Abstract
Facial paralysis can be a devastating consequence resulting from blunt and penetrating trauma to the head and neck, as well as surgical injury, either accidental or due to involvement by tumor. In addition, the etiology can be attributed to a variety of other causes, ranging from infectious to metabolic, and is frequently idiopathic in nature. The incidence of facial nerve injury during temporomandibular joint (TMJ) surgeries varies among surgeons. There are many factors that could contribute to the injury of the temporal and zygomatic branches of the facial nerve. These nerves lie in a confluence of superficial fascia, temporalis fascia, and periosteum and may be injured by any dissection technique that attempts to violate the integrity of these regions. Excessive or heavy-handed retraction causes compression and/or stretching of nerve fibers resulting in neuropraxia. The facial nerve then enters the parotid gland, where the main trunk branches into the upper and lower divisions at the pes anserinus. The nerve further divides into five main branches: the temporal, zygomatic, buccal, marginal mandibular, and cervical. The temporal branch lies within the superficial muscular aponeurotic system at the level of the zygomatic arch. In this paper, we evaluate the facial nerve function based on the House–Brackmann grading index after the preauricular approach for the treatment of condylar fractures, pathologies, and TMJ ankylosis cases. The nerve functional regeneration postfacial nerve injury has been evaluated and reported in this retrospective study.
Keywords: Facial paralysis, House–Brackmann grading, neuropraxia, superficial muscular aponeurotic system
INTRODUCTION
Facial paralysis can be a devastating consequence resulting from blunt and penetrating trauma to the head and neck, as well as surgical injury, either accidental or due to involvement by tumor. In addition, the etiology can be attributed to a variety of other causes, ranging from infectious to metabolic, and is frequently idiopathic in nature.[1]
The incidence of facial nerve injury during temporomandibular joint (TMJ) surgeries varies among surgeons. There are many factors that could contribute to the injury of the temporal and zygomatic branches of the facial nerve. These nerves lie in a confluence of superficial fascia, temporalis fascia, and periosteum and may be injured by any dissection technique that attempts to violate the integrity of these regions. Excessive or heavy-handed retraction causes compression and/or stretching of nerve fibers resulting in neuropraxia; this may be the reason for a significant number of nerve injuries associated with TMJ surgery.[2,3]
Facial nerve injury may also be caused by inadvertent suture ligation of facial nerve branches, particularly during wound closure. To prevent this undue complication, deep blind bites with the suture needle should be avoided. The use of electrocautery in deep sites that are potentially close to facial nerve branches or within the parotid gland should also be avoided. Furthermore, one should avoid crushing or clamping tissue indiscriminately, particularly during episodes of brisk bleeding.[4] Excessive swelling or hematoma formation may result in transient facial nerve injury. Furthermore, patients with previous TMJ surgery have an increased incidence of facial nerve injury.[5]
ASSESSMENT
Precise characterization of facial nerve paralysis must be accomplished to provide proper patient counseling regarding prognosis and treatment. The House–Brackmann 6-point scale of facial nerve function is the most commonly used standardized tool for assessing the degree of facial weakness.[6,7] This scale is deficient, however, in terms of characterizing facial paralysis localized to one particular facial distribution.
Careful assessment and documentation of facial nerve function should include a detailed description of the status of motion of the upper, middle, and lower face. Special attention should be paid to the eye not only in terms of eyelid closure, lower lid laxity, and brow height but also to visual acuity, presence of Bell's phenomenon, and corneal irritation. Aside from overall symmetry, other important functional considerations include nasal valve collapse and oral competence.
Grades of House- Brackmann scale for facial nerve function were as follows:[8]
Grade I – Normal
Normal facial function in all areas.
Grade II – Slight dysfunction
Gross: Slight weakness noticeable on close inspection; may have very slight synkinesis
At rest: Normal symmetry and tone
Motion: Forehead – moderate-to-good function; eye – complete closure with minimum effort; mouth – slight asymmetry.
Grade III – Moderate dysfunction
Gross - Obvious but not disfiguring difference between two sides; noticeable but not severe synkinesis contracture, and/or hemifacial spasm
At rest – Normal symmetry and tone
Motion: Forehead – slight-to-moderate movement; eye – complete closure with effort; mouth – slightly weak with maximum effort.
Grade IV – Moderate-severe dysfunction
Gross: Obvious weakness and/or disfiguring asymmetry
At rest: Normal symmetry and tone
Motion: Forehead – none; eye – incomplete closure; mouth – asymmetry with maximum effort.
Grade V – Severe dysfunction
Gross: Only barely perceptible motion
At rest: Asymmetry
Motion: Forehead – none; eye – incomplete closure; mouth – slight movement.
Grade VI – Total paralysis
No movement.
CASE REPORTS AND ASSESSMENT OF FACIAL NERVE INJURY
Case 1
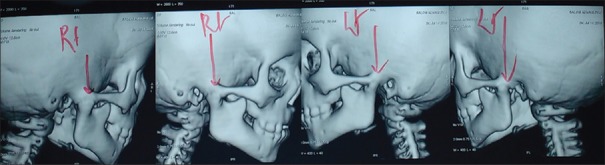
A patient reported to the department of oral and maxillofacial surgery with a complaint of reduced mouth opening and sought treatment for the same. The patient was examined, and the investigations were carried out to diagnose it as a case of TMJ ankylosis [Figure 1].
Figure 1.
Computed tomography with three-dimensional reconstruction showing bony ankylosis of the right and left side
Unilateral condylectomy with gap arthroplasty was carried out as a treatment procedure and the approach utilized was the preauricular approach [Figure 2].
Figure 2.

Preauricular incision on the right and left side
Facial nerve function was assessed postoperatively, and according to House–Brackmann grading index, it was a Grade II [Figure 3].
Figure 3.

Facial nerve function evaluation after 3 months
The patient was continuously reviewed to assess the facial nerve function and showed improvement following physiotherapy.
Case 2
The case of keratocystic odontogenic tumor of the left mandible extending from 34 to the sigmoid notch was reported [Figure 4]. The treatment planned for this patient was:
Figure 4.
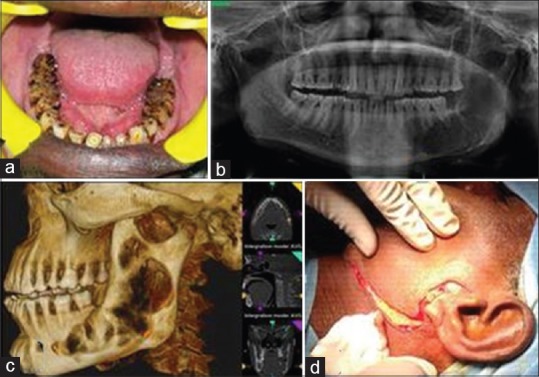
(a) Intraoral view (b) orthopantomogram (c) computed tomography with three-dimensional reconstruction view (d) preauricular, Hinds, and Risdon's incision
Surgical excision of the lesion with a wide margin of around 1 cm
Carnoy's solution application postexcision
Reconstruction using free fibula osteocutaneous flap.
For the surgical excision of the lesion, a combination of preauricular, Hinds, and Risdon's incisions was given. After blunt dissection, osteotomy was carried out on the region of the left condyle and in the region of 34. Chemical cauterization and reconstruction using free fibula was carried out next.
Facial nerve function was assessed postoperatively, and according to House–Brackmann grading index, it was a Grade III. The patient was managed conservatively for improvement of facial nerve function by physiotherapy. During the follow-up visits, the facial nerve function was evaluated, and in the duration of 6 months postoperatively, there was improvement noted in the function of facial nerve from Grade III to Grade I [Figure 5].
Figure 5.

Frontal view and marginal mandibular nerve injury House–Brackmann score – Grade 3
Case 3
The case is that of left parasymphyseal fracture with bilateral condylar fracture. The necessary investigations of computed tomography facial bones with three-dimensional reconstruction were carried out which confirmed the diagnosis of left parasymphyseal fracture with bilateral condylar fracture with lateral displacement on the right side [Figure 6].
Figure 6.
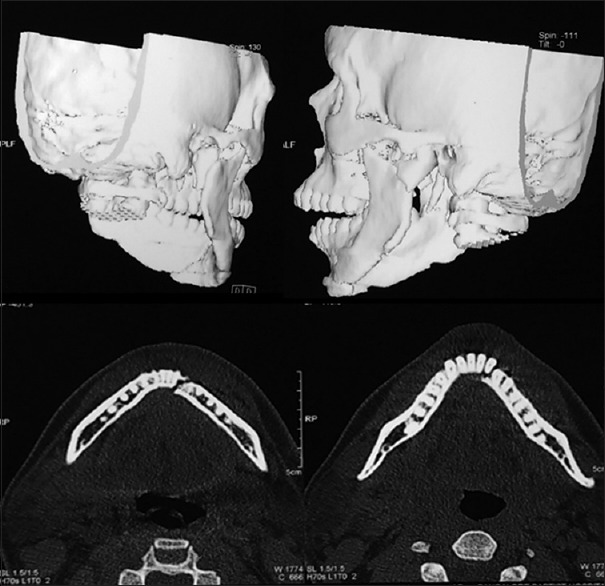
Right and left condylar fracture and left parasymphyseal fracture
The treatment planned was to treat the condylar fracture by open reduction and internal fixation owing to reduced mouth opening (12 mm) and deviation toward the right side using the retromandibular incision. The facial nerve and its branches were encountered and protected [Figure 7].
Figure 7.

Intraoperative view
Postoperative facial nerve function was evaluated which, however, showed facial nerve injury with House–Brackmann score of Grade III. The temporal, zygomatic, and marginal mandibular branches of facial nerve showed weakness on the right side. The condition was managed conservatively following physiotherapy. After a duration of 3 months, the facial nerve function was improved from Grade III to Grade I [Figure 8].
Figure 8.

Postoperative improvement of function
DISCUSSION
Facial nerve is considered the “Queen of The Face” as it innervates the muscles of facial expression. Anatomic variations and multiple innervation patterns of the peripheral branches render facial nerve to an increased risk during various surgical procedures to TMJ using preauricular approach.[9] Facial nerve injury following various surgical procedures to the maxillofacial region ranges from 0% to 48%.[9] Incidence of facial nerve injury following TMJ surgeries ranges from 1% to 32%.[10] Out of the several methods used for evaluating the motor function of facial nerve, House–Brackmann facial nerve grading system has gained some importance. This was introduced in 1983 and modified by House and Brackmann in 1985 and accepted by the American Academy of Otolaryngology and Head and Neck Surgery.[8] It is a comprehensive method of evaluation of motor function, both at rest and in function. It carries an interobserver reliability of 93%.[8]
The facial nerve is the second most commonly damaged cranial nerve, being involved in 1% to 3% of head injury patients. The common site of injury is within the facial nerve canal. The occurrence of facial nerve paralysis depends on the type of temporal bone fracture and its incidence is 20% with longitudinal fractures and 50% in transverse fractures.[11] Intraneural hematoma (40%–50%), nerve disruption (9%–26%), contusion (36%), or impinging bone fragments may cause its dysfunction. Furthermore, the facial nerve is relatively fixed at geniculate ganglion where it is tethered by greater superficial petrosal nerve causing injury. The meatal foramen due to its narrow size in the labyrinthine segment is another potential site of facial nerve compression, especially in the presence of edema or hematoma. The mechanism of facial nerve injury in our case cannot be attributed to temporal bone fracture as the fracture line is much higher for facial nerve path.[11]
Facial nerve injury is a well-recognized risk of TMJ surgeries regardless of the surgical approach. The actual reported incidence of damage, however, varies among studies from 1% to 55%.[5] According to Keith,[12] the incidence of facial nerve injury resulting from TMJ surgery ranges from 1% to 25%. In the present series of cases, the nerve injuries were mainly transient in nature, usually resolving within 6 months.
Neuropraxia of the temporal and zygomatic branches of the facial nerve that was encountered at the immediate postoperative observation was most likely due to the surgical trauma induced from the retraction and handling of tissues in this area. Excessive or heavy-handed retraction causes compression or stretching of nerve fibers, which results in nerve sheath edema and neuropraxia. This may be responsible for a significant number of nerve injuries associated with TMJ surgery. The normal anatomical variation in the distribution of the facial nerve branches may also be related to the incidence of clinically apparent injury.
In a study conducted by Do Egito Vasconcelos et al., it was found that the incidence of facial nerve injury increased significantly in patients who had TMJ ankylosis and those who had gap arthroplasty,[10] which is in agreement with the cases presented in this study.
In their study, the evaluation of facial nerve injury was based solely on clinical assessment using the House–Brackmann facial nerve injury grading system.[8]
The increased incidence of facial nerve injury in patients who have undergone previous TMJ surgery (100%) may be explained by the fact that surgical scarring leads to fibrosis and distortion of the fascial layers, thereby causing a distortion of the anatomical planes and making an accurate surgical dissection more difficult at a second intervention. Roychoudhury et al. reported that 20% of 50 cases of operated ankylosis resulted in postoperative injury to the facial nerve.[13] Nogueira and Vasconcelos[14] showed that 31% of patients operated on for the treatment of ankylosis showed facial nerve injury, and 75% of these patients had undergone at least one surgical intervention prior.
Kaban et al., on analyzing the distribution of the types of ankylosis in a series of patients, observed that both the surgical approach and the type of ankylosis might influence the grade of injury.[15] Nogueira and Vasconcelos noted that facial nerve injury occurred in 75% of cases of osseous ankylosis and in 25% of those with fibro-osseous ankylosis.[14] This indicated that the degree of surgical difficulty and the duration of surgery, with subsequent aggressive handling of the tissue, are important factors in the incidence of facial nerve injury.
Postoperative facial nerve injury is a multifactorial complication that is transient in nature and does not depend on the surgical approach alone. Other contributing factors include the type of surgery, the surgical difficulties encountered, the duration of surgery, and previous surgery to the joint. All of these factors play an important role in postoperative facial nerve injury.[2]
The time taken for the recovery of motor function ranged between 1 and 6 months among various authors.[10,16] In the present study, maximum amount of recovery occurred at 1–3 months, and in 6-month postoperative period, all the patients showed recovery of normal motor nerve function.
These findings are consistent with previous authors who stated that preauricular approach is safe and cosmetic and results in temporary impairment of function.[10,16,17]
The time taken for recovery of the temporal branch was more compared to zygomatic branch. Cormack et al.[18] have reported eight types of facial nerve branching patterns after their study on 100 cadaver dissections of which there are multiple anastomoses between the branches. The incidence of cross-anastomosis between zygomatic and buccal branches is high (87% and 100%).[16] Temporal branch lies about 2 cm on average (0.8–3.5 cm) from anterior concavity of external auditory canal and crosses zygomatic arch from 2.5 cm to 3.5 cm from lateral orbital rim.[10,19] It lies deep to the temporoparietal fascia, and at the zygomatic arch, it lies in a condensation of superficial fascia, temporalis fascia, and periosteum and is most vulnerable in this region. If the tissue dissection violates the integrity of this region, it results in temporal nerve weakness. Stretching of the nerve and excessive retraction of the tissues resulting in edema and compression of the nerve might be the possible reasons for the delayed recovery of the temporal branch in our series. However, a larger sample size is needed to draw further conclusions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Gordin E, Lee TS, Ducic Y, Arnaoutakis D. Facial nerve trauma: Evaluation and considerations in management. Craniomaxillofac Trauma Reconstr. 2015;8:1–3. doi: 10.1055/s-0034-1372522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elmadawy A, Hegab A, Alahmady H, Shuman M. Clinical and electromyographic assessment of facial nerve function after temporomandibular joint surgery. Int J Oral Maxillofac Surg. 2015;44:1275–80. doi: 10.1016/j.ijom.2015.04.013. [DOI] [PubMed] [Google Scholar]
- 3.Ellis E, 3rd, McFadden D, Simon P, Throckmorton G. Surgical complications with open treatment of mandibular condylar process fractures. J Oral Maxillofac Surg. 2000;58:950–8. doi: 10.1053/joms.2000.8734. [DOI] [PubMed] [Google Scholar]
- 4.Block MS, Kent JN. Modified rhytidectomy approach for total temporomandibular joint reconstruction: A case report. J Oral Maxillofac Surg. 1989;47:187–90. doi: 10.1016/s0278-2391(89)80116-8. [DOI] [PubMed] [Google Scholar]
- 5.Weinberg S, Kryshtalskyj B. Analysis of facial and trigeminal nerve function after arthroscopic surgery of the temporomandibular joint. J Oral Maxillofac Surg. 1996;54:40–3. doi: 10.1016/s0278-2391(96)90301-8. [DOI] [PubMed] [Google Scholar]
- 6.House JW. Facial nerve grading systems. Laryngoscope. 1983;93:1056–69. doi: 10.1288/00005537-198308000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Brackmann DE, Barrs DM. Assessing recovery of facial function following acoustic neuroma surgery. Otolaryngol Head Neck Surg. 1984;92:88–93. doi: 10.1177/019459988409200119. [DOI] [PubMed] [Google Scholar]
- 8.House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93:146–7. doi: 10.1177/019459988509300202. [DOI] [PubMed] [Google Scholar]
- 9.Prabhu RK, Sinha R, Chowdhury SK, Chattopadhyay PK. Evaluation of facial nerve function following surgical approaches for maxillofacial trauma. Ann Maxillofac Surg. 2012;2:36–40. doi: 10.4103/2231-0746.95315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.do Egito Vasconcelos BC, Bessa-Nogueira RV, da Silva LC. Prospective study of facial nerve function after surgical procedures for the treatment of temporomandibular pathology. J Oral Maxillofac Surg. 2007;65:972–8. doi: 10.1016/j.joms.2006.06.280. [DOI] [PubMed] [Google Scholar]
- 11.Lee GY, Halcrow S. Petrous to petrous fracture associated with bilateral abducens and facial nerve palsies: A case report. J Trauma. 2002;53:583–5. doi: 10.1097/00005373-200209000-00034. [DOI] [PubMed] [Google Scholar]
- 12.Keith DA. Boston, MA: Blackwell Science; 1988. Surgery of the Temporomandibular Joint: Success, Failure and Complication of Temporomandibular Joint Surgery; pp. 272–88. [Google Scholar]
- 13.Roychoudhury A, Parkash H, Trikha A. Functional restoration by gap arthroplasty in temporomandibular joint ankylosis: A report of 50 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:166–9. doi: 10.1016/s1079-2104(99)70267-2. [DOI] [PubMed] [Google Scholar]
- 14.Nogueira RV, Vasconcelos BC. Facial nerve injury following surgery for the treatment of ankylosis of the temporomandibular joint. Med Oral Patol Oral Cir Bucal. 2007;12:E160–5. [PubMed] [Google Scholar]
- 15.Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990;48:1145–51. doi: 10.1016/0278-2391(90)90529-b. [DOI] [PubMed] [Google Scholar]
- 16.Wilson AW, Ethunandan M, Brennan PA. Transmasseteric antero-parotid approach for open reduction and internal fixation of condylar fractures. Br J Oral Maxillofac Surg. 2005;43:57–60. doi: 10.1016/j.bjoms.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 17.Weinberg S, Kryshtalskyj B. Facial nerve function following temporomandibular joint surgery using the preauricular approach. J Oral Maxillofac Surg. 1992;50:1048–51. doi: 10.1016/0278-2391(92)90488-l. [DOI] [PubMed] [Google Scholar]
- 18.Henry Hollinshead W. Philadelphia: Harper & Row; 1982. Anatomy for Surgeons; pp. 314–5. [Google Scholar]
- 19.Al-Kayat A, Bramley P. A modified pre-auricular approach to the temporomandibular joint and malar arch. Br J Oral Surg. 1979;17:91–103. doi: 10.1016/s0007-117x(79)80036-0. [DOI] [PubMed] [Google Scholar]