Abstract
Background
Vaccination coverage among children entering kindergarten in the United States is high, but interstate variations exist. The relationship between state immunization laws and vaccination coverage has not been fully assessed. We evaluated associations of state laws on both measles, mumps, and rubella (MMR) and diphtheria, tetanus, and pertussis (DTaP) vaccination coverage and exemptions to school immunization requirements.
Methods
We conducted a retrospective, longitudinal analysis of the effect of state immunization laws on vaccination coverage and exemptions among US kindergarteners from SY 2008 to SY 2014. The primary outcome measures were state-level kindergarten entry vaccination coverage rates for 2-dose MMR and 4-dose DTaP vaccines. Secondary outcome measures included rates of state-level exemptions (ie, medical, religious, philosophical) to school immunization requirements.
Results
We found that state policies that refer to Advisory Committee on Immunization Practices recommendations were associated with 3.5% and 2.8% increases in MMR and DTaP vaccination rates. Health Department–led parental education was associated with 5.1% and 4.5% increases in vaccination rates. Permission of religious and philosophical exemptions was associated with 2.3% and 1.9% decreases in MMR and DTaP coverage, respectively, and a 1.5% increase in both total exemptions and nonmedical exemptions, respectively.
Conclusions
We found higher vaccination coverage and lower nonmedical exemption rates for MMR and DTaP vaccines in states adopting Advisory Committee on Immunization Practices guidelines for school entry. Adherence to these best practices was a successful strategy to increase vaccination coverage and reduce vaccination exemptions.
Keywords: children, coverage, exemptions, law, immunization
School immunization requirements have been credited with improved vaccination coverage and decreased incidence of vaccine-preventable diseases [1]. All states provide medical exemptions to the requirements, and some state laws also offer exemptions for religious and/or philosophical reasons [1]. In 2015, the United States experienced the largest measles outbreak since its elimination in 2000 [2]. The majority of cases were among persons who were intentionally unvaccinated [2]. As a result, California passed a law removing nonmedical exemptions and joined West Virginia and Mississippi, 2 states that have disallowed nonmedical exemptions for years. Several other states tried but failed to eliminate nonmedical exemptions [3].
The median proportion of kindergartners exempted from 1 or more vaccines has increased from 1.1% in the 2009–2010 school year (SY 2009) to 1.7% in the 2014–2015 school year (SY 2014), with private schools reporting higher rates of nonmedical exemptions compared with public schools [4–6]. Although nonmedical exemptions have been increasing, overall vaccination coverage in the United States remains high but varies by state. For example, vaccination coverage for diphtheria, tetanus, and pertussis (DTaP) requirements in SY 2014 ranged from 84.3% (significantly below the “herd immunity” level) in Colorado to 99.6% in Maryland [4]. The reasons behind the different coverage rates are only partially understood and are limited to research on the effect of immunization laws on exemptions [7–10].
State-level data suggest that exemption rates do not correlate with vaccination coverage [4]. This discordance highlights the importance of assessing immunization laws separately with respect to both coverage and exemptions. The paper extends the existing literature [11] by making the important distinction between how vaccination policies may differentially affect the number of exemptions and the proportion of the population that is vaccinated. The objective of this investigation was to evaluate how state vaccination laws are associated with coverage and exemption rates, using the recent data from SY 2008–SY 2014. We also seek to demonstrate which laws are more associated with increasing coverage rates and decreasing exemption rates. The results of these analyses lend insight to state lawmakers and Department of Health (DOH) officials regarding which policies are most valuable in securing adequate vaccination coverage for their communities.
METHODS
Study Design
We conducted a retrospective, longitudinal analysis of the effect of state immunization laws on vaccination coverage and exemptions among US kindergarteners from SY 2008 to SY 2014. The primary outcome measures were state-level kindergarten entry vaccination coverage rates for 2-dose measles, mumps, and rubella (MMR) and 4-dose DTaP vaccines. Secondary outcome measures included rates of state-level exemptions (ie, medical, religious, philosophical) to school immunization requirements.
Data Sources and Variables
This study utilized data from the legislative code for each state, obtained from the Thomson Reuters Westlaw database for 2008–2014, and the Inter-university Consortium for Political and Social Research State Vaccination Requirements and Exemption Law Database for 2008–2011 [12, 13]. Both databases were utilized to ensure data fidelity across the years of the study. Individual state DOH websites were also accessed to clarify any ambiguity. State laws and codes were systematically reviewed by two authors (B.E.S. and O.K.V.K.) for consistency in interpretation; inconsistencies were discussed with the whole team until consensus was reached. We included all immunization laws, regardless of when they were enacted. The study has benefitted from the authors’ (O.K.V.K. and Y.T.Y.) legal expertise to accurately interpret language captured by the immunization laws. We recorded the history of changes over time for each state and each component of the law during the study period. Table 1 and 2, summarizes a list of all vaccination-related laws investigated in this study.
Table 1.
US Vaccination Laws—SY 2008 to SY 2014
| Variable Name | Description | No. States With Law (SY 2014) | States With Law Present/Absent |
|---|---|---|---|
| Annual recertification | State law requires an annual or more frequent health care provider recertification for medical exemptions | 9 | Present: AR, CT, GA, KS, MA, NM, NY, TX, WV |
| DOH-led parental education | If enhanced education regarding benefits of vaccination or risks of nonvaccination during the exemption process is required, the state designates that the state Department of Health is responsible for providing education to the parents | 6 | Present: AZ, AR, MI, OR, UT, VT |
| Exclusion during outbreak | State law expressly allows for exclusion of exempted students from school during an outbreak | 27 | Present: AZ, AR, CA, CO, DE, DC, FL, GA, HI, ID, LA, ME, MO, MT, NV, NH, NJ, NY, ND, OH, RI, TX, UT, VA, WA, WI, WY |
| Grace period | A grace, provisional, or conditional enrollment period is allowed for children who are not up to date with vaccinations | 45 | Absent: AL, CT, DC, ID, KS, MI |
| Parental notarization | Parental notarization/affidavit is required for religious/philosophical exemption | 14 | Present: AK, AR, DE, GA, IA, KY, MN, MT, NE, NH, NM, TN, TX, VA |
| Penalties | Penalties exist for parents whose children are not up to date, such as fines and/or exclusion from state aid | 17 | Present: AZ, CA, CT, DE, FL, GA, IL, IN, KS, LA, MA, MS, NV, OK, PA, TN, VA |
| Policy referral to ACIP guidelines | The state authorities refer to the ACIP guidelines for vaccination requirements within the legislative code | 46 | Absent: KS, MI, SC, SD, WI |
| Provider-led parental education | If enhanced education regarding benefits of vaccination or risks of nonvaccination during the exemption process is required, the state designates a health care provider to be responsible for providing education to the parents | 3 | Present: CA, OR, WA |
| Religious and philosophical exemptions | The state allows for both religious and philosophical exemptions | 19 | Present: AR, AZ, CA, CO, ID, LA, ME, MI, MN, ND, OH, OK, OR, PA, TX, UT, VT, WA, WI |
| Scalable exemptions | The law and/or standardized exemption form allows exemption of individual required vaccinations | 37 | Absent: CT, HI, KS, LA, MA, MS, NE, NV, NJ, OH, OK, PA, TX, UT |
| Standardized exemption form | A standardized exemption form is required for all exemption applications | 39 | Absent: LA, ME, MA, MO, NV, NJ, NC, OH, PA, SD, TN, WI |
Abbreviations: ACIP, Advisory Committee on Immunization Practices; DOH, Department of Health; SY, school year.
Table 2.
US Vaccination Laws With Nonsignificant Associations With Vaccine Coverage and Exemption Rates—SY 2008 to SY 2014
| Variable Name | Description | No. States With Law (SY 2014) | States With Law Present/Absent |
|---|---|---|---|
| Annual DOH audit | The state Department of Health performs an annual audit of school immunization records | 51 | Present: all states and DC |
| Copy of record | Schools are required to keep a copy of provider records/student immunization cards | 51 | Present: all states and DC |
| Day care requirement | Immunization regulations for entry to day care are present | 51 | Present: all states and DC |
| Day care mirror | Immunization entry requirements for day care facilities follow the same guidelines as those for public schools | 45 | Absent: MS, MO, MT, NE, PA, WV |
| DOH approval | Exemption application must be reviewed by the health department for approval | 5 | Present: AL, AR, MI, MN, WV |
| Education during exemption process | State law requires education about the benefits of vaccination or the risks of being unvaccinated in the exemption process | 8 | Present: AZ, AR, CA, MI, OR, UT, VT, WA |
| Exclusion during emergency | Exemptions may not be recognized during epidemic, outbreak, and/or emergency | 15 | Present: AL, AK, AR, CA, CO, GA, HI, ID, IA, KY, MD, MA, NV, ND, TX |
| Exemption during vaccine shortages | In the case of a vaccine shortage, children are allowed to attend school with a temporary exemption | 23 | Present: AL, AK, AZ, CA, CO, CT, DC, FL, GA, ID, IL, IA, LA, ME, MN, MO, NJ, NY, ND, OK, OR, TX, WY |
| Parental acknowledgement | If the state allows for exclusion during outbreak, parental acknowledgement of this is required during the exemption process | 8 | Present: AK, AZ, AR, CA, CT, MT, ND, WA |
| Philosophical exemptions expressly excluded | If religious exemptions are allowed, legislative language expressly excludes exemptions based on philosophical beliefs | 5 | Present: DE, IA, NJ, NC, WV |
| Physician signature | Only physicians can sign exemption forms | 23 | Present: AL, AK, AZ, CT, FL, HI, IN, KS, MS, MO, MT, NE, NV, NM, NY, NC, ND, OH, SC, SD, UT, VA, WY |
| Private school requirement | Immunization regulations governing private school entry requirements exist | 47 | Absent: IN, MI, OH, SD |
| Private school mirror | Immunization entry requirements for private schools follow the same guidelines as those for public schools | 48 | Absent: IN, MI, OH |
| School name required | The school name must be included on the exemption application form | 2 | Present: AR, UT |
| Temporary exemptions | The state allows for temporary exemptions based on medical contraindications | 19 | Present: AZ, CA, CT, FL, GA, HI, IN, IA, MD, MI, MT, NJ, NY, NC, PA, SC, VA, WA, WV |
| Homeschool tracking | The state has a method for monitoring the immunization status of homeschooled children | 5 | Present: CO, MN, ND, PA, TN |
Abbreviations: DOH, Department of Health; SY, school year.
State-level vaccination coverage and exemption rates for each year were obtained from the Centers for Disease Control and Prevention’s (CDC’s) SchoolVaxView website and Morbidity and Mortality Weekly Reports (MMWR) for kindergarten-aged children [4]. These data were collected by federally funded state, local, and territorial immunization programs. We chose to focus on vaccination coverage for MMR and DTaP due to the high communicability of the diseases targeted by these vaccines, and the burden of recent measles and pertussis outbreaks across the US. For the purpose of our analysis, we did not include exemption rate by vaccine type (referred to as scalable exemptions) but focused on total exemptions as outcome variables to standardize the analytic approach.
To account for socioeconomic conditions that may be linked with vaccination coverage and exemption, the following state-level characteristics were selected for inclusion in the analysis: poverty and insurance percentages for those under the age of 18 years; the percentage of individuals older than age 25 years with a college degree; and the rate of family medicine and pediatric physicians per 10 000 population. Physician density information was obtained through the Area Health Resource Files (AHRF) [14]. State-level population demographic information was accessed through the Census Bureau’s American Community Survey and Model-based Small Area Income & Poverty Estimates [15, 16].
Statistical Analysis
A total of 357 state-year data points were available for analysis (7 years × 50 states plus the District of Columbia). Descriptive statistics for state-level vaccination coverage and exemption rates and state immunization laws were calculated by year. Independent-sample t tests and correlation analyses were conducted to assess frequencies and relationships among vaccination laws and outcome variables by year and across years.
Predictors of vaccination coverage and exemption rates between SY 2008 and SY 2014 were determined by a mixed-effects model. All possible interactions were assessed in the final multivariable models. Visual inspection of residual plots did not reveal any obvious deviations from homoscedasticity or normality. All statistical analyses were conducted in SAS 9.3 (SAS Institute, Cary, NC); mixed effects models were conducted using PROC MIXED.
Law Effectiveness Indexing
We constructed indices of law effectiveness to assess the strength of all combined state vaccination legislative policies on increasing MMR and DTaP vaccination coverage rates and reducing total exemptions. Following the methodology of Bradford et al., we used the regression coefficients from the mixed effects models as weights for each statistically significant law component; state laws that were not statistically significant at the α = 0.10 level in the final models were given a weight of 0 [11]. Weights were multiplied by the corresponding indicator variables for each law, and these results were summed to create the index; each state-year received an index score. The index score values were then averaged across each state for all the years of the study, creating a list of 51 state index scores. These scores were grouped into 3 categories based on the index tertiles: less effective, average, more effective. States with “more effective” laws for vaccination coverage are those in the highest tertile, as higher index scores are associated with higher coverage rates. Conversely, states with “less effective” laws for vaccination exemption are in the highest tertile, as states with higher index scores are associated with higher exemption rates. The state index scores for both the coverage effectiveness index and exemption effectiveness index were mapped onto a geographic display of the US for SY 2008–SY 2014. The full indices for all 357 state-years included in this analysis, as well as statistical correlations with existing indexes, are available upon request.
RESULTS
Laws and Vaccination Coverage
Laws Associated With Increased Coverage
Both policy referral to the Advisory Committee on Immunization Practices (ACIP) guidelines and DOH-led parental education during the exemption process were associated with increased vaccination coverage for MMR and DTaP. State policy referral to ACIP was associated with a 3.5% increase and a 2.8% increase in MMR and DTaP vaccination rates (P = .01 and P = .05, respectively), and DOH-led parental education was associated with a 5.1% increase and a 4.5% increase in MMR and DTaP vaccination rates (P = .01 and P = .01, respectively).
These 2 components also had significant interactions with time. Regression plots and by-year comparisons revealed that the presence of these policies predicted statistically significantly higher coverage rates for MMR and DTaP in SY 2008 and SY 2009, but this relationship was no longer statistically significant in subsequent years (data available upon request). The main model results can be found in Table 3.
Table 3.
Mixed Effects Regression Results: MMR and DTaP Vaccine Coverage Rates for 50 US States and District of Columbia—SY 2008 to SY 2014
| MMR | DTaP | |
|---|---|---|
| Regulation variablea | Estimate (SE) | Estimate (SE) |
| ACIPb | 3.49 (1.38)* | 2.81 (1.48)** |
| DOH-led parental education | 5.05 (1.61)* | 4.47 (1.73)* |
| Religious and philosophical exemptions | –2.34 (0.80)* | –1.88 (0.85)** |
| Grace period | 1.27 (1.00) | 2.03 (1.06)*** |
| Scalable exemptions | –1.09 (0.60)*** | –1.33 (0.65)** |
Abbreviations: ACIP, Advisory Committee on Immunization Practices; DOH, Department of Health; DTaP, pediatric diphtheria and tetanus toxoids and acellular pertussis vaccine; MMR, measles, mumps, and rubella vaccine; SY, school year.
* P ≤ .01; **P ≤ .05; ***P ≤ .10.
aFor a detailed description of the variable, please see Table 1.
bState refers to ACIP for their vaccination requirements.
Laws Associated With Decreased Coverage
State laws allowing both religious and philosophical exemptions and laws permitting scalable exemptions were associated with decreased MMR and DTaP coverage rates. Allowance of religious and philosophical exemptions was associated with a 2.3% decrease and a 1.9% decrease in MMR and DTaP vaccination rates (P = .01 and P = .03, respectively). Laws permitting scalable exemptions were associated with a 1.1% decrease and a 1.3% decrease in MMR and DTaP vaccination rates (P = .04 and P = .03, respectively) (Table 3).
Laws with Nonsignificant Association With Coverage
Grace periods were marginally significant only for DTaP coverage rates (Table 3). None of the other laws investigated had a detectable association on coverage (data not shown). State medical, nonmedical, and total exemption rates (ie, the percentage of kindergarten children exempted from vaccination requirements) did not have a statistically significant association with coverage rates (data not shown).
Laws and Exemptions to School Immunization Requirements
Laws Associated With Increased Exemptions
State laws allowing both philosophical and religious exemptions, requiring standardized exemption forms, and provider-led parental education during the exemption process were associated with increased exemption rates. Allowance of religious and philosophical exemptions was associated with a 1.5% increase in both total exemptions and nonmedical exemptions (P ≤ .001 and P < .001, respectively). Laws requiring standardized exemption forms were associated with a 0.7% increase in both total exemptions and nonmedical exemptions (P = .04 and P = .05, respectively) (Table 4).
Table 4.
Mixed Effects Regression Results: Vaccine Exemption Rates for 50 US States and District of Columbia—SY 2008 to SY 2014
| Total Exemptions | Medical Exemptions | Nonmedical Exemptions | |
|---|---|---|---|
| Regulation variablea | Estimate (SE) | Estimate (SE) | Estimate (SE) |
| Religious and philosophical exemptions | 1.51 (0.39)* | –0.08 (0.08) | 1.54 (0.36)* |
| Provider-led parental education | 1.91 (1.03)*** | –0.27 (0.17) | 2.08 (1.01)** |
| ACIPb | –0.87 (0.47)*** | –0.04 (0.10) | –0.87 (0.44)** |
| Grace period | –0.18 (0.39) | –0.02 (0.09) | –0.03 (0.36) |
| Standardized exemption form | 0.74 (0.36)** | 0.10 (0.07) | 0.68 (0.34)** |
| Notarization | 0.23 (0.45) | 0.02 (0.09) | 0.08 (0.41) |
| Annual recertification | –0.99 (0.53)*** | –0.10 (0.10) | –0.78 (0.48) |
| Scalable exemptionsb | –0.09 (0.28) | –0.04 (0.05) | –0.03 (0.26) |
| Penalties | –0.11 (0.36) | 0.02 (0.07) | –0.06 (0.34) |
| Exclusion during outbreak | –0.04 (0.35) | –0.04 (0.07) | 0.02 (0.32) |
Abbreviations: ACIP, Advisory Committee on Immunization Practices; SY, school year.
* P ≤ .01; **P ≤ .05; ***P ≤ .10.
aFor a detailed description of the variable, please see Table 1.
bState refers to ACIP for their vaccination requirements.
Provider-led parental education was associated with a 2.1% increase in nonmedical exemptions (P = .04) but also had a significant interaction with time. Regression plots and by-year comparisons revealed that the presence of this policy predicted statistically significantly higher nonmedical exemption rates in SY 2008 and SY 2009. Conversely, the presence of this policy predicted statistically significantly lower medical exemption rates from SY 2008 to SY 2011. These relationships were no longer statistically significant in subsequent years (data available upon request). This pattern indicates that states requiring provider-led education of parents during the exemption process had higher nonmedical exemptions and lower medical exemptions but that the effect of this law has tapered across time. The main model results can be found in Table 4.
Laws Associated With Decreased Exemptions
Policy referral to ACIP guidelines was significantly associated with a 0.9% decrease in nonmedical exemptions (P = .05). Annual recertification was marginally significant (P = .10) and was associated with a 1% decrease in total exemptions.
Laws With Nonsignificant Association With Exemptions
The policies of grace periods, parental notarization, scalable exemptions, penalties, and student exclusion during an outbreak were not associated with vaccination exemption rates. None of the other laws investigated had a detectable association with exemption (data not shown).
Law Effectiveness Indices
The construction of the law effectiveness indices for vaccination coverage and vaccination exemption took into account the influence of all laws that were found to be statistically significant in multivariate modeling. Creating a multifactorial index provides a cohesive presentation of how a state’s policy orientation is associated with vaccination coverage and vaccination exemption by evaluating the combination of laws within a state, rather than looking at policies in isolation. It is important to note that not every state in the “more effective” category had the same combination of policies in place across each year of the study.
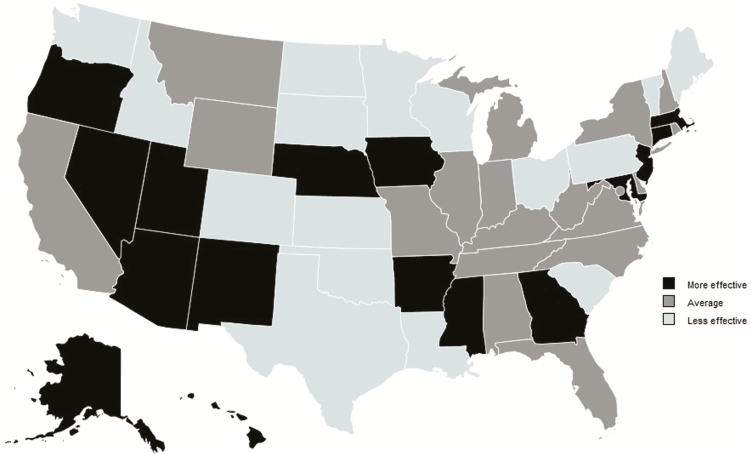
Vaccination Coverage Law Effectiveness Index
Sixteen states were found to have a more effective vaccination coverage policy combination for SY 2008 to SY 2014. The laws associated with higher coverage rates included policy referral to ACIP guidelines, DOH-led parental education, and grace periods. Sixteen states were found to have a less effective vaccination coverage policy combination from SY 2008 to SY 2014. States allowing scalable exemptions and religious and philosophical exemptions had lower vaccination coverage. A visual representation of index results for vaccination coverage law effectiveness can be found in Figure 1.
Figure 1.
States’ policy combinations beneficial to increased vaccination coverage: States by tertile of vaccination coverage law effectiveness index, 2008–2014. Sources: Authors’ analysis of data from 2008–2014 Centers for Disease Control and Prevention school assessment reports, 2008–2014 data from Thomson Reuters Westlaw database, 2008–2011 data from Inter-University Consortium for Political and Social Research State Vaccination Requirements and Exemption Law Database, and 2008–2014 data from Area Health Resource Files. Index categories correspond to the tertiles of state index values, which were created through the summation of state policy coefficients produced through mixed effects regression-generated weights. The designation of “more effective” indicates that, overall, a given state has a stronger policy combination to facilitate increased vaccination coverage rates, as compared to other states. The designation of “less effective” indicates that, overall, a given state’s policy combination is less strong when compared with other states.
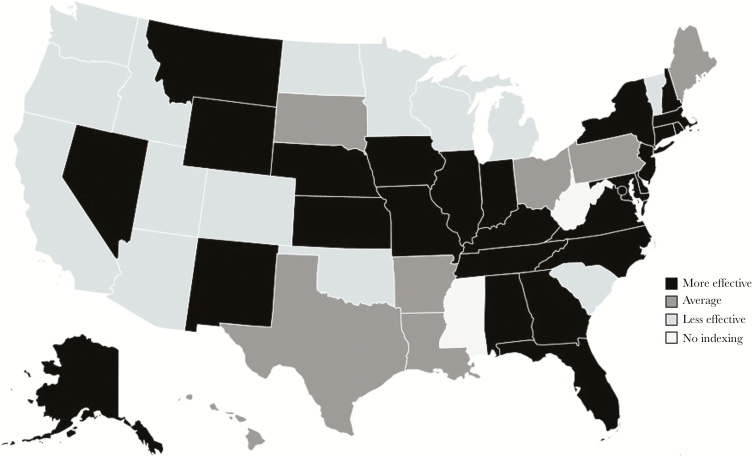
Vaccination Exemption Law Effectiveness Index
Twenty-seven states were found to have a more effective vaccination exemption policy combination from SY 2008 to SY 2014. The laws associated with lower exemptions rates included policy referral to ACIP guidelines and annual recertification. Fourteen states were found to have a less effective vaccination exemption policy combination from SY 2008 to SY 2014. States allowing religious and philosophical exemptions and those requiring provider-led parental education and standardized exemption forms had higher total exemption rates. A depiction of exemption law effectiveness can be found in Figure 2.
Figure 2.
States’ policy combinations beneficial to decreased exemption rates: States by tertile of vaccination exemption law effectiveness index, 2008–2014. Sources: Authors’ analysis of data from 2008–2014 Centers for Disease Control and Prevention school assessment reports, 2008–2014 data from Thomson Reuters Westlaw database, 2008–2011 data from Inter-University Consortium for Political and Social Research State Vaccination Requirements and Exemption Law Database, and 2008–2014 data from Area Health Resource Files. Note: Index categories correspond to the tertiles of state index values, which were created through the summation of state policy coefficients produced through mixed effects regression-generated weights. The designation of “more effective” indicates that, overall, a given state has a stronger policy combination to facilitate decreased exemption rates, as compared with other states. The designation of “less effective” indicates that, overall, a given state’s policy combination is less strong when compared with other states. Mississippi and West Virginia did not permit nonmedical exemptions from vaccination requirements during our study period. Their scores were not included in the index for total exemptions.
DISCUSSION
Our study may be the most comprehensive and contemporary longitudinal assessment of immunization laws in the United States with respect to their effect on both vaccination coverage and exemptions. We show novel findings of higher vaccination coverage and lower nonmedical exemption rates for MMR and DTaP vaccines in states adopting ACIP guidelines for school entry. By referring to the ACIP guidelines in their legislative code, states are ensuring that their executive agencies (eg, the DOH, school systems) are required to maintain consistent and current standards for childhood vaccinations. Adherence to these best practices was a successful strategy to increase vaccination coverage and reduce vaccination exemptions.
Although states with vaccine-related education requirements often have more rigorous exemption processes, how the education is communicated to hesitant parents varies by state and may be vital to ensuring high vaccination coverage [17, 18]. Our findings show that states with laws requiring parents to receive vaccination-related education from the DOH had higher MMR and DTaP vaccination coverage. However, the state law requiring parents to receive vaccination-related education from health care providers during the exemption application process was associated with increased nonmedical exemptions. Although the delivery mechanism of DOH-provided education varies across states (eg, online module with printed completion certificate, in-person educational session, or parent acknowledgement that evidence-based material has been reviewed on the application form), the content presented to parents is standardized and evidence based [19–21]. In other words, each parent in a given state receives the same educational content, whereas education delivered by medical providers is not necessarily beholden to this same standard of consistency. Provider-led education may also face opposition from parents who feel strongly about not vaccinating their children and may backfire [18]. This requirement may place strain on the patient–provider relationship, with some providers choosing to discharge patients whose parents continue to refuse vaccination [22]. Parents seeking exemptions for their children may seek care from providers who are more willing to accommodate this choice, thereby reducing the impact of any education provided [23, 24]. In addition, under some state laws, providers conducting education and/or signing exemptions may include providers who are traditionally opposed to vaccination (ie, chiropractors, naturopaths) negatively impacting the effect of provider-led education on nonmedical exemptions [25]. This discordant impact of state-mandated parental education is a noteworthy phenomenon that requires further investigation.
Allowance of religious and philosophical exemptions was associated with lower MMR and DTaP vaccination coverage and higher exemption rates, consistent with previous reports [5, 9, 26]. However, attempts to entirely remove the option of nonmedical exemptions should be weighed carefully and in the context of the relative rigor of all state-level immunization statutes to minimize the risk of public backlash [27, 28].
An interesting component to these results is that the trend of influence for direct referral to ACIP guidelines, DOH-led parental education, and provider-led parental education varied across years. It is possible that exogenous factors not tested within our models (ie, use of standing orders for vaccinations, improved access to health care, variability in the implementation of the Affordable Care Act and Medicaid expansion by state, and the stringency of regulatory oversight for compliance with the laws) may have influenced the interpretation, application, or individual behavior surrounding these specific laws. Additionally, the strength of laws and regulations is often contingent on awareness, compliance, and enforcement [29]. Although our study did not evaluate these components of implementation, this is an area for future research.
Consistent with a study by Bradford et al., our results found that state mandates for standardized exemption forms were associated with increased total and nonmedical exemption rates [11]. Although the standardization of the exemption process may benefit state DOHs in tracking and reporting exemption information, it likely also simplifies the process for securing an exemption.
Limitations
The variables used in these analyses are proxy measures for the implementation of state-level population policy levers designed to influence individual behavior (vaccine acceptance). State-level legislative measures lack the granular information available through county- or school-level assessments and are susceptible to modification through executive branch regulation, interpretation, and enforcement. Therefore, our analyses may not adequately account for the factors on the ground that directly modify the influence of immunization laws. Similarly, over the past several years, efforts on behalf of professional organizations (ie, American Academy of Pediatrics), the Centers for Disease Control and Prevention, and local and state health departments have intensified to address vaccine hesitancy and vaccine refusal. Increased vaccination rates may be a function of these efforts rather than legislative policy changes, and it is impossible for us to prove a causal relationship. Further, immunization laws have existed for years; it is impossible to say for certain if changes in vaccination rates during the study period were due to the cumulative effect of existing laws or legislative changes enacted during the study period. Also, our approach considered each legal component independently; therefore, we cannot assess the cumulative effect of multiple legal components together in a given state. In addition, state policy referring to ACIP guidelines was present in all but 5 states. As such, this variable could have simply been acting as a proxy for other state-level factors not measured in our study, and our findings may be influenced by other factors in the states that did not include ACIP recommendations.
Furthermore, the near-ubiquitous implementation of policies referring to ACIP guidelines across the United States leaves limited room for action in this area. Additional analysis of other factors outside of ACIP guidelines, such as DOH-led parental education programs, would benefit our understanding of policy actions that may influence vaccination coverage and exemption behaviors.
School vaccination coverage report data obtained through the CDC are gathered through multiple methods that vary by state. These methods may have introduced inaccuracies or bias into our findings. Some states did not report outcome data during the years of this study (up to 6% missing data). Missing data was addressed through the use of the restricted maximum likelihood estimating the method in the mixed effects models, which can provide unbiased estimates and standard errors for incomplete repeated-measures data sets [30].
CONCLUSION
State laws had variable associations on state vaccination coverage or exemption rates for DTaP and MMR vaccines. The most effective laws, whether designed to improve coverage or minimize exemptions, employed best practices and evidence-based education. Future efforts should focus on enforcement and funding of effective policies such as following ACIP guidelines to optimize state vaccination coverage levels and reduce the risk of disease transmission.
Acknowledgments
The authors would like to thank Dr. Amy Campbell for her assistance reviewing legal documents and Ranee Seither, MPH, for her technical assistance with the CDC data. We would like to acknowledge Ms. Ellen Darabaner, MLS, for her librarian assistance and expertise and Dr. Bradford for sharing his methodology of index development. The manuscript also benefited from the thoughtful editorial contributions of Allison Krug, MPH.
Author contributions. Dr. Shaw conceptualized and designed the study and data collection instrument and critically reviewed and revised all drafts of the manuscript. Emily Mader, MPH, MPP, designed the data collection instrument, conducted data analysis, drafted the initial manuscript, and reviewed subsequent drafts. Brittany Bennett, MPH, collected and entered data and reviewed the manuscript. Olesya Vernyi-Kellogg, Esq, collected data from the Thomson Reuters Westlaw and the Inter-university Consortium for Political and Social Research State Vaccination Requirements and Exemption Law Databases, assisted with interpretation of legal language from other sources (ie, the DOH), and reviewed the manuscript. Dr. Yang critically reviewed and revised the manuscript and assisted with interpretation of the legal code and findings. Dr. Morley designed the study, oversaw the analysis, and critically reviewed the manuscript.
All authors approved the final draft of the manuscript and agreed to be accountable for all aspects of the work.
Financial support. This work was partially supported by the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) under grant number D54HP23297 (“Academic Administrative Units”), for roughly $10 000 (total award amount $154 765; 90% of this project was financed with nongovernmental sources), corresponding to the amount of effort dedicated to this project by the lead author. The information, content, and conclusions are those of the authors and should not be construed as the official position or policy of the HRSA, HHS, or the US Government, nor should any endorsements be inferred by the HRSA, HHS, or the US Government.
Potential conflicts of interest. Dr. Shaw served as consultant for Pfizer, Inc. All other authors have no conflicts to disclose. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Omer SB, Salmon DA, Orenstein WA, et al. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med 2009; 360:1981–8. [DOI] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention. Measles | cases and outbreaks Available at: http://www.cdc.gov/measles/cases-outbreaks.html. Accessed 12 April 2016.
- 3. State laws. S381, Reg Sess 2015–2016 (RI 2015); H522, 52nd Leg (NM 2015); S3 46, Reg Sess 2015–2016 (NC 2015); H212, Reg Sess 2015–2016 (VT 2015); H687, Reg Sess 2015–2016 (MD 2015); H2006, 84th Leg (TX 2015) Maine, Pennsylvania, Texas, and Washington: H2009, Reg Sess 2015–2016 (WA 2015); H419, 127th Sess (ME 2015); H883, Reg Sess 2015–2016 (PA 2015); H2006, 84th Leg (TX 2015); S381, Reg Sess 2015–2016 (RI 2015); H522, 52nd Leg (NM 2015); S346, Reg Sess 2015–2016 (NC 2015); H212, Reg Sess 2015–2016 (VT 2015); H687, Reg Sess 2015–2016 (MD 2015); H2006, 84th Leg (TX 2015); H277, Reg Sess 2015–2016 (CA 2015); H98, Reg Sess 2015–2016 (VT 2015).
- 4. Seither R, Calhoun K, Knighton CL, et al. Vaccination coverage among children in Kindergarten - United States, 2014-15 School Year. MMWR Morb Mortal Wkly Rep 2015; 64:897–904. [DOI] [PubMed] [Google Scholar]
- 5. Shaw J, Tserenpuntsag B, McNutt LA, Halsey N. United States private schools have higher rates of exemptions to school immunization requirements than public schools. J Pediatr 2014; 165:129–33. [DOI] [PubMed] [Google Scholar]
- 6. Lai YK, Nadeau J, McNutt LA, Shaw J. Variation in exemptions to school immunization requirements among New York State private and public schools. Vaccine 2014; 32:7070–6. [DOI] [PubMed] [Google Scholar]
- 7. Thompson JW, Tyson S, Card-Higginson P, et al. Impact of addition of philosophical exemptions on childhood immunization rates. Am J Prev Med 2007; 32:194–201. [DOI] [PubMed] [Google Scholar]
- 8. Rota JS, Salmon DA, Rodewald LE, et al. Processes for obtaining nonmedical exemptions to state immunization laws. Am J Public Health 2001; 91:645–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Omer SB, Pan WK, Halsey NA, et al. Nonmedical exemptions to school immunization requirements: secular trends and association of state policies with pertussis incidence. JAMA 2006; 296:1757–63. [DOI] [PubMed] [Google Scholar]
- 10. Yang YT, Debold V. A longitudinal analysis of the effect of nonmedical exemption law and vaccine uptake on vaccine-targeted disease rates. Am J Public Health 2014; 104:371–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bradford WD, Mandich A. Some state vaccination laws contribute to greater exemption rates and disease outbreaks in the United States. Health Aff (Millwood) 2015; 34:1383–90. [DOI] [PubMed] [Google Scholar]
- 12. Westlaw Online Legal Research | Legal Solutions Available at: http://legalsolutions.thomsonreuters.com/law-products/westlaw-legal-research/. Accessed 12 April 2016.
- 13. State Vaccination Requirements and Exemption Law Database Available at: http://www.icpsr.umich.edu/icpsrweb/HMCA/studies/34486. Accessed 9 September 2015.
- 14. Area Health Resources Files Available at: http://ahrf.hrsa.gov/. Accessed 12 April 2016.
- 15. US Census Bureau. American Community Survey. Available at: https://www.census.gov/programs-surveys/acs/. Accessed 22 December 2015.
- 16. US Census Bureau. Small Area Income and Poverty Estimates (SAIPE) Program. Available at: https://www.census.gov/did/www/saipe/. Accessed 12 January 2016.
- 17. Blank NR, Caplan AL, Constable C. Exempting schoolchildren from immunizations: states with few barriers had highest rates of nonmedical exemptions. Health Aff (Millwood) 2013; 32:1282–90. [DOI] [PubMed] [Google Scholar]
- 18. Nyhan B, Reifler J, Richey S, Freed GL. Effective messages in vaccine promotion: a randomized trial. Pediatrics 2014; 133:e835–42. [DOI] [PubMed] [Google Scholar]
- 19. Oregon Health Authority. Nonmedical vaccine exemptions Available at: https://public.health.oregon.gov/PreventionWellness/VaccinesImmunization/GettingImm unized/Pages/non-medical-exemption.aspx#parents. Accessed 29 April 2016.
- 20. Michigan Department of Health and Human Services. Immunization waiver information Available at: http://www.michigan.gov/mdhhs/0,5885,7-339- 73971_4911_4914_68361-344843-- 00.html. Accessed 29 April 2016.
- 21. Vermont Department of Health. School entry immunization Available at: http://healthvermont.gov/hc/imm/schoolentry.aspx. Accessed 29 April 2016.
- 22. O’Leary ST, Allison MA, Fisher A, et al. Characteristics of physicians who dismiss families for refusing vaccines. Pediatrics 2015; 136:1103–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mergler MJ, Omer SB, Pan WK, et al. Association of vaccine-related attitudes and beliefs between parents and health care providers. Vaccine 2013; 31:4591–5. [DOI] [PubMed] [Google Scholar]
- 24. Delamater PL, Leslie TF, Yang YT. Change in medical exemptions from immunization in California after elimination of personal belief exemptions. JAMA 2017; 318:863–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Washington State Department of Health. School and Child Care Exemptions. Available at: https://www.doh.wa.gov/CommunityandEnvironment/Schools/Immunization/Exemptions. Accessed 7 September 2016.
- 26. Omer SB, Richards JL, Ward M, Bednarczyk RA. Vaccination policies and rates of exemption from immunization, 2005-2011. N Engl J Med 2012; 367:1170–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rogers K. California doctors are advertising ludicrous medical exemptions to anti-vaxxers Available at: http://motherboard.vice.com/read/california-doctors-are-advertising-ludicrous- medical-exemptions-to-anti-vaxxers-vaccines-vaccinations-sb277. Accessed 6 May 2016.
- 28. Gostin LO. Law, ethics, and public health in the vaccination debates: politics of the measles outbreak. JAMA 2015; 313:1099–100. [DOI] [PubMed] [Google Scholar]
- 29. Fell JC, Waehrer G, Voas RB, et al. Effects of enforcement intensity on alcohol impaired driving crashes. Accid Anal Prev 2014; 73:181–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Littell RC, Henry PR, Ammerman CB. Statistical analysis of repeated measures data using SAS procedures. J Anim Sci 1998; 76:1216–31. [DOI] [PubMed] [Google Scholar]