Abstract
Purpose:
To put an algorithmic approach for the treatment of condylar fractures according to the condition of occlusion.
Patients and Methods:
This study had been carried out between May 2016 and April 2017. Forty patients were included (6 females and 34 males) with their ages ranged between 3 and 60 years. Patients were managed through two approaches as follows: maxillomandibular fixation (MMF) only regimen and MMF with open reduction and internal fixation regimen. The operated cases were 12 with bilateral condylar/subcondylar fractures, and the rest were unilateral 28 cases.
Results:
Data were assessed demographically, time lapse before the intervention, surgically, functionally, and radiologically. In general, there were no significant differences between closed and open methods.
Conclusion:
Retromandibular approach was convenient for internal fixation of condylar fracture with a good outcome. In our work, there were no significant differences between closed and open methods in the treatment of condylar fractures.
Keywords: Closed method, condylar fracture, open method, trauma
INTRODUCTION
Condylar fracture is a common site for mandibular fracture and constitutes about one-third of all mandibular fractures.[1]
The condyle is the most commonly injured area in the pediatric mandible.[2] There is a growth center in the condyle, and the mandible reaches its adult size in females 2 years before males (16 years in females).[3]
Etiology of condylar fracture is usually due to trauma and violence. Trauma occurs more common at young age and violence has more prevalence in females.[4]
Condylar fracture is associated with pain, reduced mouth opening, and deviation of the mandible. With suboptimal treatment, temporomandibular joint (TMJ) ankylosis, and internal derangement may occur.[5]
Since 1925, there was debate for approaching condylar fracture.[6] The most commonly used incisions to expose the condyle are as follows: intraoral, coronal, preauricular, postauricular, endaural, endoscopic, rhytidectomy, transparotid, submandibular, and retromandibular approach.[7]
In 1967, Hinds and Girotti had described retromandibular approach which later was modified by Koberg and Momma in 1978.[8,9]
This approach allows direct access to the posterior surface of the ramus of the mandible. Furthermore, it is a short distance from the condyle and sigmoid notch. In addition, it leaves an acceptable scar. Nowadays, retromandibular incision is adopted by most oral and maxillofacial surgeons.
In this manuscript, an algorithmic approach was used for the treatment of condylar fractures according to the condition of occlusion.
PATIENTS AND METHODS
The study protocol was approved by the Ethical Committee (MFM-IRB) of our university, code number MS/16.04.09. It had been carried out between May 2016 and April 2017. Forty patients were included (6 females and 34 males) and their ages ranged between 3 and 60 years. Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
All cases had been diagnosed with a recent posttraumatic condylar fracture, and this diagnosis had been confirmed after good history taking, thorough physical examination, and radiological imaging. None of our cases had a previous history of TMJ dysfunction. The operated cases were 12 with bilateral condylar fractures and the rest were unilateral 28 cases.
Exclusion criteria included cases that had severely comminuted mandibular fractures and cases that had multiple displaced maxillofacial fractures associated with the mandibular ones. Furthermore, uncooperative patients and patients refusing the surgery were excluded from the study. In addition, patients unfit for surgery due to medical illness such as recent stroke, myocardial infarction, atherosclerosis, deep venous thrombosis, and those with a history of chemotherapy or radiotherapy were added to the exclusion criteria.
Patients were managed through two approaches as follows: maxillomandibular fixation (MMF) only regimen and MMF with open reduction and internal fixation (ORIF) regimen.
According to the condition of occlusion, patient with good occlusion was closed with MMF. The wires were removed after 21 days and were replaced with elastic bands (1/8) for additional 7 days postoperatively.
In pediatric cases, they were managed with MMF only and elastic bands were used from the start (no wires) for 14 days.
If there was open bite on the contralateral side of the fracture or an anterior open bite in bilateral cases of condylar fracture, we would proceed to ORIF.
Cases associated with anterior mandibular fractures were managed first by internal fixation of anterior mandibular fractures then occlusion was assessed. If malocclusion still persists, internal fixation would be made through the retromandibular incision. In some cases, the fracture was approached through an already existing wound in the submandibular or retromandibular regions.
Surgical technique
Retromandibular incision
Guided by Emam et al.,[10] a 3 cm long incision was marked 2 cm posterior and parallel to the posterior border of the ascending ramus from a point 1 cm only below the lobe of the ear.
The incision was deepened through the skin and subcutaneous tissue to the level of platysma. The retromandibular vein [Figure 1a] was usually located in the middle of the incision. Then, dissection was continued in a plane deeper to the vein to protect marginal branch of facial nerve [Figure 1b]. The pterygomasseteric sling was incised, and the fracture was exposed with the help of retractors.
Figure 1.
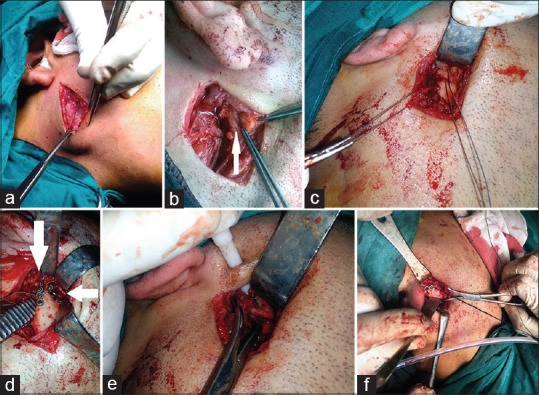
(a) Exposure of vein through retromandibular incision. (b) marginal mandibular nerve through retromandibular incision. (c) wire insertion through retromandibular incision. (d) two plates fixation through retromandibular incision. (e) insertion of cable as trocar through retromandibular incision. (f) Manipulation of plate through silk suture through retromandibular incision
To facilitate reduction, two holes were made in both the proximal and distal segments on their lateral edges. Then, a wire loop was inserted to connect both holes. By pulling the wire, the fractured segments were reduced and rotated to the right position [Figure 1c].
In all open cases, fixation was done by using 2 miniplates. One of them was applied parallel to the ramus margin (marginal plate) and the second plate was applied in a 45 degree angle with the marginal one [Figure 1d].
In some cases, fixation of the proximal segment was made through the use of a trocar [Figure 1e]. Sometimes, a silk suture was passed through an empty hole of the plate after fixation of the first screw to ease the adjustment of the plate in the correct position [Figure 1f].
Follow-up
All patients underwent postoperative facial computed tomography, skull X-ray and panorama views at three stages. These stages were as follows: immediate postoperative, 3 months, and 6 months postoperatively.
In open group, facial nerve function was assessed 12 h postoperatively and 3 months postoperatively.
Data analysis
Statistical package for the (SPSS) version 15 (SPSS, Inc, Chicago, ll) was used for the statistical analysis. Qualitative data were presented as number and percent. Quantitative data were presented as mean ± standard deviation (SD) unpaired t-test was used. The value of P < 0.05 was considered to be statistically significant.
RESULTS
Demographic results
Gender results
The male-to-female ratio of the total patient material was about 5.7:1 [Figure 2]. There was a significant difference in the presence of condylar fractures between males and females (P < 0.05).
Figure 2.
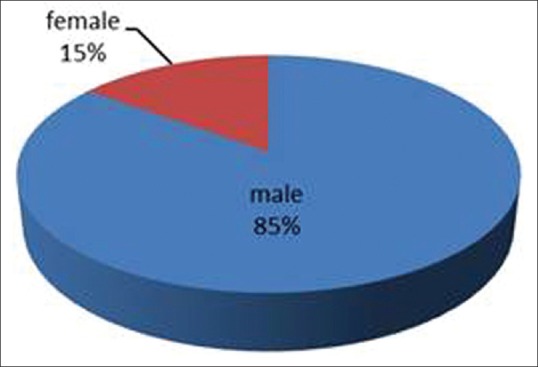
Gender distribution
Age results
Mean age at the time of the surgery was 19.1 years (minimum 3, maximum 60). The peak age was 20 years. Adult patients (>18Y in males, and >16Y in females) were 47.5% (19/40). Pediatric patients counted 52.5% [Figure 3].
Figure 3.
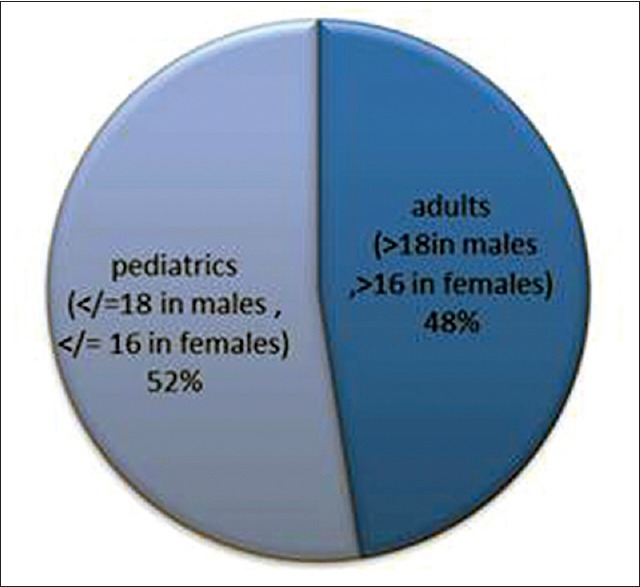
Age distribution
Site and association of fractures results
In this study, 30% of patients presented with bilateral condylar/subcondylar fractures. About 37.5% of the fractures (15/40) occurred in the left condyle and 32.5% of the fractures (13/40) occurred in the right condyle.
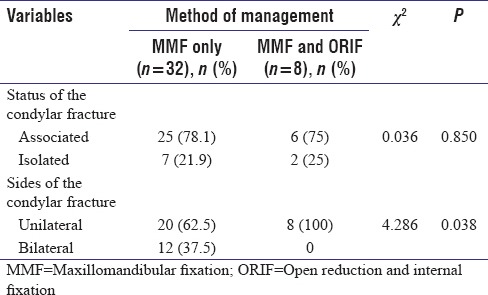
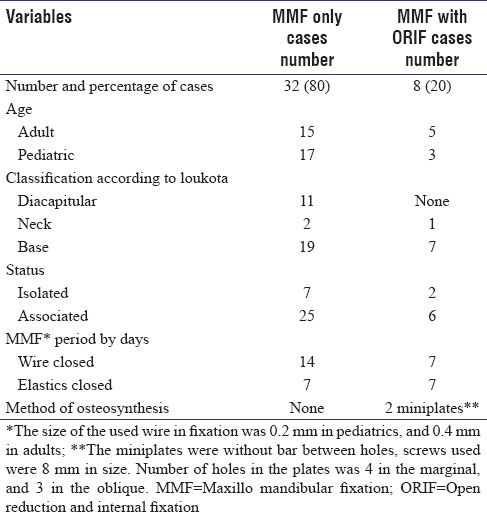
In 22.5% of the patients (9/40), there was only a fracture of the condylar process without accompanying fractures (isolated fracture). Parasymphyseal fracture of the mandible was associated with condylar fracture in 27.5% of the patients (11/40), (3 cases of them were with bilateral C/SC fracture). In 27.5% of patients (11/40), additional symphyseal fractures were diagnosed. Associated angle fractures were diagnosed in 12.5% (5/40). Furthermore, body fractures were diagnosed in 10% (4/40). Statistically, mandibular symphyseal and parasymphyseal fractures (anterior mandibular fractures) were significantly associated with fractures of the mandibular condyle (P < 0.05). There was a significant P value between ORIF and unilateral cases [Table 1].
Table 1.
Fracture status and side relation with the method of management
Etiology results
Road traffic accidents (RTA) were the most frequent cause as they constituted 57.5% of cases [Figure 4]. Falls came next (37.5% of cases) and violence came last (5% of cases).
Figure 4.
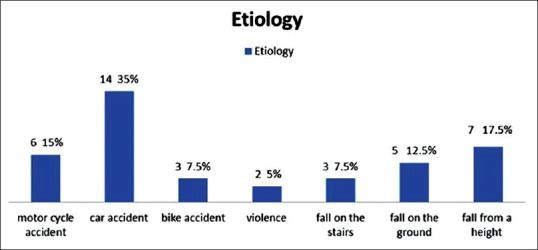
Etiology distribution
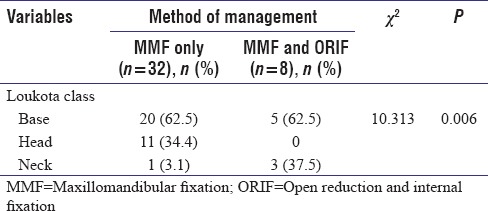
Fractures classification results
In this study, the condylar fractures were 52 fractures in 40 cases. Their sites were at the condylar base (59.7%), the diacapitular area (28.8%) and the condylar neck (11.5%).[11]
Condylar head (diacapitular) fractures did not need ORIF, and there was a significant difference between the use of ORIF and other levels of fracture (neck and base) [Table 2].
Table 2.
Class classification and management
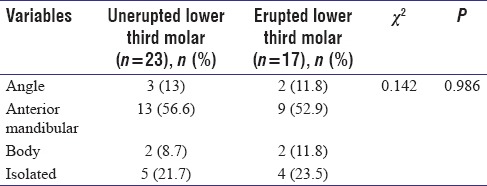
Presence of unerupted lower third molar tooth in the side of the fracture
There were 42.5% (17/40) of the cases with erupted lower third molar tooth (present or extracted) in the fracture side. They were associated with angular fractures in two cases.
The remaining cases (unerupted) 57.5% (23/40) were associated with angular fracture in three cases.
There was no significance between eruption status of the 3rd molar and the association of the mandibular condylar fracture with an angular one [Table 3].
Table 3.
Angle fracture relation with unerupted lower third molar tooth
Time lapse before intervention
Of all cases, 67.5% were treated within the first 7 days after the time of the accident. The interval between injury and operation ranged from 0 to 17 days [Figure 5].
Figure 5.
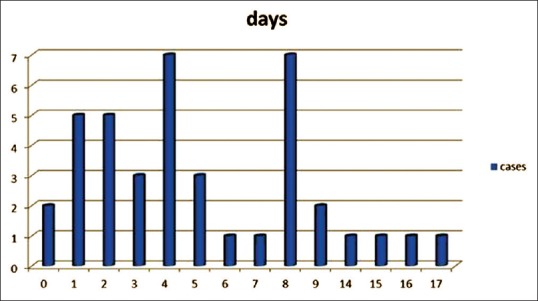
Elapsed time between injury and operation
Analysis of surgical intervention data
Data of the cases managed with closed reduction and cases managed with ORIF were expressed in Table 4.
Table 4.
Analysis of surgical intervention data
Regarding the length of hospital stay, hospitalization time ranged from 1 to 10 days, with a mean duration of 2.6 days. The longer hospitalization times were due to other reasons, e.g., concomitant body injuries such as brain and limb injuries.
Results of functional findings
Maximum active interincisal opening
The mean preoperative maximal active interincisal opening was 21.4 mm (range 12–31 with SD 5.1 mm) and the mean postoperative maximal active interincisal opening after 1 month reached up to 30.1 mm (range 20–44 with SD 7.4 mm). It increased to 40 mm (range 30–49 with SD 6 mm) after 6 months [Figure 6].
Figure 6.
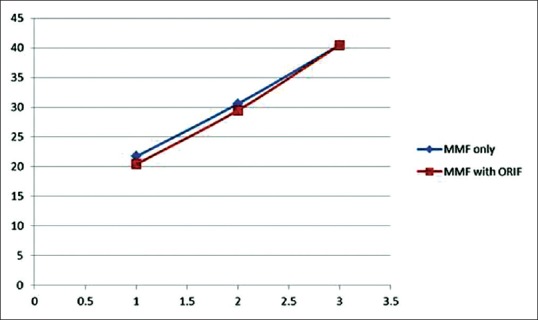
The average values (vertical axis) of preoperative, 3 months postoperative and 6 months postoperative incisal openings (1, 2, and 3 in the horizontal axis) in both methods of management, Maxillo mandibular fixation only and Maxillo mandibular fixation with open reduction and internal fixation
Cases managed by MMF only showed a significant increase of the incisal opening by 41% after 3 months and after 6 months by 88.3% in comparison to preoperative incisal opening.
Furthermore, cases managed with ORIF with MMF; there was a significant increase in average incisal opening, which increased by 44.6% after 3 months and after 6 months by 98.5% in comparison to preoperative incisal opening.
Pre- and post-operative bite
There were 62.5% (25/40) of cases suffering from a preoperative open bite. Nearly 56% (14/25) of them were associated with anterior mandibular fractures [Table 5].
Table 5.
Relation of open bite with the management
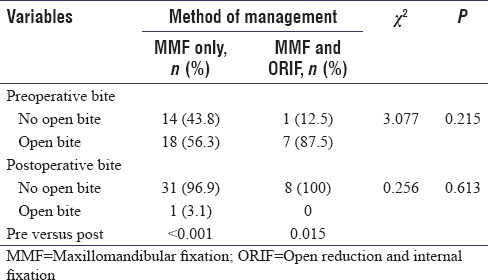
There were 37.5% (15/40) of cases, which presented with no open bite. Nearly 40% (6/15) of them were condylar fractures associated with anterior mandibular fractures.
All cases showed no open bite postoperatively except one case. The case was associated with anterior mandibular fracture. The mandible was closed forcefully with MMF to close the open bite. After we opened the MMF, the bite returned to be open.
We also noticed that 62.5% (5/8) of cases fixed by ORIF were associated with anterior mandibular fractures. All of them were suffering from an open bite that was not corrected after fixation of the associated anterior mandibular fracture. Actually, open bite increased after reduction of the associated anterior body fracture, and hence, we had to open on the condylar fracture to correct the bite.
Assessment of facial nerve function
Among the open group, two cases showed postoperative transient weakness of marginal mandibular branch of the facial nerve. They showed temporary moderate weakness grade 3 according to the House-Brackmann Facial Nerve Grading System.[12] Temporary weakness of facial nerve lasted for 2 months in one patient and for 3 months in the other one.
Radiographic results
Angle of coronal displacement of the fractured side
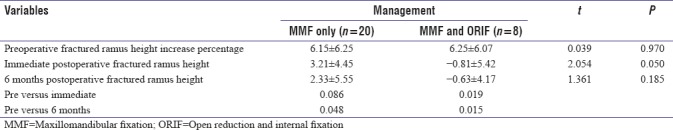
The mean preoperative acute angle of coronal displacement of the fractured side (52 sides of the 40 cases) was 23.9° (range 0–89 with SD 24.5°). While the mean postoperative angle reached 16.4° (range 0–89 with SD 22.3°) in the immediate postoperative stage and decreased to 5° (range 0–54 with SD 12.6°) after 6 months [Figures 7 and 8]. The average decrease in angle was 23.9° in the open group, and the average decrease in angle was 17.5° in the closed group. There was no significant difference between both methods as regards decrease of angle [Table 6].
Figure 7.
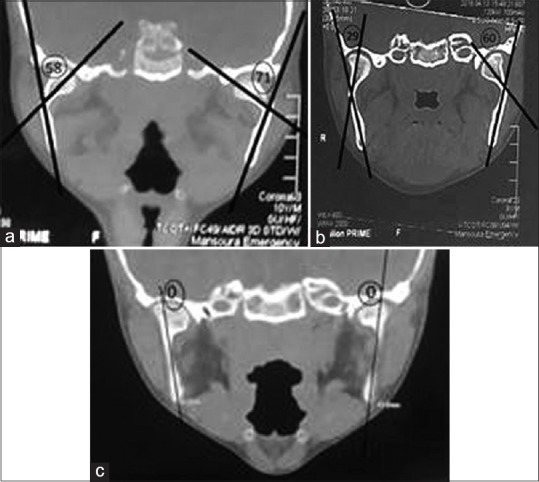
(a) Preoperative view of angles of coronal displacement of the fractured side.(b) immediate postoperative view of angles of coronal displacement of the fractured side. (c) 6 months postoperative view of angles of coronal displacement of the fractured side
Figure 8.
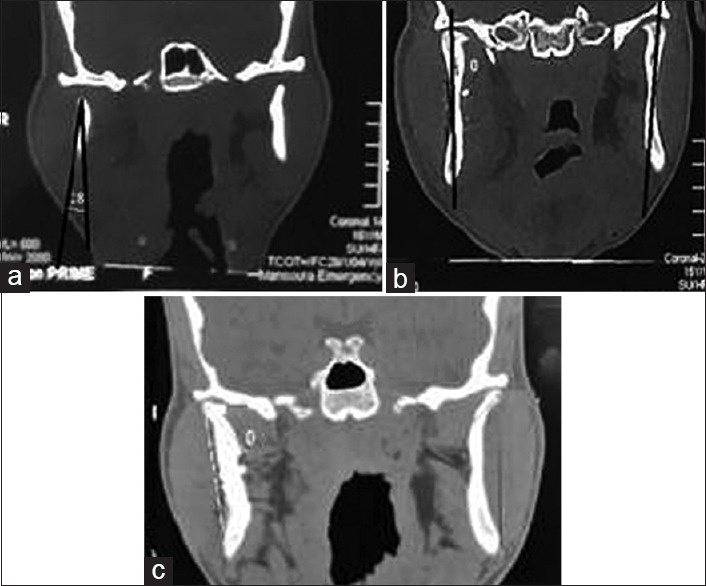
(a) Preoperative view of angles of coronal displacement of the fractured side. (b) immediate postoperative view of angles of coronal displacement of the fractured side. (c) 6 months postoperative view of angles of coronal displacement of the fractured side
Table 6.
Angle of coronal displacement of the fractured side preoperatively and postoperatively
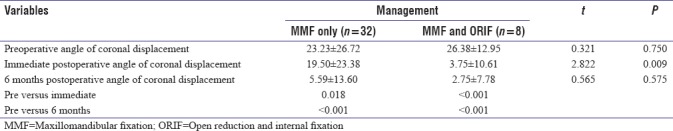
Ramus height difference percentage
The mean preoperative ramus height difference percentage between both sides of the mandible in unilateral condylar fracture (28 cases) was 4.2% increase on normal side (range 80–120 with SD 7.6%).
The mean postoperative percentage difference in ramus height between normal and fractured side decreased to 1% (range 82.5–136 with SD 7.8%) in the immediate postoperative period and to 0.4% (range 80–130 with SD 6.7%) after 6 months. The ramus height difference percentage was 0% in the open group and was 0.6% in the closed group after 6 months with no significant difference between both groups [Table 7].
Table 7.
Ramus height difference pre- and post-operatively
DISCUSSION
The management of mandibular condylar fracture has opened a wide debate in maxillofacial surgery. The first recommendations for medical treatment of TMJ fractures (conservative treatment with immobilization using a chin cap and a leather cuff) date back to 1500 BC in the Edwin Smith's papyrus.[13] Perthes, in 1924, performed the first surgical treatment by means of plate osteosynthesis.[14]
Nonsurgical management has taken the priority for its reduced percentage of morbidity, easier implementation, prevention of surgical complications, the fewer incidences of ankylosis and vascular necrosis, in comparison with the ORIF. After the development of plate and screw fixation devices, ORIF takes its place. ORIF had better outcomes in terms of adequate anatomical reduction of the fracture, posterior ramus height restoration, restoration of facial symmetry, and early mobilization of the jaw. Till now, there is no consensus for the management of condylar fractures with closed method (MMF only) or open (ORIF) methods.[15]
In this study, males female's ratio was 5.7:1 where males constituted (85%) of the total cases. It is explained by the fact that men constitute the main working force in our society. This supports the statistics of Wong[16] and Badar and Syed[17] where there was male predominance. On the other hand, Zachariades et al., in a review study of 466 condylar fractures cases found no significant difference between males and females.[18] This can be attributed to the fact that more women work outdoors in some occupations which leads to more exposure to craniomaxillofacial fractures.
As regards age groups, adult patients constituted 47.5% of condylar fractures and 52.5% of cases were pediatric patients. In a study done by Iida and Matsuya, Condylar fractures were more frequent in children <14 years of age, especially those below 6 years.[19] In another study, Condylar fractures age groups ranged between 17 and 32 years of age.[20]
RTA were the most common cause of condylar fracture with (57.5%). This data were similar to a study done by Sawazaki et al. who mentioned that RTA was the most common cause of condylar fracture (55.33%).[21] In our study, falls, assault and violence were of less frequency.
The study reported that condylar base fractures were the most common class of the fractures (59.7%), then condylar head fractures came second (28.8%). These results came in accordance with Reddy who reviewed 175 cases of condylar fractures and showed that condylar base fractures were the most common type of fracture.[22]
The isolated condylar fracture was presented in about 25% of cases. The rest of cases were associated with other mandibular fractures. Anterior mandibular fractures were present in half of cases of associated fractures. The frequency of angle (12.5%) and body fractures (10%) came behind. Zachariades et al. had mentioned that condylar fractures resulted from the transmission of force which is not fully absorbed in the area of its primary application.[18]
There are studies that suggest that unerupted lower third molars (M3) increase the fragility of the mandibular angle and simultaneously decrease the risk of condylar fracture.[23] In this thesis, there was no significant difference between the presence of unerupted lower third molar teeth and the angular fracture.
Fractures were treated within the first 7 days after the accident in 67.5% of the cases. The fourth day was the mean time after the accident. There was no effect of the time interval between the time of trauma and time of surgery on the prognosis of the preoperative open bite.
As regards internal fixation, 20% of the cases (8/40) were openly reduced and internally fixed. Three of these patients were pediatrics, and the remaining were adults. All of them were unilateral cases. Seven cases (87.5%) of them were with condylar base fracture, and the remaining one was a neck fracture.
All open treatment group were unilateral cases. On the other hand, the presence of bilateral condylar fractures in isolation did not mandate an ORIF. This was in accordance with management of Kellman.[24] In contrast, Ellis believed that any unilateral condylar fracture could be treated with MMF only. In addition, he did not believe that he could manage bilateral condylar fractures efficiently by MMF.[25]
The criteria for ideal surgical approach are to be less invasive, easy learning, versatile, good exposure, and low incidence of complications.[26]
Retromandibular approach was our choice as it provides direct access to the whole posterior ramus and condylar neck. We preferred it over preauricular incision because we did not need to internally fix diacapitular fracture cases. Preauricular approach gives good exposure of the TMJ. However, it poorly exposes the subcondylar region and makes placement of miniplates a difficult issue. Submandibular approach is a long way from the fractured condyle. Hence, placing screws may require a percutaneous trocar, especially for screw placement in the proximal segment.[25]
Transoral approach with endoscopic assistance has taken its place for management of condylar fracture. This approach has advantages of no scar formation and the minimum injury to the facial nerve. It has disadvantages such as difficulties in maintaining bone fragment stability.[27] Schmelzeisen et al. had reported equivocal results between both ordinary ORIF and endoscopic ORIF.[28]
In this study, we experienced postoperative facial nerve weakness in 25% of cases that were managed by ORIF. One case had complete recovery of facial nerve weakness after 2 months and the other case after 3 months. Manisali et al. noted that postoperative facial nerve weakness occurred in 30% of their cases, of whom 33% had complete recovery within 1 month and the remaining within 3 months.[29] Published reports with level I evidence showed that permanent facial nerve palsy after ORIF of condylar neck and base fractures is not a major concern.[30]
Two straight miniplates (2.0 mm) were used. One was placed parallel to the posterior border of the condylar neck and the other was placed at a 45 angle to the first one. We followed the same management of Tominaga et al., and Pilling et al. to increase the stability of fracture.[31,32]
There was no significant difference between MMF closure period and postoperative interincisal opening. However, we used to close MMF for 28 days (21 days rigid then 7 days with elastics) in closed method cases and for 21 days (14 days rigid then 7 days with elastics) in ORIF cases. In pediatric cases younger than 10 years, elastics were enough to be used during the whole period of MMF application. Vural et al. preferred not to use rigid MMF.[33] Unlikely, Throckmorton advocated closing of MMF.[34] In our opinion, patient's compliance was an important factor for controlling this issue.
A nondisplaced or minimally displaced condylar fractures can be easily managed by keeping the patient on a soft diet only if the patient is compliant with the regimen. However, a patient who was kept on excellent occlusion on elastic MMF may lose this occlusal relationship easily and quickly, if elastics were broken or were not replaced in a timely fashion. The mean postoperative hospitalization time in our group was 2.6 days, similar to that published by other papers.[35]
Needless to say, cases with complications or associated body injuries had a mean hospitalization time for 10 days.
The mean preoperative maximal active interincisal opening for our group (40 cases) was 21.4 mm (range: 12–31 with SD 5.1 mm) while the mean postoperative maximal active interincisal reached 40 mm after 6 months (39.9 in MMF only cases, and 40.5 in ORIF ones). This was supported by the results of Hlawitschka et al. that found that the postoperative mouth opening was not <30 mm in both methods of the management.[36] Furthermore, Joos and Kleinheinz noted that after 12 months the average mouth opening was 41 mm in the nonsurgical group and 45 mm in the surgical group.[37] Rowe and Williams mentioned that a 35 mm postoperative interincisal mouth opening is convenient.[38]
Last but not least, the degree of preoperative angle of coronal displacement of the fractured condyle and preoperative fractured ramus height decrease percentage were not with fixed indicative values. Furthermore, the postoperative results of both variables were not with significance with both methods of management. These results directed us to focus on other variables to be a good comparative variable.[25] Schneider et al. did not support this opinion, and they reported that fractures with a deviation of more than 10°, or a shortening of the ascending ramus of more than 2 mm, should be treated with open reduction and fixation, irrespective of the level of the fracture.[39]
There was a limitation in our study where only forty cases were managed over a 1 year period. However, there were many advantages such as the study contained pediatric cases and it was conducted in a single institution by the same surgeons in all cases. Furthermore, open cases were approached by the same incision.
In summary, management of condylar fracture was adjusted according to the state of occlusion. Cases with good occlusion were managed with MMF. Cases with associated anterior mandibular fractures were corrected first and if occlusion was good MMF would be enough. If occlusion was not corrected, internal fixation would be done [Figure 9]. In future, we will try to expand the number of the cases, increase the period of follow-up and to share the experience with other centers.
Figure 9.
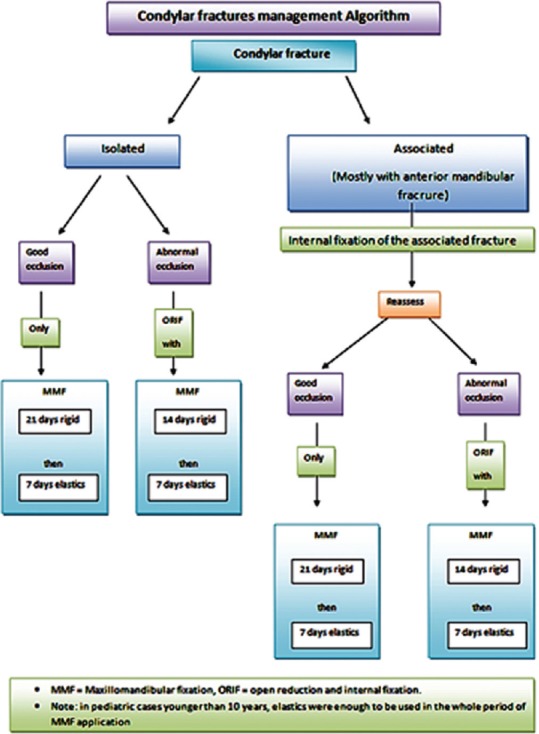
Algorithmic approach for condylar fracture
CONCLUSION
Till now, the condylar fracture has no consensus for treatment. In this study, management was dependent mainly on the condition of occlusion of the mandible. The retromandibular approach was convenient for internal fixation of condylar fracture with a good outcome. In this work, there was no significant difference between closed and open methods in the treatment of condylar fractures.
Consent
Informed consent was obtained from all patients or their parents.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sharif MO, Fedorowicz Z, Drews P, Nasser M, Dorri M, Newton T, et al. Interventions for the treatment of fractures of the mandibular condyle. Cochrane Database Syst Rev. 2010;4:CD006538. doi: 10.1002/14651858.CD006538.pub2. [DOI] [PubMed] [Google Scholar]
- 2.Ghasemzadeh A, Mundinger GS, Swanson EW, Utria AF, Dorafshar AH. Treatment of pediatric condylar fractures: A 20-year experience. Plast Reconstr Surg. 2015;136:1279–88. doi: 10.1097/PRS.0000000000001811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wheeler J, Phillips J. Pediatric facial fractures and potential long-term growth disturbances. Craniomaxillofac Trauma Reconstr. 2011;4:43–52. doi: 10.1055/s-0031-1272901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chrcanovic BR, Abreu MH, Freire-Maia B, Souza LN. 1,454 mandibular fractures: A 3-year study in a hospital in Belo Horizonte, Brazil. J Craniomaxillofac Surg. 2012;40:116–23. doi: 10.1016/j.jcms.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 5.Villarreal PM, Monje F, Junquera LM, Mateo J, Morillo AJ, González C, et al. Mandibular condyle fractures: Determinants of treatment and outcome. J Oral Maxillofac Surg. 2004;62:155–63. doi: 10.1016/j.joms.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 6.Silverman SL. A new operation for displaced fractures at the neck of the mandibular condyle. Dent Cosmos. 1925;67:876–7. [Google Scholar]
- 7.Klatt J, Pohlenz P, Blessmann M, Blake F, Eichhorn W, Schmelzle R, et al. Clinical follow-up examination of surgically treated fractures of the condylar process using the transparotid approach. J Oral Maxillofac Surg. 2010;68:611–7. doi: 10.1016/j.joms.2009.04.047. [DOI] [PubMed] [Google Scholar]
- 8.Hinds EC, Girotti WJ. Vertical subcondylar osteotomy: A reappraisal. Oral Surg Oral Med Oral Pathol. 1967;24:164–70. doi: 10.1016/0030-4220(67)90256-3. [DOI] [PubMed] [Google Scholar]
- 9.Koberg WR, Momma WG. Treatment of fractures of the articular process by functional stable osteosynthesis using miniaturized dynamic compression plates. Int J Oral Surg. 1978;7:256–62. doi: 10.1016/s0300-9785(78)80091-x. [DOI] [PubMed] [Google Scholar]
- 10.Emam HA, Jatana CA, Ness GM. Matching surgical approach to condylar fracture type. Atlas Oral Maxillofac Surg Clin North Am. 2017;25:55–61. doi: 10.1016/j.cxom.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Loukota RA, Eckelt U, De Bont L, Rasse M. Subclassification of fractures of the condylar process of the mandible. Br J Oral Maxillofac Surg. 2005;43:72–3. doi: 10.1016/j.bjoms.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 12.House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93:146–7. doi: 10.1177/019459988509300202. [DOI] [PubMed] [Google Scholar]
- 13.Wolfhart W. Bern/Stuttgart: Papyrus Edwin Smith; 1966. [Google Scholar]
- 14.Perthes G. About fractures and laxations fractures of the jawbone head and their surgical treatment. Verh Dtsch Ges. 1924;133:418–34. [Google Scholar]
- 15.Landes CA, Day K, Lipphardt R, Sader R. Prospective closed treatment of nondisplaced and nondislocated condylar neck and head fractures versus open reposition internal fixation of displaced and dislocated fractures. Oral Maxillofac Surg. 2008;12:79–88. doi: 10.1007/s10006-008-0108-6. [DOI] [PubMed] [Google Scholar]
- 16.Wong KH. Mandible fractures: A 3-year retrospective study of cases seen in an oral surgical unit in Singapore. Singapore Dent J. 2000;23:6–10. [PubMed] [Google Scholar]
- 17.Badar MA, Syed SA. Etiology of mandibular condylar fractures; a study from tertiary care hospital of Lahore. PODJ. 2014;34:42–5. [Google Scholar]
- 18.Zachariades N, Mezitis M, Mourouzis C, Papadakis D, Spanou A. Fractures of the mandibular condyle: A review of 466 cases. Literature review, reflections on treatment and proposals. J Craniomaxillofac Surg. 2006;34:421–32. doi: 10.1016/j.jcms.2006.07.854. [DOI] [PubMed] [Google Scholar]
- 19.Iida S, Matsuya T. Paediatric maxillofacial fractures: Their aetiological characters and fracture patterns. J Craniomaxillofac Surg. 2002;30:237–41. doi: 10.1054/jcms.2002.0295. [DOI] [PubMed] [Google Scholar]
- 20.Newman L. A clinical evaluation of the long-term outcome of patients treated for bilateral fracture of the mandibular condyles. Br J Oral Maxillofac Surg. 1998;36:176–9. doi: 10.1016/s0266-4356(98)90492-2. [DOI] [PubMed] [Google Scholar]
- 21.Sawazaki R, Lima Júnior SM, Asprino L, Moreira RW, de Moraes M. Incidence and patterns of mandibular condyle fractures. J Oral Maxillofac Surg. 2010;68:1252–9. doi: 10.1016/j.joms.2009.03.064. [DOI] [PubMed] [Google Scholar]
- 22.Reddy NV, Reddy PB, Rajan R, Ganti S, Jhawar DK, Potturi A, et al. Analysis of patterns and treatment strategies for mandibular condyle fractures: Review of 175 condyle fractures with review of literature. J Maxillofac Oral Surg. 2013;12:315–20. doi: 10.1007/s12663-012-0428-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Antic S, Saveljic I, Nikolic D, Jovicic G, Filipovic N, Rakocevic Z, et al. Does the presence of an unerupted lower third molar influence the risk of mandibular angle and condylar fractures? Int J Oral Maxillofac Surg. 2016;45:588–92. doi: 10.1016/j.ijom.2014.09.018. [DOI] [PubMed] [Google Scholar]
- 24.Kellman RM. Cummings Otolaryngology Head and Neck Surgery. 5th ed. Philadelphia: Mosby; 2010. Maxillofacial trauma; pp. 318–41. [Google Scholar]
- 25.Ellis E., 3rd Method to determine when open treatment of condylar process fractures is not necessary. J Oral Maxillofac Surg. 2009;67:1685–90. doi: 10.1016/j.joms.2009.03.062. [DOI] [PubMed] [Google Scholar]
- 26.Rao JK, Gehlot N, Siwach V. Evaluation of retro mandibular approach to open reduction and internal fixation of condylar fractures: A Cross-sectional study. J Maxillofac Oral Surg. 2014;13:488–94. doi: 10.1007/s12663-013-0559-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kleinheinz J, Meyer C. London: Quintessence Publishing Company; 2009. Fractures of the Mandibular Condyle: Basic Considerations and Treatment. [Google Scholar]
- 28.Schmelzeisen R, Cienfuegos-Monroy R, Schön R, Chen CT, Cunningham L, Jr, Goldhahn S. Patient benefit from endoscopically assisted fixation of condylar neck fractures – A randomized controlled trial. J Oral Maxillofac Surg. 2009;67:147–58. doi: 10.1016/j.joms.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 29.Manisali M, Amin M, Aghabeigi B, Newman L. Retromandibular approach to the mandibular condyle: A clinical and cadaveric study. Int J Oral Maxillofac Surg. 2003;32:253–6. doi: 10.1054/ijom.2002.0270. [DOI] [PubMed] [Google Scholar]
- 30.Downie JJ, Devlin MF, Carton AT, Hislop WS. Prospective study of morbidity associated with open reduction and internal fixation of the fractured condyle by the transparotid approach. Br J Oral Maxillofac Surg. 2009;47:370–3. doi: 10.1016/j.bjoms.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 31.Tominaga K, Habu M, Khanal A, Mimori Y, Yoshioka I, Fukuda J, et al. Biomechanical evaluation of different types of rigid internal fixation techniques for subcondylar fractures. J Oral Maxillofac Surg. 2006;64:1510–6. doi: 10.1016/j.joms.2006.03.038. [DOI] [PubMed] [Google Scholar]
- 32.Pilling E, Eckelt U, Loukota R, Schneider K, Stadlinger B. Comparative evaluation of ten different condylar base fracture osteosynthesis techniques. Br J Oral Maxillofac Surg. 2010;48:527–31. doi: 10.1016/j.bjoms.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 33.Vural E, Ragland J, Key JM. Manually provided temporary maxillomandibular fixation in the treatment of selected mandibular fractures. Otolaryngol Head Neck Surg. 2008;138:528–30. doi: 10.1016/j.otohns.2007.12.025. [DOI] [PubMed] [Google Scholar]
- 34.Throckmorton GS, Ellis E., 3rd Recovery of mandibular motion after closed and open treatment of unilateral mandibular condylar process fractures. Int J Oral Maxillofac Surg. 2000;29:421–7. [PubMed] [Google Scholar]
- 35.Martini MZ, Takahashi A, de Oliveira Neto HG, de Carvalho Júnior JP, Curcio R, Shinohara EH, et al. Epidemiology of mandibular fractures treated in a Brazilian level I trauma public hospital in the city of São Paulo, Brazil. Braz Dent J. 2006;17:243–8. doi: 10.1590/s0103-64402006000300013. [DOI] [PubMed] [Google Scholar]
- 36.Hlawitschka M, Loukota R, Eckelt U. Functional and radiological results of open and closed treatment of intracapsular (diacapitular) condylar fractures of the mandible. Int J Oral Maxillofac Surg. 2005;34:597–604. doi: 10.1016/j.ijom.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 37.Joos U, Kleinheinz J. Therapy of condylar neck fractures. Int J Oral Maxillofac Surg. 1998;27:247–54. doi: 10.1016/s0901-5027(05)80505-3. [DOI] [PubMed] [Google Scholar]
- 38.Rowe NL, Williams JL. Vol. 1. Edinburgh, United Kingdom: Churchill Livingstone; 1985. Maxillofacial Injuries; pp. 337–63. [Google Scholar]
- 39.Schneider M, Erasmus F, Gerlach KL, Kuhlisch E, Loukota RA, Rasse M, et al. Open reduction and internal fixation versus closed treatment and mandibulomaxillary fixation of fractures of the mandibular condylar process: A randomized, prospective, multicenter study with special evaluation of fracture level. J Oral Maxillofac Surg. 2008;66:2537–44. doi: 10.1016/j.joms.2008.06.107. [DOI] [PubMed] [Google Scholar]


