Abstract
Arum maculatum, commonly known as wild Arum, is a woodland plant species of the Araceae family. All parts of this plant are considered toxic. We report a case of a young man who allegedly consumed poisonous wild tuber with suicidal intention. He presented to our emergency department 3 h later with features of angioedema. He was managed successfully with adrenaline and hydrocortisone. He was discharged after 4 days of observation. Later, the wild tuber plant was identified to be A. maculatum. We recommend that all patients who present with unknown substance poisoning should be managed according to the principles of intensive care, irrespective of the diagnosis.
Key Words: Arum maculatum poisoning, plant poisoning, wild Arum, wild tuber poisoning
INTRODUCTION
Arum maculatum is a common woodland plant species of the Araceae family. It is widespread across temperate northern Europe and is known by an abundance of common names including snakeshead, adder's root, Arum, wild Arum, Arum lily, lords and ladies, devils and angels, cows and bulls, cuckoo-pint, Adam and Eve, bobbins, naked boys, starch-root, wake robin, friar's cowl, and jack in the pulpit.[1] The attractive red-to-orange berries are extremely poisonous. They contain oxalates of saponins which have needle-shaped crystals which irritate the skin, mouth, tongue, and throat, and result in swelling of throat, difficulty breathing, burning pain, and upset stomach. However, their acrid taste coupled with the almost immediate tingling sensation in the mouth when consumed mean that large amounts are rarely taken, and serious harm is unusual. All parts of the plant can produce allergic reactions in many people, and the plant should be handled with care.[2]
There is not much literature on A. maculatum poisoning. The manifestations of previously reported cases were vomiting, seizures, spasticity, difficulty in speaking, and altered sensorium. Only one case report described airway compromise during the hospital stay.[3] Our patient presented with upper airway obstruction with angioedema and was successfully managed with conservative measures without the need for the definitive airway.
CASE REPORT
A 20-year-old male presented to our emergency room 3 h after intentional consumption of 50 g of a wild poisonous tuber. On arrival, he was conscious, oriented, but unable to vocalize due to extensive swelling of lips with swollen tongue protruding outside the oral cavity, drooling of saliva and he preferred sitting position [Figure 1]. He was complaining of severe burning sensation over tongue, throat, and epigastrium and was breathless. His pulse rate was 150/min, blood pressure 120/80 mmHg, and room air oxygen saturation 95%. With a diagnosis of angioedema due to unknown tuber poisoning, he was treated with adrenaline nebulization, adrenaline 0.5 mg intramuscular injection, hydrocortisone 200 mg intravenous injection, and oxygen by face mask. Meanwhile, we prepared for endotracheal intubation and emergency surgical airway, in case his airway gets further compromised. He improved initially with medications alone, but oral swelling recurred after 1 h with persistent drooling of saliva. Hence, he was treated with adrenaline nebulization every 2–4th hourly and hydrocortisone 100 mg intravenous every 8th hourly. Emergency surgical airway equipment were kept ready bedside, and he was closely monitored. After 24 h, tongue swelling started reducing, and he was gradually improving. His routine laboratory reports were within normal limits [Table 1]. Later, his relatives brought the samples of the poisonous wild tuber for identification [Figures 2 and 3]. After discussing with the toxicologist, we identified the tuber to be A. maculatum. The patient was discharged after 4 days of observation.
Figure 1.

Angioedema with drooling of saliva from mouth
Table 1.
Laboratory values of the patient
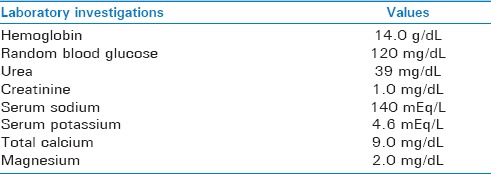
Figure 2.

Arum maculatum plant
Figure 3.

Wild tuber (Arum maculatum)
DISCUSSION
A. maculatum is a common woodland plant species of the Araceae family. It is widespread across temperate northern Europe and is known by an abundance of common names including snakeshead, adder's root, Arum, wild Arum, Arum lily, lords and ladies, devils and angels, cows and bulls, cuckoo-pint, Adam and Eve, bobbins, naked boys, starch-root, wake robin, friar's cowl, and jack in the pulpit.[1] The leaves of the plant are used commonly by the local people as a vegetable. The roots of the A. maculatum species are used in such treatments as diaphoretics, expectorants, and vermifuges. Terpenes or terpenoids are active against bacteria, fungi, viruses, and protozoa. A terpenoid constituent, capsaicin, has a wide range of biological activities in humans, affecting the nervous, cardiovascular, and digestive system, as well as finding use as an analgesic.[4]
The fresh tuber contains a volatile, acrid principle and starch, albumen. It also contains gum, sugar, extractive, lignin and salts of potassium, calcium, oxalates, and saponin. The root of the cuckoo-pint, when roasted well, is edible and when ground was once traded under the name of Portland sago. Its use is said to be very harsh on the skin, producing sores, and blisters.[2,5] It was also used as a substitute for arrowroot. If prepared incorrectly, it can be highly toxic and so should be prepared with due diligence and caution.[2]
The attractive red-to-orange berries are extremely poisonous. They contain oxalates of saponins which have needle-shaped crystals which irritate the skin, mouth, tongue, and throat, and result in swelling of throat, difficulty breathing, burning pain, and upset stomach. However, their acrid taste coupled with the almost immediate tingling sensation in the mouth when consumed mean that large amounts are rarely taken and serious harm is unusual. It is one of the most common causes of accidental plant poisoning based on attendance at hospital A and E departments. All parts of the plant can produce allergic reactions in many people, and the plant should be handled with care.[2]
It is rare for large amounts to be ingested because it rarely passes the oral area due to the calcium oxalate crystals formed which may pierce the mouth, throat, and digestive tract causing pain. When ingested in larger amounts, the symptoms include gastrointestinal discomfort, cardiovascular collapse, central nervous system depression, and rarely death. The management aims toward precipitating the oxalate in the digestive tract in the form of an insoluble calcium salt. Therefore, it is advised to administer lime water, chalk or magnesium in water, and stimulants such as black coffee or caffeine. Diuresis may be necessary to maintain renal function.[6]
The binding of the calcium with the oxalic acids also lowers the levels of available calcium in the body.[3] Depletion of calcium interferes with electrical activity of the heart, muscles, and nerves. Calcium depletion inhibits the action of calcium pump involved in the action potential of the muscles. The target organs are the kidneys followed by the nervous system.[7] It affects the kidneys by binding to calcium ions forming calcium salts.[8] In fatal cases of ingestion of oxalate-containing plants, pathological findings are principally in the kidneys, digestive tract, and brain. The postmortem findings in kidneys were small multiple hemorrhages, congestion, cellular cloudy swelling, sclerosis and hyaline degeneration of the tubules, and lesions traceable to an interstitial tubular glomerulonephrosis.[6]
A study in Switzerland found only one incident, in 29 years, where A. maculatum produced “serious” poisoning. In the UK, during a 4 years' period from 1996 to 1999, there were 23 visits to hospital resulting from poisoning by plants from the Arum genus. None resulted in serious harm. The only genus recording a higher total was the Solanum with 31 cases.[9]
Three cases were reported by Frazer in 1861. Two of them presented with recurrent seizures with spasticity of all four limbs, bloody frothing from mouth and dilated pupils. They were managed successfully and discharged without morbidity. One other patient had angioedema with extensive swelling of lips, tongue, and hard palate. He succumbed to death due to asphyxia within 9 h of ingestion. Frazer suggested that immediate emetics, melted fresh butter, zinc sulfate, and strong coffee might help in Arum poisoning. However, there is no scientific evidence for his recommendation.[10]
In our patient, initially, we were not aware of the actual toxic substance. With the clinical findings of angioedema causing airway compromise, he was managed symptomatically with medications and kept on close monitoring. If he had worsened clinically, securing the airway with endotracheal intubation or emergency surgical airway would have been the treatment options. Later, the toxic substance was found to be A. maculatum. There is not much literature on A. maculatum poisoning, clinical findings, and their management. Till date, no specific antidote has been reported.
Wild tuber poisoning is a life-threatening emergency which may require emergency resuscitation and aggressive airway management. Delay in establishing a patent airway may increase morbidity and mortality of critically ill patient. All emergency physicians must be able to promptly recognize “cannot intubate and cannot ventilate” situation and be skilled in performing surgical airway.[11]
CONCLUSION
Airway management is of utmost importance in any critically ill patient with alleged history of poisoning. A. maculatum contains oxalates which will form calcium oxalate crystals that are responsible for clinical manifestations. Emergency physicians should be aware of the toxic effects of A. maculatum. There is no specific antidote for this poison. Airway management may reduce the mortality and aggressive fluid administration may prevent the renal injury.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published, and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mauseth JD. Botany. Cram101 Textbook Reviews. 5th ed. Jones and Bartlett learning; 2016. Growth and division of the cell. [Google Scholar]
- 2.“Arum maculatum”. World Heritage Encyclopedia. [Last accessed on 2002 Apr 21]. Available from: http://www.worldebooklibrary.org/articles/Arum_maculatum .
- 3.Weaver CM, Heaney RP, Nickel KP, Packard PI. Calcium bioavailability from high oxalate vegetables: Chinese vegetables, sweet potatoes, and rhubarb. J Food Sci. 1997;62:524–5. [Google Scholar]
- 4.Safari E, Amiri M, Bahador A, Amiri M, Esmaeili D. The study of antibacterial effects of alcoholic extracts of Arum maculatum, Allium hirtifolium and Teucrium polium against nosocomial resistance bacteria. Int J Curr Microbiol Appl Sci. 2014;3:601–5. [Google Scholar]
- 5.Usman MR, Salgar SD, Nagpal N, Shaikh MZ. Poisonous Herbal Plants. New Delhi: Educreation Publishing; 2016. Herbs; p. 80. [Google Scholar]
- 6.Sanz P, Reig R. Clinical and pathological findings in fatal plant oxalosis. A review. Am J Forensic Med Pathol. 1992;13:342–5. doi: 10.1097/00000433-199212000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Akhan O, Ozmen MN, Coşkun M, Ozen S, Akata D, Saatçi U, et al. Systemic oxalosis: Pathognomonic renal and specific extrarenal findings on US and CT. Pediatr Radiol. 1995;25:15–6. doi: 10.1007/BF02020832. [DOI] [PubMed] [Google Scholar]
- 8.Hesse A, Siener R, Heynck H, Jahnen A. The influence of dietary factors on the risk of urinary stone formation. Scanning Microsc. 1993;7:1119–27. [PubMed] [Google Scholar]
- 9.John R. Arum maculatum, Cuckoopint, Lords and Ladies”. The Poison Garden. 2009. [Last accessed on 2009 Aug 01]. Available from: http://www.thepoisongarden.co.uk/swiss_cases.htm .
- 10.Frazer W. Cases of poisoning by Arum maculatum. Br Med J. 1861;1:654. [Google Scholar]
- 11.Anandhi D, Raju KP, Saya RP, Pandit VR. Difficult airway management in a case of hair dye poisoning. Int J Acad Med. 2017;3:120–3. [Google Scholar]


