (0.245)*** | |
| % Any psychiatric problem | 0 | 88.2 | 45.0 | 58.8 | 61.3 | 46.8 |
| 1+ | 90.1 | 73.2*** | 66.4 | 71.0 | 67.4*** | |
| % Went to AA in prior 12 months | 0 | 51.2 | 63.0 | 48.7 | 41.6 | 38.7 |
| 1+ | 71.8*** | 69.3 | 50.7 | 39.6 | 46.6 | |
| AA meeting attendance in prior 12 months, mean (SD) | 0 | 11.38 (33.5) | 73.88 (106.3) | 46.03 (85.7) | 36.02 (73.7) | 38.79 (83.2) |
| 1+ | 32.84 (60.3)*** | 74.36 (104.3) | 34.66 (70.4) | 31.20 (72.1) | 23.26 (55.5) | |
| % Went to treatmentb | 0 | 55.1 | 29.5 | 18.3 | 16.2 | 11.3 |
| 1+ | 75.1*** | 47.7*** | 38.5*** | 25.6* | 22.1** | |
| % Female | 0 | 33.9 | 43.6 | 41.8 | 45.3 | 42.7 |
| 1+ | 38.2 | 41.7 | 40.7 | 39.6 | 41.6 | |
| % Less than high school diploma/GED | 0 | 7.9 | 9.4 | 11.1 | 11.0 | 10.5 |
| 1+ | 24.5*** | 22.6*** | 23.4*** | 20.3* | 21.6** | |
| % Minority race/ethnicity | 0 | 26.0 | 24.8 | 29.4 | 32.9 | 31.5 |
| 1+ | 48.8*** | 47.4*** | 50.2*** | 48.5*** | 52.4*** | |
| % Married/partnered | 0 | 50.4 | 48.3 | 43.8 | 43.1 | 46.0 |
| 1+ | 28.0*** | 29.8*** | 31.8* | 33.3 | 34.2* |
SD, standard deviation; ASI, alcohol severity index; AA, Alcoholics Anonymous; GED, high school diploma equivalent; significance levels for bivariate comparisons of those with and without an indicator of low social status: *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001. aSum of three social status indicators: living in a low poverty neighborhood, living in unstable housing situation and being unemployed (dichotomized as 0 versus 1+). bTreatment use at baseline was assessed for lifetime prior to recruitment episode and for past year thereafter.
Table 2.
Correlations among time-varying values for key study variables
| (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Low social status | 1 | 1 | 0.311* | 0.011 | −0.236* | 0.322* | 0.157* | 0.202* | 0.270* | −0.019 | 0.332* |
| (2) Unstable housing | 0.488* | 0.316* | 0.210* | 0.322* | −0.417* | 0.287* | 0.095* | 0.186* | 0.196* | 0.038 | 0.448* |
| (3) Unemployed | 1 | 0.273* | 0.332* | −0.057 | −0.232* | 0.128* | 0.178* | 0.236* | 0.267* | −0.004 | 0.302* |
| (4) High-poverty neighborhood | 1 | 0.267* | 0.152* | −0.158* | 0.574* | 0.027 | 0.112* | 0.150* | −0.038 | 0.150* | |
| (5) Low educationa | 1 | −0.056 | −0.094* | 0.302* | 0.043 | 0.154* | 0.162* | −0.077* | 0.076 | ||
| (6) Maleb | 1 | −0.014 | 0.166* | 0.013 | 0.020 | −0.103* | −0.024 | 0.117* | |||
| (7) Married/partneredc | 1 | −0.134* | −0.011 | −0.160* | −0.109* | −0.055* | −0.094* | ||||
| (8) Minority race/ethnicityb,d | 1 | −0.061* | 0.127* | 0.062 | −0.046* | 0.058 | |||||
| (9) ASI alcohol problems | 1 | 0.202* | 0.343* | −0.115* | 0.381* | ||||||
| (10) Any co-morbid drug problemse | 1 | 0.459* | −0.053* | 0.207* | |||||||
| (11) Any co-morbid psychiatric problemse | 1 | −0.037 | 0.345* | ||||||||
| (12) # AA meetings attended | 1 | 0.152* | |||||||||
| (13) Returned to alcohol treatmentf | 1 |
Tetrachoric correlations among dichotomous indicators; Pearson's correlations for continuous variables indicated with italics.
*P < 0.05
aReferent: At least a high school diploma or GED.
bBaseline value (not time-varying).
cReferent: Single, divorced or widowed.
dReferent: White/Caucasian.
eReferent: No problems.
fReferent: Did not go to treatment in past year.
Random Effects Models
Table 3 displays results from the stepwise models for the composite outcome. In the unadjusted model (Model 1), time was significantly and inversely related to low social status, while time-squared was significantly and positively related to low social status. However, in the final adjusted model (Model 3) neither the linear nor quadratic main effects of time were significant, indicating social status did not change significantly from baseline to year 7 after controlling for the effects of problem severity, help-seeking and demographic characteristics. Greater alcohol problem severity (adjusted odds ratio [AOR] = 2.59) and co-morbid drug (AOR = 2.71) and psychiatric (AOR = 1.48) problems were associated with low social status (Model 3; P ≤ 0.10 for all). AA attendance and returning to treatment also were associated with low social status over time. Significant interactions of drug problem severity and AA meeting attendance with time indicated that the impact of these variables declined over the 7-year period. In the final model, demographic control variables (less education, female gender, minority race/ethnicity and index treatment program type) remained significantly related to social status across models, with patients recruited from detoxification sites and inpatient programs showing worse outcomes than outpatient clients over time.
Table 3.
Adjusted odds ratios and 95% confidence intervals from stepwise random effect models of time, demographics, problem severity and service utilization regressed on composite indicator of low social status across waves
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Time | 0.580** | (0.469–0.718) | 0.603** | (0.487–0.745) | 1.003 | (0.762–1.322) |
| Time-squared | 1.070** | (1.037–1.104) | 1.065** | (1.032–1.099) | 1.024 | (0.987–1.061) |
| Effects on intercept | ||||||
| Less than high school educationa | 3.423** | (1.556–7.527) | 3.380** | (1.491–7.662) | ||
| Male | 0.588+ | (0.329–1.054) | 0.517* | (0.282–0.947) | ||
| Married/partneredb | 0.569+ | (0.315–1.027) | 0.558+ | (0.304–1.027) | ||
| Minority race/ethnicityc | 2.354** | (1.296–4.272) | 2.417** | (1.304–4.481) | ||
| Type of treatment program at recruitmentd | ||||||
| Other outpatient | 1.130 | (0.490–2.603) | 1.044 | (0.443–2.462) | ||
| Hospital inpatient | 7.798** | (3.633–16.74) | 6.679** | (3.018–14.78) | ||
| Long-term residential | 4.925** | (1.667–14.55) | 4.724** | (1.548–14.41) | ||
| Detoxification | 21.480** | (7.907–58.36) | 18.150** | (6.486–50.79) | ||
| ASI alcohol problem severity | 2.586* | (1.156–5.785) | ||||
| Any drug problemse | 2.707** | (1.607–4.558) | ||||
| Any psychiatric problemse | 1.476+ | (0.999–2.180) | ||||
| # of AA meetings attended past year | 1.004* | (1.000–1.007) | ||||
| Went to treatment in past yearf | 2.122** | (1.443–3.121) | ||||
| Effects on linear slopeg | ||||||
| Any drug problems | 0.821** | (0.726–0.928) | ||||
| # of AA meetings attended past year | 0.999** | (0.998–1.000) | ||||
| Constant | 7.362** | (4.899–11.06) | 2.070* | (1.069–4.007) | 0.358* | (0.150–0.852) |
| /lnsig2u | 2.080 | (1.784–2.376) | 1.716 | (1.407–2.030) | 1.756 | (1.437–2.070) |
| sigma_u | 2.830 | (2.442–3.280) | 2.358 | (2.020–2.750) | 2.406 | (2.052–2.820) |
| Rho | 0.709 | (0.644–0.766) | 0.628 | (0.554–0.700) | 0.638 | (0.561–0.710) |
| Observations | 1,900 | 1,895 | 1,855 | |||
| Number of cases | 491 | 490 | 488 | |||
*P < 0.05, **P < 0.01, +P < 0.1.
aReferent: At least a high school diploma or GED.
bReferent: Single, divorced or widowed.
cReferent: White/Caucasian.
dReferent: HMO Outpatient.
eReferent: No problems.
fReferent: Did not go to treatment in past year.
g Note: Interaction with Time.
Results of random effects models for the three separate factors comprising the composite social status variable (Table 4) showed that the relationship between alcohol problem severity and social status was driven primarily by the association between alcohol problems and unemployment (AOR = 2.33); alcohol problem severity was not significantly related to unstable housing or living in a high-poverty neighborhood. Drug problem severity also was only significantly related to unemployment, and psychiatric problem severity was not associated with any of the three indicators of social status. As with the composite outcome variable, there were significant interactions of drug problem severity and AA meeting attendance with time when predicting unemployment. Returning to treatment was associated with higher odds of both unemployment and unstable housing. The strongest predictors of living in a high-poverty neighborhood were minority race/ethnicity (AOR = 28.61) and being recruited from a detoxification program (AOR = 10.97).
Table 4.
Adjusted odds ratios and 95% confidence intervals from random effect models of time, demographics, problem severity and service utilization regressed on three indicators of low social status across waves
| Unstable housing | Unemployed | High-poverty neighborhood | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Time | 1.032 | (0.744–1.431) | 0.941 | (0.738–1.200) | 1.109 | (0.791–1.554) |
| Time-squared | 0.994 | (0.952–1.038) | 1.024 | (0.992–1.057) | 0.994 | (0.951–1.038) |
| Effects on intercept | ||||||
| Less than high school educationa | 1.514 | (0.881–2.601) | 4.214** | (2.253–7.882) | 3.678* | (1.300–10.41) |
| Male | 2.608** | (1.573–4.323) | 0.503** | (0.314–0.805) | 1.873 | (0.795–4.416) |
| Married/partneredb | 0.330** | (0.188–0.580) | 0.646+ | (0.400–1.043) | 0.622 | (0.256–1.514) |
| Minority race/ethnicityc | 1.672* | (1.031–2.714) | 0.976 | (0.607–1.570) | 28.610** | (11.69–70.01) |
| Type of treatment program at recruitmentd | ||||||
| Other outpatient | 3.557** | (1.496–8.457) | 1.297 | (0.645–2.610) | 0.954 | (0.246–3.701) |
| Hospital inpatient | 5.468** | (2.685–11.14) | 6.633** | (3.579–12.30) | 2.542+ | (0.869–7.432) |
| Long-term residential | 18.070** | (7.485–43.61) | 4.782** | (1.996–11.46) | 2.107 | (0.453–9.793) |
| Detoxification | 17.220** | (8.099–36.62) | 8.842** | (4.247–18.41) | 10.970** | (3.061–39.35) |
| ASI alcohol problem severity | 1.059 | (0.471–2.384) | 2.329* | (1.187–4.567) | 1.394 | (0.548–3.547) |
| Any drug problemse | 1.673+ | (0.960–2.915) | 2.525** | (1.620–3.937) | 1.043 | (0.548–1.986) |
| Any psychiatric problemse | 1.373 | (0.850–2.218) | 1.267 | (0.894–1.796) | 1.288 | (0.779–2.131) |
| # of AA meetings attended past year | 1.000 | (0.997–1.003) | 1.003+ | (1.000–1.005) | 0.999 | (0.996–1.003) |
| Went to treatment in past yearf | 2.594** | (1.708–3.938) | 1.760** | (1.264–2.449) | 1.063 | (0.673–1.679) |
| Effects on linear slopeg | ||||||
| Any drug problems | 0.892 | (0.770–1.034) | 0.885* | (0.796–0.985) | 1.015 | (0.875–1.177) |
| # of AA meetings attended past year | 1.000 | (0.999–1.001) | 0.999* | (0.998–1.000) | 1.000 | (0.999–1.001) |
| Constant | 0.004** | (0.002–0.012) | 0.204** | (0.099–0.419) | 0.004* | (0.001–0.015) |
| /lnsig2u | 0.586 | (0.076–1.100) | 1.251 | (0.939–1.560) | 2.605 | (2.277–2.930) |
| sigma_u | 1.340 | (1.039–1.730) | 1.869 | (1.599–2.190) | 3.678 | (3.122–4.330) |
| Rho | 0.353 | (0.247–0.480) | 0.515 | (0.437–0.590) | 0.804 | (0.748–0.850) |
| Observations | 1,871 | 1,867 | 1,824 | |||
| Number of cases | 497 | 497 | 467 | |||
*P < 0.05, **P < 0.01, +P < 0.1.
aReferent: At least a high school diploma or GED.
bReferent: Single, divorced or widowed.
cReferent: White/Caucasian.
dReferent: HMO Outpatient.
eReferent: No problems.
fReferent: Did not go to treatment in past year.
gNote: Interaction with time.
The models using lagged variables (full models available upon request) showed that 30-day alcohol, drug and psychiatric problems reported at a prior interview were not significantly associated with social status assessed 2 years later, but prior AA meetings attended marginally reduced the odds of having indicators of low social status later (AOR = 0.998; 95% CI = 0.995, 1.000; P < 0.10). As in the concurrent models, reports of returning to treatment during a previous interview also were associated with marginally higher odds of low social status later (AOR = 1.52; 95% CI = 0.97, 2.38; P < 0.10). These lagged effects were consistent with the concurrent predictors in the model as well. When accounting for lagged effects, alcohol problem severity (AOR = 3.06; 95% CI = 0.91, 10.30; P < 0.10) and psychiatric problems (AOR = 1.83; 95% CI = 1.14, 2.93; P < 0.05) in the 30 days prior to the interview and returning to treatment in the 12 months prior to the interview (AOR = 2.12; 95% CI = 1.27, 3.55; P < 0.01) were associated with higher odds of low social status over time.
DISCUSSION
In this sample of alcohol-dependent treatment clients, after accounting for covariates, social status did not change significantly over the 7-year follow-up period. The proportion of people reporting none of the indicators of low social status increased from 27% at baseline to ~40% for all subsequent waves, demonstrating that those who were relatively less disadvantaged maintained this status over time. Although the proportion with low social status at baseline did not markedly improve after the 1-year follow-up, there was a reduction in the proportion of people who reported two or more indicators of low social status over time. Changes in social status were largely due to changes in employment and housing status, rather than changes in neighborhood poverty. Using a much shorter 1-year follow-up period, LoCastro and colleagues (2009) noted relatively little change in one employment outcome (proportion of days paid for work) after completing treatment as part of the COMBINE trial. Secondary benefits of alcohol and drug treatment such as re-employment, achieving and/or maintaining stable housing, and improved economic circumstances may require substantial targeted programming and relatively long time periods before they emerge. Programs that integrate more of a social model approach to service provision (Kaskutas, 1998) may be particularly beneficial for these secondary treatment outcomes, especially if they emphasize employment and housing support.
We also found low social status over time was predicted by ongoing alcohol, drug and psychiatric problems; continued AA attendance and ongoing treatment; as well as several demographic characteristics, including minority race/ethnicity, having less than a high school education and being female. In our sample, the relationship of drug problems with low social status weakened significantly over time. Others have documented long-term negative impacts of ongoing AUD on poverty (Buu et al., 2007) and unemployment (French et al., 2011), but the pattern of results for ongoing service utilization (both formal treatment and AA) was counter to our expectations, as there was little improvement over time even for those who sought additional treatment. Prior research has suggested that clients benefit from receiving continued support after an index treatment event (Mertens et al., 2005) or from involvement with AA after treatment (Fiorentine and Hillhouse, 2000; Moos and Moos, 2006; Witbrodt et al., 2014). In this sample, however, ongoing service utilization indicated relatively poor prognosis that may have been concurrent with an event of unemployment, homelessness or incarceration. It is noteworthy that the association of AA attendance with low social status weakened over time and that the lagged models suggested there may be a long-term protective effect of continued AA involvement. This question deserves further study. Future studies also could investigate mechanisms of effect, such as the contribution of police surveillance to arrest (and therefore imprisonment and loss of social status) of people after AUD treatment (particularly among people of minority race/ethnicity) or the contribution of heavy drinkers in the networks of homeless people (Wenzel et al., 2012) to ongoing AUD or to social status over time.
Study Limitations and Strengths
A strength of our study is that we used an outcome that combined several relatively severe conditions such as unemployment, living in unstable housing or being homeless, incarceration and living in an impoverished area. However, a study limitation is that we did not have information on the duration or onset of episodes of unemployment or living in unstable or impoverished conditions. Our study was primarily concerned with the hypothesis that there is a selection effect that links social status with alcohol problems; that is, people with AUD lose social status over time. Another possibility is that there is an influence effect, whereby exposure to conditions of low social status (such as unemployment or poverty) causes alcohol and other drug problems over time (Buu et al., 2007; Johnson et al., 1997). Use of disaggregated outcomes in larger samples and with detailed information on timing of outcomes would allow for more specificity in the conclusions we can draw about how AUD impacts social status over time. Future studies with larger samples should seek to replicate our findings from this representative group of alcohol treatment program clients.
We do not know details about exactly what supportive services were received at each treatment episode, and we do not know about such services the clients may have received elsewhere, such as through mental health providers or the welfare system (Ammon et al., 2008). Additional research using program administrative data could be informative for describing the contribution of particular programmatic elements to client outcomes. Replication of these results using newer data also would be beneficial, although the findings from this representative treatment sample that included a 7-year follow-up period and linked neighborhood data offer a contribution to the extant literature on long-term sequelae of alcohol and drug problems. Finally, there was loss-to-follow-up over the course of the study, although the response rate at the final interview still was respectable (67%) for a sample recruited from alcohol treatment programs. Alcohol problem severity at baseline was associated with attrition, but we note that the proportion of cases with low social status was highly stable over time, which suggests that there was not selective attrition of these people over the course of the study.
Recommendations for Future Research
We restricted our current sample to participants with a DSM-IV diagnosis of alcohol dependence who were enrolled in alcohol treatment. Future studies should assess social status and long-term social integration of alcohol-dependent individuals who do not receive treatment. Replication with established multi-dimensional measures of social status, such as the Townsend Index which incorporates employment status, car ownership and housing tenure/crowding (Krieger et al., 2003; Morris and Carstairs, 1991), also may be instructive for improving treatment services and social integration of people with AUD. Long-term follow-up of individuals who obtain additional services such as employment and housing support during and after AUD treatment will help us to better understand the dynamics between problem severity and long-term social status. The current analyses focused on past-30-day problem severity as the primary independent variables; additional research on the role of abstinence and other measures of recovery (Kaskutas et al., 2014) as predictors of social status would be informative. Finally, prior work has shown that individuals with high psychiatric problem severity may especially benefit from involvement in AA, particularly from getting a sponsor and becoming involved in AA-related service (Subbaraman et al., 2011). Studies should examine whether these factors are related to social status among AUD patients with psychiatric co-morbidities.
CONCLUSIONS
Specialty addiction treatment alone is not sufficient to have positive long-term impacts on social status of alcohol-dependent people. Recovery-oriented systems of care emphasize neighborhood-based delivery of services and development of community-based recovery support systems that provide ongoing, integrated services to prevent relapse (Sheedy and Whitter, 2009). These notions are consistent with paradigms encouraging a shift from a model of treatment as repeated episodes of acute care toward a model of chronic care focused on longer-term recovery management (White et al., 2002, 2006). Implicit in these models is a need for ancillary support services during the protracted treatment and recovery process from addiction. Wraparound services, including educational, vocational and housing support, are effective (Institute of Medicine, 1990; McLellan et al., 1998; Milby et al., 1996) and recommended, but still are not yet commonly integrated into drug and alcohol treatment (Paino et al., 2016). Employment and housing support services may have profound benefits for the social integration and social status of people with AUD, and the impacts may be particularly important for people with co-morbid drug or psychiatric problems.
ACKNOWLEDGEMENTS
The authors would like to thank Dr Amy Mericle for her comments on early drafts of this manuscript.
FUNDING
This work was supported by the National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism (NIAAA) under Grant R01AA020328. The original longitudinal study was supported by NIAAA under Grants R01AA09750, P50AA005595 and R01AA015927. The NIAAA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR. Washington, DC: American Psychiatric Publishing, Inc. [Google Scholar]
- Ammon L, Bond J, Matzger H, et al. (2008) Gender differences in the relationship of community services and informal support to seven-year drinking trajectories of alcohol-dependent and problem drinkers. J Stud Alcohol Drugs 69:140–50. [DOI] [PubMed] [Google Scholar]
- Braun BL, Hannan P, Wolfson M, et al. (2000) Occupational attainment, smoking, alcohol intake, and marijuana use: ethnic-gender differences in the CARDIA study. Addict Behav 25:399–414. [DOI] [PubMed] [Google Scholar]
- Buu A, Mansour M, Wang J, et al. (2007) Alcoholism effects on social migration and neighborhood effects on alcoholism over the course of 12 years. Alcohol: Clin Exp Res 31:1545–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Gfroerer J, Conway KP, et al. (2014) Unemployment and substance outcomes in the United States. Drug Alcohol Depend 142:350–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorentine R, Hillhouse MP (2000) Drug treatment and 12-step program participation: the additive effects of integrated recovery activities. J Subst Abuse Treat 18:65–74. [DOI] [PubMed] [Google Scholar]
- French MT, Maclean JC, Sindelar JL, et al. (2011) The morning after: alcohol misuse and employment problems. Appl Econ 43:2705–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstein DR, Lewin LS (1990) Treating drug problems. N Engl J Med 323:844–8. [DOI] [PubMed] [Google Scholar]
- Gossop M, Stewart D, Marsden J (2008) Attendance at narcotics anonymous and alcoholics anonymous meetings, frequency of attendance and substance use outcomes after residential treatment for drug dependence: a 5 year follow-up study. Addiction 103:119–25. [DOI] [PubMed] [Google Scholar]
- Hser Y-I, Anglin MD, Grella C, et al. (1997) Drug treatment careers: a conceptual framework and existing research findings. J Subst Abuse Treat 14:543–58. [DOI] [PubMed] [Google Scholar]
- Hu FB, Goldberg J, Hedeker D, et al. (1998) Comparison of population-averaged and subject-specific approaches for analyzing repeated binary outcomes. Am J Epidemiol 147:694–703. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (1990) Broadening the Base of Treatment for Alcohol Problems. Washington, D.C: National Academy Press. [PubMed] [Google Scholar]
- Johnson TP, Freels SA, Parsons JA, et al. (1997) Substance abuse and homelessness: social selection or social adaptation? Addiction 92:437–45. [PubMed] [Google Scholar]
- Kaskutas LA. (1998) Methodology and characteristics of programs and clients in the social model process evaluation. J Subst Abuse Treat 15:19–25. [DOI] [PubMed] [Google Scholar]
- Kaskutas LA. (2009) Alcoholics anonymous effectiveness: faith meets science. J Addict Dis 28:145–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Borkman TJ, Laudet A, et al. (2014) Elements that define recovery: the experiential perspective. J Stud Alcohol Drugs 75:999–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kertesz SG, Crouch K, Milby JB, et al. (2009) Housing first for homeless persons with active addiction: are we overreaching? Milbank Q 87:495–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Waterman PD, Chen JT, et al. (2003) Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures—the public health disparities geocoding project (US). Public Health Rep 118:240–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LoCastro JS, Youngblood M, Cisler RA, et al. (2009) Alcohol treatment effects on secondary nondrinking outcomes and quality of life: the COMBINE study. J Stud Alcohol Drugs 70:186–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Hagan TA, Levine M, et al. (1998) Supplemental social services improve outcomes in public addiction treatment. Addiction 93:1489–99. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, et al. (1992) The fifth edition of the addiction severity index. J Subst Abuse Treat 9:199–213. [DOI] [PubMed] [Google Scholar]
- McVicar D, Moschion J, van Ours JC (2015) From substance use to homelessness or vice versa? Soc Sci Med 136–137:89–98. [DOI] [PubMed] [Google Scholar]
- Mertens JR, Weisner CM, Ray GT (2005) Readmission among chemical dependency patients in private, outpatient treatment: patterns, correlates and role in long-term outcome. J Stud Alcohol 66:842–7. [DOI] [PubMed] [Google Scholar]
- Milby JB, Schumacher JE, Raczynski JM, et al. (1996) Sufficient conditions for effective treatment of substance abusing homeless persons. Drug Alcohol Depend 43:39–47. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS (2003) Long-term influence of duration and intensity of treatment on previously untreated individuals with alcohol use disorders. Addiction 98:325–37. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS (2006) Participation in treatment and alcoholics anonymous: a 16-year follow-up of initially untreated individuals. J Clin Psychol 62:735–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris R, Carstairs V (1991) Which deprivation? A comparison of selected deprivation indices. J Public Health Med 13:318–26. [PubMed] [Google Scholar]
- Mäkelä K. (2004) Studies of the reliability and validity of the addiction severity index. Addiction 99:398–410. [DOI] [PubMed] [Google Scholar]
- Paino M, Aletraris L, Roman P (2016) The relationship between client characteristics and wraparound services in substance use disorder treatment centers. J Stud Alcohol Drugs 77:160–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL. (2016) Co-occurring substance abuse and mental health problems among homeless persons: suggestions for research and practice. J Soc Distress Homeless 25:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins LN, Cuttler L, Keating S (1991) NIMH Diagnostic Interview Schedule, Version III, Revised. Rockville, MD: National Institute of Mental Health. [Google Scholar]
- Sheedy CK, Whitter M (2009) Guiding Principles and Elements of Recovery-Oriented Systems of Care: What do we know from the research? [HHS Publication No. (SMA) 09–4439] [Accessed: 2015-05-01. Archived by WebCite® at http://www.webcitation.org/6YDADCmUP]. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration.
- StataCorp (2015) Stata Statistical Software: Release 14.0. College Station, TX: Stata Corporation. [Google Scholar]
- Subbaraman MS, Kaskutas LA, Zemore SE (2011) Sponsorship and service as mediators of the effects of Making Alcoholics Anonymous Easier (MAAEZ), a 12-step facilitation intervention. Drug Alcohol Depend 116:117–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai J, Rosenheck RA, Kasprow WJ, et al. (2013) Risk of incarceration and clinical characteristics of incarcerated veterans by race/ethnicity. Soc Psychiatry Psychiatr Epidemiol 48:1777–86. [DOI] [PubMed] [Google Scholar]
- Twisk JWR. (2013) Applied Longitudinal Data Analysis for Epidemiology: A practical guide. New York: Cambridge University Press. [Google Scholar]
- Weisner C, Schmidt L (1995) The Community Epidemiology Laboratory: studying alcohol problems in community- and agency-based populations. Addiction 90:329–42. [DOI] [PubMed] [Google Scholar]
- Wenzel SL, Hsu HT, Zhou A, et al. (2012) Are social network correlates of heavy drinking similar among black homeless youth and white homeless youth? J Stud Alcohol Drugs 73:885–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White WL, Boyle M, Loveland D (2002) Alcoholism/addiction as a chronic disease: from rhetoric to clinical reality. Alcohol Treat Q 20:107–29. [Google Scholar]
- White WL, Kurtz E, Sanders M (eds) (2006) Recovery Management. Chicago, IL: Great Lakes Addiction Technology Transfer Center (ATTC) Network. [Google Scholar]
- Witbrodt J, Ye Y, Bond J, Chi F, Weisner C, Mertens J (2014) Alcohol and drug treatment involvement, 12-step attendance and abstinence: 9-year cross-lagged analysis of adults in an integrated health plan. J Subst Abuse Treat 46:412–9. [DOI] [PMC free article] [PubMed] [Google Scholar]