Abstract
Background
One of the factors that determine success of an epidural anaesthetic is correctly locating the epidural space. Being able to predict the skin to lumbar epidural space distance can serve as a guide to performing epidural anaesthesia and in turn increase the success rate.
Aim
To determine the correlation between the BMI, gender and age on SLESD of adults scheduled for elective surgical procedure under lumbar epidural anaesthesia.
Design of Study
It was across sectional descriptive study carried out on consenting patients scheduled for elective surgery under lumbar epidural anaesthesia.
Setting
The study was carried out in the main theatre complex and the obstetric theatre of the University of Ilorin Teaching Hospital, Ilorin, Nigeria.
Methodology
One hundred and twenty patients of ASAI and II physical status between the ages of18-65years scheduled for elective surgical procedures under epidural anaesthesia were enrolled into the study. This was a cross sectional descriptive study involving both sexes. Using a septic technique epidural anaesthesia was established in the sitting position using the midline approach at L3/L4orL4/L5 interspace. The epidural space was identified by loss of resistance to air. The
SLESD in centimetres (cm) was rounded up to the nearest 0.25cm. Data were collected and analyzed using Spearman´s correlation to evaluate the relationship between BMI, weight, sex, age, height and the SLESD.
Results
The mean SLESD was 4.60±0.83 cm with a range of 3cm-8cm. The SLESD was significantly influenced by BMI and weight with both having positive correlation and P value of 0.001 and 0.004 respectively. We formulated a relationship between skin to lumbar epidural space and body mass index based on linear regression analysis: Depth cm= a + b × (BMI)
Where a =3.33 and b =0.05.There was no correlation between SLESD and height, age or sex of the patients.
Conclusion
There was positive linear correlation between the body mass index, body weight and the skin to lumbar epidural space distance. Whereas, the age, sex and height had no correlation with the skin to lumbar epidural space distance.
Keywords: BMI, Epidural space, Distance, Correlation
Introduction
Lumbar epidural anaesthesia is a regional anaesthetic technique first described by Fidel Pages1 in 1921 . It is performed by injecting local anaesthetic agents into the epidural space. Epidural anaesthesia is particularly useful for lower abdominal and lower limbs surgeries. Several factors affect the success of epidural anaesthes ia even when it is being administered by skilled anaesthetists. One of such factors is obesity which makes it difficult to identify anatomical landmarks. Brummet et al2 showed that failure rates of epidural anaesthesia in normal patients was 5.1% and in the obese patients it was 7.7% while that of the morbidly obese was the highest at 11.7%.
Many studies have been performed to predict the distance from skin to lumbar epidural space (SLESD) in different populations3, 4 . This is because the knowledge of skin to epidural space distance (SLESD) may help in planning the procedure and may be an indicator of risk of success or failure of the procedure. Studies have shown that there has been an increase from skin to epidural space measured over the past three decades5,6,7. In the 1980s and 1990s the mean lumbar epidural space was 4.2-4.9cm. Recently Clinkscales et al7 in the United States of America reported mean skin to lumbar space distance (SLESD) of 5.3cm in Michigan paturients. Perhaps this gradual increment in skin to lumbar epidural space distance (SLESD) reflects increasing prevalence of obesity worldwide. Eastwood et al8 reported that there was an ethnic difference in body deposition of fat and that African Caribbean's living in London had more abdominal and lower body subcutaneous adipose tissues compared to the Europeans. A study conducted by Ilori and Djunda9 reported that Nigerian adults may have tendency to accumulate truncal subcutaneous adipose tissue which may influence skin to lumbar epidural space distance (SLESD).
The incidence of accidental dural puncture after an epidural approach ranges from 0.19% to 3.6%10. Once the accidental dural puncture occurs post dural puncture headache occurs in 50% of the patients with significant morbidity11 . Predicting the probable skin to epidural space distance (SLESD) in patients will guide insertion of epidural needle for epidural anaesthesia thus potentially reducing the rate of accidental dural puncture and its complications.
The objective of this study was to determine the correlation between the BMI, gender and age on skin to lumbar epidural space distance (SLESD) of adults scheduled for lumbar epidural anaesthesia in the University of Ilorin Teaching Hospital, Ilorin, Nigeria.
Patients & Methods
The study was conducted in the University of Teaching Hospital in North Central Nigeria. After
approval by the Hospital Ethics Committee, one hundred and twenty (120) patients with ASA I and II physical status between the ages of 18 -65 years scheduled for surgical procedures under epidural anaesthesia were enrolled. It was a cross sectional descriptive study involving both sexes. Sample size was calculated using the formula for a single sample mean12 n= d2 /e2 where d is the standard deviation of previous skin to lumbar epidural space distance (SLESD) which was 0.06 from a previous study in Nigeria9 and e is the desired size of the standard error 0.55%. Exclusion criteria included patients with lumbar spine deformities, patients who had allergy to bupivacaine, contraindications to epidural anaesthesia and patients with generalized oedema. Preoperative assessment was carried out on all patients the night before surgery. The patient's name, hospital number, sex, age, weight, height, body mass index (BMI) diagnosis and surgical procedure to be carried out were recorded on the study proforma. A detailed history and physical examination was done on all patients and their vital signs recorded. Patients were instructed to observe normal fasting guidelines. The procedure of the epidural anaesthesia was explained to all patients and written informed consent was obtained at the preoperative assessment.
In the operating suite patients were connected to a multi-parameter monitor (Dash 4000 by GE Medical Systems information Technology Inc. 8200w. Tower Ave Milwaukee USA, September 2007) and the baseline measurements of heart rate (HR), blood pressure (BP) which included(systolic, diastolic and mean arterial pressure), temperature, respiratory rate (RR), peripheral arterial oxygen saturation (SpO2) and electrocardiogram (ECG) were recorded. Intravenous access was secured with a size 16 gauge cannula either on the right or left forearm. The patients were placed in a sitting position on the edge of the operating table with the feet resting on a stool. The patients were positioned leaning forward hugging a pillow with neck flexed i.e. chin touching the chest. The skin of the back was prepared with povidone iodine and draped under aseptic precautions. The procedure for lumbar epidural injection was performed using a midline approach. The skin, subcutaneous tissue and interspinous space at L3/L4 or L4/L5 were infiltrated with 3mls of 2% plainlidocaine using a 25 gaugeneedleona 5ml syringe. Subsequently, an 18 gauge epidural needle (Baltonsp.zo .o. NovySwiat 7/14, 00-496Warszawa, Poland)with 1cmmarking was inserted gradually using a stylet to the ligamentum flavum after which the stylet was removed and a 10cc syringe containing air was attached to the needle and advanced gradually until the epidural space was identified by loss of resistance to air. The loss of resistance syringe was then removed and the skin to epidural space distance noted from the markings on the epidural needle. The skin to epidural space distance was determined by subtracting the length of the needle outside the skin from the whole length of the needle. The distance was then rounded up to the nearest 0.25cm as done in a previous study by Stamakis et al13 . The lumbar segment used and the SLESD were recorded in the study proforma
An epidural catheter was then threaded in slowly into the epidural space and about 3-5cm of the catheter was left in the epidural space. A test dose using 3mls of 2% lidocaine with adrenaline (1:200,000) was given in the epidural space to exclude subarachnoid and intravenous catheter placement. Subsequently, patients were managed according to the requirement of the surgical procedure. Drop out criteria was failure to identify the epidural space through the midline approach. Data were analyzed using SPSS (Version 20) software. Quantitative data were presented as mean ±SD. Spearman´s correlation coefficient (rs) was used to test the correlation between the skin to lumbar epidural space and patients height, sex, age, weight and body mass index . A p value of 0.05 was taken as being statistically significant.
Results
The general characteristic of the subjects are shown in Table 1. The means of age, weight andheight of subjects were 42.88±15.44 years, 70.47±11.19 kg and 1.62±0.07m respectively.Among the subjects involved in the study 34(28.3%) were males and 86(71.3%) werefemales. The mean skin to lumbar space distance in males was 4.50±0.82cm while thatof females was 4.63±0.83cm and was not
Table 3. Spearman’s correlation analysis between weight, age, height, number of attempts and BMI with skin to epidural distance.
| Variables | Correlation coefficient | p-value |
| BMI | 0.30 | 0.001* |
| Age | 0.04 | 0.680 |
| Sex | 0.08 | 0.416 |
| Weight | 0.30 | 0.001 |
| Height | -0.49 | 0.590 |
statistically significant p=0.449. The proportion of subjects with BMI<18.5, BMI 18.5-24.9 and BMI ≥ 25 were 4.2%, 31.7% and 64.2% respectively.Table 2: shows that the mean of skin to lumbar epidural distance in all subjects was 4.60±0.83cm with the mean skin to epidural space distances of subjects with BMI<18.5, 18.5-24.5 and ≥ 25 were 3.98±0.73cm, 4.43±0.84cm and 4.72±0.81cm respectively.
Table 1. General Characteristics.
| Variable | Number | Mean ± SD |
| Age (years) | 120 | 42.88±15.44 |
| Weight(Kg) | 120 | 70.47±11.19 |
| Height(m) | 120 | 1.62±0.07 |
| Sex | ||
| Male | 34(28.3%) | |
| Female | 86(71.3%) | |
| BMI | ||
| <18.5Kg/m2 | 5(4.2%) | 16.45±3.09 |
| 18.6-24.9Kg/m2 | 38(31.7%) | 23.17±1.52 |
| ≥25 Kg/m2 | 77(64.2%) | 29.60±3.64 |
Table 2. Skin to epidural distance based on BMI.
| BMI Classification | Mean ± SD | Range |
| <18.5Kg/m2 | 3.98± 0.73 | 3.00-5.00 |
| 18.6-24.9Kg/m2 | 4.43±0.84 | 3.00- 7.00 |
| ≥25 Kg/m2 | 4.72±0.81 | 3.50- 8.00 |
| Total | 4.60±0.83 | 3.00-8.00 |
| p- value =0.045 | ||
A significant difference in skin to lumbar epidural space distance based on BMI classification was observed in this study p=0.045. Multiple regression analysis showed that weight had the strongest relationship (r=0.30, p=0.000) with skin to lumbar epidural space distance when compared to BMI (r=0.27, p=0.001) and height (r=-0.12, p=0.450).
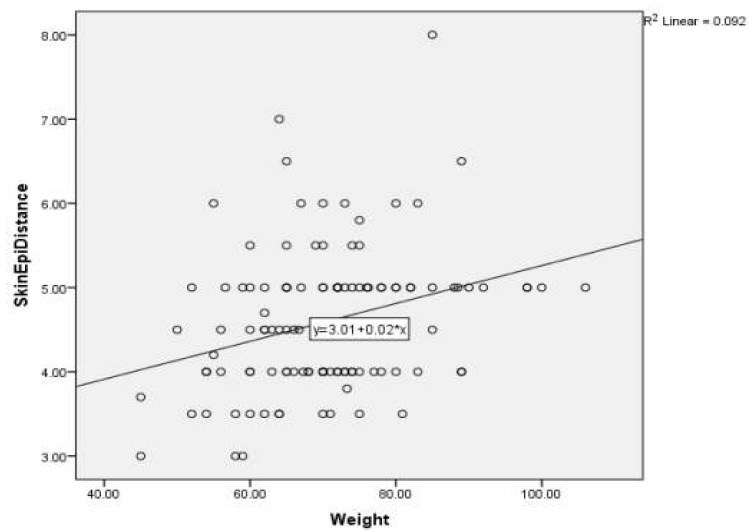
Table 3 , Fig. 1 and Fig. 2 shows that using Spearman´s correlation there is a positive correlation between skin to lumbar epidural space distance and BMI(rs=0.30, p=0.001), and also a positive correlation between SLESD and weight(rs=0.30, p=0.001). Height (rs=-0.49, p=0.597) however showed a negative correlation which implies that taller subjects had shorter skin to lumbar epidural space and was not statistically significant p=0.597. Age had no correlation (rs=0.04, p=0.680) and was not statistically significant p=0.680. There was no correlation between the numbers of attempts in locating the epidural space and BMI (rs=0.00, p=0.966).
Fig.1. Spearman’s correlation test between skin to epidural distance and BMI.
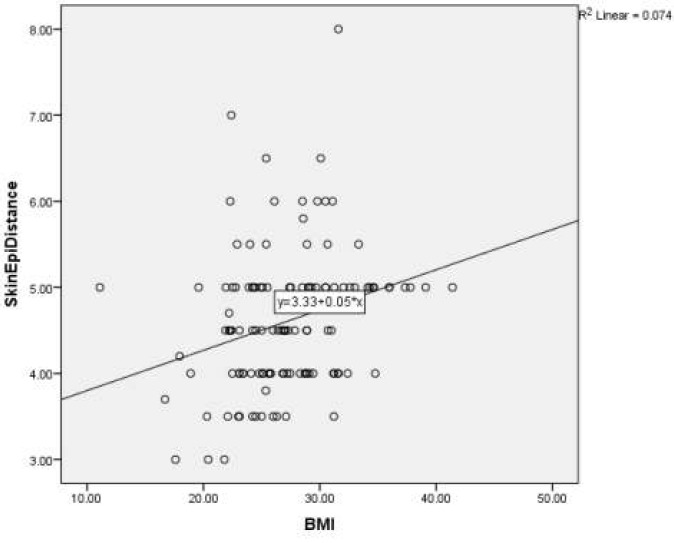
Fig.2. Spearman’s correlation test between skin to epidural distance and weight.
Discussion
The mean length from skin to lumbar epidural space in this study was 4.6±0.83cm with a range of 3-8cm.This is similar to that reported by Cha et al14 4.6±0.69 cm among Korean adults. However the result was different from that of Ilori and Djunda9 in a prospective study carried
out in Calabar, Nigeria where the mean skin tolumbar epidural space distance (SLESD) recorded was longer (5.29±0.06 cm) than what was found in this study. The reason for the variation in the skin to lumbar epidural space distance (SLESD) may be due to the fact that the studies were carried out in different regions of Nigeria, thus confirming the report by D´Alonzo and colleagues15 who stated that vertebral shape, and body composition and shape may be influenced by a person's ethnicity or race. Sharma et al16 in their study “effect of ethnicity on SLESD in paturients” also concluded that both ethnicity and BMI had significant influence on the skin to lumbar epidural space distance ( SLESD). In this study, patients with BMI <18.5, 18.5-24.5 and ≥ 25, the mean epidural space depth increased from 3.98±0.93 to 4.43± 0.84 and 4.72±0.81cm respectively. As the BMI increased, the depth in the epidural space increased and the difference was statistically significant p=0.045, this finding was similar to that reported by several authors2,9,17,18 . Sutton and Linter4 estimated that if the distance of skin to epidural space was less than 4cm it was associated with a threefold increase in accidental dural puncture therefore for patients with low BMI <18.5 there is an increased chance of accidental dural puncture. The mean distance of skin to lumbar epidural space distance (SLESD) of BMI <18.5 in this study was 3.98±0.93cm, thus knowledge of this may help reduce the rate of accidental dural puncture in patients that fall within this BMI group. Though a previous study4 suggested an increased risk of dural puncture amongst patients with low BMI, we had no incidence of dural puncture in our study. There is a positive correlation existing between skin to lumbarepidural space distance (SLESD) and BMI in this study (p = 0.001) which implies that with increasing BMI the skin to lumbar epidural space distance (SLESD) also increases. Several authors9,17,18 have also reported a good correlation between skin to lumbar epidural space distance (SLESD) and BMI. Using linear regression analysis we formulated a predictive equation of depth of lumbar epidural space in relation to the BMI to be depth cm =a+b× (BMI). Where ´a´ is the constant and equal to 3.33 and ´b´ is the regression coefficient and equal to 0.05. Therefore BMI could be a guideline for predicting the depth of epidural space during epidural anaesthesia. There was no correlation between BMI and the number of attempts in locating the lumbar epidural space. There was a positive correlation between weight and SLESD rs=0.30 with a p value of 0.001 which implies that with increase in weight the skin to lumbar epidural space distance ( SLESD) increases. This result is similar to that reported by Ilori and9 Djunda r=0.525, p=0.000 in Nigerian adults. Several authors have also reported a good correlation between skin to lumbar epidural space distance(SLESD) with weight and BMI9,17,18 .
The result of relationship between age and skin to lumbar epidural space distance (SLESD) has been conflicting. In our study there was no correlation between age and SLESD rs=0.038, 18 p=0.680. Komalijit et al also reported no relationship between age and the depth of epidural space. However Ilori and Djunda9 showed that age had a significant correlation with skin to lumbar epidural space distance (SLESD) in females r=0.407, p=0.001 but not in males. However Stamatakis et al3 in Greek population reported moderate correlation with longer skin to lumbar epidural space distance (SLESD) in males than females. In our study sex had no correlation with skin to lumbar epidural space distance (SLESD) which is similar to that reported by Komalijit et al18 .
Height had a negative correlation rs= -0.49 and was not statistically significant p=0.597 which is similar to that reported by Ilori and Djunda9 who also reported a negative correlation value of rs= -0.055 and a p value of 0.55 in Nigerian adults. This negative correlation means that in Nigerian adults, taller individuals had shorter skin to lumbar epidural space distance (SLESD)which is contrary to positive correlation documented by other authors13,19.
Limitations
It is possible that the Tuohy needles may have been placed lateral to the mid line or at an angle to the skin. Also, the study populations were largely of Yoruba ethnicity and may not be representative of the general population.
Conclusions
There was positive linear correlation between the body mass index, body weight and the skin to lumbar epidural space distance. Whereas, the age, sex and height had
no correlation with the skin to lumbar epidural space distance.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Grant support: None
References
- 1.Morgan GE. Practice of Anesthesiology. In: Morgan GE, Mikhail MS, Murray MJ, editors. Clinical Anesthesiology. 5th USA: McGraw-Hill; 2013. p. 3. [Google Scholar]
- 2.Brummet CM, William BS, Hurley RW, Erdek MA. A prospective observational study of the relationship between body mass index and depth of epidural space during lumbar transforaminal epidural steroid injection. Reg. Anesth Pain Med. 2009;34:100–105. doi: 10.1097/AAP.0b013e31819a12ba. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fakhe FE, Amjad I, Hana K, Mohammed T, Amir N, Ahmed A, Ihtisham U. The relationship of skin to epidural space depth with different physical parameters in obstetric patients. Pakistan Armed Forces Medical Journal. 2009;59:95–102. [Google Scholar]
- 4.Sutton DN, Linter SP. Depth of extradural space andduralpuncture. Anaesthesia. 1991;46:97–115. doi: 10.1111/j.1365-2044.1991.tb09348.x. [DOI] [PubMed] [Google Scholar]
- 5.Harrison GR, Clowes NW. The depth of lumber epidural space from skin. Anaesthesia. 1985;40:685–692. doi: 10.1111/j.1365-2044.1985.tb10953.x. [DOI] [PubMed] [Google Scholar]
- 6.Meiklejohn BH. Distance from skin to lumbar epidural space in obstetric population. Regional Anaesthesia. 1990;15:134–140. [PubMed] [Google Scholar]
- 7.Clinkscales CP, Greenfield MLVH, Vanarse M, Polley LS. An observational study of the relationship between lumbar epidural space depth and body mass index in Michigan paturients. International Journal of Obstetric Anaesthesia. 2007;16:323–330. doi: 10.1016/j.ijoa.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 8.Eastwood SV, Tillin T, Dehbi H, Wright A, Forouhi UG, Godsland I. Ethnic differences in associations between fat deposition and incident of diabetes and underlying mechanism: The SABRE study. Obesity. 2015;23(5):699–706. doi: 10.1002/oby.20997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ilori IU, Djunda EK. Influence of physical characteristic on skin to lumbar epidural space distance in Nigeria adults. British Journal of medicine and medical research. 2016;17(11):1–6. [Google Scholar]
- 10.Spirgge JD, Haper SJ. Accidental dural puncture and post dural puncture headache in obstetric anaesthesia: Presentation and Management: A 23 year survey in a district hospital. Anaesthesia. 2008;63:36–43. doi: 10.1111/j.1365-2044.2007.05285.x. [DOI] [PubMed] [Google Scholar]
- 11.Choi PT, Galmski SE, Takeuchi L, Stefen L, Tamayo C, Jadad AR. Post dural puncture headache is a common complication of neuraxial blockade in parturient. A meta-analysis of obstetrical studies. Can J Anaesth. 2003;50:460–469. doi: 10.1007/BF03021057. [DOI] [PubMed] [Google Scholar]
- 12.Basgul A, Hancy A, Korkmas F, Eksyoglu B. A clinical prediction of skin to lumbar epidural space distance in urologic surgery patients. Reg Anesth Pain Med. 2004:29–52. [Google Scholar]
- 13.Stamakis E, Moka E, Siafaka I, Argyra E, Vadalova A. Prediction of the distance from the skin to epidural space in the Greek population, using mathematical models. Pain Practice. 2005:5–7. doi: 10.1111/j.1533-2500.2005.05209.x. [DOI] [PubMed] [Google Scholar]
- 14.Cha SM, Jung VH, Kim DS, Park JS, Kang H, Baek CW. Distance from the lumbar epidural space to the skin in Korean adults. Anesth Pain Med. 2011;6(1):16–20. [Google Scholar]
- 15.D´Alonzo RC, White WD, Schult JR, Jakilsch PM, Hibib AS. Ethnicity and the distance to the epidural space in paturients. Reg Anesth Pain Med. . 2008;33(1):24–29. doi: 10.1016/j.rapm.2007.06.399. [DOI] [PubMed] [Google Scholar]
- 16.Sharma V, Swinson AK, Hughes C, Mokashi S, Russel K. Effect of ethnicity and body mass index on the distance from skin to lumbar epidural space in paturients. Anaesthesia. 2011;66:907–912. doi: 10.1111/j.1365-2044.2011.06812.x. [DOI] [PubMed] [Google Scholar]
- 17.Gurrici S, Hartriyanti Y, Hautvast JG, Deurenberg P. Differences in the relationship between body fat and body mass index between two different Indonesian ethnic group: The effect of body build. European Journal of clinical nutrition. 1999;53:468–540. doi: 10.1038/sj.ejcn.1600778. [DOI] [PubMed] [Google Scholar]
- 18.Komalyit KR, Tej KK, Suneet K, Shikha G, Sandeep K. Distance from skin to epidural space: correlation with body mass index. J Anaesth Clin Pharmacol. 2011;27(1):39–42. [PMC free article] [PubMed] [Google Scholar]
- 19.Agung S, Yusmein U, Sri R. The relationship between body mass index with distance of skin epidural space in 3rd and 4th lumbar epidural anesthesia in non-obstetric surgery of Indonesian patients. Journal of the Medical Sciences. 2012;44(1):75–71. [Google Scholar]


