Abstract
Objective
Multiple studies have shown disparities in mortality after traumatic injury based on race and insurance status. It is unknown if injury severity affects these disparities.
Methods
Adults (ages 18–64) in the 2003–2008 National Trauma Data Bank were stratified into six groups based on race and insurance status. Patients with Injury Severity Score (ISS) ≥ 9 were included. Multivariable logistic regression compared the odds of death between the six race/insurance groups within different injury severity levels (ISS 9–15; ISS>15 & Systolic Blood Pressure (SBP)>90; ISS>15 & SBP<90). Age, gender, ISS, Glasgow Coma Scale motor, hypotension (SBP<90), and mechanism of injury were controlled for. Clustering was used to account for potential inter-facility survival differences and multiple imputation was employed to account for missing data.
Results
760,598 patients met inclusion criteria. Crude mortality for moderately injured was 0.75% for insured white patients and 1.52% (p<0.01) for uninsured blacks. Among hypotensive severely injured patients, the difference in mortality increased from 34.5% for insured whites compared to 58.9% for uninsured blacks (p<0.01). Adjusted analysis revealed increasing disparities between race/insurance groups as the injury worsened. The odds of death for uninsured black patients compared to insured whites of similar injury increases from 1.82 when moderately injured to 3.14 when severely injured and hypotensive, and for uninsured Hispanic patients it increases from 1.28 to 2.67.
Conclusions
Disparities in trauma mortality effecting minority and uninsured patients appear to worsen with increasing injury. Understanding why the most severely injured suffer from greater disparities may help us develop effective solutions to mitigate inequities.
Keywords: Healthcare disparities, injuries, insurance, race, trauma severity indices
Category: Shock, Sepsis, Trauma, Critical Care
Background
Trauma is a leading cause of death in the United States and worldwide. In the U.S., traumatic injury is the number one cause of death for people from the ages of one to 44, and is one of the top five causes of mortality overall.1
However, survival after similar traumatic injury is not equal among all patients. It has been shown that racial and ethnic minorities have worse outcomes after trauma.2,3 The odds of mortality with moderate to severe injury are significantly worse for both Black and Hispanic patients after controlling for important potential confounders such as age, injury severity, and mechanism of injury.4 Similarly, patients without insurance have also been found to have an increased risk of dying. It has been suggested that lack of insurance is more strongly associated with mortality than race alone.4 Looking at approximately 9,000 motor vehicle crash victims treated in state-designated trauma centers, Tepas et. al. demonstrated that being uninsured was significantly related to death within 24 hours of injury.5 Other studies have demonstrated that lack of health insurance increases a trauma patient’s adjusted odds of mortality by approximately 50% during their hospital stay,4 and up to two years post-injury.6
An important consideration in the analysis of these risk factors is the substantial interplay between race and insurance status. While only 11% of white, non-Hispanic U.S. citizens were uninsured in 2008, 19% of black and 31% of Hispanics were uninsured.7 Given the link between race/ethnicity and insurance coverage, it can be difficult to fully separate their individual effects on health outcomes.8 Therefore, it is important to assess the combined effect of race and insurance status when evaluating the increased risk of death these potentially vulnerable populations face.
Importance
Despite the awareness of the increased risks to uninsured and minority populations, we have not yet made substantive progress in reducing them. A major cause for this appears to be the lack of knowledge regarding the underlying mechanisms that drive these inequities. Without developing an understanding of exactly what is driving these inequities, we cannot create effective solutions to eliminate them.
A first step in the process of elucidating these factors is determining if there are certain populations within these groups most at risk. One factor that is well known to directly effect mortality risk is injury severity. It is expected that mortality increases as people are more severely injured. However, we do not yet know if this risk increases proportionally for patients of all races and insurance statuses. If vulnerable groups can be identified, and if the mechanisms behind race and insurance related disparities can be thus discovered, there exists the possibility of targeting policy interventions to reduce or eliminate them.
Goals
Our objective was to determine whether severity of injury affects disparities in in-hospital mortality related to race and insurance status. As mortality tends to increase with increasing injury severity, we hypothesize that disparities will become increasingly apparent among populations with worse injuries. Revealing the subset of individuals where the greatest disparities exist may help direct interventions at the groups most in need.
Methods
Study design and setting
This study was a retrospective analysis of six years of patients included in the merged National Trauma Data Banks (NTDB) between 2003–2008. The NTDB is maintained by the American College of Surgeons-Committee on Trauma and contains approximately 3 million records from 1051 participating trauma centers. The Johns Hopkins Hospital and Johns Hopkins School of Public Health Institutional Review Boards approved this study.
Population studied
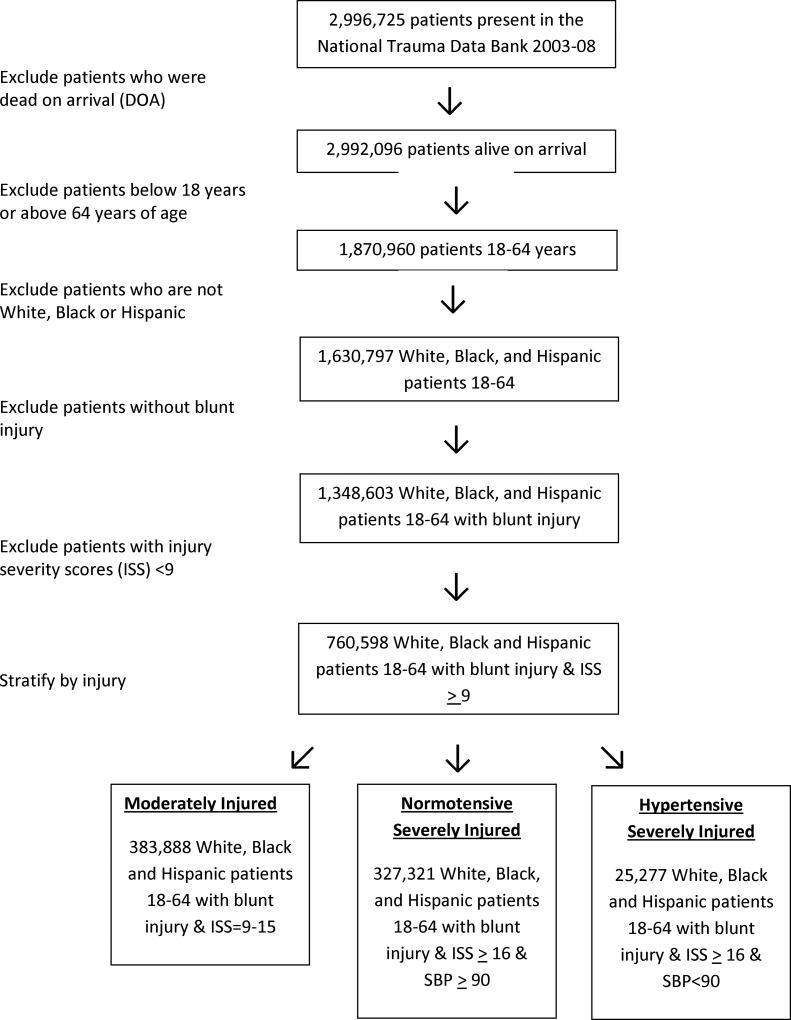
The population studied was comprised of trauma patients aged 18–64 years contained within the NTDB and suffering blunt injury and an Injury Severity Score (ISS) ≥ 9 on admission to the emergency department who were white, black or Hispanic were included. (Figure 1) As data reporting to the NTDB is voluntary and some institutions systematically do not submit patient insurance, patients from facilities that did not submit any data on insurance status were excluded. Patients with missing insurance data from facilities that did not systematically fail to report insurance data were included in the final analysis and their insurance data were imputed (see below). Those patients who died on or prior to arrival in the Emergency Department were excluded due to difference in injury mechanism and comorbid disease prevalence.9,10 Pediatric patients were excluded due to differences in injury patterns, pathophysiology, and treatment needs.11 Patients of “other” race or ethnicities were excluded due to anticipated small cell size, as our primary covariate was categorical. Only patients with blunt injuries were included due to the known differences in mortality between blunt, penetrating, and burn injury mechanisms so that a more homogenous patient population could be analyzed.12,13
Figure 1.
Patient Inclusion Criteria
Primary data analysis
Demographic data on age, gender, and insurance status were assessed. Insurance status was classified as: insured (private/commercial insurance, public insurance (Medicaid) or other governmental insurance) or uninsured. After testing for and finding an interaction between race and insurance status, patients were stratified by race and insurance status into white insured, black insured, Hispanic insured, white uninsured, black uninsured, and Hispanic uninsured. Univariate analysis was undertaken using Pearson’s Chi squared test for categorical variables and student’s t test for continuous variables. Crude mortality rates were also calculated within each race/insurance strata for the different injury levels.
Multivariable logistical regression was employed to compare adjusted odds of in-hospital mortality for the six race/insurance groups with white insured patients as the reference. The multivariate model controlled for patient level characteristics known to predict mortality after trauma including: age, gender, injury severity score (ISS), Glasgow Coma Scale motor score (GCS-M),14 presence of hypotension (systolic blood pressure <90) on arrival to the Emergency Department,15 year of admission, and mechanism of injury. To statistically account for inter-hospital variations in mortality, cluster-correlated robust estimate of variance that adjusted for within-hospital cluster correlation was used.16 In order to investigate potential differences in magnitude of disparities between different injury severity groups, patients were further stratified into three different degrees of injury; a moderately injured group consisting of patients with ISS 9–15 on presentation to the emergency department, a normotensive severely injured group with ISS>15 & systolic blood pressure (SBP)>90, and a hypotensive severely injured group with ISS>15 & SBP<90.
Given the importance of co-morbidity in predicting mortality outcomes, we performed a subset analysis focusing on younger patients aged 18–40 who are presumed to have few co-morbidities. Missing data has also been a concern in trauma injury analysis. In order to combat this, in all analyses we utilized multiple imputation, which has been shown to be a valid tool to account for missing values within the dataset.17 We imputed the following variables: death, insurance, race, type of injury, gender, and presence of hypotension, as they had the highest amount of missing data amongst variables considered for analysis. We imputed our dataset 5 times and specified initial values for our random number seeds in order to allow for reproducibility. We then compared the point estimates from our regression model from the imputed dataset to the point estimates from our original dataset. Statistical analyses were performed using Stata MP Statistical Software: Release 11, StataCorp, College Station, TX, 2009. Statistical significance was set at p <.05.
Results
There were no qualitative differences in regression output between the original and the imputed datasets (Supplemental Table 2), and we were therefore retained patients who were missing variables in the original dataset. The percentage of patients missing data for the following variables are shown in parentheses: death (2.5%), insurance (16%), race (6%), type of injury (1%), gender (1%), and presence of hypotension (5.5%). There were 2,996,725 patient cases collected into the NTDB from the years 2003–2008. Of these, 1,673,707 were between the ages of 18–64 and either white, black, or Hispanic. The final analysis was limited to 760,598 patients with ISS ≥ 9 and blunt injuries only. (Figure 1) The study population was 71% men, 15% black, 11% Hispanic, and 18% uninsured. The overall median age was 39 years, although uninsured and minority patients were younger (Table 1).
Table 1.
Baseline Characteristics by Race/Insurance Group. P-values represent Chi-square comparisons of proportions between race/insurance groups (H0: there are no differences in proportions between groups).
| White Insured |
Black Insured |
Hispanic Insured |
White Uninsured |
Black Uninsured |
Hispanic Uninsured |
P value | |
|---|---|---|---|---|---|---|---|
| Male (%) | 246,020 (68.3) | 40,989 (68.4) | 34,449 (77.5) | 65,690 (75.8) | 20,542 (79.4) | 22,026 (83.6) | <0.001 |
| Median Age in years (IQR) | 42 (27–52) | 39 (27–49) | 33 (24–45) | 36 (25–46) | 36 (26–46) | 30 (23–41) | <0.001 |
| ISS (%) | |||||||
| 9 to 15 | 185135 (51.4) | 29,218 (48.7) | 22,279 (50.1) | 43,043 (49.7) | 12,729 (49.2) | 13,605 (51.7) | <0.001 |
| 16 to 24 | 86,236 (23.9) | 12,915 (21.5) | 10,783 (24.3) | 20,715 (23.9) | 5,439 (21.0) | 6,281 (23.8) | |
| >24 | 162,870 (17.5) | 9,507 (15.9) | 8,733 (18.9) | 14,564 (16.8) | 3,852 (14.9) | 4,313 (16.4) | |
| SBP < 90 (%) | 14,423 (4.0) | 2,491 (4.1) | 2,068 (4.7) | 4,186 (4.8) | 1,342 (5.2) | 1,168 (4.4) | <0.001 |
| Mechanism of Injury (%) | |||||||
| Motor Vehicle Traffic | 193,660 (53.8) | 35,576 (59.3) | 25,733 (57.9) | 47,044 (54.3) | 14,313 (55.3) | 14,880 (56.5) | <0.001 |
| Cyclist | 6,136 (1.7) | 409 (0.7) | 389 (0.9) | 1,352 (1.5) | 228 (0.9) | 275 (1.0) | |
| Pedestrian | 1,356 (0.4) | 290 (0.5) | 205 (0.5) | 453 (0.5) | 143 (0.5) | 148 (0.6) | |
| Fall | 88,595 (24.6) | 10,754 (17.9) | 9,483 (21.3) | 17,076 (19.7) | 3,748 (14.5) | 5,148 (19.5) | |
| Struck by/against | 20,425 (5.7) | 6,916 (11.5) | 3,754 (8.4) | 8,297 (9.6) | 4,610 (17.8) | 3,218 (12.2) | |
| Deaths (%) | 14, 601 (4.1) | 2,676 (4.5) | 2,409 (5.4) | 5,107 (5.9) | 1,706 (6.6) | 1,574 (6.0) | <0.001 |
SBP = systolic blood pressure on ED presentation. ISS=Injury Severity Score.
Crude mortality for all injury levels ranged from 4.1% for white insured patients, to 6.6% and 6.0% for uninsured black and Hispanic patients. The race/insurance composition was comparable across the three injury levels, with 44–48% white insured patients in each category. There were slightly more uninsured and minority patients who were the most severely injured: moderately injured 11.2% white uninsured, 3.3% black uninsured, 3.5% Hispanic uninsured vs. hypotensive severely injured 13.4% white uninsured, 4.0% black uninsured, 3.7% Hispanic uninsured (p <0.001).
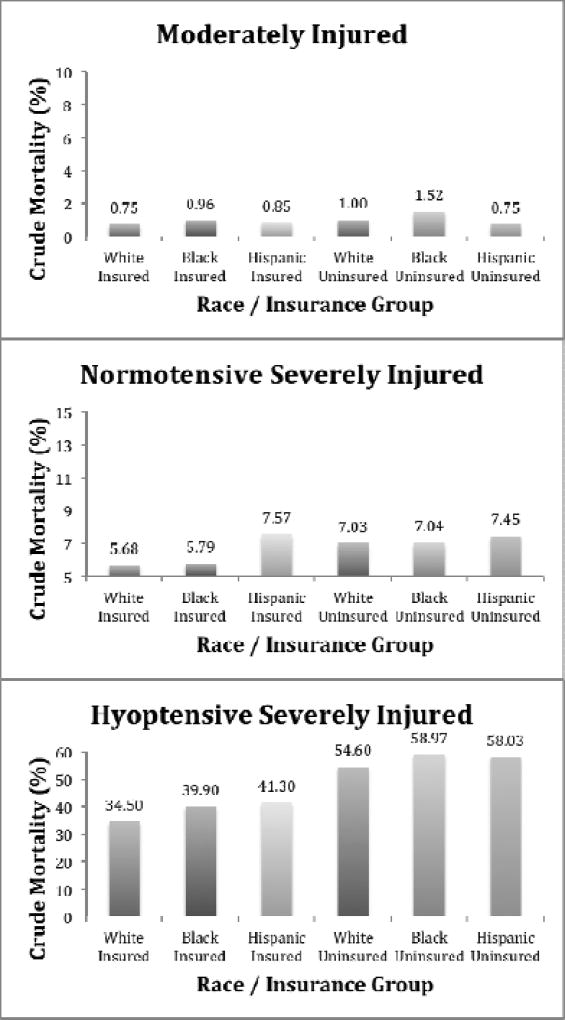
Unadjusted mortality had a 6-fold difference between injury levels, and the difference between the race/insurance groups also enlarged dramatically as the severity of the injury increased (Figure 2).
Figure 2.
Crude Mortality By Race and Insurance for Injury Levels
Adjusted analysis also revealed a greater difference in mortality disparities between race/insurance groups as the degree of injury worsened (Table 2). Among moderately injured patients, the odds of death were significantly higher for black patients and white uninsured patients, but no statistically significant difference in mortality was found between Hispanic and white patients. However, for normotensive severely injured patients, odds of death for all uninsured and minority patients were significantly higher than for the insured white reference group. These disparities were even greater for severely injured patients who presented with hypotension.
Table 2.
Adjusted Odds of Death for Race/Insurance Groups Stratified by Injury Level. Regression adjusts for age, Gender, GCS motor score, Injury Severity Score (ISS), Systolic Blood Pressure (SBP), mechanism of injury, year of admission, and inter-facility differences.
| White Insured |
Black Insured |
Hispanic Insured |
White Uninsured |
Black Uninsured |
Hispanic Uninsured |
|
|---|---|---|---|---|---|---|
| Moderately Injured (ISS=9–15) | ||||||
| 1 (ref) | 1.26* (1.05–1.50) | 1.21 (0.83–1.75) | 1.72* (1.30–2.27) | 1.82* (1.45–2.28) | 1.28 (0.91–1.80) | |
| Normotensive Severely Injured (ISS ≥16 & SBP≥90) | ||||||
| 1 (ref) | 1.33* (1.19–1.47) | 1.41* (1.17–1.72) | 1.70* (1.50–1.92) | 2.10* (1.87–2.36) | 1.64* (1.37–1.95) | |
| Hypotensive Severely Injured (ISS ≥16 & SBP<90) | ||||||
| 1 (ref) | 1.53* (1.30–1.81) | 1.56* (1.29–1.90) | 2.15* (1.86–2.49) | 3.14* (2.23–4.42) | 2.67* (2.09–3.40) | |
Significant differences, p<0.05, are denoted by *.
The sensitivity analysis that was performed on patients under the age of 40 also revealed an increase in the odds of death for higher injury levels (Supplemental Table 1).
Discussion
This study demonstrates that disparities in trauma mortality affecting uninsured and minority patients when compared with non-minority and insured patients increase as severity increases. A severely injured, uninsured black patient in this study was 3.2 times more likely to die than a similarly injured insured white patient. However, significant race/insurance-based inequities in survival were not found in moderately injured patients.
Several previous studies have demonstrated race and insurance based disparities in trauma outcomes;2–6 however, the causal factors that drive these disparities, and the populations and subpopulations at highest risk, are still largely unknown. This study found that among trauma victims, the patients most affected by disparities are those that suffer the most severe injuries. In order to better understand the mechanisms driving these disparities, it is important to examine which factors would potentially create differences in outcomes for severely injured patients that would not exist, or exist to a lesser extent, for only moderately injured people.
As injury severity increases, immediate, effective and intensive medical management become increasingly important. One potential driver of disparities between uninsured/minority and insured/non-minority patients may be that they are unable to access the increased level of care required to treat severe injuries. More specifically, uninsured /minority patients may experience differences in the timeliness of and appropriate delivery of emergent life-saving procedures. Black patients have been shown to have longer emergency department wait times than white patients,18 and are less likely to obtain a CT scan for headache.19 There is evidence to suggest that uninsured trauma patients are more likely to be transferred to another hospital, resulting in a delay in treatment.20–23 White and colleagues reported that uninsured patients who present with equally high acuity are less likely to receive radiographic imaging than insured patients.24 Weitzman et. al showed that black patients with chest pain are half as likely to receive thrombolysis for myocardial infarction.25 Further, Cuthbert et. al reported that ethnic minorities are more likely to be discharged directly home after moderate to severe traumatic brain injury.26 It is possible that these or other subtle differences in care may matter more for severely injured patients, who are in greater need of their timely provision. Unfortunately, due to the retrospective nature of this study, we were limited to the variables contained within the dataset and were not able to further evaluate these potential causes within this study. Further research is needed in order to assess in detail the contribution of these factors.
Another potential contributing factor to the worsening gap in mortality between insured or non-minority patients and uninsured or minority patients may be that the latter present predominately to hospitals that lack sufficient resources to handle severely injured patients. It has been shown that hospitals serving predominantly minority patients have worse outcomes after trauma.27 However, there is varying data concerning the quality of care provided by hospitals caring predominately for the underserved in the U.S. Safety net hospitals have been shown to have equivocal outcomes to non-safety net hospitals, for both traumatic28 and non-traumatic care.29 Part of this uncertainty may be due to differing definitions in what qualifies as a safety net hospital. McHugh et. al showed that varying definitions of safety net hospitals capture different hospitals and consequently show distinctive relative outcomes.30 None of these definitions of safety net hospitals reviewed by the authors were based on serving a majority of ethnic or racial minorities, and none looked at the breakdown of severe versus moderate injury. It is possible that safety net hospitals that specifically care for minority populations do not have the resources to care for severely injured patients, even though their outcomes for moderately injured patients may be equivocal to other hospitals. More work is needed to understand how patient populations truly differ between safety net hospitals and the quality and extent of care that is provided at hospitals serving these populations.
Another important explanation to consider is whether having health insurance lowers baseline health, creating poorer physiologic reserves that are unable to withstand severe injury. This is especially important to consider given that insurance status appears to be an even greater predictor of mortality than even race.4 However, given the relatively young median age, especially in the uninsured minority populations, this is unlikely to be the sole contributing factor. Additionally, the subset analysis performed on patients under the age of 40, who are unlikely to have many co-morbidities, shows an even greater disparity between insured or non-minority patients and uninsured or minority patients amongst severely injured patients.
There are several threats to the internal validity of this study based on our study design and available data. First, this study is retrospective and cross-sectional and therefore cannot be used to demonstrate causality, but rather to highlight associations of interest. Further studies should investigate the effects of injury severity on disparities after trauma in a prospective fashion. One limitation of the NTDB is that data reporting is voluntary and certain data are not consistently reported. In order to address this issue, we were able to impute missing data for several variables. Reassuringly, the analysis of the original, non-imputed dataset was reliably consistent with the imputed analysis.17 However, the substantial inconsistency in reporting of the comorbid conditions within the NTDB precluded analysis of the effects of comorbidity as a potential confounder. In an attempt to address this limitation, we did perform a subset analysis of patients aged 18–40 years in whom the prevalence of comorbid conditions and the consequences of those comorbid conditions should be much less. This method has been carried out in several other studies throughout the trauma literature.28,31 This examination was reassuring, as it demonstrated no qualitative differences between the age-restricted analysis and that carried out on the entire study population. While we attempted to address these known confounders, there are likely other confounding variables that are unmeasured or unknown that may have biased our results.
This study focused on the adult trauma populations. Additional studies are needed to investigate the association between injury severity and disparities at the extremes of age. Although it has been shown that insurance coverage is a strong predictor of outcomes for patients suffering both blunt and penetrating injury,32 this study analyzed only patients with blunt injuries. The results of this study revealed thus may not be generalizable to patients with other mechanisms of injury such as penetrating injuries and burns. Additional studies are needed to elucidate the relationship between trauma disparities and injury severity for these groups.
Uninsured minority patients suffer higher odds of death than insured and white patients after a similar injury. The results of this study revealed this disparity to be the greatest among those patients who have the most severe injuries and are most likely to die. Understanding insurance and race dependent differences is an essential step toward eliminating health care disparities. The exact mechanisms that lead to the observed higher mortality rates need further investigation. Potential contributors, such as differences in timeliness and appropriateness of emergent care, quality of care in hospitals that treat uninsured and minority patients, pre-hospital care, time to operation, co-morbidities, impact of income level and other disparities that may also impact survival, warrant careful scrutiny. Understanding the underlying cause of the disparities will permit the creation of programs and policies to close the gap between patients of different races and insurance statuses.
Supplementary Material
Footnotes
Accepted for a ten minute oral presentation at the 2012 Association for Academic Surgery conference held in Las Vegas, Nevada and was considered for the medical student award.
References
- 1.National Center for Health Statistics. Deaths: Leading causes for 2007. (DHHS Pub. no. [PHS] 2011–1250.) Hyattsville, MD: U.S. Public Health Service; 2011. [Google Scholar]
- 2.Haider AH, Efron DT, Haut ER, et al. Black children experience worse clinical and functional outcomes after traumatic brain injury: an analysis of the National Pediatric Trauma Registry. J Trauma. 2007 May;62(5):1259–62. doi: 10.1097/TA.0b013e31803c760e. discussion 1262–3. [DOI] [PubMed] [Google Scholar]
- 3.Shafi S, de la Plata CM, Diaz-Arrastia R, et al. Ethnic disparities exist in trauma care. J Trauma. 2007 Nov;63(5):1138–42. doi: 10.1097/TA.0b013e3181568cd4. [DOI] [PubMed] [Google Scholar]
- 4.Haider AH, Chang DC, Efron DT, et al. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008 Oct;143(10):945–9. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 5.Tepas JJ, 3rd, Pracht EE, Orban BL, et al. Insurance status, not race, is a determinant of outcomes from vehicular injury. J Am Coll Surg. 2011 Apr;212(4):722,7. doi: 10.1016/j.jamcollsurg.2010.12.016. discussion 727–9. [DOI] [PubMed] [Google Scholar]
- 6.Zarzaur BL, Stair BR, Magnotti LJ, et al. Insurance type is a determinant of 2-year mortality after non-neurologic trauma. J Surg Res. 2010 May;160(2):196–201. doi: 10.1016/j.jss.2009.06.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.U.S. Census Bureau. Income, Poverty, and Health Insurance Coverage in the United States: 2008. (Current population reports P60–236) Washington, DC: US Government Printing Office; 2009. [Google Scholar]
- 8.Fiscella K, Franks P, Gold MR, et al. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000 May;283(19):2579–84. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- 9.McMahon DJ, Schwab CW, Kauder D. Comorbidity and the elderly trauma patient. World J Surg. 1996 Oct;20(8):1113,9. doi: 10.1007/s002689900170. discussion 1119–20. [DOI] [PubMed] [Google Scholar]
- 10.Perdue PW, Watts DD, Kaufmann CR, et al. Differences in mortality between elderly and younger adult trauma patients: geriatric status increases risk of delayed death. J Trauma. 1998 Oct;45(4):805–10. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- 11.Kissoon N, Dreyer J, Walia M. Pediatric trauma: differences in pathophysiology, injury patterns and treatment compared with adult trauma. CMAJ. 1990 Jan;142(1):27–34. [PMC free article] [PubMed] [Google Scholar]
- 12.Santaniello JM, Luchette FA, Esposito TJ, et al. Ten year experience of burn, trauma, and combined burn/trauma injuries comparing outcomes. J Trauma. 2004 Oct;57(4):696,700. doi: 10.1097/01.ta.0000140480.50079.a8. dicussion 700–1. [DOI] [PubMed] [Google Scholar]
- 13.Haider AH, Chang DC, Haut ER, et al. Mechanism of injury predicts patient mortality and impairment after blunt trauma. J Surg Res. 2009 May;153(1):138–42. doi: 10.1016/j.jss.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 14.Al-Salamah MA, McDowell I, Stiell IG, et al. Initial emergency department trauma scores from the OPALS study: the case for the motor score in blunt trauma. Acad Emerg Med. 2004 Aug;11(8):834–42. doi: 10.1111/j.1553-2712.2004.tb00764.x. [DOI] [PubMed] [Google Scholar]
- 15.Oyetunji T, Crompton JG, Efron DT, et al. Simplifying physiologic injury severity measurement for predicting trauma outcomes. J Surg Res. 2010 Apr;159(2):627–32. doi: 10.1016/j.jss.2009.08.026. [DOI] [PubMed] [Google Scholar]
- 16.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000 Jun;56(2):645–6. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 17.Oyetunji TA, Crompton JG, Ehanire ID, et al. Multiple imputation in trauma disparity research. J Surg Res. 2011 Jan;165(1):e37–41. doi: 10.1016/j.jss.2010.09.025. [DOI] [PubMed] [Google Scholar]
- 18.Karve SJ, Balkrishnan R, Mohammad YM, et al. Racial/ethnic disparities in emergency department waiting time for stroke patients in the United States. J Stroke Cerebrovasc Dis. 2011 Jan-Feb;20(1):30–40. doi: 10.1016/j.jstrokecerebrovasdis.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 19.Harris B, Hwang U, Lee WS, et al. Disparities in use of computed tomography for patients presenting with headache. Am J Emerg Med. 2009 Mar;27(3):333–6. doi: 10.1016/j.ajem.2008.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosen H, Saleh F, Lipsitz SR, et al. Lack of insurance negatively affects trauma mortality in US children. J Pediatr Surg. 2009 Oct;44(10):1952–7. doi: 10.1016/j.jpedsurg.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 21.Rosen H, Saleh F, Lipsitz S, et al. Downwardly mobile: the accidental cost of being uninsured. Arch Surg. 2009 Nov;144(11):1006–11. doi: 10.1001/archsurg.2009.195. [DOI] [PubMed] [Google Scholar]
- 22.Sabharwal S, Zhao C, McClemens E, et al. Pediatric orthopaedic patients presenting to a university emergency department after visiting another emergency department: demographics and health insurance status. J Pediatr Orthop. 2007 Sep;27(6):690–4. doi: 10.1097/BPO.0b013e3181425653. [DOI] [PubMed] [Google Scholar]
- 23.Koval KJ, Tingey CW, Spratt KF. Are patients being transferred to level-I trauma centers for reasons other than medical necessity? J Bone Joint Surg Am. 2006 Oct;88(10):2124–32. doi: 10.2106/JBJS.F.00245. [DOI] [PubMed] [Google Scholar]
- 24.White FA, French DLZF, Jr, et al. Care without coverage: is there a relationship between insurance and ED care? J Emerg Med. 2007 Feb;32(2):159–65. doi: 10.1016/j.jemermed.2006.05.043. [DOI] [PubMed] [Google Scholar]
- 25.Weitzman S, Cooper L, Chambless L, et al. Gender, racial, and geographic differences in the performance of cardiac diagnostic and therapeutic procedures for hospitalized acute myocardial infarction in four states. Am J Cardiol. 1997 Mar;79(6):722–6. doi: 10.1016/s0002-9149(96)00857-0. [DOI] [PubMed] [Google Scholar]
- 26.Cuthbert JP, Corrigan JD, Harrison-Felix C, et al. Factors that predict acute hospitalization discharge disposition for adults with moderate to severe traumatic brain injury. Arch Phys Med Rehabil. 2011 May;92(5):721–730 e3. doi: 10.1016/j.apmr.2010.12.023. [DOI] [PubMed] [Google Scholar]
- 27.Haider AH, Ong'uti S, Efron DT, et al. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: a nationwide analysis of 434 hospitals. Arch Surg. 2012 Jan;147(1):63–70. doi: 10.1001/archsurg.2011.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vettukattil AS, Haider AH, Haut ER, et al. Do trauma safety-net hospitals deliver truly safe trauma care? A multilevel analysis of the national trauma data bank. J Trauma. 2011 Apr;70(4):978–84. doi: 10.1097/TA.0b013e31820b5d0c. [DOI] [PubMed] [Google Scholar]
- 29.Eisert SL, Mehler PS, Gabow PA. Can America's urban safety net systems be a solution to unequal treatment? J Urban Health. 2008 Sep;85(5):766–78. doi: 10.1007/s11524-008-9296-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McHugh M, Kang R, Hasnain-Wynia R. Understanding the safety net: inpatient quality of care varies based on how one defines safety-net hospitals. Med Care Res Rev. 2009 Oct;66(5):590–605. doi: 10.1177/1077558709334895. [DOI] [PubMed] [Google Scholar]
- 31.Weygandt PL, Losonczy LI, Schneider EB, et al. Disparities in mortality after blunt injury: Does insurance type matter? J Surg Res. 2012 Oct;177(2):288–294. doi: 10.1016/j.jss.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greene WR, Oyetunji TA, Bowers U, et al. Insurance status is a potent predictor of outcomes in both blunt and penetrating trauma. Am J Surg. 2010 Apr;199(4):554–7. doi: 10.1016/j.amjsurg.2009.11.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.