Abstract
Listeria monocytogenes (L. monocytogenes) causes the third highest number of foodborne illness deaths annually. L. monocytogenes contamination of sliced deli meats at the retail level is a significant contributing factor to L. monocytogenes illness. The Centers for Disease Control and Prevention's Environmental Health Specialists Network (EHS-Net) conducted a study to learn more about retail delis' practices concerning L. monocytogenes growth and cross-contamination prevention. This article presents data from this study on the frequency with which retail deli refrigerator temperatures exceed 41°F, the Food and Drug Administration (FDA)-recommended maximum temperature for ready-to-eat food requiring time and temperature control for safety (TCS) (such as retail deli meat). This provision was designed to control bacterial growth in TCS foods. This article also presents data on deli and staff characteristics related to the frequency with which retail delis refrigerator temperatures exceed 41°F. Data from observations of 445 refrigerators in 245 delis showed that in 17.1% of delis, at least one refrigerator was >41°F. We also found that refrigeration temperatures reported in this study were lower than those reported in a related 2007 study. Delis with more than one refrigerator, that lacked refrigerator temperature recording, and had a manager who had never been food safety certified had greater odds of having a refrigerator temperature >41°F. The data from this study suggest that retail temperature control is improving over time. They also identify a food safety gap: some delis have refrigerator temperatures that exceed 41°F. We also found that two food safety interventions were related to better refrigerated storage practices: kitchen manager certification and recording refrigerated storage temperatures. Regulatory food safety programs and the retail industry may wish to consider encouraging or requiring kitchen manager certification and recording refrigerated storage temperatures.
Keywords: : retail delis; food safety; FDA Food Code; Listeria monocytogenes,; refrigerated storage; temperatures; risk assessment
Introduction
Listeria monocytogenes (L. monocytogenes) is a persistent public health concern in the United States; it causes the third highest number of deaths annually among the major foodborne pathogens (Scallan et al., 2011). Ready-to-eat (RTE) foods are the major source of human listeriosis cases (Hitchins and Whiting, 2001; Yang et al., 2006). Of 23 RTE foods linked to L. monocytogenes, deli meats pose the greatest risk of listeriosis per year and per serving (Food and Drug Administration [FDA]/Food Safety and Inspection Service [FSIS]/Centers for Disease Control and Prevention [CDC], 2003). Also, an FSIS risk assessment indicates that 83% of listeriosis cases attributed to deli meat are associated with meat sliced and packaged at retail locations (Endrikat et al., 2010).
These findings indicate that L. monocytogenes contamination of sliced deli meats at the retail level is a significant contributing factor to L. monocytogenes illness. Thus, prevention of L. monocytogenes cross-contamination and growth in retail delis (i.e., delis) is critical to reducing L. monocytogenes illnesses (Pouillot et al., 2015; Gallagher et al., 2016). Yet few studies have been conducted on deli L. monocytogenes cross-contamination and growth prevention practices; information on these practices is critical to developing effective interventions (Lubran et al., 2010; Maitland et al., 2013). To address this need, the CDC's Environmental Health Specialists Network (EHS-Net) examined deli food safety policies and practices.
The purposes of this study were to identify gaps in deli policies and practices relevant to preventing L. monocytogenes cross-contamination and growth and to identify deli and staff characteristics related to these policies and practices. This article focuses on data collected in this study on delis' refrigerated storage practices. The FDA Food Code provides the basis for state and local codes that regulate retail food service in the United States. It contains a provision recommending that RTE food requiring time and temperature control for safety (TCS) (such as deli meat) be maintained at 41°F or less (FDA, 2013b [3-501.16]). FSIS also recommends keeping deli meat at 41°F or below (FSIS, 2015).
These provisions are based on findings indicating L. monocytogenes can grow in deli meat at very low refrigeration temperatures (Duh and Schaffner, 1993; Wijtzes et al., 1993; Alavi et al., 1999; FDA-FSIS-CDC, 2003; Chan and Wiedmann, 2009) and that maintaining such foods at 41°F or below is important in reducing the risk of L. monocytogenes illnesses (U.S. FDA Food Code 2013, Annex 3, 2013; Gallagher et al. 2016). This article presents data on the frequency with which delis' refrigerator temperatures exceed 41°F, and on deli and staff characteristics related to this frequency.
This article also compares data from this study and a previous study (EcoSure, 2008) to assess changes in temperatures over time. Finally, this article evaluates the public health impact of these changes on L. monocytogenes contamination of RTE foods prepared at retail locations.
Materials and Methods
EHS-Net, a collaborative program of CDC, FDA, FSIS, and health departments, designed and conducted this study. A CDC cooperative agreement funded six health departments in California, Minnesota, New York State, New York City, Rhode Island, and Tennessee (hereafter referred to as jurisdictions) to participate in EHS-Net and in this study. The FSIS also provided funding for this study through an interagency agreement. Four of the six jurisdictions had adopted the FDA Food Code provision requiring TCS food to be stored at 41°F or less. The remaining jurisdictions required storing TCS food at 45°F or less.
Sample
The study sample consisted of randomly selected delis located in the six EHS-Net jurisdictions. EHS-Net personnel in each jurisdiction chose a geographical area in which to recruit delis for study participation. Within each of these areas, EHS-Net personnel (i.e., data collectors) collected data in ∼50 delis. We defined a deli as an establishment that slices meat or cheese and prepares or serves RTE foods, and where, typically, food is taken elsewhere to be eaten. Both free-standing delis and delis in grocery stores were eligible for participation.We included in the study only delis wherein managers and food workers spoke English well enough to be interviewed in English.
Data collection and analysis
Data collection took place from January to September, 2012. Data collectors requested study participation and arranged for data collection visits through telephone calls. At the deli, data collectors interviewed a manager (someone who had authority over the deli) about his or her characteristics, and the deli's characteristics and policies and practices relevant to L. monocytogenes prevention (Table 1). Managers also completed an eight-item, written, multiple-choice food safety knowledge assessment. Data collectors also interviewed a food worker (someone who prepared food in the deli) about his or her characteristics (Table 1). The interview also assessed worker food safety knowledge through five Yes/No items. To increase manager participation and cooperation, data collectors asked managers to choose the worker to be interviewed.
Table 1.
Deli, Manager, and Worker Characteristics
| n | % | |
|---|---|---|
| Deli characteristics | ||
| Ownership type (N = 245) | ||
| Chain | 158 | 64.5 |
| Independent | 87 | 35.5 |
| Number of customers (N = 210) | ||
| ≤99 | 53 | 25.2 |
| 100–299 | 77 | 36.7 |
| ≥300 | 80 | 38.1 |
| Number of managers (N = 245) | ||
| 1 | 82 | 33.5 |
| ≥2 | 163 | 66.5 |
| Number of shifts in a typical day (N = 245) | ||
| 1 or 2 | 100 | 40.8 |
| ≥3 | 145 | 59.2 |
| Number of hours in a typical shift (N = 245) | ||
| ≤7 | 85 | 34.7 |
| ≥8 | 160 | 65.3 |
| Average number of workers per shift (N = 244) | ||
| ≤2 | 91 | 37.3 |
| >2 | 153 | 62.7 |
| Manager food safety training required by deli (N = 242) | ||
| No | 42 | 17.4 |
| Yes | 200 | 82.6 |
| Manager food safety certification required by deli (N = 239)a | ||
| No | 108 | 45.2 |
| Yes | 131 | 54.8 |
| Number of refrigerators (N = 245)b | ||
| 1 | 134 | 54.7 |
| ≥2 | 111 | 45.3 |
| Ever record the temperature of the refrigerators (N = 244) | ||
| No | 85 | 34.8 |
| Yes | 159 | 65.2 |
| Average number of chubs (plastic tubes of meat) sold per week (N = 245) | ||
| <50 | 145 | 59.2 |
| ≥50 | 100 | 40.8 |
| Policy on maximum number of days deli can hold an opened chub (N = 245) | ||
| ≤4 days | 57 | 23.3 |
| 4–7 days | 171 | 69.8 |
| >7 days | 17 | 6.9 |
| Manager characteristics | ||
| Experience in retail food industry (N = 245) | ||
| <10 years | 42 | 17.1 |
| 10 to 20 years | 94 | 38.4 |
| >20 years | 109 | 44.5 |
| Experience as manager in current deli (N = 245) | ||
| ≤5 years | 130 | 53.1 |
| >5 years | 115 | 46.9 |
| Ever food safety certified (N = 245)a | ||
| No | 63 | 25.7 |
| Yes | 182 | 74.3 |
| Currently food safety certified (N = 245)a | ||
| No | 96 | 39.2 |
| Yes | 149 | 60.8 |
| Food safety knowledge (N = 245) | ||
| Answered ≤75% correctly | 56 | 22.9 |
| Answered >75% correctly | 189 | 77.1 |
| Worker characteristics | ||
| Experience in retail food industry (N = 240) | ||
| <10 years | 114 | 47.5 |
| ≥10 years | 126 | 52.5 |
| Experience in current deli (N = 241) | ||
| ≤5 years | 155 | 64.3 |
| >5 years | 86 | 35.7 |
| Food safety knowledge (N = 241) | ||
| Answered <100% correctly | 120 | 49.8 |
| Answered 100% correctly | 121 | 50.2 |
Certification defined as having taken and passed a food safety test and been issued a certificate.
These data were collected through observation; all other characteristics data were collected through manager and worker interviews and a manager survey.
Finally, data collectors observed food preparation and storage practices in the deli kitchen area. This observation included measuring the ambient air temperature of up to five refrigerators (walk-ins and reach-ins) in which deli products were stored. Data collectors took ambient air temperatures by placing their own calibrated thermocouple thermometers in the center of the refrigerators. The study protocol and data collection instruments can be found on the CDC website (CDC, 2017).
Each EHS-Net jurisdiction's institutional review board cleared the study protocol. We did not collect data that could identify individual delis, managers, or workers.
We calculated descriptive statistics on deli and staff characteristics and refrigerator temperatures. We also conducted simple logistic regression models, stratifying by jurisdiction, to examine associations between explanatory variables (deli and staff characteristics) and the outcome variable of whether any deli refrigerator temperatures exceeded 41°F. We used SAS version 9.3 (SAS Institute, Inc., Cary, NC) to analyze the data.
Comparison of temperatures across studies
To assess temperature changes over time, we compared temperatures of deli refrigerators from this study with temperatures of deli meat products stored in deli refrigerators from a study conducted by Ecosure in 2007 (Ecosure, 2008). In the Ecosure study, trained shoppers made one sliced deli meat purchase in randomly selected grocery stores and took the temperature of the deli meat product immediately after purchase with a calibrated thermometer supplied by Ecosure. The study collected meat samples in 47 states with a median of 12 samples per state (range 1–110) for a total of 891 measurements. The Ecosure study found that 58% of deli meat product temperatures were >41°F. Given the dynamics of these temperature measurements, we have treated the air temperatures as if they were food temperatures for risk assessment (Evans and Woolfe, 2008; Zubeldia et al. 2016; Mercier et al., 2017). The deli meat temperature findings in the Ecosure study (2008) are consistent, as a surrogate, with concurrent FDA deli refrigerator temperature findings (FDA 2009, 2010), providing close agreement between deli refrigerator and corresponding deli meat temperature. This close agreement allowed us to use deli refrigerator temperatures from this study as a proxy for deli meat temperatures to evaluate the impact of changes in public health risk due to changes in retail practices.
Evaluation of public health impact of refrigerator temperature changes
We examined the public health impact of changes in refrigerator temperatures using an existing interagency retail L. monocytogenes risk assessment [described by Pouillot et al. (2015)] used to evaluate the public health impact of retail practices, including temperature control (Gallagher et al., 2016). This risk assessment is based on a discrete event risk assessment model of deli operations that includes temperature-dependent bacterial growth and cross-contamination while serving customers.
The model is written in R version 3.4 (R Development Core Team, 2017). Model results are based on Monte Carlo simulations of 100 retail stores with 1 million servings per store. Monte Carlo modeling uses probability distributions to describe each of the input variables—refrigerator temperatures. For each model run, random draws are made for each input variable from these probability distributions to generate specific input values. The model then uses these values to estimate the risk of illness per serving. By evaluating the results from numerous runs, the variability and uncertainty of the risk of illness per serving can be quantitatively determined. We ran the risk assessment model using the previous temperature distribution from Ecosure (2008) and again with the temperature distribution from this study.
Results
Deli and staff characteristics
Of the 691 managers of eligible delis contacted by data collectors, 43.1% (298) agreed to participate in the study. In all delis, data collectors interviewed the managers and gave them the food safety knowledge assessment. In 98.7% (294) of delis, data collectors also interviewed a food worker. In 82.2% (245) of delis, data collectors measured refrigerator temperatures; the data presented hereunder are from these delis.
According to manager data, 64.5% of delis were chains (A chain establishment shares its name and operations with other establishments. Chain ownership may be private, franchise, or corporate.); 38.1% served 300 or more customers on their busiest days; 65.2% recorded refrigerator temperatures; and 69.8% had a policy stating that opened chubs (plastic tubes of meat common in delis) could be held in refrigeration for 4–7 days (Table 1). Manager data also indicated that 44.5% of managers had >20 years of experience in the retail food industry, and 77.1% answered at least six of eight (≥75%) food safety knowledge questions correctly. According to worker data, 52.5% of workers had more than 10 years of experience in the retail food industry, and 50.2% answered all five (100%) food safety knowledge questions correctly. See Table 1 for additional descriptive data on deli and staff characteristics.
Refrigerator temperatures
Data collectors measured temperatures in 445 refrigerators in 245 delis. Half of delis (54.7%, 134) had only one refrigerator; 23.7% (58) had two; 11.4% (28) had three; 5.7% (14) had four; and 4.5% (11) had at least five. Most (89.2%) refrigerators measured at 41°F or below (Table 2). Of the 11% (48) of refrigerators that were >41°F, almost half (47.9%, 23) were only one degree >41°F (i.e., 42°F).
Table 2.
Number and Percentage of Deli Refrigerator Temperatures (N = 445 Refrigerators)
| Refrigerator temperature | n | % |
|---|---|---|
| ≤ 41°F | 397 | 89.2 |
| 42°F | 23 | 5.2 |
| 43°F | 8 | 1.8 |
| 44°F | 6 | 1.3 |
| 45°F | 6 | 1.3 |
| 46–52°F | 5 | 1.1 |
In 82.9% of delis, no refrigerators were >41°F. In 17.1% of delis, at least one refrigerator was >41°F. In 4.1% of delis, between one forth and one third of refrigerators were >41°F. In 5.3% of delis, between one half and two-thirds of refrigerators were >41°F, and in 7.7% of delis, all refrigerators were >41°F (Table 3).
Table 3.
Number and Percentage of Deli Refrigerators >41°F (N = 245 Delis)
| Number of refrigerators in deli >41°F | n | % |
|---|---|---|
| 0 | 203 | 82.9 |
| 1 | 37 | 15.1 |
| 2 | 4 | 1.6 |
| 3 | 1 | 0.4 |
| Percentage of refrigerators in deli >41°F | n | % |
|---|---|---|
| 0 | 203 | 82.9 |
| 20.0–33.3 | 10 | 4.1 |
| 50.0–66.7 | 13 | 5.3 |
| 100 | 19 | 7.7 |
The percentage of delis with a refrigerator temperature >41°F did not significantly differ by jurisdiction (χ2 = 2.975, df = 5, p = 0.70).
Deli and staff characteristics associated with refrigerator temperatures
Simple logistic regression analyses identified 3 (of 19) characteristics significantly associated (p ≤ 0.05) with at least one deli refrigerator measuring >41°F. Compared with delis with only one refrigerator, delis with more than one refrigerator had greater odds of a refrigerator measuring >41°F. Compared with delis in which staff recorded refrigerator temperatures, delis in which staff did not record refrigerator temperatures had greater odds of a refrigerator measuring >41°F. Finally, delis whose manager had never been food safety certified, compared with those whose managers had been certified, had greater odds of having a refrigerator >41°F (Table 4).
Table 4.
Simple Logistic Regression Analyses on Deli, Manager, and Worker Characteristics Associated with at least one Deli Refrigerator Measuring Above 41°F
| n | OR(95% CI) | p value | |
| Deli characteristics | |||
| Ownership type (N = 245) | |||
| Chain | 25 | – | – |
| Independent | 17 | 1.44 (0.66, 3.14) | 0.355 |
| Number of customers (N = 210) | 0.713 | ||
| ≤99 | 11 | 1.43 (0.57, 3.57) | 0.442 |
| 100 to 299 | 12 | 1.03 (0.44, 2.43) | 0.947 |
| ≥300 | 13 | – | – |
| Number of managers (N = 245) | |||
| 1 | 12 | – | – |
| ≥2 | 30 | 1.24 (0.58, 2.63) | 0.581 |
| Number of shifts in a typical day (N = 245) | |||
| 1 or 2 | 18 | 1.36 (0.64, 2.89) | 0.420 |
| ≥ 3 | 24 | – | – |
| Number of hours in a typical shift (N = 245) Number of hours in a shift |
|||
| ≤ 7 | 13 | – | – |
| ≥ 8 | 29 | 1.37 (0.66, 2.85) | 0.406 |
| Average number of workers per shift (N = 244) | |||
| ≤ 2 | 13 | – | – |
| > 2 | 29 | 1.25 (0.58, 2.68) | 0.569 |
| Manager food safety training is required by deli (N = 242) | |||
| No | 9 | 1.95 (0.75, 5.04) | 0.170 |
| Yes | 33 | – | – |
| Manager food safety certification is required by delia (N = 239) | |||
| No | 21 | 1.44 (0.70, 2.93) | 0.321 |
| Yes | 19 | – | – |
| Number of refrigerators (N = 245)b | |||
| 1 | 16 | – | – |
| ≥ 2 | 26 | 2.33 (1.10, 4.94) | 0.027c |
| Ever record the temperature of the refrigerator(s) (N = 244) | |||
| No | 20 | 2.25 (1.08, 4.71) | 0.031c |
| Yes | 22 | – | – |
| Average number of chubs (plastic tubes of meat) sold per week (N = 241) | |||
| < 50 | 23 | 1.59 (0.76, 3.29) | 0.217 |
| ≥ 50 | 19 | – | – |
| Policy on maximum number of days deli can hold an opened chub (N = 241) | |||
| ≤4 days | 1.01 (0.24, 4.28) | 0.993 | |
| 4–7 days | 1.02 (0.26, 4.01) | 0.997 | |
| >7 days | – | – | |
| Manager characteristics | |||
| Manager experience in retail food industry (N = 241) | 0.489 | ||
| < 10 years | 5 | – | – |
| 10 to 20 years | 16 | 1.69 (0.57, 4.97) | 0.344 |
| > 20 years | 21 | 1.90 (0.66, 5.47) | 0.232 |
| Experience as manager in current deli (N = 245) | |||
| ≤ 5 years | 21 | – | – |
| > 5 years | 21 | 1.16 (0.59, 2.27) | 0.671 |
| Ever food safety certified (N = 245)a | |||
| No | 15 | 2.39 (1.08, 5.29) | 0.032c |
| Yes | 27 | – | – |
| Currently food safety certified (N = 245)a Currently food safety certified |
|||
| No | 19 | 1.52 (0.76, 3.06) | 0.241 |
| Yes | 23 | – | – |
| Food safety knowledge (N = 245) | |||
| Answered ≤75% correctly | 10 | 1.24 (0.54, 2.84) | 0.616 |
| Answered >75% correctly | 32 | – | – |
| Worker characteristics | |||
| Experience in retail food industry (N = 240) | |||
| < 10 years | 21 | 1.43 (0.58, 2.24) | 0.697 |
| ≥ 10 years | 21 | – | – |
| Experience in current deli (N = 241) | |||
| ≤ 5 years | 26 | – | – |
| > 5years | 16 | 1.14 (0.57, 2.28) | 0.703 |
| Food safety knowledge (N = 241) | |||
| Answered <100% correctly | 25 | 1.66 (0.82, 3.34) | 0.160 |
| Answered 100% correctly | 17 | – | – |
Ns vary because of missing data.
Certification defined as having taken and passed a food safety test and been issued a certificate.
These data were collected through observation; all other characteristics data were collected through manager and worker interviews and a manager survey.
P value is significant (p ≤ 0.05).
OR, odds ratio; CI, confidence interval.
Comparison with previous temperature data
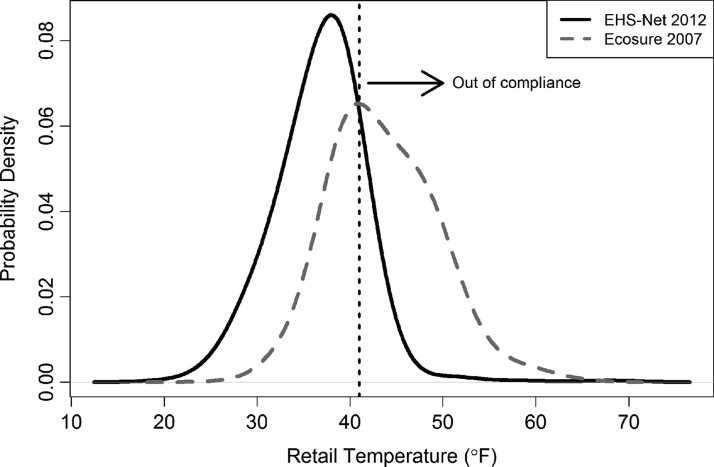
Comparison of temperatures between the Ecosure study and the current study found a mean temperature difference of 6.8°F (43.6°F; 36.8°F, respectively). A nonparametric Wilcoxon test indicates this difference is significant (p < 10–15). The temperatures from this study were also less dispersed than the Ecosure temperatures (SD = 4.9°F vs. 5.7°F, respectively). This decrease in variance is statistically significant based on a Fligner-Killeen test (p < 10–9). The temperature distributions are shown in Figure 1. The area to the right of 41°F (shown as a vertical line) indicates the proportion of deli with refrigerators >41°F. The total probability of temperatures >41°F is depicted as the area under the probability distribution curves and to the right of the 41°F line. The percentage of temperatures >41°F was 58.1% for the Ecosure study and 10.8% for this study. Overall, the temperatures reported in this study were significantly lower than those reported in the Ecosure study, as depicted by the left shift in the probability density curve (Fig. 1).
FIG. 1.
Temperature distribution comparison between Ecosure (2008) and this study. All individual retail temperature measurements used. EHS-Net, Environmental Health Specialists Network.
Evaluation of impact of refrigerator temperature changes
Pouillot et al. (2015) and Gallagher et al. (2016) describe a federal interagency quantitative retail risk assessment model for L. monocytogenes that evaluates the public health impact of retail practices. The model incorporates temperature-dependent bacterial growth during refrigerated storage. Using the Ecosure study temperature data, the risk assessment model estimated a per serving listeriosis risk to the susceptible population (generally older adults, fetuses, newborns, and immunocompromised people) of 1.4 × 10–7 for RTE food prepared in delis. Using this study's temperature data in this risk assessment model led to a statistically significant risk reduction of 13%, that is, 1.2 × 10–7risk per serving. In other words, we found that the risk of listeriosis from eating deli meats has dropped an estimated 13% per serving based on this more recent temperature data. For comparison, Gallagher et al. (2016) found that a 16% reduction in the risk per serving would occur if all products were stored at or <41°F; that is, if all retail deli refrigerator temperatures were at or <41°F. The difference between the current estimated 13% and the ideal 16% risk per serving reductions is due to the observed 10.8% still >41°F.
Discussion
Data from this study indicate that in about one in six delis, at least one refrigerator was >41°F. Refrigerators >41°F cannot maintain the food within at 41°F or below, as recommended by FDA. Although this figure represents a relatively small proportion of delis, and the majority of refrigerators were only 1° >41°F, several studies have shown that L. monocytogenes can grow at very low temperatures (averaging 29°F) (Duh and Schaffner, 1993; Wijtze et al., 1993; USDA-ARS, 1997; Alavi et al., 1999; FDA/FSIS/CDC, 2003; Chan and Wiedmann, 2009). The interagency federal risk assessment also found that strict temperature control during refrigerated storage in delis reduces the risk of listeriosis (Gallagher et al., 2016). These findings highlight the importance of keeping refrigerators at low temperatures, and indicate that delis need to continue to focus on improving their refrigerated storage practices.
Although the data from this study indicate that some delis are not adequately controlling refrigerator temperatures, they also suggest that deli temperature control is improving over time. The percentage of in-compliance temperatures was significantly higher in this study than in the older Ecosure study. Given that research has shown that refrigerator temperature control can significantly impact foodborne illness prevention (Gallagher et al., 2016), this finding is encouraging. And indeed, risk assessment models show that these temperature reductions lead to a reduction in the risk of listeriosis.
Our finding that delis in which staff did not record refrigerator temperatures were more likely to have refrigerator temperatures >41°F suggests that recording plays a role in ensuring proper refrigeration temperature. Temperature recording, along with its prerequisite monitoring, can alert management to inadequate temperatures that would likely go unnoticed, and therefore unaddressed, without monitoring and recording. FDA guidance recommends that to achieve active managerial control of foodborne illness risk factors, retail establishments should implement food safety management systems. Monitoring and recording temperatures at critical control points, such as refrigerated storage, can be an important part of such a system (U.S. FDA Food Code 2013, Annex 4, 2013).
The finding that delis in our study without a certified manager were more likely to have refrigerator temperatures >41°F supports a growing body of research showing that manager certification is important to retail establishment food safety (Hedberg et al., 2006; Cates et al., 2009; Bogard et al., 2013; Brown et al., 2014; Brown et al., 2016; FDA, 2014). Indeed, FDA guidance states that a certified manager can be an important factor in an effective food safety management system, and the 2013 FDA Food Code contains a provision stating that all retail establishments should have a certified manager on staff (FDA, 2013b [2-102.12]; U.S. FDA Food Code 2013, Annex 4, 2013).
The finding that delis with multiple refrigerators were more likely to have refrigerator temperatures >41°F suggests that effectively maintaining adequate temperatures for multiple refrigerators may be challenging. Delis with multiple refrigerators may be busier than those with only one refrigerator, resulting in opening and closing refrigerators more frequently, making adequate temperatures maintenance more difficult. More research is needed to explore the relationship between number of deli refrigerators and refrigeration temperatures.
This study has several limitations. First, because we collected data in only delis with some English-speaking staff, our data may not represent delis with no English-speaking staff. Second, because interviewed workers were chosen by managers and not randomly, worker data may not represent the full range of workers. Third, the study's relatively low response rate may have resulted in an overrepresentation of delis with better food safety practices. Fourth, the study collected cross-sectional data, which do not allow causal inferences about relationships between explanatory and outcome variables.
Finally, there were some limitations associated with differences in the data collection methods of the two studies from which temperature data were compared may limit interpretation of the comparison. Temperatures from this study were for refrigerators, whereas the Ecosure study temperatures were for food found in refrigerated storage. Also, data collection for this study was scheduled in advance with management, whereas data collection for the Ecosure study was not scheduled and management was not aware of the data collection.
Conclusions
The findings presented here are valuable because they suggest that retail temperature control is improving over time, and may lead to a reduction in the risk of listeriosis. They also identify a food safety gap: some delis have refrigerator temperatures that exceed 41°F, the FDA-recommended maximum temperature for TCS food, a temperature designed to control bacterial growth. In addition, we found that two FDA food safety interventions, kitchen manager certification and refrigerated storage temperature recording, were related to better refrigerated storage practices. Regulatory food safety programs and the retail industry should consider encouraging or requiring kitchen manager certification, as well as recording refrigerated storage temperatures. They may also wish to focus interventions on delis with multiple refrigerators, given that these delis were more likely have to refrigerator temperatures >41°F.
Acknowledgments
This publication is based on data collected and provided by the Centers for Disease Control and Prevention's (CDC) Environmental Health Specialists Network (EHS-Net), which is supported by a CDC grant award (CDC-RFA-EH05-013). We thank the deli managers and workers who agreed to participate in this study and the EHS-Net staff who assisted with study design and data collection. We also thank the U.S. Department of Agriculture's Food Safety and Inspection Service (FSIS) for its financial support of this study through interagency agreement #FSIS-IA-10-091, Kristin Holt (FSIS) for her assistance and support, and Brenda Le (CDC), Denita Williams (FDA), and Carol Selman (NEHA) for their work on study development and implementation. We also thank Laurie Williams and her colleagues (FDA) for helpful comments on drafts of this article. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of CDC or the Agency for Toxic Substances and Disease Registry.
Disclosure Statement
No competing financial interests exist.
References
- Alavi SH, Puri VM, Knabel RH, Mohtar RH, Whiting RC. Development and validation of a dynamic growth model for Listeria monocytogenes in fluid whole milk. J Food Protect 1999;62:170–176 [DOI] [PubMed] [Google Scholar]
- Bogard A, Fuller C, Radke V, Selman C, Smith K. Ground beef handling and cooking practices in restaurants in eight states. J Food Protect 2013;76:2132–2140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown L, Hoover E, Ripley D, Matis B, Nicholas D, Hedeen N, Faw B. Retail deli slicer cleaning frequency—Six selected sites, United States, 2012. Morb Mortal Wkly Rep 2016;65:306–310 [DOI] [PubMed] [Google Scholar]
- Brown L, Le B, Wong M, Reimann D, Nicholas D, Faw B, Davis E, Selman C. Restaurant manager and worker food safety certification and knowledge. Foodborne Pathog Dis 2014;11:1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cates S, Muth M, Karns S, Penne M, Stone C, Harrison J, Radke V. Certified kitchen managers: Do they improve restaurant inspection outcomes? J Food Protect 2009;72:384–391 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2017. EHS-Net Retail Deli Study Protocol. Available at: www.cdc.gov/nceh/ehs/ehsnet/study_tools/ehs-net-retail-deli-study.pdf accessed May15, 2017
- Chan YC, Wiedmann M. Physiology and genetics of Listeria monocytogenes survival and growth at cold temperatures. Crit Rev Food Sci Nutr 2009;49:237–253 [DOI] [PubMed] [Google Scholar]
- Duh YH, Schaffner DW. Modeling the effect of temperature on the growth rate and lag time of Listeria innocua and Listeria monocytogenes. J Food Protect 1993;56:205–210 [DOI] [PubMed] [Google Scholar]
- EcoSure. 2007 U.S. cold temperature evaluation: Design and summary pages. 2008. Available at: http://foodrisk.org/exclusives/EcoSure accessed May15, 2017
- Endrikat S, Gallagher D, Pouillot R, Hicks-Quesenberry H, LaBarre D, Schroder C, Kause J. A comparative risk assessment for Listeria monocytogenes in prepackaged versus retail sliced deli meat. J Food Protect 2010;73:612–619 [DOI] [PubMed] [Google Scholar]
- Evans JA, Woolfe ML. Temperature monitoring and measurement. In: Brown M. (ed.). Chilled Foods: A Comprehensive Guide, 3rd ed. Cambridge, UK: Woodhead Publishing, 2008 [Google Scholar]
- Gallagher D, Pouillot R, Hoelzer K, Tang J, Dennis SB, Kause JR. Listeria monocytogenes in retail delicatessens: An interagency risk Assessment-risk mitigations. J Food Protect 2016;79:1076–1088 [DOI] [PubMed] [Google Scholar]
- Hedberg C, Smith J, Kirkland E, Radke V, Jones T, Selman C; the EHS-Net Working Group. Systematic environmental evaluations to identify food safety differences between outbreak and nonoutbreak restaurants. J Food Protect 2006;69:2697–2702 [DOI] [PubMed] [Google Scholar]
- Hitchins A, Whiting R. Food-borne Listeria monocytogenes risk assessment. Food Addit Contam 2001;18:1108–1117 [DOI] [PubMed] [Google Scholar]
- Lubran MB, Pouillot R, Bohm S, Calvey EM, Meng J, Dennis S. Observational study of food safety practices in retail deli departments. J Food Protect 2010;73:1849–1857 [DOI] [PubMed] [Google Scholar]
- Maitland J, Boyer R, Gallagher D, Duncan S, Bauer N, Kause J, Eifert J. Tracking cross-contamination transfer dynamics at a mock retail deli market using GloGermTM. J Food Protect 2013;76:272–282 [DOI] [PubMed] [Google Scholar]
- Mercier S, Villeneuve S, Mondor M, Ismail Uysal I. Time–temperature management along the food cold chain: A review of recent developments. Compr Rev Food Sci Food Saf 2017;16:647–667 [DOI] [PubMed] [Google Scholar]
- Pouillot R, Gallagher D, Tang J, Hoelzer K, Kause J, Dennis S. Listeria monocytogenes in retail delicatessens: An interagency risk assessment-model and baseline results. J Food Protect 2015;78:134–145 [DOI] [PubMed] [Google Scholar]
- R Development Core Team. 2017. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. Available at: www.R-project.org accessed May15, 2017
- Scallan E, Hoekstra R, Angulo F, Tauxe R, Widdowson M-A, Roy S, Jones J, Griffin P. Foodborne illness acquired in the United States—Major pathogens. Emerg Infect Dis 2011;17:7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Agriculture, Food Safety and Inspection Service. 2015. Best Practices Guidance for Controlling Listeria monocytogenes in Retail Delicatessens. Available at: www.fsis.usda.gov/wps/wcm/connect/29d51258-0651-469b-99b8-e986baee8a54/Controlling-LM-Delicatessens.pdf?MOD=AJPERES accessed May15, 2017
- [U.S. FDA] U.S. Food and Drug Administration Food Code 2013, Annex 3. Public Health Reasons/Administrative Guidelines. 2013. Available at: www.fda.gov/downloads/Food/GuidanceRegulation/RetailFoodProtection/FoodCode/UCM374510.pdf accessed May15, 2017
- [U.S. FDA] U.S. Food and Drug Administration; Food Safety and Inspection Service; and Centers for Disease Control and Prevention. 2003. Quantitative assessment of the relative risk to public health from foodborne Listeria monocytogenes among selected categories of ready-to-eat foods. Available at: www.fda.gov/food/foodscienceresearch/risksafetyassessment/ucm183966.htm accessed May15, 2017
- [U.S. FDA] U.S. Food and Drug Administration. FDA report on the occurrence of foodborne illness risk factors in selected institutional foodservice, restaurant, and retail food store facility types. 2009. Available at: https://wayback.archive-it.org/7993/20170406023004/ https://www.fda.gov/Food/GuidanceRegulation/RetailFoodProtection/FoodborneIllnessRiskFactorReduction/ucm224321.htm accessed May15, 2017
- [U.S. FDA] U.S. Food and Drug Administration. FDA trend analysis report on the occurrence of foodborne illness risk factors in selected institutional foodservice, restaurant, and retail food store facility types (1998–2008), 2010. Available at: https://wayback.archive-it.org/7993/20170406022950; www.fda.gov/Food/GuidanceRegulation/RetailFoodProtection/FoodborneIllnessRiskFactorReduction/ucm223293.htm accessed May15, 2017
- [U.S. FDA] U.S. Food and Drug Administration. FDA retail risk factor study: background information. 2014. Available at: www.fda.gov/Food/GuidanceRegulation/RetailFoodProtection/FoodborneIllnessRiskFactorReduction/ucm230315.htm accessed May15, 2017
- [U.S. FDA] U.S. Food and Drug Administration Food Code 2013, Chapter 2. Management and personnel. 2013a. Available at: www.fda.gov/downloads/Food/GuidanceRegulation/RetailFoodProtection/FoodCode/UCM374510.pdf accessed May15, 2017
- [U.S. FDA] U.S. Food and Drug Administration Food Code 2013, Chapter 3. Food. 2013b. Available at: www.fda.gov/downloads/Food/GuidanceRegulation/RetailFoodProtection/FoodCode/UCM374510.pdf accessed May15, 2017
- [U.S. FDA] U.S. Food and Drug Administration Food Code 2013, Annex 4. Management of food safety practices–achieving active managerial control of foodborne illness risk factors. 2013. Available at: www.fda.gov/downloads/Food/GuidanceRegulation/RetailFoodProtection/FoodCode/UCM374510.pdf accessed May15, 2017
- Wijtzes TP, McClure J, Zwietering MH, Roberts TA. Modelling bacterial growth of Listeria monocytogenes as a function of water activity, pH and temperature. Int J Food Microbiol 1993;18:139–149 [DOI] [PubMed] [Google Scholar]
- Yang H, Mokhtari A, Jaykus L, Morales R, Cates S, Cowen P. Consumer phase risk assessment for Listeria monocytogenes in deli meats. Risk Anal 2006;26:89–103 [DOI] [PubMed] [Google Scholar]
- Zubeldia BB, Jiménez MN, Claros MTV, Andrés JLM, Martin-Olmedo P. Effectiveness of the cold chain control procedure in the retail sector in Southern Spain. Food Control 2016;59:614–618 [Google Scholar]