Abstract
Stereotactic radiosurgery (SRS) is a treatment option, which is capable of pinpoint irradiation and thus, reduce the potential late complications. However, any type of radiation therapy is not recommended for brain tumor patients under the age of 3 years. SRS is not routinely recommended for patients than 2 years of age in consideration of infant skull brittleness for frame fixation, and lack of treatment evidence for the safety and effects of stereotactic radiosurgery in infants. We experienced the case of Gamma Knife treatment upon an infantile pineoblastoma where repeated tumor excision had already been perfromed and chemotherapy resistance was apparent. Radiosurgery resulted in symptom improvement and dramatic tumor shrinkage on MRI after radiosurgery. Therefore, here we report on the difficulty and usefulness of Gammaknife radiosurgery in this infant patient.
Keywords: Gamma Knife treatment, pineoblastoma, infant, dissemination, bevacizumab, general anesthesia
Introduction
Currently, radiotherapy is one of the mainstay treatment of many childhood cancers. However, for malignant brain tumor patients under the age of 3 years, still in the myelination period, it is recommended that such treatment is avoided where possible; due to their high susceptibility to radiation disorders such as intellectual development impairment. Yet there are many cases of malignant brain tumor where radical surgery or chemotherapy is not effective, and in which difficulty in retreatment upon potential recurrence is not uncommon. The current situation is such that no established standard treatment exists for cases of infant onset or repeated recurrence of malignant brain tumors. This necessitates that the treatment method vary depending on each case. One potential option is stereotactic radiosurgery (SRS), which is capable of pinpoint irradiation and expected to maximally reduce late complications. On the other hand, the role of SRS has not yet been clarified and there have been practically no reports on its use. One form of SRS treatment in particular, Gamma Knife treatment, was contraindicated in consideration of infant skull brittleness for frame fixation. However, as we experienced a case of Gamma Knife treatment on an infant, here we report on the treatment’s usefulness and the necessary procedure.
Case report
This case indicated an enlargement of the head around 3 months after birth, and a tumor was present in two areas (the right temporal region and the occipital region). By 7 months of age, 3 excisions had been performed and the tumor diagnosed as a pineoblastoma. In consideration of the patient’s age radiation therapy, such as craniospinal irradiation (CSI) and boost irradiation, was not performed and chemotherapy was administered repeatedly. Two months after removal, tumor growth was observed on the ventrolateral medulla side. Based on the site of the lesion, we judged that the risk of resection was high and so performed SRS treatment under general anesthesia, with the aim of controlling the tumor. As the tumor was of large volume and some parts were difficult to judge due to the weak contrast, at the point of 10 months of age, the tumor was irradiated only within the range which could be performed safely (PIV: 1.7cm3 received 14Gy to the 55% isodose line). However, when checked again 2 months later, an increase was observed which was considered to be residual tumor. Accordingly, the second course of radiotherapy was performed, with the exception of the area irradiated previously (PIV: 2.6 cm3 received 14 Gy to the 50% isodose line) (Fig. 1). Before irradiation, steroids were administered to relieve symptoms of tumor growth. However due to the occurrence of frequent apneic attacks starting from the day after irradiation took place, supplemental administration of bevacizumab 10 mg/kg was carried out from the second day after treatment. The apnea attacks disappeared one day later. After 1week of treatment, the baby was able to swallow milk and meal, and showed significant improvement and limb movement activity increased. 1 month after treatment MR imaging showed more dramatic tumor shrinkage and multiple administration of bevacizumab continued up to the current point (7 months after treatment) (Fig. 2).
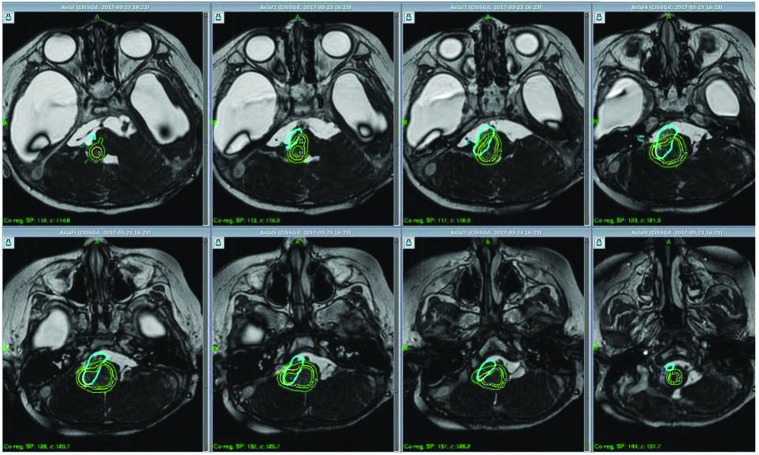
Figure 1.
The 14Gy50% isodose line (yellow line) was shown in a sequence of axial view for regrowth tumor; the prescription isodose volume was 2.6cc. The blue line shows previous irradiation area (PIV1.7cc, 14Gy55% isodose line). The 18Gy and 10Gy irradiation area were marked by the inner and external green line each.
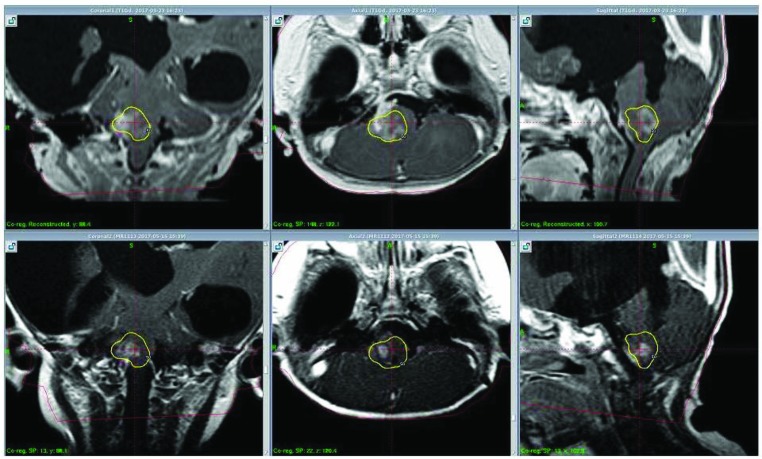
Figure 2.
Top:2nd treatment Bottom: Approximately 2 months after the 2nd treatment.
Discussion
Complete removal of pineoblastoma is often difficult due to the invasive nature of the tumor, and in the case of young patients, the high degree of dissemination (15) (5); making radiotherapy an indispensable treatment tool. However, for patients below the age of 3 who cannot be principally treated with CSI, there have been reports that following combination treatment of extraction and chemotherapy, average survival time after treatment is 0.9 years(8). According to the most convincing of recent reports in a survey of 299 pineoblastomas, the 5-year survival rate was 15% for patients under the age of 5 and 57% for those above; showing the difficulty of treating such a high risk group including infants (16). On the other hand, it has also been reported that by combining treatment with multi-modalities, a long-term prognosis can be expected regardless of age (5). This is thought to be so even in cases of STR from invasiveness and localization, where through combination with radiation therapy, the same survival rate as GTR can be obtained. It is therefore necessary to consider carefully each treatment policy according to each individual case (16). Although SRS has been reported as an effective alternative treatment for re-extraction/conventional irradiation of remaining lesions, there is still debate over various factors such as the timing of treatment and the actual irradiation dose (9) (13) (5) (12), necessitating reliable future reporting.
In our case, repeated tumor excision had already taken place and chemotherapy resistance was apparent. The lesions were located on the dorsal side of the brain stem and there was tumor infiltration of the cerebral parenchyma, direct surgery was considered to be of extremely high risk and so SRS was chosen as an alternative. A special frame auxiliary device was created to disperse and reduce the weight of the frame pins during treatment (Fig. 3). Additionally, although in this case the areas for potential pin fixation placement were limited due to multiple craniotomies, by using the frame auxiliary device the stability of the head was able to be secured at the time of pin fixation. This was also advantageous in that it allowed precise adjustments to take place before pin fixation. Our searches for treatment cases of patients less than 2 years of age returned only one by Witt et al. (17). In their case a male infant presenting with a malignant rhabdoid tumor was initially treated with chemotherapy for 6 months. At age 1 year and 2 months the infant underwent Gamma Knife treatment, with frame fixation using a pin fixation reinforcement tool known as ‘piers’.
Figure 3.
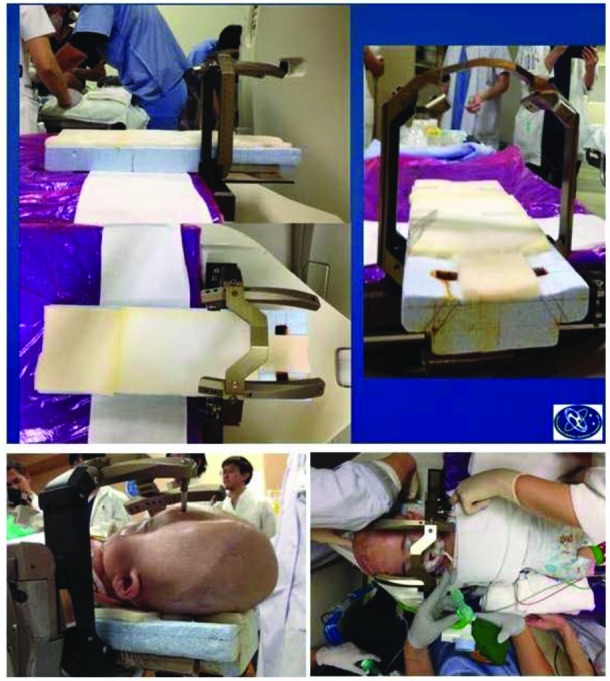
These pictures showing a special frame auxiliary device which was created to disperse and reduce the weight of the frame pins during treatment.
Another consideration was that there is no evidence for the safety and effects of stereotactic radiosurgery in infants. Therefore, agreement was obtained from the family for stereotactic radiotherapy to take place; as treatment methods for local control of lesions, such as surgery or chemotherapy, had been exhausted. In the treatment plan, the boundary of the tumor and its relationship to its surroundings was made clear using a 3D heavily T2 WI image and attempts made to reduce irradiation volume as much as possible (7). Effort was given to minimize the duration of anesthesia and acquisition of thin slide images as well as radiosurgery procedure. Discussion took place in advance concerning the risks of general anesthesia management relative to the expected irradiation time possible, calculated based on the preliminary simulation, and measures devised to increase treatment safety.
In our case, apneic attacks occurred frequently from the day after irradiation took place. Bevacizumab, an anti-VEGF antibody,in addition to steroids was administered on suspicion of acute radiation injury. One month after Gammaknife treatment, imaging study showed a remarkable reduction of the tumor, suggesting there had been synergistic effect in combination with the radiation therapy and bevacizumab although there are only few pediatric cases of bevacizumab use after radiotherapy (10) (6) (2). However, at present, due to the lack of clarity surrounding the appropriate usage, dose and duration for use, careful examination on a case by case basis is necessary (4) (11) (1) (14).
Currently, due to more widespread use of cone-beam CT (CBCT) and immobilization with mask fixation system, alternative irradiation methods to single dose radiation, such as IGRT and fractionated radiation may be possible for more aggressive intervention to intractable pediatric brain tumors, particularly for high risk groups. One of the reasons why SRS was chosen as an alternative to direct surgery in our case was to shorten the patient’s time under general anesthesia. Monitored anesthesia care is a method for appropriately controlling the level of sedation required, without necessarily requiring an airway being secured (3). In the future, we plan to introduce SRS application further for young children to ensure safety.
Acknowledgments
Authors’ disclosure of potential conflicts of interest
Dr. Hayashi reports grants, personal fees and non-financial support from ELEKTA during the conduct of the study; grants from EISAI, personal fees from Tokyo Kaijo Nichido, outside the submitted work. Drs. Aihara, Chiba, Horiba, Kawamata, and Tamura have nothing to disclose.
Author contributions
Conception and design: Ayako Horiba, Motohiro Hayashi
Data collection: Ayako Horiba, Noriko Tamura, Kentaro Chiba
Data analysis and interpretation: Ayako Horiba, Motohiro Hayashi, Yasuo Aihara
Manuscript writing: Ayako Horiba
Final approval of manuscript: Motohiro Hayashi, Takakazu Kawamata
References
- 1. Abrams DA, Hanson JA, Brown JM, Hsu FP, Delashaw JB, Bota DA. Timing of surgery and bevacizumab therapy in neurosurgical patients with recurrent high grade glioma. J Clin Neurosci. 2015;22(1):35–9. Epub 2014/12/04. doi: 10.1016/j.jocn.2014.05.054. PubMed PMID: 25481268. [DOI] [PubMed] [Google Scholar]
- 2. Benesch M, Windelberg M, Sauseng W, Witt V, Fleischhack G, Lackner H, et al. Compassionate use of bevacizumab (Avastin) in children and young adults with refractory or recurrent solid tumors. Ann Oncol. 2008;19(4):807–13. Epub 2007/12/03. doi: 10.1093/annonc/mdm510. PubMed PMID: 18056650. [DOI] [PubMed] [Google Scholar]
- 3. Das S, Ghosh S. Monitored anesthesia care: An overview. J Anaesthesiol Clin Pharmacol. 2015;31(1):27–9. doi: 10.4103/0970-9185.150525. PubMed PMID: 25788769; PubMed Central PMCID: PMCPMC4353148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Duan C, Perez-Torres CJ, Yuan L, Engelbach JA, Beeman SC, Tsien CI, et al. Can anti-vascular endothelial growth factor antibody reverse radiation necrosis? A preclinical investigation. J Neurooncol. 2017. Epub 2017/04/19. doi: 10.1007/s11060-017-2410-3. PubMed PMID: 28425047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Farnia B, Allen PK, Brown PD, Khatua S, Levine NB, Li J, et al. Clinical outcomes and patterns of failure in pineoblastoma: a 30-year, single-institution retrospective review. World Neurosurg. 2014;82(6):1232–41. Epub 2014/07/18. doi: 10.1016/j.wneu.2014.07.010. PubMed PMID: 25045788. [DOI] [PubMed] [Google Scholar]
- 6. Glade Bender JL, Adamson PC, Reid JM, Xu L, Baruchel S, Shaked Y, et al. Phase I trial and pharmacokinetic study of bevacizumab in pediatric patients with refractory solid tumors: A Children’s Oncology Group Study. J Clin Oncol. 2008;26(3):399–405. doi: 10.1200/JCO.2007.11.9230. PubMed PMID: 18202416. [DOI] [PubMed] [Google Scholar]
- 7. Hayashi M, Chernov MF, Tamura N, Yomo S, Tamura M, Horiba A, et al. Usefulness of the advanced neuroimaging protocol based on plain and gadolinium-enhanced constructive interference in steady state images for gamma knife radiosurgery and planning microsurgical procedures for skull base tumors. Acta Neurochir Suppl. 2013;116:167-78. doi: 10.1007/978-3-7091-1376-9_26. PubMed PMID: 23417476. [DOI] [PubMed] [Google Scholar]
- 8. Hinkes BG, von Hoff K, Deinlein F, Warmuth-Metz M, Soerensen N, Timmermann B, et al. Childhood pineoblastoma: experiences from the prospective multicenter trials HIT-SKK87, HIT-SKK92 and HIT91. J Neurooncol. 2007;81(2):217–23. Epub 2006/08/29. doi: 10.1007/s11060-006-9221-2. PubMed PMID: 16941074. [DOI] [PubMed] [Google Scholar]
- 9. Lekovic GP, Gonzalez LF, Shetter AG, Porter RW, Smith KA, Brachman D, et al. Role of Gamma Knife surgery in the management of pineal region tumors. Neurosurg Focus. 2007;23(6):E12. doi: 10.3171/FOC-07/12/E12. PubMed PMID: 18081477. [DOI] [PubMed] [Google Scholar]
- 10. Liu AK, Macy ME, Foreman NK. Bevacizumab as therapy for radiation necrosis in four children with pontine gliomas. Int J Radiat Oncol Biol Phys. 2009;75(4):1148–54. doi: 10.1016/j.ijrobp.2008.12.032. PubMed PMID: 19857784; PubMed Central PMCID: PMCPMC4155738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lubelski D, Abdullah KG, Weil RJ, Marko NF. Bevacizumab for radiation necrosis following treatment of high grade glioma: a systematic review of the literature. J Neurooncol. 2013;115(3):317–22. Epub 2013/09/05. doi: 10.1007/s11060-013-1233-0. PubMed PMID: 24005770. [DOI] [PubMed] [Google Scholar]
- 12. Mirza B, Mønsted A, Harding J, Ohlhues L, Roed H, Juhler M. Stereotactic radiotherapy and radiosurgery in pediatric patients: analysis of indications and outcome. Childs Nerv Syst. 2010;26(12):1785–93. Epub 2010/07/29. doi: 10.1007/s00381-010-1134-x. PubMed PMID: 20668863. [DOI] [PubMed] [Google Scholar]
- 13. Mori Y, Kobayashi T, Hasegawa T, Yoshida K, Kida Y. Stereotactic radiosurgery for pineal and related tumors . Prog Neurol Surg. 2009;23:106-18. Epub 2009/03/23. doi: 10.1159/000210057. PubMed PMID: 19329865. [DOI] [PubMed] [Google Scholar]
- 14. Nonoguchi N, Miyatake S, Fukumoto M, Furuse M, Hiramatsu R, Kawabata S, et al. The distribution of vascular endothelial growth factor-producing cells in clinical radiation necrosis of the brain: pathological consideration of their potential roles. J Neurooncol. 2011;105(2):423–31. Epub 2011/06/18. doi: 10.1007/s11060-011-0610-9. PubMed PMID: 21688077. [DOI] [PubMed] [Google Scholar]
- 15. Raleigh DR, Tomlin B, Buono BD, Roddy E, Sear K, Byer L, et al. Survival after chemotherapy and stem cell transplant followed by delayed craniospinal irradiation is comparable to upfront craniospinal irradiation in pediatric embryonal brain tumor patients. J Neurooncol. 2017;131(2):359–68. Epub 2016/10/24. doi: 10.1007/s11060-016-2307-6. PubMed PMID: 27778212. [DOI] [PubMed] [Google Scholar]
- 16. Tate M, Sughrue ME, Rutkowski MJ, Kane AJ, Aranda D, McClinton L, et al. The long-term postsurgical prognosis of patients with pineoblastoma. Cancer. 2012;118(1):173–9. Epub 2011/06/29. doi: 10.1002/cncr.26300. PubMed PMID: 21717450. [DOI] [PubMed] [Google Scholar]
- 17. Witt TC, Lo SS, Timmerman RD. Successful treatment of a skull base malignant rhabdoid tumor with surgery, chemotherapy and gamma Knife-based stereotactic radiosurgery in a young child. Stereotact Funct Neurosurg. 2007;85(6):310–3. Epub 2007/08/17. doi: 10.1159/000107372. PubMed PMID: 17709987. [DOI] [PubMed] [Google Scholar]