Abstract
Objectives: The American Southeast has been labeled the “Stone Belt” due to its relatively high burden of urinary stone disease, presumed to be related to its higher temperatures. However, other regions with high temperatures (e.g., the Southwest) do not have the same disease prevalence as the southeast. We seek to explore the association of stone disease to other climate-associated factors beyond temperature, including precipitation and temperature variation.
Methods: We identified all patients who underwent a surgical procedure for urinary stone disease from the California Office of Statewide Health Planning and Development (OSHPD) databases (2010–2012). Climate data obtained from the National Oceanic and Atmospheric Administration (NOAA) were compared to population adjusted county operative stone burden, controlling for patient and county demographic data as potential confounders.
Results: A total of 63,994 unique patients underwent stone procedures in California between 2010 and 2012. Multivariate modeling revealed that higher precipitation (0.019 average increase in surgeries per 1000 persons per inch, p < 0.01) and higher mean temperature (0.029 average increase in surgeries per 1000 persons per degree, p < 0.01) were both independently associated with an increased operative stone disease burden. Controlling for county-level patient factors did not change these observed effects.
Conclusions: In the state of California, higher precipitation and higher mean temperature are associated with increased rates of stone surgery. Our results appear to agree with the larger trends seen throughout the United States where the areas of highest stone prevalence have warm wet climates and not warm arid climates.
Keywords: : urolithiasis, outcomes, geography, climate
Introduction
Urinary stone disease is a common and potentially debilitating disease. In the United States, the lifetime prevalence of urinary stone disease has been estimated to be between 10% and 15%.1–3 Treating urinary stone disease is costly, with estimated expenditures of 2.1 billion dollars in 2001,4 and the prevalence and burden of urinary stone disease are increasing.5 Given the impact of urinary stone disease, there is a need to define both the intrinsic and extrinsic risk factors in its development. Intrinsic risks include chronic disease (e.g., insulin resistance), male sex, and genetic predisposition,6–10 while extrinsic factors include but are not limited to diet, certain medication use, and immobility.
Geographic variation is one of the most studied extrinsic factors affecting urinary stone disease risk. A landmark study characterizing stone prevalence in the United States using data from the Cancer Prevention Study II11 established the concept of a “stone belt.” It identified an increasing prevalence of urinary stone disease in the United States moving from north to south and west to east.12 Many have interpreted the stone belt maps to support the conclusion that higher temperatures are associated with increased risk of stone disease.13 This is postulated to occur secondary to insensible water loss from perspiration, which leads to dehydration, urine concentration, and urine supersaturation.
However, higher temperature does not fully account for the stone belt phenomenon. If temperature alone was the primary environmental driving factor, the American Southwest should have a similar stone prevalence to the Southeast. Although the differences between the two areas could be related to intrinsic patient factors endemic to those areas, it is interesting to note that there are important environmental differences between the two regions. Specifically, the Southeast has higher rates of precipitation, while a large portion of the Southwest is arid desert.14
We hypothesized that increased precipitation is an unrecognized extrinsic risk factor for urinary stone disease because it imposes a greater burden for thermoregulation in individuals who live in hot wet climates as opposed to hot dry climates.15 In this study, we sought to test the associations among temperature, precipitation, and operative urinary stone disease in California, a populous state with a varied climate.
Methods
After obtaining permission from the California Protection of Human Subjects Committee, we utilized data from the California Office of Statewide Health Planning and Development (OSHPD) to identify all inpatient and outpatient kidney stone procedures, including ureteroscopy, extracorporeal shockwave, and percutaneous procedures, from 2010 through 2012. We combined both the Patient Discharge Dataset (PDD) and Ambulatory Surgery Database (ASD) to identify inpatient and outpatient procedures, respectively. Together, the two datasets capture all inpatient or outpatient (if licensed by the California Department of Public Health) surgeries in the state of California at nonfederal facilities. There were a total of 337 unique facilities identified. For each encounter, as much as 25 diagnostic codes, in the form of the International Classification of Diseases, Ninth Revision (ICD-9), and 20 procedural codes (ICD-9 for PDD, current procedural terminology for ASD) exist. In addition, each patient encounter is coded with a unique patient identifier assigned to each individual person so that they can be followed longitudinally within and between datasets.
We chose patients undergoing operative stone procedures as our metric of burdensome stone disease. This included anyone undergoing ureteroscopic, percutaneous, or shockwave lithotripsy with a diagnosis of urolithiasis. We excluded those persons with a diagnosis associated with malignancy or stricture disease (Table 1).
Table 1.
Inclusion and Exclusion Criteria
| Procedure code | Diagnosis code for urolithiasis | Excluded codesa | |
|---|---|---|---|
| Inpatient | 56.0-ureteroscopic lithotripsy | 592.0 or 592.1 or 592.9 | Malignancy: 188.0–188.9, 189.1, 189.2, 189.8, 189.9 UPJ obstruction/ureteral stricture: 593.3, 593.2, 753.21 |
| 59.95 or 9851-shockwave lithotripsy | |||
| 55.03 or 55.04-percutaneous lithotripsy | |||
| Outpatient | 52,351 or 52,352 or 52,353-ureteroscopic lithotripsy | ||
| 50,590 for shockwave lithotripsy | |||
| 50,080 or 50,081 for percutaneous lithotripsy |
ICD-9 diagnosis codes that were excluded in the inpatient or outpatient setting.
UPJ = ureteropelvic junction.
Urinary stone procedures were examined at the county level (58 counties total). A patient's home zip code was used to map their county of residence using the R zip code package. Specifically, the zip code package provides an estimate of the longitude and latitude for the zip code, and this was used to assign a patient's county. Each individual with a stone procedure was only counted once, and when more than one zip code was available, we used the zip code associated with the first procedure. Each county's operative stone burden was then adjusted for overall county population, by dividing the number of persons with operative stone disease in that county by that county's population (obtained from the United States Census data for 2010). We reported this number in persons with operative stone disease per 1000 persons. Publicly available climate data for each county were obtained from the National Oceanic and Atmospheric Administration (NOAA) over the study period.16 The climate variables we chose to investigate included total annual precipitation, mean temperature, the annual number of days over 90°, and temperature variation. Temperature was expressed in degrees Fahrenheit (F), and temperature variation for each county was analyzed based on monthly temperatures and their variation around each county's annual mean temperature.
We controlled for relevant county-level population factors by accessing publicly available census data from the Centers for Disease Control and Prevention (CDC)'s Behavioral Risk Factor Surveillance System and from the US Census Bureau's Population Estimate Program17,18 over our study period. We included median county age, gender ratio of persons over 18, percentage of the population with diabetes, and percentage classified as obese (defined as body mass index >30) in our fully adjusted models.
Statistical analysis
We explored pair-wise associations between population adjusted county operative stone burden and variables of interest with univariate general linear regression models or the Student's t-test. We fit general multivariate linear regression models to measure the impact of our climate factors of interest, while controlling for county-level population factors, on the rate of operative stone disease. We obtained the model of best fit by performing backward stepwise elimination of variables. Specifically, variables were eliminated if their removal did not significantly decrease goodness of fit of the model by the likelihood ratio test. Statistical analysis was performed with R 3.3.1 software. Choropleth maps were created using the “choroplethr” package. A two-sided p-value of 0.05 was taken to indicate statistical significance.
Results
During the years 2010 to 2012, 63,994 patients underwent 81,861 urinary stone procedures in California. The patient demographics of the analytic cohort are included in Table 2. The mean patient age was 54.1 years (SD 15.6 years) and the cohort showed a slight predominance of men (56%). The population was 65.5% White, 17.6% Hispanic, 8.6% Asian, and 3.4% Black. The median county population was 181,098 persons with a mean of 605,893. Over the 58 counties in the state, the mean county operative stone disease rate was 1.77 per 1000 persons (range 0.05–3.16). The census county data revealed an overall mean county age of 36.1 years (range 19.0–44.6). There was a county average of 102.1 males per 100 females (range 86.0–192.2). The mean county prevalence of diabetes was 8.1% (range 5.7%–11.0%), and the mean prevalence of obesity was 24.5% (15.0%–31.8%) (Table 3).
Table 2.
Demographics of the 63,994 Patients Undergoing an Operation for Urinary Stone Disease
| Characteristic | |
|---|---|
| Age (years) | |
| Mean | 54.1 |
| SD | 15.6 |
| Surgerya, n (%) | |
| PCNL | 5491 (8.6) |
| SWL | 27,830 (43.5) |
| URS | 31,170 (48.7) |
| Payer, n (%) | |
| Private | 52,201 (81.6) |
| Medicare | 7497 (11.7 |
| Medi-Cal | 3248 (5.1) |
| Other | 1048 (1.6) |
| Race/ethnicity, n (%) | |
| White | 41,886 (65.5) |
| Hispanic | 11,249 (17.6) |
| Black | 2207 (3.4) |
| Asian | 5503 (8.6) |
| Other | 3149 (4.9) |
| Gender, n (%) | |
| Male | 35,645 (55.7) |
| Female | 28,349 (44.3) |
In all, 2130 patients had multiple types of procedures in the same encounter.
PCNL = percutaneous nephrolithotomy; SD = standard deviation; SWL = extracorporeal shockwave lithotripsy; URS = ureteroscopy.
Table 3.
County-Level Variables Descriptive Statistics and Multivariate Model for Operative Stone Burden Per 1000 Persons Per Year
| Variable | Mean (range) | β1a(95% CI β1) | pb |
|---|---|---|---|
| Temperature | 56.1 (36.9, 74.0) | 0.029 (0.004, 0.054) | 0.03 |
| Annual precipitation in inches | 32.6 (3.7, 75.6) | 0.020 (0.016, 0.022) | <0.01 |
| Median county age | 36.1 (29.0, 44.6) | 0.001 (−0.042, 0.044) | 0.99 |
| Ratio male/female | 1.02 (0.86, 1.92) | −0.001 (−0.003, 0.001) | 0.85 |
| % population with diabetes | 8.1 (5.7, 11.0) | −0.019 (−0.195, 0.157) | 0.83 |
| % population obese | 24.45 (15.0, 31.8) | 0.014 (−0.039, 0.067) | 0.60 |
The table above provides the overall descriptive statistics for the county climate data and demographic data. Also displayed is the slope and 95% CI of the multivariate model predicting County operative stone cases per 1000 persons.
Slope coefficient from multivariate model predicting county operative stone burden per 1000 persons before backward stepwise elimination.
Test of significance for coefficient from multivariate model predicting county operative stone burden per 1000 persons before backward stepwise elimination.
The annual mean temperature across the 58 counties was 56° (SD 7.4), the mean number of days over 90° was 46 (range 0–164), and the mean annual rainfall was 32.6 inches (range 3.7–75.6). In the regions with the lowest quartile of rainfall (<21 inches per year), the average stone surgery rate was 1.5 per 1000 persons compared with 2.2 per 1000 persons in the highest quartile of rainfall (>44 inches per year) (p < 0.01).
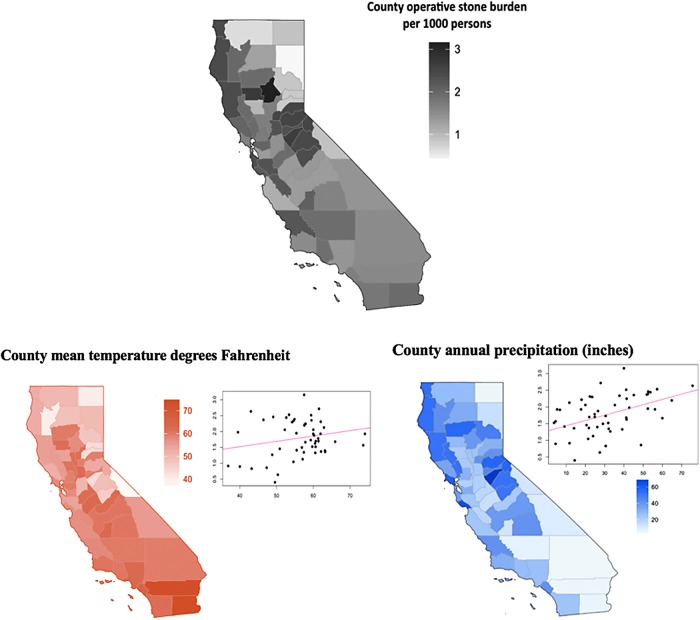
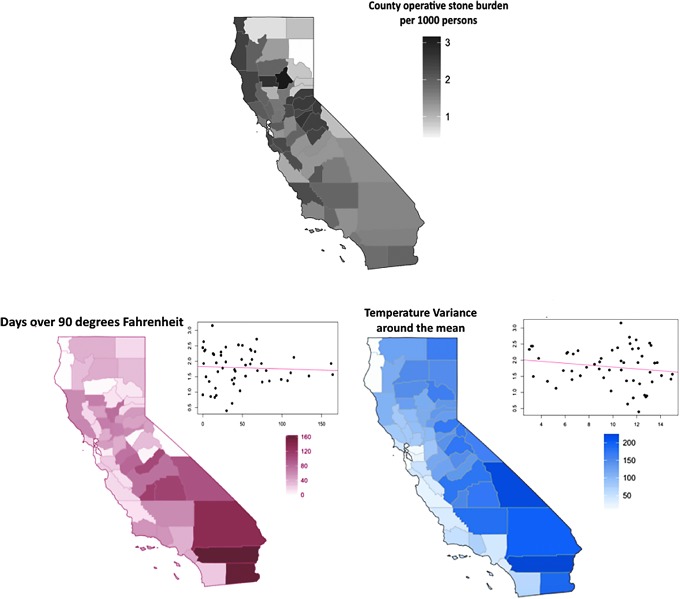
Of the four climate variables of interest (mean temperature, days over 90°, annual precipitation, and temperature variance), only rainfall was significantly associated with higher rates of operative stone burden in univariate modeling (Figs. 1 and 2). However, when precipitation was included in the model, both the number of days over 90° and annual mean temperature were associated with increased operative stone burden. With precipitation included, annual mean temperature was a better predictor than days over 90° for stone burden in our final model (log likelihood −38.6 and −41.6, p < 0.001) and including both temperature variables together did not improve the quality of the model fit (log likelihood −38.6 and −38.6, p = 0.87). For this reason, only annual mean temperature was kept in our final model.
FIG. 1.
Operative stone burden across the state of California and yearly precipitation and mean temperature. Each map shows the variables' relative magnitude for each county in California. The adjacent scatter plots compare the variable to county operative stone burden per 1000 persons. The fitted univariate regression line is also included on the scatter plots. With univariate modeling, only precipitation was significantly associated with county stone burden (p < 0.01). There was a trend toward significance for mean temperature (p = 0.10).
FIG. 2.
Operative stone burden across the state of California and days over 90° and temperature variation. Each map shows the variables' relative magnitude for each county in California. The adjacent scatter plots compare the variable to county operative stone burden per 1000 persons. The fitted univariate regression line is also included on the scatter plots. There was no significant association between stone burden and number of days over 90° (p = 0.41) and temperature variance (p = 0.23).
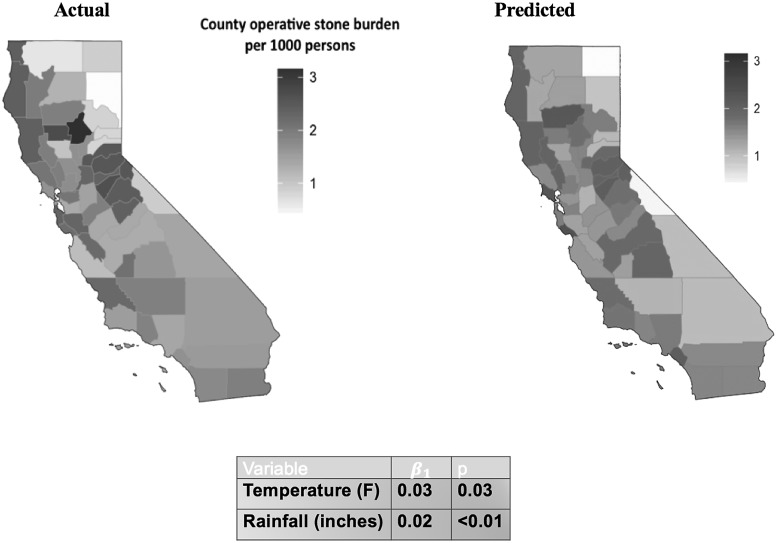
With multivariate modeling, annual precipitation (0.019 average increase in surgeries per 1000 persons per inch, p < 0.01) and mean temperature (0.029 average increase in surgeries per 1000 persons per degree, p < 0.01) were both independently associated with an increased operative stone disease burden (Fig. 3). The inclusion of county-level demographic factors (median county age, number of males per 100 females, obesity prevalence, and diabetes prevalence) in the fully-adjusted multivariate model did not change the significance or magnitude of the effects of precipitation and mean temperature on county operative stone burden (Table 3). The final model, including mean temperature and precipitation, accounted for 34% of the variance between county rates of operative urinary stone disease (Fig. 3).
FIG. 3.
Operative stone burden across the state of California by county: Mean temperature and annual precipitation fitted model. The right panel reveals the actual county operative stone burden per 1000 persons. The left panel reveals the fitted prediction of actual county operative stone burden per 1000 persons based on the model of best fit (the table with the model is on the bottom). Note that the similarities in the maps, as the best fit model, including only precipitation and mean temperature, explain ∼35% of the variance in operative stone burden between counties.
Discussion
In this study, we present operative stone disease prevalence (as a metric for overall urinary stone disease burden) over the 58 counties in California and defined the importance of climate and geography on stone disease prevalence. We found that increased annual precipitation and increased mean temperature were independently correlated with an increased rate of operative urinary stone disease. This association persisted even after controlling for county level factors, such as median age, sex, and the prevalence of obesity and diabetes mellitus.
Our findings are strengthened by the fact that both metrics of temperature we explored (mean temperature and days over 90°) were significantly associated with operative stone burden with multivariate modeling. As these two different temperature related variables were both significantly associated with operative stone disease, our findings are less likely to be spurious. It is interesting to note, however, that neither mean temperature (although there was a strong trend toward univariate significance) nor number of days over 90° is significantly associated with operative stone burden univariately, but become highly significant when analyzed with precipitation in multivariate modeling. This is likely explained by the relatively small degree of variation in county mean temperature in California compared to precipitation. In other words, if two counties with similar temperatures had differing operative stone burden rates, the difference in precipitation between the two counties accounted for the differing rates.
There is increasing interest in explaining the geographic variation in urinary stone disease and how climate change may impact these effects. Based on the “stone belt” concept, Brikowski and colleagues estimated that increasing temperatures due to global warming will lead to 1.6 to 2.2 million new urinary stone disease cases by 2050.13 However, given our findings which suggest that precipitation is also associated with increased urinary stone disease, we believe that accounting for precipitation (and potentially other extrinsic factors) could lead to more accurate forecasts. In a broader sense, over the entire United States, including precipitation and temperature together better correlates with the higher prevalence of stone disease in the “stone belt,” where the southeast is known to have more precipitation than the southwest. The importance of our findings is further strengthened given that the Environmental Protection Agency (EPA) predicts that global warming will also increase global precipitation. In fact, in the contiguous 48 States, total annual precipitation has steadily increased 0.17 inches per decade since 1901. The EPA also notes that some areas have seen proportionally higher increase in precipitation relative to others, with the southwest experiencing a decrease.19,20
We postulate that the increased rate of stone burden in hot climates with higher precipitation could be related to the increased inefficiency of human body thermoregulation in wet heat vs dry heat, leading to greater insensible fluid losses.15 However, there are limited data examining the physiologic effects of precipitation on urinary stone disease or urine composition. One study measured changes in urinary composition at four centers at different locations in the United States and compared the findings to the mean 24-hour temperature and humidity.21 They found that higher temperature alone was correlated with increased urinary excretion of calcium and supersaturation of calcium oxalate and calcium phosphate. Another investigation in New York City correlated increased emergency department visits for urinary stone disease to hotter more humid weather conditions.22 Yet another explored the rates of emergency department visits for one Northern Italian hospital over a variety of environmental conditions.23 Their findings differed from others as humidity was negatively associated with urinary stone visits despite temperature being positively associated. This seemingly contradictory finding might be explained by the fact that Italy is considered to have a temperate and dry climate compared with other locations.14 More importantly, humidity may not be the most appropriate variable to consider by itself, as relative humidity is defined as the ratio of partial pressure of water vapor to the equilibrium vapor pressure of water. Due to this, less water vapor is required to attain a high relative humidity at lower temperatures. Based on our hypothesis that hotter and wetter climates potentiate stone risk, Heat Index would theoretically be a better correlate. The Heat Index was created in an attempt to quantify the increased health risk and perceived temperature humans experience in weather that is together hotter and more humid.24 Unfortunately, Heat Index was not universally available for us to study, but climates that are wetter and hotter generally have higher average heat indexes (hence the appropriateness of using precipitation). Future studies could explore the effects of Heat Index in local climates where this measure is available.
Despite its strengths, our study has several limitations. First, we cannot account completely for climate variation within a county (for example, a county could have multiple different microclimates). In addition, a patient's reported ZIP code may not describe where they actually live (e.g., PO Box) or where they spend most of their time (i.e., they work in a neighboring zip code). Along these lines, patients may also have differing degrees of exposure to the outside climate (working outside vs in an air-conditioned office). Our results are also limited by the fact that although we adjust for patient factors at the county level, we are unable to perform this at the patient level, and as a result, some risk factors may not accurately be accounted for in our study. Another potential limitation is that operative stone burden may be associated with variations in the treatment of stone disease in different locations. Finally, we acknowledge that not all ambulatory surgery centers necessarily report to California Department of Public Health (CDPH) and, thus, would not be reported in the OSHPD database. This is a result of a court case in 2007 where it was ruled that freestanding ambulatory surgery centers would no longer be licensed by CDPH.25 However, despite the fact that these centers are no longer covered by OSHPD, it is important to remember that this would result in few lithotripsy procedures being unreported. In fact, only 15 of the 754 freestanding centers in the state perform any sort of lithotripsy procedures at all,26 and their impact is unlikely to significantly alter our findings which are based on the 337 inpatient and outpatient centers. Furthermore, a study exploring ambulatory surgery trends in California from 2005 to 2010 did not observe a difference in reported procedure volume after 2007 (the highest ambulatory surgical volume reported was actually for 2010).27
Despite these limitations, our study has many strengths. California is the most populous state in the United States, encompassing 14% of the entire country's population. Coupled with the OSHPD's ability to capture all nonfederal outpatient or inpatient procedures, we are able to provide a population-based sample that includes all urinary stone disease that required intervention. We feel that operative stone burden is an excellent metric for overall clinically significant stone disease. Supporting this is the fact that the yearly reported incidence of urinary stone disease is 1 to 3 persons per 1000 persons per year28 (which is similar to our mean county prevalence over the 3-year period of ∼2/1000 persons). Moreover, California is a large state with multiple microclimates,14 making it an ideal region to explore the impact of climate variation on urinary stone disease. Another strength of this study is that we controlled for county-level patient intrinsic urinary stone risk factors, including diabetes prevalence, obesity prevalence, sex, and median age in our analysis. Finally, we were able to analyze our data at the level of the 58 counties which allows for granular insight into climate trends over a variety of regions.14 Although it could be argued that differences in county operative stone burden could be attributed to differences in access to care, California actually has a homogenous distribution of urologists throughout the state. In contrast to the rest of the United States, where rural areas have less urologists per person, most of the counties in California (even the more rural ones) had similar number of urologists per population.29 Furthermore, in our study some of the highest operative stone burden rates were found in more rural counties, further providing evidence that access to care issues likely did not impact our results.
Conclusions
California counties with higher annual mean precipitation and mean temperatures have higher rates of operative urinary stone disease. Together, precipitation and temperature explain over one third of the geographic variation in stone burden across California, highlighting the importance of these climate variables in models of stone risk. Future efforts to evaluate additional patient-level and environmental factors are warranted to better understand the geographic variation in urinary stone disease and to develop policies to provide additional stone prevention efforts and resources.
Abbreviations Used
- ASD
Ambulatory Surgery Database
- CDC
Centers for Disease Control and Prevention
- CDPH
California Department of Public Health
- EPA
Environmental Protection Agency
- ICD-9
International Classification of Diseases, Ninth Revision
- NOAA
National Oceanic and Atmospheric Administration
- OSHPD
Office of Statewide Health Planning and Development
- PCNL
percutaneous nephrolithotomy
- PDD
Patient Discharge Dataset
- SWL
extracorporeal shockwave lithotripsy
- UPJ
ureteropelvic junction
- URS
ureteroscopy
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Norlin A, Lindell B, Granberg PO, Lindvall N. Urolithiasis. A study of its frequency. Scand J Urol Nephrol 1976;10:150–153 [DOI] [PubMed] [Google Scholar]
- 2.Sierakowski R, Finlayson B, Landes RR, Finlayson CD, Sierakowski N. The frequency of urolithiasis in hospital discharge diagnoses in the United States. Invest Urol 1978;15:438–441 [PubMed] [Google Scholar]
- 3.Johnson CM, Wilson DM, O'Fallon WM, Malek RS, Kurland LT. Renal stone epidemiology: A 25-year study in Rochester, Minnesota. Kidney Int 1979;16:624–631 [DOI] [PubMed] [Google Scholar]
- 4.Pearle MS, Calhoun EA, Curhan GC. Urologic diseases in America project: Urolithiasis. J Urol 2005;173:848–857 [DOI] [PubMed] [Google Scholar]
- 5.Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int 2003;63:1817–1823 [DOI] [PubMed] [Google Scholar]
- 6.Taylor EN, Stampfer MJ, Curhan GC. Obesity, weight gain, and the risk of kidney stones. JAMA 2005;293:455–462 [DOI] [PubMed] [Google Scholar]
- 7.Taylor EN, Curhan GC. Body size and 24-hour urine composition. Am J Kidney Dis 2006;48:905–915 [DOI] [PubMed] [Google Scholar]
- 8.Maalouf NM, Cameron MA, Moe OW, Sakhaee K. Novel insights into the pathogenesis of uric acid nephrolithiasis. Curr Opin Nephrol Hypertens 2004;13:181–189 [DOI] [PubMed] [Google Scholar]
- 9.Maalouf NM, Sakhaee K, Parks JH, Coe FL, Adams-Huet B, Pak CYC. Association of urinary pH with body weight in nephrolithiasis. Kidney Int 2004;65:1422–1425 [DOI] [PubMed] [Google Scholar]
- 10.Nowicki M, Kokot F, Surdacki A. The influence of hyperinsulinaemia on calcium-phosphate metabolism in renal failure. Nephrol Dial Transplant 1998;13:2566–2571 [DOI] [PubMed] [Google Scholar]
- 11.Soucie JM, Thun MJ, Coates RJ, McClellan W, Austin H. Demographic and geographic variability of kidney stones in the United States. Kidney Int 1994;46:893–899 [DOI] [PubMed] [Google Scholar]
- 12.Mandel NS, Mandel GS. Urinary tract stone disease in the United States veteran population. I. Geographical frequency of occurrence. J Urol 1989;142:1513–1515 [DOI] [PubMed] [Google Scholar]
- 13.Brikowski TH, Lotan Y, Pearle MS. Climate-related increase in the prevalence of urolithiasis in the United States. Proc Natl Acad Sci U S A 2008;105:9841–9846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peel MC, Finlayson BL, McMahon TA. Updated world map of the Köppen-Geiger climate classification. Hydrol Earth Syst Sci 2007;11:1633–1644 [Google Scholar]
- 15.Burse RL. Sex differences in human thermoregulatory response to heat and cold stress. Hum Factors 1979;21:687–699 [DOI] [PubMed] [Google Scholar]
- 16.National Centers for Environmental Information (NCEI). Climate Data Online: Dataset Discovery. Datasets j Climate Data Online (CDO) j National Climatic Data Center (NCDC). Available at: www.ncdc.noaa.gov/cdo-web/ (accessed April29, 2017)
- 17.Gregson J. Poverty, sprawl, and restaurant types influence body mass index of residents in California counties. Public Health Rep 2011;126(Suppl):141–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Diabetes home. Centers for Disease Control and Prevention. May 2, 2016. Available at: www.cdc.gov/diabetes/data/county.html?states=%2Fdiabetes%2Fatlas%2Fobesityrisk%2F6%2Fatlas.html&go=Go (accessed April29, 2017)
- 19.Blunden J, Arndt DS, eds. State of the climate in 2015. B Am Meteorol Soc 2016;97:S1–SS275 [Google Scholar]
- 20.National Centers for Environmental Information (NCEI). April 17, 2017. Available at: www.ncei.noaa.gov (accessed April29, 2017)
- 21.Eisner BH, Sheth S, Herrick B, Pais VM, Sawyer M, Miller N, Hurd KJ, Humphreys MR. The effects of ambient temperature, humidity and season of year on urine composition in patients with nephrolithiasis. BJU International 2012;110(11 Pt C):E1014–E1017 [DOI] [PubMed] [Google Scholar]
- 22.Sirohi M, Katz BF, Moreira DM, Dinlenc C. Monthly variations in urolithiasis presentations and their association with meteorologic factors in New York City. J Endourol 2014;28:599–604 [DOI] [PubMed] [Google Scholar]
- 23.Cervellin G, Comelli I, Comelli D, Meschi T, Lippi G, Borghi L. Mean temperature and humidity variations, along with patient age, predict the number of visits for renal colic in a large urban Emergency Department: Results of a 9-year survey. J Epidemiol Glob Health 2012;2:31–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.NWS heat safety home page, and US Department of Commerce, NOAA, National Weather Service. January 1, 2001. Accessed April29, 2017
- 25.Klütz BG. Outpatient surgery services in California: Oversight, transparency, and quality. B and R Klütz Con- sulting. California Health Foundation. 2015. Available at: www.chcf.org/∼/media/MEDIA%20LIBRARY%20Files/PDF/PDF%20O/PDF%20OutpatientSurgeryOversightQuality.pdf (accessed April1, 2017)
- 26.Ambulatory Surgery Centers: Big business, little data. Accessed June19, 2017 Available at: www.chcf.org/publications/2013/06/ambulatory-surgery-centers
- 27.Raheem OA, Mirheydar HS, Miller DL, Palazzi KL, Chang DC, Sur RL. Contemporary trends in the ambulatory surgical treatment of urolithiasis: Population-based analysis. J Endourol 2015;29:1189–1192 [DOI] [PubMed] [Google Scholar]
- 28.Curhan GC. Epidemiology of stone disease. Urol Clin North Am 2007;34:287–293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Odisho AY, Fradet V, Cooperberg MR, Ahmad AE, Carroll PR. Geographic distribution of urologists throughout the United States using a county level approach. J Urol 2009;181:760–765 [DOI] [PubMed] [Google Scholar]