Abstract
Global climate change exacerbated by human energy use threatens to have a profound impact on human health, including from infectious diseases. Particularly vulnerable populations include the immunocompromised, including persons with HIV infection. Global warming can be expected to increase the geographic range of pathogens such as Vibrio cholerae as well as vectors that transmit disease, including ticks and mosquitoes. Higher temperatures also contribute to increased pathogen and vector efficiency in spreading disease. Natural disasters due to climate change result in population displacement, in creased population density, and living conditions conducive to the spread of infectious diseases. Political mobilization is crucial to implementing and enforcing policies for prudent energy use, reversing the drivers of global warming, and ensuring that we are prepared for the adverse health consequences of climate change. This article summarizes a presentation by Robert T. Schooley, MD, at the IAS-USA continuing education program held in Berkeley in May 2017.
Keywords: Global warming, climate change, natural disasters, infectious diseases, disease vectors, cholera, dengue, HIV
Climate change is occurring. The world is warming. Within the scientific community there is clear consensus that this warming reflects not just planetary cycles of warming and cooling that have been present since the earth was formed, but changes caused by human actions. Human energy use is the primary driver climate change, and directly reflects the product of the number of humans on the planet and how much energy each person uses per day.
An urgent question that must be faced is: How do these changes affect humans from the perspectives of general effects and of health effects, including infectious disease-related morbidity and mortality? Direct effects of climate change include accelerated weather extremes resulting in increased air pollution and more heat waves, and a greater number of more-fragile humans who are more susceptible to infectious diseases. Indirect effects include changes in biophysical systems such as rising oceans and melting glaciers. Such changes can result in deterioration of social and economic structures and conditions, including loss of property, loss of jobs, large-scale population displacement, and poorer nutrition and reduced availability of food on a global scale. Among the vulnerable groups of persons in the setting of climate change and its consequences are those with immunodeficiency, including those with HIV infection.
Infectious Disease and Climate Change
Climate change can influence risk of infectious diseases in variety of ways, including expansion of the ranges of pathogens and vectors (eg, ticks, mosquitoes), increases in pathogen or vector efficiency, and via the consequences of more frequent natural catastrophes (flood, drought, etc).
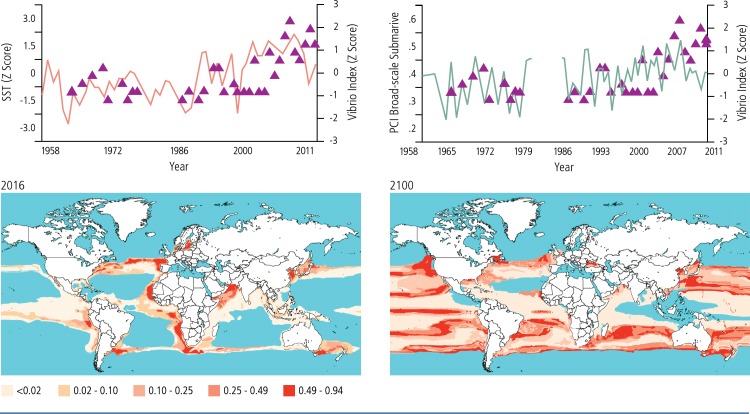
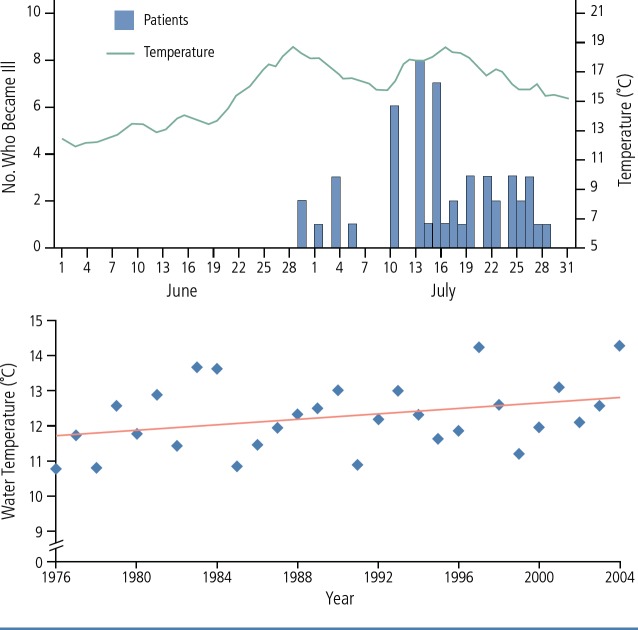
With regard to expansion of the range of pathogens, a prime example is the spread of Vibrio cholerae. V. cholerae, like many bacteria, grow better in warm water, high pH conditions, and where there is abundant chitin. Chitin is a product of plankton that flourish in the presence of nitrogen runoff into rivers. In rivers in India, for example, increased agriculture and fertilization of crops has resulted in increased levels of nitrogen in rivers, tidal estuaries, and ocean water, resulting in blooms of the blue green algae (phytoplankton) in which V. cholerae thrives.1 Figure 1 shows the increase in surface temperature and increase in phytoplankton and V. cholerae populations over time in the North Atlantic Ocean, and the increasing number of cholera outbreaks as this has occurred.2 Figure 1 also shows the alarming increase in seawater area capable of supporting V. cholerae that is projected to occur between 2016 and 2100.3 Outbreaks of gastroenteritis due to Vibrio parahaemolyticus in Alaskan oysters from Prince William Sound have also recently been documented.4 As shown in Figure 2, cases occurred as the daily water temperature in June 2004 rose to above 15°C. Figure 2 also shows the increase in mean water temperature that had occurred between 1976 and 2004.
Figure 1.
Top—Surface temperature and phytoplankton and Vibrio Index in the southern North Sea.2 Bottom—seawater area capable of supporting Vibrio cholerae in 2016 and according to projection for 2100.3
Figure 2.
Top—Surface water temperature at a Prince William Sound oyster farm and number of cases of Vibrio parahaemolyticus infection. Bottom—Mean daily water temperature in the Gulf of Alaska, 1976–2004.4
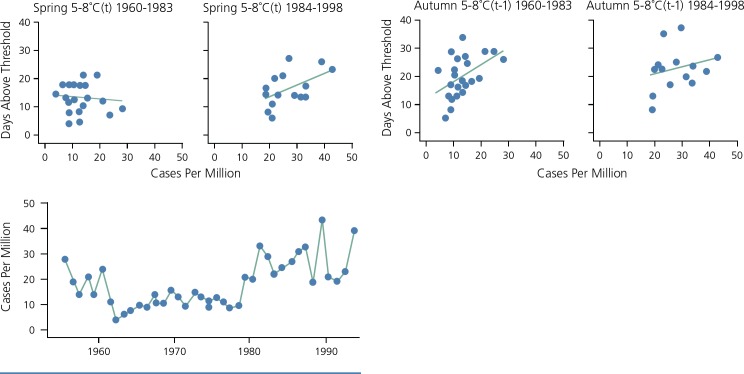
An example of effects of changes in vector ranges is the northward spread of tick-borne encephalitis that has been observed as Sweden has warmed. The ticks (Ixodes ricinus) are dormant in winter and emerge when night temperatures rise above 4°C to 5°C. As shown in Figure 3, the number of cases of tick-borne encephalitis has increased with an increasing number of spring nights that have exceeded the temperature threshold of 5°C to 8°C.5
Figure 3.
Relationship between spring and autumn temperatures and tick-borne encephalitis (TBE) in Sweden.5
Dengue is another disease projected to undergo dramatic geographic spread with warming. Amplification of dengue virus in Anopheles aegypti, the mosquito vector, occurs at temperatures above 18°C. At higher temperatures, the virus grows faster in the mosquito and allows the mosquito to become infectious earlier in its life cycle.6 Figure 4 shows reported outbreaks of dengue between 1970 and 1996, and projected areas at risk for dengue from 1990 to 2085.7 A similar distribution might be expected for Zika, chikungunya, and yellow fever viruses, as well as Plasmodium falciparum, because these pathogens are spread by similar vectors.
Figure 4.
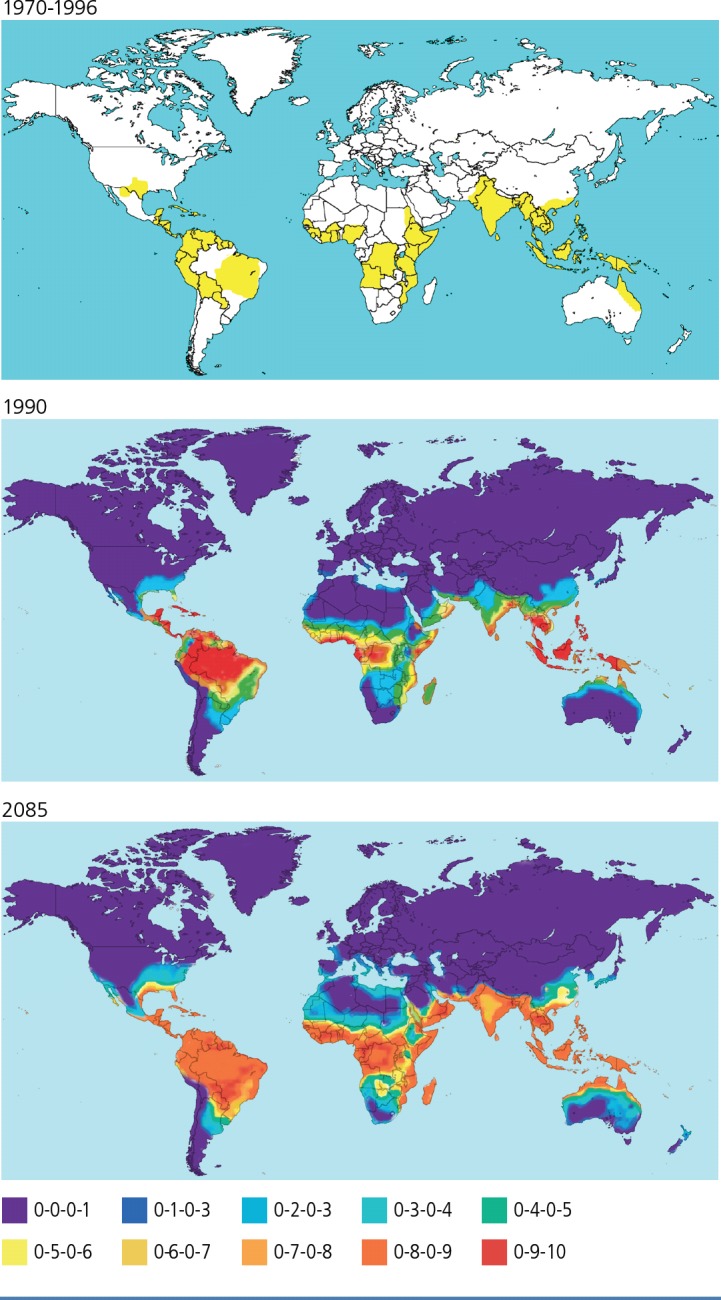
Top—Recorded outbreaks of dengue, 1970-1996. Bottom—Projected areas at risk for dengue, 1990–2085.7
Increased pathogen or vector efficiency comes along with warming, because higher temperatures are associated with increased pathogen and vector replication rates. Increased population density, whether due to the growth of the world's population or to displacement caused by natural catastrophes related to climate change, or otherwise, allows the more efficient spread of many diseases, particularly respiratory and vector-borne diseases.
Natural catastrophes, including those associated with climate change, have a profound impact on spread of infectious diseases. Natural catastrophes do not affect all populations equally; there are greater negative effects on persons at the extremes of age, those in less affluent circumstances that may include insufficient housing, those with less food security (including the homeless), and those with already compromised health, including immunocompromised populations. These conditions also increase vulnerability to infectious diseases.
In many locales in Africa, sustained drought has affected agrarian society, with many people driven from rural area to cities, such as Cape Town and Nairobi. There, many live in impoverished, crowded conditions much more conducive to transmission of infectious diseases than habitation in farming areas. Floods in Haiti, Mozambique, and elsewhere have resulted in dislocation of populations to shanty towns, refugee camps, and other assemblages that have been stricken by cholera and dengue, and are more permissive of spread of tuberculosis and HIV.
The following select list shows some of the infectious disease consequences of recent natural disasters:
-
Flooding
-
–Cholera and enterotoxigenic Escherichia coli: Bangladesh 1998 and 2004
-
–Salmonella enterica, Cryptosporidium parvum, and hepatitis A and E: Indonesia 1992, 2002, and 2004
-
–Norovirus, salmonella, V cholerae: Hurricane Katrina in US 2003
-
–Leptospirosis: Taiwan 2001, Brazil 1996, and Puerto Rico 2017 and 2018
-
–
-
Crowding
-
–Measles: Philippines after the Pinatubo eruption and Pakistan after the 2005 earthquake
-
–Meningitis: Pakistan after the 2005 earthquake
-
–Vector-borne diseases: Malaria in numerous locations after flooding and earthquakes
-
–
-
Others
-
–Tetanus and mucormycosis: following natural disasters and associated trauma in numerous locations
-
–Coccidiodomycosis: California following dust storms triggered by earthquake-driven landslides
-
–
Outbreaks of disease in the setting of climate change are multifactorial, as illustrated by the Zika virus outbreak in Brazil. The El Niño drove a drying and warming condition in northeastern Brazil, where Zika first appeared. Mosquitoes can flourish in these conditions, with the drying of rivers leaving standing pools of water in which mosquitos can more readily replicate. With the drying of the rivers, people began to bring water to their homes in buckets, also a perfect breeding ground for the vector mosquitoes. The public health awareness of outbreaks was low, as Zika virus disproportionately affected people in lower economic conditions. Pregnant women and immunocompromised persons were further disproportionately affected by the disease.
Combating Infectious Morbidity From Climate Change—What Can We Do?
What can we do about the climate changes caused by human energy use, and infectious morbidity related to these changes? Climate-independent interventions include epidemic surveillance and mobilization capacity at local and multinational levels; maintaining vaccination status; ensuring food security; reducing displacement; and prevention and treatment of HIV. Climate-specific interventions include gaining and disseminating knowledge about climate change and its effects; concerted and coordinated action in reversing the drivers of climate change; and political mobilization.
A productive way of looking at climate science is captured by Richard Levins and Richard Lewontin in The Dialectical Biologist, in which they state, “[t]he fact that the future might be like the past is what makes science possible, while the fact that the future might not be like the past is what makes science necessary.”8
The Trump administration's attitude toward climate science appears to be best summarized in a statement from Budget Director Mike Mulvaney: “We're not going to be spending money on that anymore.”9 Funding for the Environmental Protection Agency (EPA) was to be reduced by 31%, under the first budget proposal of this administration, with substantial cutbacks also being aimed at the National Oceanographic and Atmospheric Administration, National Science Foundation, President's Emergency Plan for AIDS Relief, United States Agency for International Development, and the National Institutes of Health. The Fogarty International Center was slated for elimination by Trump's first budget proposal, but was saved by congressional action. Career scientists have left the EPA in droves, leaving it with fewer employees than during the time of the Reagan administration. Such changes will have a profound impact on our ability to effect necessary changes in energy use, and our ability to prevent or respond to health consequences of climate change.
With regard to concerted and coordinated action, we must strive for more prudent energy use. This requires personal and federal actions. On a personal level, if each one of us uses less energy per day, less heat will be generated, and that is a good thing. However, a great challenge at the individual level and the national level is what is known as the Tragedy of the Commons. This was an English observation (William Foster Lloyd, 1833) regarding the depletion of the commons occurring because each of several farmers considered only their own cattle's use of the shared land for grazing. We must realize that global risk is shared and overcome the urge to ‘get our own piece while we can. Proactive steps must be put into place to deal with natural disasters and disease outbreaks. Through a lack of expertise and will, the administration's failure to reconstruct crucial infrastructure in Puerto Rico and the US Virgin Islands following Hurricanes Irma and Maria has left Americans living in these islands vulnerable to infectious diseases and morbidity from other causes. Proactive efforts to detect disease outbreaks and to anticipate natural disasters are critical responsibilites of competent government agencies.
Political mobilization in this area is crucial. Pressure must be brought to bear on such players as President Trump, Duke Energy, Koch Industries, Halliburton, ExxonMobil, Shell, EPA Director Scott Pruitt, and Secretary of State Mike Pompeo.
We who have been involved with HIV as patients, scientists, and healthcare professionals know how crucial research, practitioner, and especially patient mobilization has been to the enormous progress made in treating HIV. We practitioners have learned much from our patients in this regard. It is to be hoped that we all can come together with the same spirit and urgency to mobilize our society and our public servants to enact social and energy policies that may save us from some of the coming climate change.
For those wishing to learn more about climate change and health, the author recommends Climate Change and the Health of Nations: Famines, Fevers, and the Fate of Populations by Anthony J. McMichael with Alistair Woodward and Cameron Muir.10,11
Footnotes
Presented by Dr Schooley in May 2017. First draft prepared from transcripts by Matthew Stenger. Reviewed and edited by Dr Schooley in May 2018.
Financial affiliations in the past 12 months: Dr Schooley has served as a consultant to CytoDyn, Pfizer, and VIR. He has received grant support from Gilead Sciences, Inc, and holds stock or stock options in Antiva Biosciences and CytoDyn.
References
- 1. Chowdhury FR, Nur Z, Hassan N, von SL, Dunachie S. Pandemics, pathogenicity and changing molecular epidemiology of cholera in the era of global warming. Ann Clin Microbiol Antimicrob. 2017; 16(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vezzulli L, Grande C, Reid PC, et al. Climate influence on Vibrio and associated human diseases during the past half-century in the coastal North Atlantic. Proc Natl Acad Sci USA. 2016;113(34): E5062–E5071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Escobar LE, Ryan SJ, Stewart-Ibarra AM, et al. A global map of suitability for coastal Vibrio cholerae under current and future climate conditions. Acta Trop. 2015;149:202–211. [DOI] [PubMed] [Google Scholar]
- 4. McLaughlin JB, DePaola A, Bopp CA, et al. Outbreak of Vibrio parahaemolyticus gastroenteritis associated with Alaskan oysters. N Engl J Med. 2005;353(14):1463–1470. [DOI] [PubMed] [Google Scholar]
- 5. Lindgren E, Gustafson R. Tick-borne encephalitis in Sweden and climate change. Lancet. 2001;358(9275):16–18. [DOI] [PubMed] [Google Scholar]
- 6. Ramachandran VG, Roy P, Das S, Mogha NS, Bansal AK. Empirical model for estimating dengue incidence using temperature, rainfall, and relative humidity: a 19-year retrospective analysis in East Delhi. Epidemiol Health. 2016;38:e2016052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hales S, de WN, Maindonald J, Woodward A. Potential effect of population and climate changes on global distribution of dengue fever: an empirical model. Lancet. 2002;360(9336):830–834. [DOI] [PubMed] [Google Scholar]
- 8. Levins R, Lewontin R. The Dialectical Biologist. Cambridge, Massachusetts: Harvard University Press, 1987. [Google Scholar]
- 9. Greenfieldboyce N. Trump's Budget Slashes Climate Change Funding. NPR Morning Edition. March 16, 2017.
- 10. McMichael A. Climate Change and the Health of Nations: Famines, Fevers, and the Fate of Populations. Oxford, UK: Oxford University Press, 2017. [Google Scholar]
- 11. Polgreen PM, Polgreen EL. Infectious Diseases, Weather, and Climate. Clin Infect Dis. 2018;66(6):815–817. [DOI] [PubMed] [Google Scholar]