Abstract
Background
The acceptable goal of treatment of bimaxillary protrusion is the retraction of maxillary and mandibular incisors with a resultant decrease in soft tissue convexity. This can be achieved by both surgical and orthodontic treatment methods. The aim of this study was to conduct a systematic literature review on the outcome of either method and other associated factors.
Methodology
Electronic databases (PubMed, Cochrane, Medline) were searched to identify studies that assessed hard and soft tissues changes in patients treated for bimaxillary protrusion with surgery or orthodontics. Abstracts that appeared to fulfill the initial selection criteria were selected, and the full-text original articles were retrieved and analyzed. Only articles that fulfilled the final selection criteria were finally considered. Their references were also hand-searched for possible missing articles from the database searches.
Results
The initial literature search identified 215 articles while 71 full text articles were retrieved for further analysis. Twenty-four publications were included in the final review. Most of the studies were retrospective with no randomized control trial. The studies showed high heterogeneity in type and technique of space closure, anchorage, orthodontic appliance and surgery. Surgical treatment was carried out for more severe cases than orthodontic treatment. Both methods achieved increased inter-incisal angle, however shorter treatment time appeared to be associated with surgery.
Conclusion
Satisfactory outcome were achieved with both treatment protocols. However, surgery was more indicated in severe cases.
Keywords: bimaxillary protrusion, surgical, orthodontic, systematic review
Introduction
Bimaxillary protrusion is characterized by protrusive dentition and lips with reduced inter-incisal angle. It is relatively common in African /Asian populations with varying degree of severity1. The negative perception of this trait and its effects on quality of life in most cultures makes the patient to seek treatment1-3.
The goal of treatment is retraction of maxillary and mandibular incisors with a resultant decrease in soft tissue convexity. This is achieved by extraction of premolar teeth followed by orthodontic retraction of anterior teeth using maximum anchorage mechanics4-6, surgical treatment methods are also employed7-9. Both methods have their advantages and disadvantages. Shorter treatment time is associated with surgical treatment however complications are often more reported with surgery when compared with orthodontic treatment method7-9.
The aim of this study was to review the available surgical and orthodontic treatment protocols in patients with bimaxillary protrusion. The objectives were to compare the two treatment methods in terms of correction of interincial angle, rate of space closure and complications.
Methods
Literature search
This systematic review was performed between June 2017 to September 2017 in accordance with the PRISMA statement10. We searched the PubMed, Medline, Cochrane and Prospero databases using the keywords and search strings as follows: (Bimaxillary Protrusion [mesh] OR Bimaxillary proclination OR bimaxillary dentoalveolar proclination) AND ((treatment OR orthodontic treatment)). The search was restricted to human studies published in English. In addition, the ‘‘related articles’’ options in PubMed Medline and manual search of bibliographies of identified articles were used to retrieve additional studies.
Criteria for eligibility
Studies were included if they reported on: pretreatment interincisal angle, pre-treatment molar relationship, other vertical/ antero- posterior discrepancy, outcomes for patients who had been treated with surgical or orthodontic method, and followed-up of for at least 6 months. Reviews, case reports of a single case and articles that did not report pre and post treatment cephalometric analyses were excluded. The title and abstract of the identified articles were screened based on these criteria after which the full text of all eligible articles were retrieved for further analysis. References of the included articles were screened to further identify potentially eligible articles.
Quality assessment
Recognizing that more methodologically sound studies may provide more reliable conclusions, the quality of each study was assessed using a modified quality assessment checklist for observational studies11 to evaluate the methodologic soundness of each article. The list comprise four domains representing the key components of methodological quality examined as follows:
Study design
Prospective study design with a mean follow up time clearly stated as 1 year or more.
Study population
Scores were given if eligibility (Inclusion and exclusion) criteria clearly described with sufficient descriptions of baseline characteristics which include demographics and traits of bimaxillary protrusion. In addition, studies with number of cases ≥ 50 were given scores.
Interventions
Description of details of treatment technique including all relevant predictor variables.
Outcome measurements
Studies with information on all relevant outcome measures and explanation on adverse events like complications provided as well as identical interval between measurements for all patients. Studies with information on statistical analysis were similarly scored.
A score of 0 or 1 was given depending on if each item was documented or not. The maximum score is 10.
Data collection
A proforma was used to record the data from the eligible articles. Information collected included primary author, year of publication, study type, age and number of patients, follow up, and documented complications.
Statistical analysis
Descriptive statistics was used for analysis. The characteristics of the included publications were summarized and presented in tables.
Results
The initial electronic searches of databases retrieved 215 potentially eligible articles, 7 publications were identified from other sources. After initial review of the titles and abstracts, 71 articles were selected for screening, and 151 were rejected (Fig. 1). Of the 71 articles selected for further consideration, 47 were excluded because they did not meet the inclusion criteria which left 24 full-text articles for further consideration and analysis. Of the 24 included articles reviewed, all were retrospective cohort studies except one which was prospective. The study characteristics of the selected publications are reported in Table 1.
Fig. 1. Flow Chart of the Literature Selection Process.
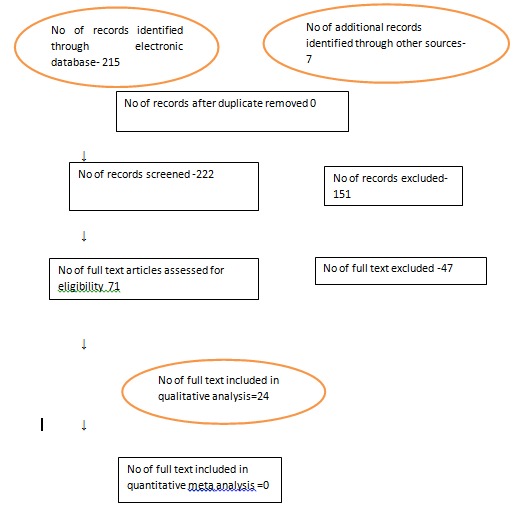
Table 1. study characteristics.
| Author/Year | Country | Study Design | Study Group/ Type | No of patients | M/F | Mean Age | Measurements Outcome(Soft tissue/dental/both) | Observation Period (months) |
| Yao et al/ 2008 | Taiwan | retrospective | Ortho/Edgewise | 47 | 4/43 | 23.5 | both | 24 |
| Hosseinzadeh-Niki et al / 2016 | Iran | retrospective | Ortho/fixed straight wire | 18 | 0/18 | 16.4 | both | 24 |
| Monga et al /2016 | India | retrospective | Ortho/fixed straight wire | 18 | 4/14 | 17.3 | both | 20 |
| Sakthi et al/2014 | India | Prospective | Ortho/surgery graft | 40 | 20/20 | 21.5 | both | 6 |
| Huang et al / 2015 | China | retrospective | Ortho/ NR | 60 | 15/45 | 23.5 | both | 12 |
| Xie et al/2013 | china | retrospective | Surgery | 20 | 1/19 | 29.0 | both | 36 |
| Solem et al /2013 | USA | retrospective | Ortho/skeletal, intra oral anchorage | 24 | 4/20 | 24 | both | 12 |
| Felembam et al/2013 | Saudi Arabia | Case series | Ortho / FA , 2stage vs enmasse retraction | 2 | 1/1 | 22 | both | 18 |
| Raypeyma et al/2013 | Iran | retrospective | Surgery/ single jaw, bimax | 40 | 14/26 | 27 | both | |
| Choo et al/2011 | USA | retrospective | Surgery/ perisegmental corticotomy | 24 | 0/24 | 27.3 | both | |
| Sharma/ 2010 | Nepal | retrospective | ortho | 30 | 15/15 | 18.4 | both | |
| Park et al/2008 | Korea | retrospective | Surgery/ ant segmental osteotomy | 30 | 1/29 | 36 | both | |
| Lee et al/ 2007 | Korea | retrospective | Ortho/surgery | 65 | 0/65 | 26 | both | |
| Bills et al/ 2005 | USA | retrospective | Ortho edgewise | 48 | 10/38 | 21.8 | both | NR |
| Baek et al/2005 | Korea | retrospective | Ortho/ Surgery | 46 | 0/46 | - | ||
| Tan /1996 | singapore | retrospective | Ortho Edgewise | 50 | / | - | both | 26 |
| Diels et al/2005 | USA | retrospective | Ortho/edgewise | 60 | 30/30 | 14.5 | both | 35 |
| Lew/ 1989 | China | retrospective | Ortho/ Begg | 32 | / | 22 | both | ? |
| O’Reilly /1989 | USA | retrospective | Surg/ subapical osteotomy | 14 | 0/14 | 25.5 | both | 6 |
| Lew et al /1989 | China | retrospective | Surg/ subapical osteotomy | 19 | / | 23 | both | 19.8 |
| Keating / 1986 | UK | retrospective | Ortho/NR | 30 | 13/17 | 11.8 | both | 61 |
| KIm et al/ 2002 | Korea | retrospective | Surgical/ corticotomy osteotomy | 20 | 2/18 | 21-33 | both | 12 |
| Chung et al/ 2011 | Korea | Case series | Ortho/ NR | 2 | 0/2 | 23-25 | both | NR |
| Koyama et al/ 2011 | Japan | retrospective | Ortho/ pm extraction, implant skeletal anchorage/ headgear | 28 | 3/25 | 24.9 | both |
A total of 767 patients were treated for bimaxillary protrusion with either methods. The gender characteristics were reported in all the articles except for three publications with overwhelming female preponderance (137/630). Age was reported as mean and range in all but two publications ranging from 24.6-31.6 years. (Table 1).
Quality assessment: Table 2 depicts the quality assessment scores of the 24 publications. Majority of the studies were scored average suggesting that most of the studies were of moderate quality.
Orthodontic treatment method
Fourteen studies4-6,12-22 evaluated treatment outcome obtained with the use of orthodontic method mainly Begg, edgewise or fixed straight wire appliances. There is wide variation in the type of anchorage device (skeletal vs non-skeletal), and stage of retraction (enmasse vs 2 stage retraction) techniques.
Surgical treatment method
Seven studies23-29 assessed outcome after surgical treatment mostly osteotomies under local anesthesia eg subapical, segmental, perisegmental, bimaxillary procedures were reported in all studies with one study reporting the additional use of bone graft30.
Both methods:
Three studies30-32utilized a comparative study design involving both treatment protocols. The study by Baek et al31 indicated that better results were reported with anterior subapical osteotomies when compared with orthodontics even though the difference was not statistically significant. Similarly, Lee et al32 reported larger amount of basal bone retraction and greater change in the upper lip projection/angulation with bimaxillary anterior subapical osteotomy when compared with orthodontics with or without corticotomy. Sakthi et al30 also found faster retraction rate corresponding to higher rate of space closure and better anchorage control when surgery was carried out.
Outcome Measure:
All the studies assessed changes in both dental and soft tissues however, there is wide variation in parameters assessed with majority reporting on inter-incisal angle, upper/lower incisor retraction, upper/lower lip retraction, naso-labial angle increase, improvement in lip procumbency, treatment time, space closure and iatrogenic complications.
Discussion
The current approach to health care delivery is hinged on evidence.Clinicians prescribing one treatment method over others depend on current best evidence for rational decision making. Therefore, this present systematic review attempted to provide current evidence for which treatment method is better in treatment of bimaxillary protrusion subjects.
An earlier systematic review of orthodontic treatment demonstrated that upper and lower lips retract and nasolabial angle increases following premolar extraction in biprotrusive patients. This study however focused only on single treatment (orthodontics) in non-growing patients and as such cannot provide current comparative evidence on both treatment methods .
In this review, the level of evidence from the selected reports was moderate/low. There was no randomized clinical trial with the majority of studies being retrospective in design. The potential for bias as a result of the quality of studies analyzed should be borne in mind.
Because of the variable outcome parameters adopted for evaluating outcome measure, direct comparison of the 767 patients was not feasible. The three comparative studies provided the only opportunity for direct comparison of treatment outcome. Although, the sample size was not large enough, it is noteworthy that the better result reported in surgical protocols is devoid of major complications commonly associated with corresponding surgical procedures. Concerns about the complications of surgical treatment especially loss of tooth vitality, periodontial problems and root resorption have earlier been expressed34.
Conclusions
In conclusion, based on the available evidence, both methods achieved increased inter-incisal angle and improved convexity with satisfactory outcome. Shorter treatment time appeared to be associated with surgery. Surgery may be indicated in severe incisor proclination, adult desirous of short treatment time, and those with additional vertical and antero-postereior discrepancy eg gummy smile, basal bone prognathism cases. For better and valid comparison of result, there is need to standardize classification, treatment technique and treatment effect with more well conducted prospective studies.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Grant support: None
References
- 1.Farrow AL, Zarrinnia K, Azizi K. Bimaxillary protrusion in black Americans--an esthetic evaluation and the treatment considerations. Am J Orthod Dentofacial Orthop. 1993;104(3):240–250. doi: 10.1016/S0889-5406(05)81725-1. [DOI] [PubMed] [Google Scholar]
- 2.Almutairi TK, Albarakati SF, Aldrees AM. Influence of bimaxillary protrusion on the perception of smile esthetics. . Saudi Med J. 2015;36(1):87–93. doi: 10.15537/smj.2015.1.9480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aldrees AM, Shamlan MA. Morphological features of bimaxillary protrusion in Saudis. . Saudi Med J. 2010;31(5):512–519. [PubMed] [Google Scholar]
- 4.Bills DA, Handelman CS, BeGole EA. Bimaxillary dentoalveolar protrusion: traits and orthodontic correction. Angle Orthod. 2005;75(3):333–339. doi: 10.1043/0003-3219(2005)75[333:BDPTAO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Sharma JN. Skeletal and soft tissue point A and B changes following orthodontic treatment of Nepalese Class I bimaxillary protrusive patients. Angle Orthod. . 2010;80(1):91–96. doi: 10.2319/010409-6.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hosseinzadeh-Nik T, Eftekhari A, Shahroudi AS, Kharrazifard MJ. Changes of the Mandible after Orthodontic Treatment with and without Extraction of Four Premolars. J Dent (Tehran). 2016;13(3):199–206. [PMC free article] [PubMed] [Google Scholar]
- 7.Chu YM, Bergeron L, Chen YR. Bimaxillary protrusion: an overview of the surgical-orthodontic treatment. Semin Plast Surg. 2009;23(1):32–39. doi: 10.1055/s-0028-1110099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jacobs JD, Bell WH. Combined surgical and orthodontic treatment of bimaxillary protrusion. Am J Orthod. 1983;83(4 ):321–333. doi: 10.1016/0002-9416(83)90228-2. [DOI] [PubMed] [Google Scholar]
- 9.Iino S, Sakoda S, Miyawaki S. An adult bimaxillary protrusion treated with corticotomy-facilitated orthodontics and titanium miniplates. Angle Orthod. 2006;76(6):1074–1082. doi: 10.2319/103105-384. [DOI] [PubMed] [Google Scholar]
- 10.The PRISMA Group. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(6):1–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Huisstede B, Miedema HS, van Opstal T, de Ronde MT, Verhaar JA, Koes BW. Interventions for treating the radial tunnel syndrome: a systematic review of observational studies. J Hand Surg Am. 2008;33:72–78. doi: 10.1016/j.jhsa.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 12.Tan TJ. Profile changes following orthodontic correction of bimaxillary protrusion with a preadjusted edgewise appliance. Int J Adult Orthodon Orthognath Surg. 1996;11(3):239–251. [PubMed] [Google Scholar]
- 13.Lew K. Profile changes following orthodontic treatment of bimaxillary protrusion in adults with the Begg appliance. Eur J Orthod. 1989;11(4):375–381. doi: 10.1093/oxfordjournals.ejo.a036009. [DOI] [PubMed] [Google Scholar]
- 14.Keating PJ. The treatment of bimaxillary protrusion. A cephalometric consideration of changes in the inter-incisal angle and soft tissue profile. Br J Orthod. 1986;13(4):209–220. [PubMed] [Google Scholar]
- 15.Chung KR, Choo H, Lee JH, Kim SH. Atypical orthodontic extraction pattern managed by differential en-masse retraction against a temporary skeletal anchorage device in the treatment of bimaxillary protrusion. Am J Orthod Dentofacial Orthop. 2011;140(3):423–432. doi: 10.1016/j.ajodo.2009.08.036. [DOI] [PubMed] [Google Scholar]
- 16.Huang YP, Li WR. Correlation between objective and subjective evaluation of profile in bimaxillary protrusion patients after orthodontic treatment. Angle Orthod. 2015;85(4):690–698. doi: 10.2319/070714-476.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diels RM, KalraZ DeLoach, Powers M, Nelson SS. Changes in soft tissue profile of African-Americans following extraction treatment. Angle Orthod. 1995;65(4):285–292. doi: 10.1043/0003-3219(1995)065<0285:CISTPO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Felemban NH, Al-Sulaimani FF, Murshid ZA, Hassan AH. En masse retraction versus two-step retraction of anterior teeth in extraction treatment of bimaxillary protrusion. J Orthod Sci. 2013;2(1):28–37. doi: 10.4103/2278-0203.110330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koyama I, Iino S, Abe Y, Takano-Yamamoto T, Miyawaki S. Differences between sliding mechanics with implant anchorage and straight-pull headgear and intermaxillary elastics in adults with bimaxillary protrusion. Eur J Orthod. . 2011;33(2):126–131. doi: 10.1093/ejo/cjq047. [DOI] [PubMed] [Google Scholar]
- 20.Monga N, Kharbanda OP, Samrit V. Quantitative and qualitative assessment of anchorage loss during en-masse retraction with indirectly loaded miniscrews in patients with bimaxillary protrusion. Am J Orthod Dentofacial Orthop. 2016;150(2):274–282. doi: 10.1016/j.ajodo.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 21.Solem RC. Three-dimensional soft-tissue and hard-tissue changes in the treatment of bimaxillary protrusion. . Am J Orthod Dentofacial Orthop. 2013;144(2):218–228. doi: 10.1016/j.ajodo.2013.03.018. [DOI] [PubMed] [Google Scholar]
- 22.Yao CC, Lai EH, Chang JZ, Chen I, Chen YJ. Comparison of treatment outcomes between skeletal anchorage and extraoral anchorage in adults with maxillary dentoalveolar protrusion. Am J Orthod Dentofacial Orthop. 2008;134(5):615–624. doi: 10.1016/j.ajodo.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 23.O'Reilly MT. Integumental profile changes after surgical orthodontic correction of bimaxillary dentoalveolar protrusion in black patients. Am J Orthod Dentofacial Orthop. 1989;96(3):242–248. doi: 10.1016/0889-5406(89)90461-7. [DOI] [PubMed] [Google Scholar]
- 24.Rahpeyma A, Khajehahmadi S. Effects of bimax and segmental surgeries for correction of bimaxillary dentoalveolar protrusion class I on soft tissue parameters: upper lip thickness and curvature, nasolabial angle and nasal prominence. J Contemp Dent Pract. 2013;14(6):1087–1093. doi: 10.5005/jp-journals-10024-1456. [DOI] [PubMed] [Google Scholar]
- 25.Kim JR, Son WS, Lee SG. A retrospective analysis of 20 surgically corrected bimaxillary protrusion patients. Int J Adult Orthodon Orthognath Surg. 2002;17(1):23–27. [PubMed] [Google Scholar]
- 26.Lew KK, Loh FC, Yeo JF, Loh HS. Profile changes following anterior subapical osteotomy in Chinese adults with bimaxillary protrusion. Int J Adult Orthodon Orthognath Surg. 1989;4(3):189–196. [PubMed] [Google Scholar]
- 27.Choo H, Heo HA, Yoon HJ, Chung KR, Kim SH. Treatment outcome analysis of speedy surgical orthodontics for adults with maxillary protrusion. Am J Orthod Dentofacial Orthop. 2011;140(6):251–262. doi: 10.1016/j.ajodo.2011.06.029. [DOI] [PubMed] [Google Scholar]
- 28.Xie F, Teng L, Jin X, Zheng J, Xu J, Lu J, Zhang C, Xu M, Zeng H, Li S, Sun X. Systematic analysis of clinical outcomes of anterior maxillary and mandibular subapical osteotomy with preoperative modeling in the treatment of bimaxillary protrusion. J Craniofac Surg. 2013;24(6):1980–1986. doi: 10.1097/SCS.0b013e3182a28b45. [DOI] [PubMed] [Google Scholar]
- 29.Park JU, Hwang YS. Evaluation of the soft and hard tissue changes after anterior segmental osteotomy on the maxilla and mandible. Oral Maxillofac Surg. 2008;66(1):98–103. doi: 10.1016/j.joms.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 30.Sakthi SV, Vikraman B, Shobana VR, Iyer SK, Krishnaswamy NR. Corticotomy-assisted retraction: an outcome assessment. Indian J Dent Res. 2014;26(6):748–754. doi: 10.4103/0970-9290.152191. [DOI] [PubMed] [Google Scholar]
- 31.Baek SH, Kim BH. Determinants of successful treatment of bimaxillary protrusion: orthodontic treatment versus anterior segmental osteotomy. . J Craniofac Surg. 2005;16(2):234–246. doi: 10.1097/00001665-200503000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Lee JK, Chung KR, Baek SH. Treatment outcomes of orthodontic treatment, corticotomy-assisted orthodontic treatment, and anterior segmental osteotomy for bimaxillary dentoalveolar protrusion. Plast Reconstr Surg. 2007;120(4):1027–1036. doi: 10.1097/01.prs.0000277999.01337.8b. [DOI] [PubMed] [Google Scholar]
- 33.Leonardi R. Soft tissue changes following the extraction of premolars in nongrowing patients with bimaxillary protrusion. A systematic review. Angle Orthod. 2010;80(1):211–216. doi: 10.2319/010709-16.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoogeveen EJ, Jansma J, Ren Y. Surgically facilitated orthodontic treatment: a systematic review.A. Am J Orthod Dentofacial Orthop. 2014;145(4 Suppl):S51–S64. doi: 10.1016/j.ajodo.2013.11.019. [DOI] [PubMed] [Google Scholar]


