Significance
Inequalities in mortality and morbidity among socioeconomic groups are a highly persistent phenomenon despite having been the focus of public health policy in many countries. The United States has recently witnessed a widening of health inequalities due to rising mortality and morbidity among the lowly educated. Our study shows that, despite the financial crisis, most European countries have experienced an improvement in the health of the lowly educated in recent years. In Eastern Europe, this even represents a reversal as compared with previous decades. The 2008 financial crisis has had mixed effects without widening health inequalities. Our results suggest that European countries have been successful in avoiding an aggravation of health inequalities.
Keywords: mortality, morbidity, health inequalities, Europe, financial crisis
Abstract
Unfavorable health trends among the lowly educated have recently been reported from the United States. We analyzed health trends by education in European countries, paying particular attention to the possibility of recent trend interruptions, including interruptions related to the impact of the 2008 financial crisis. We collected and harmonized data on mortality from ca. 1980 to ca. 2014 for 17 countries covering 9.8 million deaths and data on self-reported morbidity from ca. 2002 to ca. 2014 for 27 countries covering 350,000 survey respondents. We used interrupted time-series analyses to study changes over time and country-fixed effects analyses to study the impact of crisis-related economic conditions on health outcomes. Recent trends were more favorable than in previous decades, particularly in Eastern Europe, where mortality started to decline among lowly educated men and where the decline in less-than-good self-assessed health accelerated, resulting in some narrowing of health inequalities. In Western Europe, mortality has continued to decline among the lowly and highly educated, and although the decline of less-than-good self-assessed health slowed in countries severely hit by the financial crisis, this affected lowly and highly educated equally. Crisis-related economic conditions were not associated with widening health inequalities. Our results show that the unfavorable trends observed in the United States are not found in Europe. There has also been no discernible short-term impact of the crisis on health inequalities at the population level. Both findings suggest that European countries have been successful in avoiding an aggravation of health inequalities.
Although reducing inequalities in health among socioeconomic groups has become a priority for policy-makers in many European countries, health inequalities have generally widened over the period from 1980 to the late 2000s (1–4). An update of these findings for the 2010s is urgently needed, for two reasons. The first is that unfavorable trends in mortality among the lowly educated have recently been reported from the United States (5). Since the early 2000s total mortality and self-reported morbidity have risen among middle-aged white Americans as a result of rising rates of suicide and poisonings, partly due to an epidemic of misuse of opioid painkiller drugs (6). These deaths have been labeled “deaths of despair,” because the increases in mortality were concentrated among the lowly educated who in the United States have experienced increasing economic and social disadvantage (7).
The second reason is that the impact of the 2008 financial crisis and its aftermath on health inequalities is unknown. The crisis led to an economic recession with rising unemployment and fiscal austerity in most European countries, particularly in countries that had to be bailed out by the international community such as Greece, Cyprus, and Ireland (8). Because there were important differences among countries (SI Appendix, Fig. S1), there is ample scope for assessing the impact of the crisis. Previous recessions usually have had limited effects on population health, with increases in suicide and alcohol-related deaths and decreases in road-traffic fatalities (9). So far, the evidence for the latest recession is mixed: All-cause mortality has continued to decline, but suicide rates have risen, as have some other health problems in some of the countries that were severely hit, such as Greece, Spain, and Portugal (10). However, because the negative consequences of economic crises are likely to be borne primarily by the most disadvantaged, it is important to assess the health effects by socioeconomic group. Here again, the available evidence is scarce (11, 12).
The study reported in this paper therefore aimed to assess recent trends in health inequalities in a large number of European countries, paying particular attention to the possible impact of the 2008 financial crisis. Health inequalities are quantified both on a relative scale (using ratio measures such as the Relative Index of Inequality, RII) and on an absolute scale (using difference measures such as the Slope Index of Inequality, SII) (13). Both perspectives are important. Because relative inequalities depend only on the distribution of health problems in the population, they are often more easily understood. However, because a 50% higher rate of a rare health problem is less important for the public’s health than a 10% higher rate of a much more frequent health problem, absolute inequalities, which also depend on the average rate of health problems in the population, are important too (14).
Results
Trends in Mortality.
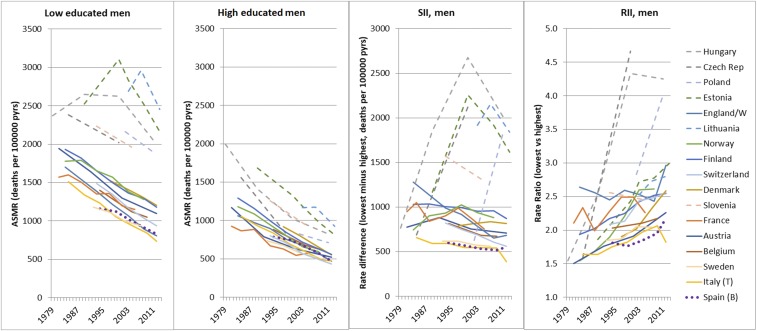
In most Western European countries, mortality has declined steadily among both the lowly and highly educated without visible signs of a trend interruption in the late 2000s (Fig. 1; results for women are given in SI Appendix, Fig. S2). Because relative declines were usually larger among the highly educated, relative inequalities as measured by the RII have generally increased considerably; because absolute declines were usually larger among the lowly educated, absolute inequalities as measured by the SII have often decreased. The only Western European country severely hit by the crisis for which we have recent mortality data, Spain, has experienced continued rapid mortality declines among both the lowly and highly educated (see SI Appendix, Table S4 for additional data).
Fig. 1.
Trends in all-cause mortality by education, men, ca. 1980 to ca. 2014. Dashed lines represent Eastern Europe. The dotted line represents Spain, the Western European country most severely hit by the economic crisis. ASMR, age-standardized mortality rate; pyrs, person-years. Results for women are shown in SI Appendix, Fig. S2.
Trends in all-cause mortality in Eastern Europe were completely different. In several Eastern European countries, particularly Hungary, Lithuania, and Estonia, a trend reversal has occurred: After a dramatic increase in previous decades, mortality has started to decline among the lowly educated, and as a result absolute inequalities in mortality have also started to go down.
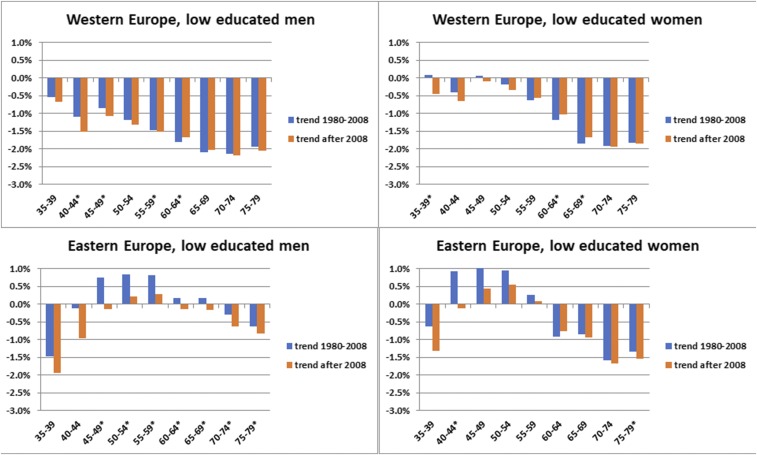
Because of the differences in trends between Western and Eastern Europe, we stratified the interrupted time-series analyses by region. These confirm that there was no change in all-cause mortality trend in recent years among either the lowly educated or highly educated in Western Europe but that a favorable change did occur among lowly educated men in Eastern Europe (Fig. 2 and SI Appendix, Table S5). These favorable changes were strongest among the middle-aged and for mortality from cancer, alcohol-related causes, and suicide, as previously rising trends slowed.
Fig. 2.
Trends in age-specific mortality among lowly educated men and women between ca. 1980 and ca. 2008 and after ca. 2008, by region and sex. Graphs show average percent annual change in mortality as estimated in interrupted time-series analyses (the trend for 1980–2008 is based on β1; the trend after 2008 is based on β1 and β2; see Materials and Methods for details). Asterisks indicate statistically significant (P < 0.05) differences between the two periods. For distinctions between Western and Eastern Europe, see SI Appendix, Table S1.
Trends were generally unchanged, but not altogether favorable, in Western Europe. There was no mortality decline among younger lowly educated women, as mortality from smoking-and alcohol-related causes went up. However, mortality from most causes of death declined among lowly educated men and women. After 2008 this decline accelerated for road injuries, whereas the increase of alcohol-related mortality slowed. There was no change in trend for suicide and causes amenable to medical care.
Trends in Self-Reported Morbidity.
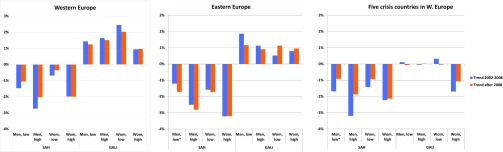
An interrupted time-series analysis for two self-reported health measures shows that the trends for self-assessed health (SAH) were somewhat similar to those for all-cause mortality but that the trends for activity limitations were different (Fig. 3 and SI Appendix, Fig. S3 and Table S6). There was a clear downward trend for the prevalence of less-than-good SAH among both the lowly and highly educated in both Western and Eastern Europe. After 2008 this decline accelerated in Eastern but not in Western Europe. Declines in less-than-good SAH have been faster among the highly educated, so that inequalities in SAH have on average increased over time.
Fig. 3.
Trends in less-than-good SAH and activity limitations among the lowly and highly educated between 2002 and 2008 and after 2008, by region and sex. Graphs show the average percent annual change in prevalence as estimated in interrupted time-series analysis (the trend for 1980–2008 is based on β1; the trend after 2008 is based on β1 and β2; see Materials and Methods for details). Asterisks indicate statistically significant (P < 0.05) differences between the two periods. For distinctions between Western and Eastern Europe, see SI Appendix, Table S3. The five crisis countries in Western Europe were Ireland, Spain, Portugal, Greece, and Cyprus. GALI, global activity limitations indicator.
In contrast to both mortality and SAH, the trend for the prevalence of activity limitations has been upwards among the lowly and highly educated in both Western and Eastern Europe, without a statistically significant change in trend in 2008. Again, because trends were more favorable among the highly educated, inequalities in activity limitations have on average increased over time (SI Appendix, Fig. S3).
In the five Western European countries most severely hit by the crisis, trends in SAH were less favorable after 2008 (Fig. 3). There was a statistically significant slow-down in the decline in less-than-good SAH among lowly educated men, but as a similar (nonsignificant) slow-down occurred among highly educated men, the gap in less-than-good SAH between lowly and highly educated men did not widen (SI Appendix, Fig. S4).
Determinants of Trends in Mortality and Self-Reported Morbidity.
A more direct assessment of the impact of the crisis is provided by country and period fixed-effects analyses in which health outcomes are regressed on crisis-related economic variables (Table 1 and SI Appendix, Table S7). If the crisis had affected population health, either directly or indirectly through the ensuing austerity measures, one would expect the economic indicators in Table 1 to be associated with mortality, SAH, and/or activity limitations. This is indeed the case, but not always in a direction indicating worse health and/or widening health inequalities as a result of the crisis.
Table 1.
Relationship between crisis-related variables and mortality, less-than-good SAH, and activity limitations, by education, for men
| Mortality, 95% CI | SAH, 95% CI | Activity limitations, 95% CI | ||||||||
| Independent variable | Education | Estimate | Lower | Upper | Estimate | Lower | Upper | Estimate | Lower | Upper |
| National income, log | Low | −0.200 | −0.283 | −0.116 | −0.188 | −0.324 | −0.053 | 0.234 | 0.009 | 0.459 |
| High | −0.327 | −0.435 | −0.220 | −0.426 | −0.646 | −0.206 | 0.190 | −0.160 | 0.541 | |
| Unemployment, % | Low | 0.008 | −0.012 | −0.004 | −0.003 | −0.008 | 0.002 | −0.002 | −0.010 | 0.006 |
| High | −0.010 | −0.016 | −0.005 | −0.006 | −0.013 | 0.002 | 0.004 | −0.008 | 0.016 | |
| Material deprivation, % | Low | −0.569 | −0.863 | −0.275 | 0.094 | −0.105 | 0.293 | 0.334 | −0.007 | 0.674 |
| High | −0.525 | −1.320 | 0.269 | −0.240 | −0.730 | 0.249 | −0.383 | −1.173 | 0.407 | |
| Social transfers, % GDP | Low | −0.002 | −0.008 | 0.005 | −0.005 | −0.017 | 0.007 | 0.022 | 0.002 | 0.042 |
| High | −0.007 | −0.016 | 0.002 | −0.022 | −0.042 | −0.003 | 0.030 | −0.001 | 0.061 | |
| Health expenditure, % GDP | Low | −0.043 | −0.069 | −0.018 | 0.020 | −0.005 | 0.045 | 0.026 | −0.017 | 0.069 |
| High | −0.053 | −0.081 | −0.025 | −0.031 | −0.073 | 0.011 | 0.004 | −0.063 | 0.072 | |
| Out-of-pocket expenses, % | Low | 0.003 | −0.007 | 0.013 | −0.005 | −0.011 | 0.001 | −0.002 | −0.013 | 0.009 |
| High | 0.006 | −0.006 | 0.017 | 0.001 | −0.010 | 0.012 | 0.004 | −0.014 | 0.021 | |
All dependent variables were log transformed. Bold type indicates 95% CI does not include 0. Control variables: country, period, survey (except for mortality), and lnGDP (except for model for national income). Multilevel model with correction for serial autocorrelation, stratified by gender and level of education. All determinants are national averages, with the exception of material deprivation, which was available for lowly and highly educated men and women separately. Similar results were found for women (SI Appendix, Table S7).
National income was negatively associated with mortality, implying that stagnation of national income slowed the mortality decline. However, the effect was stronger among the highly educated, indicating an inequalities-narrowing effect. Health care expenditure was also negatively associated with mortality, but as the effect was equally strong among the lowly and highly educated, inequalities in mortality did not widen when budgets went down. Increases in unemployment and material deprivation were associated with lower, not higher, mortality among both the lowly and highly educated, and again the effects were about equally strong in both groups. Social transfers and out-of-pocket payments for health care were not associated with mortality.
National income was also negatively associated with SAH among both the lowly and highly educated, with stronger effects among the highly educated implying that stagnation of national income narrowed inequalities in SAH. Instead of health care expenditure, social transfers were associated with SAH, but no further associations were found. The deviating trends for activity limitations that we saw in our descriptive analyses are reflected in equally deviant associations with national income: Rising national income went together with a rising prevalence of activity limitations among both the lowly and highly educated.
Discussion
Western Europe.
In Western Europe, relative inequalities in mortality (e.g., measured as rate ratios between a lower and higher socioeconomic group) have almost universally increased over the past decades, although, as a result of declining overall mortality among both lowly and highly educated groups, absolute inequalities in mortality have often declined (1, 4).
The evidence presented in this paper suggests that the financial crisis had no discernible short-term impact on health inequalities at the population level in Western Europe. This is good news, because it could easily have been different (15). Why did the very real increases in unemployment and poverty, often accompanied by cuts to social security and health services, not lead to a discernible widening of health inequalities? We think that the explanation is twofold, particularly in the case of mortality: The underlying trends were too powerful to be derailed, and the short-term effects of the crisis on people’s living conditions were too weak and too well-buffered to be translated into wide-spread health risks.
Most Western European countries have enjoyed many decades of more-or-less continuous mortality decline as a result of continuous improvements in living standards and advances in prevention (including behavior change) and health care (16). Although improvements in living standards have temporarily slowed down (or even reversed) during the economic crisis, this will not immediately outdo the effects of lifelong exposure to higher living standards of each new generation (17). Also, advances in prevention and health care have continued, as illustrated by continuing rapid declines in mortality from smoking-related conditions, conditions amenable to medical care, and ischemic heart disease (SI Appendix, Table S5).
This combines with the second factor: The effects of the economic crisis on people’s health risks were probably mixed, because some risks, such as the stress of being laid off or having financial debts, increased, contributing to a rise in the suicide rate, whereas other risks, such as the risk of dying in a car crash or of excessive drinking, declined. Previous analyses of the mortality effects of economic crises have shown that many causes of death follow a “procyclical” pattern in which mortality increases during economic upturns but decreases during downturns (18). It is likely that such procyclical effects explain our finding in Table 1 that short-term increases in unemployment and material deprivation were associated with lower, not higher, mortality among both lowly and highly educated groups. Any mortality-increasing effects of the crisis were probably also buffered by the extensive social security and financially accessible health care systems still in place in most European countries (9). The latter interpretation finds support in detailed analyses of the lack of impact of previous recessions on health inequalities in the Nordic countries (19).
Eastern Europe.
In Eastern Europe, both relative and absolute inequalities in mortality have exploded since the early 1990s, sometimes as a result of dramatically rising mortality in lower socioeconomic groups during and after the political and economic transformations following the collapse of the Soviet Union (2, 3). Whereas the rise of relative inequalities in mortality in Western Europe is the result of differences in mortality decline between lowly and highly educated groups, the enormous rise of both relative and absolute inequalities in mortality in Eastern Europe is often the result of rising mortality among the lowly educated and declining mortality among the highly educated (Fig. 1).
We consider the recent reversal of the mortality trend among the lowly educated in several Eastern European countries as our most remarkable finding. With the exception of Estonia (20), this has not been reported before, although favorable changes in national mortality trends have been noticed (21–23). Recent declines in mortality among the lowly educated in Eastern Europe are due to declines in mortality from smoking-related causes, causes amenable to medical care, and ischemic heart disease and sometimes also in mortality from alcohol-related causes and suicide (SI Appendix, Fig. S5). For the total population these changes have been attributed to a combination of long-term declines in smoking, improvements in health care, dietary changes, road-traffic safety measures, and alcohol control policies (23). Apparently, these mortality-lowering policies have finally also reached the lowly educated.
The facts that the 2008 crisis was short-lived in most Eastern European countries and that the European Commission supported massive investments in these countries’ infrastructure may also have helped. However, despite the welcome trend reversal, levels of mortality among the lowly educated in Eastern Europe remain extremely high, and trends remain disappointing, particularly among the middle-aged (Figs. 1 and 2).
Comparison with the United States.
Compared with the United States, trends in health inequalities have been more favorable in Western Europe, although declines in mortality among the lowly educated were slow among middle-aged men and were nearly absent among middle-aged women (Fig. 2). A detailed inspection of age-specific mortality trends by country revealed that no Western European country experienced the increases in mortality reported in the United States (6).
The latter have been attributed to a toxic mixture of greater socioeconomic inequalities, less comprehensive social security arrangements, a less accessible health care system, and the widespread availability of dangerous prescription drugs (7). Our results suggest that European health care systems may indeed play a role in constraining inequalities in mortality (Table 1). Equal relative effects of rising health care expenditure on mortality among lowly and highly educated groups imply larger absolute effects among the former and a narrowing of absolute inequalities in mortality when health care spending goes up—a finding that we have analyzed in more detail elsewhere (24). That we find no effects of out-of-pocket payments on mortality or self-reported morbidity (Table 1) suggests that rising out-of-pocket payments, which were part of austerity measures in several countries, have fortunately had limited effects on population health in most European countries.
SAH and Activity Limitations.
It is easier to interpret our findings for mortality than those for self-reported health problems. Trends for SAH are somewhat similar to those for mortality, and it is tempting to invoke similar explanations, but whether these are valid remains to be seen.
For activity limitations, we confess our inability to explain the results. In individual-level analyses, activity limitations are associated with risk factors similar to those for mortality and SAH, including poverty and behavioral risk factors (25). However, in aggregate-level analyses we find deviant patterns, i.e., a rising prevalence which is stronger in countries with more rapidly rising national income.
One possible explanation is that the threshold for reporting activity limitations has become lower over time as a result of societal changes captured by rising national income, such as greater access to disability benefits (26). Another possibility is that rising life expectancy has come at the cost of an expansion of disability (27). Whatever the explanation, the general widening of inequalities in activity limitations, SAH, and mortality over time, particularly when measured at a relative scale, clearly illustrates the frustratingly persistent nature of health inequalities in European welfare states.
Strengths and Limitations.
This study provides a comprehensive and robust picture of trends in health inequalities in a large number of European countries. When we started our data collection in 2016, the most recent data available were for 2014, which implies that our study covers only a short period after the onset of the crisis in 2008. Also, mortality data for the early 2010s were available for only 11 countries. While this illustrates “the contrast between the substantial efforts expended by governments to collect up-to-the-minute financial data while health data lag by several years” (28), it also means that we are studying the short-term effects of the crisis.
Despite the near-absence of discernible short-term effects, the crisis may have negative long-term effects on health and health inequalities, for example through missed opportunities for economic advancement of young generations in countries with mass youth unemployment (29). Follow-up studies are therefore necessary to determine what the long-term impact of recession and austerity on health inequalities will be.
Mortality and to a lesser extent activity limitations often represent the end of a disease process that has taken years to unfold and therefore may not be particularly suitable for the detection of short-term effects. Measurement error, particularly in the case of activity limitations, which has not been fully harmonized in the European survey from which we have taken our data (the European Union Statistics on Income and Living Conditions, EU-SILC) (30), may also reduce sensitivity. On the other hand, our analysis also included outcome measures that may respond more immediately, such as mortality from causes amenable to medical care or injuries and SAH. The latter also captures mental health problems, for which health inequalities widened within a few years after the crisis in Spain (31).
We consider the combination of mortality with morbidity data a strength of our study, despite the fact that the morbidity measures were self-reported. Both between-country and within-country inequalities in self-reported morbidity may be distorted by differences in reporting styles (32–34). However, as our main focus is on changes occurring over relatively short time periods, we consider our results to be robust against these sources of bias.
Finally, although low education is a strong marker of social disadvantage, it is possible that the health effects of the crisis are concentrated in only a subgroup of the lowly educated or that vulnerability to these health effects is better captured by other social distinctions, such as occupational class, geographic location, or ethnicity. For example, in the United Kingdom the impact of public sector budget cuts has been felt most severely in deprived regions (35), and the full effects of the crisis therefore may not be detectable in national-level data.
Conclusion
In contrast to the United States, and despite the occurrence of an economic crisis, the health of the lowly educated in Europe has improved in recent years, and health inequalities have sometimes narrowed.
Materials and Methods
Data.
We collected and harmonized register-based mortality data from 17 European countries. An overview of the mortality data sources and some key characteristics of the data are given in SI Appendix, Table S1. We also collected and harmonized data on self-reported health problems from two cross-national surveys: the European Social Survey (ESS), with biannual waves between 2002 and 2014, and the EU-SILC survey, with annual waves between 2004 and 2014. An overview of the survey data and some key characteristics are given in SI Appendix, Table S3). Together, these surveys cover 27 European countries. Both surveys include two single-item health questions: SAH (“How is your health in general”) and activity limitations (the Global Activity Limitations Indicator: “For at least the past 6 mo, to what extent have you been limited in activities people usually do?”).
Socioeconomic position was indicated by highest level of completed education with low, mid, and high corresponding to the International Standard Classification of Education (ISCED) 1997 categories 0–2, 3–4, and 5–6, respectively. We focused on educational inequalities (instead of, e.g., occupational inequalities) primarily because comparable data on educational attainment were available for both mortality and survey data in all European populations under study. Education is also the most stable measure of socioeconomic position because it is normally completed early in adulthood, which avoids most problems of reverse causation (36). The analyses were restricted to persons 35–79 y of age because education gradually loses its discriminatory power as a measure of socioeconomic status among the elderly.
For our analysis of the determinants of trends in health inequalities we extracted six indicators of economic recession and/or the policy response to the financial crisis: national income [Gross Domestic Product (GDP)], unemployment (unemployed as percentage of the labor force), material deprivation (inability to pay for at least three of nine items), social transfers (social security transfers as a percentage of GDP), health care expenditure (current expenditure on health as a percentage of GDP), and out-of-pocket payments for health (as a percentage of total health expenditure). With the exception of the poverty indicators, which were available by sex and education and only for the period 2004–2014, all these variables represent yearly national averages for the period 1980–2014.
Methods.
The mortality and self-reported morbidity rates by sex and educational level were directly age-standardized using the European Standard Population. We studied changes in the magnitude of both relative and absolute inequalities, using both simple measures [rate ratios (RR) and rate differences (RD)] and more complex (RII and SII), which take into account all education groups as well as each education group’s share in the total population and therefore provide adjustment for changes in educational composition over time (13).
To quantify changes over time in mortality and self-reported morbidity and to assess whether a recent change in trend has occurred, we conducted interrupted time-series analyses in which mortality and self-reported morbidity were modeled as a function of time, including a possible change in trend after 2008. To more directly analyze the association between changes over time in health outcomes and the crisis, we conducted panel (or pooled cross-sectional time-series) analyses in which health outcomes were modeled as a function of crisis-related economic variables using country and period fixed effects. For more details on the analysis, see SI Appendix, Box S1.
Supplementary Material
Acknowledgments
We thank Prof. Martin McKee (London School of Hygiene and Tropical Medicine) and Dr. Domantas Jasilionis (Max Planck Institute for Demographic Research) for their comments on a previous version of this paper. This study was conducted as part of the LIFEPATH project, which has received financial support from European Commission Horizon 2020 Grant 633666. Data were partly collected as part of the Developing Methodologies to Reduce Inequalities in the Determinants of Health (DEMETRIQ) project, which received support from European Commission Grant FP7-CP-FP 278511. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. For acknowledgments relating to data acquisition, see SI Appendix, Box S2.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission. T.S. is a guest editor invited by the Editorial Board.
Data deposition: The aggregate data reported in this paper have been deposited in the institutional repository of Erasmus University Rotterdam (http://hdl.handle.net/1765/106273).
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1800028115/-/DCSupplemental.
References
- 1.Mackenbach JP, et al. Changes in mortality inequalities over two decades: Register based study of European countries. BMJ. 2016;353:i1732. doi: 10.1136/bmj.i1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leinsalu M, et al. Educational inequalities in mortality in four Eastern European countries: Divergence in trends during the post-communist transition from 1990 to 2000. Int J Epidemiol. 2009;38:512–525. doi: 10.1093/ije/dyn248. [DOI] [PubMed] [Google Scholar]
- 3.Shkolnikov VM, et al. The changing relation between education and life expectancy in central and eastern Europe in the 1990s. J Epidemiol Community Health. 2006;60:875–881. doi: 10.1136/jech.2005.044719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hu Y, et al. Trends in socioeconomic inequalities in self-assessed health in 17 European countries between 1990 and 2010. J Epidemiol Community Health. 2016;70:644–652. doi: 10.1136/jech-2015-206780. [DOI] [PubMed] [Google Scholar]
- 5.Montez JK, Zajacova A. Why is life expectancy declining among low-educated women in the United States? Am J Public Health. 2014;104:e5–e7. doi: 10.2105/AJPH.2014.302146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci USA. 2015;112:15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Case A, Deaton A. Mortality and morbidity in the 21st century. Brookings Pap Econ Act. 2017;2017:397–476. doi: 10.1353/eca.2017.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Keeley B, Love P. From Crisis to Recovery: The Causes, Course and Consequences of the “Great Recession”. Organization for Economic Cooperation and Development; Paris: 2010. [Google Scholar]
- 9.Stuckler D, Basu S, Suhrcke M, Coutts A, McKee M. The public health effect of economic crises and alternative policy responses in Europe: An empirical analysis. Lancet. 2009;374:315–323. doi: 10.1016/S0140-6736(09)61124-7. [DOI] [PubMed] [Google Scholar]
- 10.Karanikolos M, et al. Financial crisis, austerity, and health in Europe. Lancet. 2013;381:1323–1331. doi: 10.1016/S0140-6736(13)60102-6. [DOI] [PubMed] [Google Scholar]
- 11.Bacigalupe A, Escolar-Pujolar A. The impact of economic crises on social inequalities in health: What do we know so far? Int J Equity Health. 2014;13:52. doi: 10.1186/1475-9276-13-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Regidor E, et al. Mortality decrease according to socioeconomic groups during the economic crisis in Spain: A cohort study of 36 million people. Lancet. 2016;388:2642–2652. doi: 10.1016/S0140-6736(16)30446-9. [DOI] [PubMed] [Google Scholar]
- 13.Mackenbach JP, Kunst AE. Measuring the magnitude of socio-economic inequalities in health: An overview of available measures illustrated with two examples from Europe. Soc Sci Med. 1997;44:757–771. doi: 10.1016/s0277-9536(96)00073-1. [DOI] [PubMed] [Google Scholar]
- 14.Mackenbach JP. Should we aim to reduce relative or absolute inequalities in mortality? Eur J Public Health. 2015;25:185. doi: 10.1093/eurpub/cku217. [DOI] [PubMed] [Google Scholar]
- 15.Suhrcke M, Stuckler D. Will the recession be bad for our health? It depends. Soc Sci Med. 2012;74:647–653. doi: 10.1016/j.socscimed.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 16.Leon DA. Trends in European Life Expectancy: A Salutary View. Oxford Univ Press; Oxford: 2011. [DOI] [PubMed] [Google Scholar]
- 17.Kuh D, Shlomo YB. A Life Course Approach to Chronic Disease Epidemiology. Oxford Univ Press; Oxford: 2004. [Google Scholar]
- 18.Ruhm CJ. Are recessions good for your health? Q J Econ. 2000;115:617–650. [Google Scholar]
- 19.Avendano M, Moustgaard H, Martikainen P. Are some populations resilient to recessions? Economic fluctuations and mortality during a period of economic decline and recovery in Finland. Eur J Epidemiol. 2017;32:77–85. doi: 10.1007/s10654-016-0152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lai T, Leinsalu M. Trends and Inequalities in Mortality of Noncommunicable Diseases. Case Study for Estonia. WHO Regional Office for Europe; Copenhagen, Denmark: 2015. [Google Scholar]
- 21.Meslé F. Mortality in central and Eastern Europe: Long-term trends and recent upturns. Demogr Res. 2004;2:45–70. [Google Scholar]
- 22.Mackenbach JP, Karanikolos M, Lopez Bernal J, Mckee M. Why did life expectancy in Central and Eastern Europe suddenly improve in the 1990s? An analysis by cause of death. Scand J Public Health. 2015;43:796–801. doi: 10.1177/1403494815599126. [DOI] [PubMed] [Google Scholar]
- 23.Jasilionis D, Meslé F, Shkolnikov VM, Vallin J. Recent life expectancy divergence in Baltic countries. Eur J Popul. 2011;27:403–431. [Google Scholar]
- 24.Mackenbach JP, et al. Trends in inequalities in mortality amenable to health care in 17 European countries. Health Aff (Millwood) 2017;36:1110–1118. doi: 10.1377/hlthaff.2016.1674. [DOI] [PubMed] [Google Scholar]
- 25.Cambois E, Solé-Auró A, Robine JM. Economic hardship and educational differentials in disability in 26 European countries. J Aging Health. 2016;28:1214–1238. doi: 10.1177/0898264316656503. [DOI] [PubMed] [Google Scholar]
- 26.Nattrass B, Altomare M, Van Soest A. Vignettes and self-reports of work disability in the United States and The Netherlands. Am Econ Rev. 2007;97:461–473. [Google Scholar]
- 27.Olshansky SJ, Rudberg MA, Carnes BA, Cassel CK, Brody JA. Trading off longer life for worsening health: The expansion of morbidity hypothesis. J Aging Health. 1991;3:194–216. [Google Scholar]
- 28.Stuckler D, Basu S, Suhrcke M, Coutts A, McKee M. Effects of the 2008 recession on health: A first look at European data. Lancet. 2011;378:124–125. doi: 10.1016/S0140-6736(11)61079-9. [DOI] [PubMed] [Google Scholar]
- 29.Mroz TA, Savage TH. The long-term effects of youth unemployment. J Hum Resour. 2006;41:259–293. [Google Scholar]
- 30.Ekholm O, Brønnum-Hansen H. Cross-national comparisons of non-harmonized indicators may lead to more confusion than clarification. Scand J Public Health. 2009;37:661–663. doi: 10.1177/1403494809341098. [DOI] [PubMed] [Google Scholar]
- 31.Bartoll X, Palència L, Malmusi D, Suhrcke M, Borrell C. The evolution of mental health in Spain during the economic crisis. Eur J Public Health. 2014;24:415–418. doi: 10.1093/eurpub/ckt208. [DOI] [PubMed] [Google Scholar]
- 32.Cawley J, Choi A. Health Disparities across Education: The Role of Differential Reporting Error. National Bureau of Economic Research; Cambridge, MA: 2015. [DOI] [PubMed] [Google Scholar]
- 33.d’Uva TB, O’Donnell O, van Doorslaer E. Differential health reporting by education level and its impact on the measurement of health inequalities among older Europeans. Int J Epidemiol. 2008;37:1375–1383. doi: 10.1093/ije/dyn146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berger N, et al. Assessing the validity of the global activity limitation indicator in fourteen European countries. BMC Med Res Methodol. 2015;15:1. doi: 10.1186/1471-2288-15-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reeves A, Basu S, McKee M, Marmot M, Stuckler D. Austere or not? UK coalition government budgets and health inequalities. J R Soc Med. 2013;106:432–436. doi: 10.1177/0141076813501101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Daly MC, Duncan GJ, McDonough P, Williams DR. Optimal indicators of socioeconomic status for health research. Am J Public Health. 2002;92:1151–1157. doi: 10.2105/ajph.92.7.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.