Abstract
Background: Although previous research on advance care planning (ACP) has associated ACP with improved quality of care at the end of life, the appropriate use of ACP remains limited.
Objective: To evaluate the impact of a pilot program using the “Honoring Choices Wisconsin” (HCW) model for ACP in a tertiary care setting, and to understand barriers to system-wide implementation.
Design: Retrospective review of prospectively collected data.
Setting/Subjects: Patients who received medical or surgical oncology care at Froedtert and the Medical College of Wisconsin.
Measurements: Patient demographics, disease characteristics, patient satisfaction, and clinical outcomes.
Results: Data from 69 patients who died following the implementation of the HCW program were reviewed; 24 patients were enrolled in the HCW program while 45 were not. Patients enrolled in HCW were proportionally less likely to be admitted to the ICU (12.5% vs. 17.8%) and were more likely to be “do not resuscitate” (87.5% vs. 80.0%), as well as have a completed ACP (83.3% vs. 79.1%). Furthermore, admission to a hospice was also higher among patients who were enrolled in the HCW program (79.2% vs. 25.6%), with patients enrolled in HCW more likely to die in hospice (70.8% vs. 53.3%). The HCW program was favorably viewed by patients, patient caregivers, and healthcare providers.
Conclusions: Implementation of a facilitator-based ACP care model was associated with fewer ICU admissions, and a higher use of hospice care. System-level changes are required to overcome barriers to ACP that limit patients from receiving end-of-life care in accordance with their preferences.
Keywords: : advanced care planning, advanced directive, end of life, palliative care, patient-centered
Introduction
Advance care planning (ACP) represents a voluntary process of communication between patients, family members/caregivers, and healthcare professionals to understand, review, and plan future healthcare decisions in accordance with the patient's preferences.1 Although previous research has associated ACP with improved quality of care at the end of life and fewer in-hospital deaths among patients, the appropriate use of ACP remains limited.2–5 Furthermore, while much of the current focus on ACP care models has been on improving completion rates of advanced directives (ADs), recent research suggests that although useful, such initiatives do not necessarily improve the quality of medical care or end-of-life care provided.6 Rather, facilitator-based care models of ACP have demonstrated that a coordinated, systematic, and patient-centered approach to ACP can more effectively improve clinical outcomes for patients, while also ensuring that patient preferences are followed.7–10 The current report describes the process of implementing an ACP pilot program in a tertiary setting and the impact on patient healthcare outcomes and family/caregiver satisfaction.
Materials and Methods
Phase I: Strategy and planning
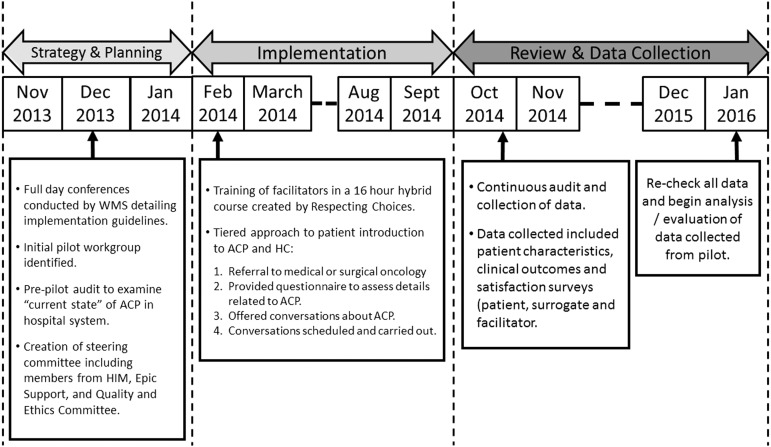
In 2013, our group joined “Honoring Choices Wisconsin” (HCW) a state-wide initiative designed to increase advocacy and education around ACP, utilizing a trained facilitator framework modeled after “Respecting Choices” (Fig. 1).11 A pilot team was assembled at our cancer center consisting of seven members: two physician champions (from the Division of Surgical Oncology and the Palliative Care Center), a clinical nurse specialist, a nurse coordinator, social worker, and two hospital chaplains. Social workers and nurses from the cancer center clinic and surgical wards were also involved to facilitate a better follow-up with patients and families across different clinical settings. As the pilot involved several layers of administrative process change and system work, Froedtert and the Medical College of Wisconsin (F&MCW) Quality Department coordinated resources to examine the “current state” of ACP in our system to identify gaps and redundancies in our system.
FIG. 1.
Planning, implementation and review of our pilot model.
Phase II: Implementation
A critical component of the pilot activity was facilitator training (16-hour hybrid online and in-person course).12 Facilitators introduced individuals and families to ACP conversations, using a tiered approach over the four-month pilot period. First, patients referred to Surgical or Medical Oncology received a letter at the time of appointment scheduling which outlined the pilot program and provider support and benefits of participation in ACP. During their appointment, patients were provided a questionnaire with queries related to ACP planning; past conversations, documents, and desire to meet regarding ACP or to revisit and/or explore future decision making. This tool was used to audit and track responses, and assisted in the future scheduling of patients seeking further information.
Phase III: Post-pilot review, data collection, and statistical analysis
In addition to documenting patient participation and completion of satisfaction surveys by patients, surrogates, and facilitators, a retrospective review of patient information and clinical outcomes among patients who died following implementation of the pilot program was performed. Categorical data were compared using Pearson's chi-squared test, while Student's t test was used to compare normally distributed continuous data, and the Kruskal–Wallis test to compare non-normally distributed continuous data. Statistical significance was defined by a p-value of <0.05. All analyses were performed using STATA statistical software, version 14.0 (StataCorp, College Station, TX).
Results
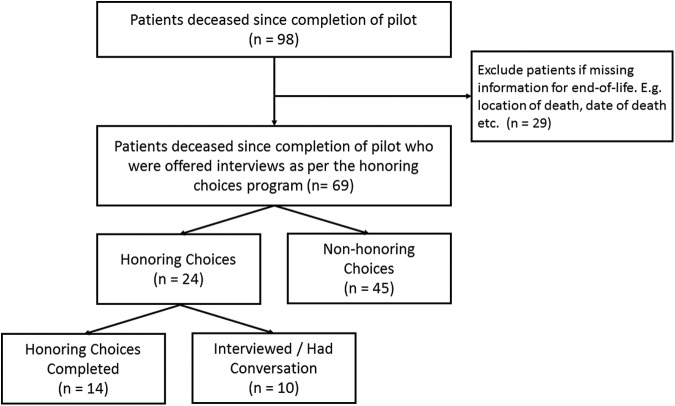
HCW pilot participation and patient characteristics of patients who died following the pilot
HCW participation was offered to 61% (294/483) of patients. Ninety-Five patients completed a meeting with a certified facilitator; 98 patients died following the completion of the pilot. Complete data on end-of-life care and location/date of death were available for 69 patients (Fig. 2); HCW ACP was initiated in 24 (35.3%, 24 of 69) patients with 14 patients completing the HCW program and 10 patients completing only the preliminary interview. Patients enrolled in the HCW program were proportionally more likely to belong to racial minority (20.0% vs. 83.3%, Table 1), were more likely to be admitted with an ACP (79.1% vs. 83.3%), and were less likely to be admitted to an ICU (17.8% vs. 12.5%). Furthermore, patients enrolled in HCW were more likely to be admitted with a “do not resuscitate” status (80.0% vs. 87.5%), be admitted to a hospice (74.4% vs. 79.2%), and die in a hospice (death in hospice: 53.3% vs. 70.8%), although these differences were not observed to be statistically significant (all p > 0.05).
FIG. 2.
Inclusion/exclusion criteria and derivation of final study cohort.
Table 1.
Comparison of Patient Characteristics and Clinical Outcomes between Patients Who Were Enrolled in Honoring Choices Program and Those Who Were Not
| Non-honoring choices | Honoring choices | Total | |||||
|---|---|---|---|---|---|---|---|
| Characteristic | N 45 | % 100.0% | N 24 | % 100.0% | p | N 69 | % 100.0% |
| Patient sex | 0.202 | ||||||
| Male | 26 | 57.8 | 10 | 41.7 | 36 | 52.2 | |
| Female | 19 | 42.2 | 14 | 58.3 | 33 | 47.8 | |
| Patient race | 0.052 | ||||||
| White | 36 | 80.0 | 14 | 16.7 | 50 | 72.5 | |
| Black | 8 | 17.8 | 6 | 58.3 | 14 | 20.3 | |
| Other/not specifieda | 1 | 2.2 | 4 | 25.0 | 5 | 7.3 | |
| Marital status | 0.850 | ||||||
| Married | 31 | 68.9 | 16 | 66.7 | 47 | 68.1 | |
| Single/divorced/widower | 14 | 31.1 | 8 | 33.3 | 22 | 31.9 | |
| Admitted within last six weeks of life | 0.592 | ||||||
| Yes | 31 | 68.9 | 15 | 62.5 | 46 | 66.7 | |
| No | 14 | 31.1 | 9 | 37.5 | 23 | 33.3 | |
| Admitted to ICU | 0.568 | ||||||
| Yes | 8 | 17.8 | 3 | 12.5 | 11 | 15.9 | |
| No | 37 | 82.2 | 21 | 87.5 | 58 | 84.1 | |
| Number of ICU days | |||||||
| Number of ICU days per patient, median (IQR)b | 1.5 (1–6) | 6 (1–12) | 0.520 | 2 (1–10) | |||
| Number of ICU days per patient, mean (SD)b | 4.6 (6.6) | 6.3 (5.5) | 0.700 | 5.1 (6.1) | |||
| Number of hospital days | |||||||
| Number of hospital days per patient, median (IQR) | 5 (0–8) | 5 (0–10.5) | 0.848 | 5 (0–9) | |||
| Number of hospital days per patient, mean (SD) | 5.42 (5.63) | 7.17 (9.17) | 0.331 | 6.02 (7.04) | |||
| Admitted to ED | 0.825 | ||||||
| Yes | 25 | 55.6 | 14 | 58.3 | 39 | 56.5 | |
| No | 20 | 44.4 | 10 | 41.7 | 30 | 43.5 | |
| Treatment received | |||||||
| Surgery | 0.495 | ||||||
| Yes | 11 | 24.4 | 7 | 29.2 | 18 | 26.1 | |
| No | 34 | 75.6 | 17 | 70.8 | 51 | 73.9 | |
| Chemotherapy | 0.611 | ||||||
| Yes | 9 | 20.0 | 6 | 25.0 | 15 | 21.7 | |
| No | 36 | 80.0 | 18 | 75.0 | 54 | 78.3 | |
| DNR status | 0.434 | ||||||
| Yes | 36 | 80.0 | 21 | 87.5 | 12 | 17.4 | |
| No | 9 | 20.0 | 3 | 12.5 | 57 | 82.6 | |
| Advanced care planning | 0.296 | ||||||
| Yes | 34 | 79.1 | 20 | 83.3 | 54 | 80.6 | |
| No | 9 | 20.9 | 4 | 16.7 | 13 | 19.4 | |
| Admission to hospice | 0.662 | ||||||
| Yes | 32 | 25.6 | 19 | 79.2 | 51 | 76.1 | |
| No | 11 | 74.4 | 5 | 20.8 | 16 | 23.8 | |
| Length of stay in hospice, days per patient, median (IQR)c | 16 (5.5–29) | 17 (8–23) | 0.762 | 16.5 (6–28) | |||
| Length of stay in hospice, days per patient, mean (SD)c | 25.4 (32.6) | 28.8 (40.3) | 0.747 | 26.6 (35.2) | |||
| Location of death | 0.370 | ||||||
| Hospice | 24 | 53.3 | 17 | 70.8 | 41 | 59.4 | |
| Home | 6 | 13.3 | 2 | 8.3 | 8 | 11.6 | |
| Otherd | 15 | 33.3 | 5 | 20.8 | 20 | 29.0 | |
Includes Hispanic, Asian, and not-specified/unknown.
Only among patients who were admitted to the ICU (n = 11).
Only among patients who were admitted to hospice (n = 51).
Includes patients who died within the hospital or at other related facilities.
Patient and provider evaluation of pilot program
Among the 32 patients who completed the survey, the HCW pilot program was perceived as favorable with a majority of patients reporting a “satisfactory” score (Table 2). Specifically, most patients reported that conversations as part of the HCW program were “helpful” (mean score = 4.97) and that they equipped patients with information that allowed them to make better decisions pertaining to their healthcare needs/preferences (mean score = 4.91). A similar pattern was also observed among healthcare agents/patient caregivers who suggested that the HCW better prepared them to understand healthcare decisions (mean score = 4.90) and make more informed healthcare decisions to honor the choices of their loved ones (mean score = 4.75). Although facilitators (n = 20) who completed the survey suggested that the program was easy to understand and complete, as well as being appropriate for patients to express their opinions/preferences, most suggested that significant improvements could be made to the wording of the HCW program and identified the use of technical terms as a source of confusion with patients (mean score = 3.95).
Table 2.
Trial Participant Evaluation
| Participants | Survey questions | Mean scorea | Example quotes |
|---|---|---|---|
| Patients (n = 32) | I feel this discussion was helpful to me | 4.97 | “Really helpful for patient and family” |
| “Excellent!” | |||
| “She made me aware of things I hadn't thought of” | |||
| “Thank you for helping me explain my wishes to my husband” | |||
| I feel better prepared to make decisions about my future healthcare needs | 4.91 | ||
| I feel the facilitator did a good job of helping me with my needs for advanced care planning | 4.97 | “I feel she made me aware of all things I needed to know” | |
| “She was very thorough and asked if I had questions. Her answers were clear and easy to understand” | |||
| “Everything was done professionally and tactfully” | |||
| “Excellent!” | |||
| Healthcare Agent (n = 20) | I feel the discussion has better prepared me to make healthcare decisions for my loved one | 4.90 | “I felt the discussion helped me be aware of what I needed to know” |
| I feel motivated to have further discussions with my loved one regarding his/her choices for future healthcare decisions. | 4.75 | “Really helped us have the conversation he never wants to have” | |
| I feel the facilitator did a good job of helping me understand my role in making healthcare decisions for my loved one in the future, if needed. | 4.95 | “I might not be the right choice” | |
| “Very pleased with her knowledge and ability to listen to our concerns” | |||
| Facilitator (n = 20) | Did the participant easily understand the instructions for completing an ACP | 4.45 | “Easy to follow along with discussion on each decision point” |
| “Thought document was too in depth” | |||
| “With explanation” | |||
| “Very well worded, not much needed to be clarified” | |||
| Did you find the document adequate for expressing his/her preferences? | 4.85 | “The patient and her husband expressed how nice and detailed the form was” | |
| “Very pleased with everything and so appreciative!” | |||
| “Wished for document to be completed sooner” | |||
| “She was able to gain a better understanding of the difference between being decisional and dying vs. not being decisional with no chance of recovery. She reflected that further understanding offered her some peace” | |||
| Were there confusing words or statements in the document you had to clarify | 3.95 | “Further clarification needed on medical interventions” | |
| “Clarification on IV Hydration and Feeding Tube use” | |||
| “CPR question needed more clarification” | |||
| “CPR and life sustaining measures clarified” | |||
| “Needed clarification for terms such as ventilator and CPR” | |||
| “Nursing home question caused some confusion” |
Mean score ranges from 1 to 5; 1 = not satisfied; 5 = satisfied.
ACP, advance care planning.
Discussion
Results from the current study are consistent with the limited data evaluating the use and efficacy of ACP models.9,10 In a recent report from Pecanac and colleagues describing their experiences of implementing an ACP model at a single, 300-bed medical center, the authors reported that implementation of an ACP model was associated with a decreased use of ICUs, an increase in the proportion of patients with a complete ACP, and a significant decrease in racial disparities with regard to end-of-life care planning.10 We similarly observed that admission to an ICU decreased from 17.8% among patients who did not complete the HCW program to 12.5% among those who competed the HCW program. Conversely, completion of an ACP increased from 79% among those not completing the HCW program to over 83% among those who completed the HCW program. Although the high completion of ACPs likely suggests a selection bias in our patient cohort, other studies have reported a comparable ACP completion ranging from 12.5% to 65.6% varying by patient and/or hospital characteristics.6,13 Taken together with existing literature, our data highlight the potential impact ACP models may have in promoting end-of-life discussions and in ensuring that a greater proportion of patients receive care in accordance with their wishes/choices.
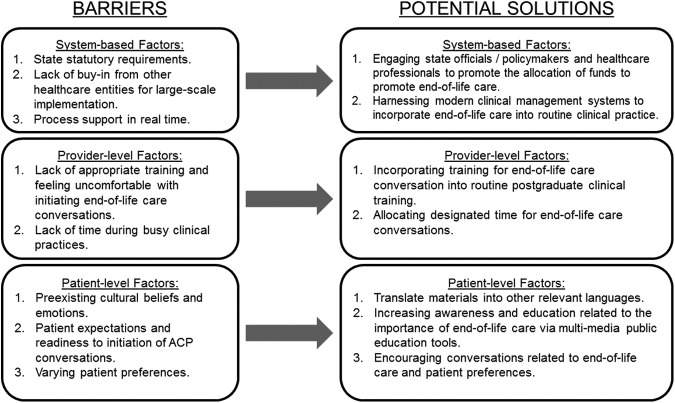
Although favorably perceived, several barriers to the widespread implementation were identified, which can be broadly classified to the levels of the patient, provider, and healthcare system (Fig. 3). Of these, patient-level factors were perhaps of greatest significance and included preexisting patient cultural beliefs, patient expectations/preferences, and readiness to the initiation of ACP conversations. For example, we observed that patients were more likely to engage in end-of-life care conversations if they were promoted in a culturally sensitive manner and if they were easy to understand and interpret. As such, a potential strategy to overcome the preexisting cultural barriers could be to ensure that ACP guidelines are translated into multiple languages catering to a diverse patient population while also being culturally sensitive and relevant to all patient groups. In addition, our study also identified several provider-level and system-based factors limiting ACP, including the lack of appropriate training for end-of-life communication and a lack of resources to ensure large-scale implementation of our program. In our experience, participation in the HCW pilot program created a sense of “community” and shared passion around ACP among facilitators and was pivotal in identifying gaps in our ACP system, while also highlighting the future steps needed to implement cultural change on a system-wide level. Moving forward, healthcare systems should adopt structured, systematic programs that address ACP for patients with serious illnesses.14,15
FIG. 3.
Patient, provider and system-based barriers to the implementation of our pilot model and potential strategies to overcome these barriers.
The current study should be interpreted with several limitations. First, being a single-center study, our results may not be generalizable to other centers given differences in patient populations and case mix. Second, outcome data were available for only 69 patients, thereby limiting our analysis and statistical power. Third, as our satisfaction surveys were not completed by all participants, the high rankings from respondents may capture only those highly satisfied with the process and may not be reflective of all patients who were treated. Finally, a significant proportion of patients were from out-of-state or neighboring areas resulting in limited accrual of follow-up data for these patients.
In conclusion, implementation of the Wisconsin Medical Society (WMS)-sponsored HCW pilot program resulted in lower use of ICUs and higher use of hospice care. Although well received by patients, surrogates, and healthcare providers, significant barriers to implementing ACP systems were identified. Moving forward, system-level changes are needed to normalize conversations around ACP and to ensure that documented wishes are followed.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Sumalinog R, Harrington K, Dosani N, Hwang SW: Advance care planning, palliative care, and end-of-life care interventions for homeless people: A systematic review. Palliat Med 2016;31:109–119 [DOI] [PubMed] [Google Scholar]
- 2.Houttekier D, Cohen J, Cools F, et al. : Advance care planning for end-of-life care. Cochrane Database of Systematic Reviews 2012;2 (DOI: 10.1002/14651858/CD009618) [DOI] [Google Scholar]
- 3.Gomes B, Calanzani N, Curiale V, et al. : Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database Syst Rev 2013:CD007760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qaseem A: Evidence-based interventions to improve the palliative care of pain, dyspnea, and depression at the end of life: A clinical practice guideline from the American College of Physicians. Ann Intern Med 2008;148:141. [DOI] [PubMed] [Google Scholar]
- 5.Zimmermann C, Riechelmann R, Krzyzanowska M, et al. : Effectiveness of specialized palliative care: A systematic review. JAMA 2008;299:1698–709 [DOI] [PubMed] [Google Scholar]
- 6.Wilson KS, Kottke TE, Schettle S: Honoring choices Minnesota: Preliminary data from a community-wide advance care planning model. J Am Geriatr Soc 2014;62:2420–2425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Respecting Choices®—Gundersen Health System. www.gundersenhealth.org/respecting-choices/ (Last accessed November3, 2016)
- 8.Moorman SM, Carr D, Kirchhoff KT, Hammes BJ: An assessment of social diffusion in the respecting choices advance care planning program. Death Stud 2012;36:301–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Song M-K, Kirchhoff KT, Douglas J, et al. : A randomized, controlled trial to improve advance care planning among patients undergoing cardiac surgery. Med Care 2005;43:1049–1053 [DOI] [PubMed] [Google Scholar]
- 10.Pecanac KE, Repenshek MF, Tennenbaum D, Hammes BJ: Respecting choices® and advance directives in a diverse community. J Palliat Med 2014;17:282–287 [DOI] [PubMed] [Google Scholar]
- 11.Honoring Choices Wisconsin—Wisconsin Medical Society. www.wisconsinmedicalsociety.org/professional/hcw/ (Last accessed November3, 2016)
- 12.Online Curriculum—Gundersen Health System. www.gundersenhealth.org/respecting-choices/online-curriculum/ (Last accessed November3, 2016)
- 13.Harrison KL, Adrion ER, Ritchie CS, et al. : Low completion and disparities in advance care planning activities among older medicare beneficiaries. JAMA Intern Med 2016;176:1872–1875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernacki RE, Ko DN, Higgins P, et al. : Improving access to palliative care through an innovative quality improvement initiative: An opportunity for pay-for-performance. J Palliat Med 2012. 15:192–199 [DOI] [PubMed] [Google Scholar]
- 15.Holley JL, Carmody SS, Moss AH, et al. : The need for end-of-life care training in nephrology: National survey results of nephrology fellows. Am J Kidney Dis 2003. 42:813–820 [DOI] [PubMed] [Google Scholar]