Abstract
Context and Aim:
In today's world of advanced dentistry, there are various aspects of restorative, esthetic, and surgical processes. Healing of an extraction socket comprises of bone as well as soft-tissue remodeling with maximum dimensional changes occurring during the first 3 months. Platelet-rich fibrin (PRF) was first developed in France as a therapeutic alternative to platelet-rich plasma to overcome many of its limitations. The present study was planned to evaluate and compare wound healing and bone regeneration in extraction sockets with and without PRF.
Materials and Methods:
The present study was carried out on 30 patients selected from the outpatient department over a period of 2½ years starting from May 2013 undergoing extraction of maxillary or mandibular teeth simultaneously to conduct a split-mouth study. The research protocol was approved by the Institutional Ethics Committee governing the use of human subjects in clinical experimentation.
Statistical Analysis Used:
Descriptive and analytical statistics were calculated using Statistical Package for Social Sciences version 19. Chi-square test was used to assess wound healing score in the two groups while paired t-test was used to compare the bone density in the socket and periapical regions at different time intervals, and unpaired t-test was used for the intergroup comparisons. P < 0.05 was considered to be significant while P < 0.001 was considered highly significant.
Results:
Patients in PRF group had better healing index when compared to without PRF group. Use of PRF showed a comparable increase in bone density too.
Conclusion:
An appreciable wound healing and bone regeneration was seen in the experimental group when compared to the control sites where no PRF was used substantiating the use of PRF as an inexpensive autologous material for socket preservation and future rehabilitation. The present study, also, showed that minimal operator expertise was required to conduct the procedure of PRF preparation and grafting when compared to bone harvesting from distant sites. The shorter duration between extractions and further rehabilitation obviates the need for a second procedure.
Keywords: Bone regeneration, platelet-rich fibrin, platelet-rich plasma, postextraction sockets, wound healing
INTRODUCTION
In today's world of advanced dentistry, there are various aspects of restorative, esthetic, and surgical processes. One of the most important competencies is the preservation of the residual alveolar ridge after routine exodontia procedures, failure of which often leads to the compromise of future placement of the implants and further rehabilitation.[1] Prevention of alveolar bone loss postextraction was first described by Greenstein and Ashman and Bruins in the year 1985. Healing of an extraction socket comprises of bone as well as soft-tissue remodeling with maximum dimensional changes occurring during the first 3 months. Platelet-rich plasma (PRP) was initially developed in the 1970s. PRP was shown to increase the rate of bone maturation and improve bone density in addition to promoting wound healing and tissue sealing. However, controversies in the literature regarding the benefits and clinical outcomes of the use of PRP cannot be neglected. Platelet-rich fibrin (PRF) was first developed in France as a therapeutic alternative to PRP to overcome many of its limitations. PRF is easy to prepare, nontoxic, and biocompatible to living tissues and relatively more economical.[2] Extraction sockets undergo resorption and remodeling of the alveolar crest. The repair process results in marked changes in the height and width of the alveolar ridge with an average of 0.7–1.5 mm of vertical and 4.0–4.5 mm of horizontal bone resorption reported. Most of these dimensional alterations take place in the first 3 months following tooth extraction.[3] The bone resorption of jaws after the loss of teeth is seen greatest during the 1st year although up to 4-fold variations have been reported across individuals over a period of 14 months.[4] Many methods have been used during the past two decades to maintain the architecture of residual alveolar ridge like the use of bone, bone substitutes, and collagen plug packed into the extraction sockets sealed with or without isocyanoacrylate.[4] Autologous fibrin concentrates are considered the best to avoid cross-infections, but their use remains very limited owing to the lack of operator competency and a comprehensive understanding about the inherent processes. Hence, the present study was planned to evaluate and compare wound healing and bone regeneration in extraction sockets with and without PRF.
MATERIALS AND METHODS
The present study was carried out on 30 patients selected from the outpatient department over a period of 2½ years starting from May 2013 undergoing extraction of maxillary or mandibular teeth simultaneously to conduct a split-mouth study. Sixty sites were selected in 30 patients and were divided into Group A (Control Group) treated without PRF and Group B (Experimental Group) treated with PRF. The research protocol herein described was approved by the Institutional Ethics Committee governing the use of human subjects in clinical experimentation. Healthy controls in the age group of 20–50 years with chronic periodontal conditions and who had teeth indicated for extractions were included in the study. Patients with immunologic diseases, uncontrolled diabetes mellitus, ongoing chemotherapy or radiotherapy, and those indicated for traumatic extractions were excluded from the study.
Preparation of the patient
The patients included in the study were explained about the procedure, frequency of visits, importance of oral hygiene maintenance, and follow-up visits before the start of the study. A detailed case history of the patient was recorded. After achievement of satisfactory oral hygiene, patients signed a written consent form regarding the extraction procedure followed by placement of PRF on one side and the other side was supposed to be considered in the control group.
Preparation of platelet-rich fibrin
The required quantity of blood (10 ml) was drawn from each patient by vein puncture of the antecubital vein into 10 ml test tubes which were kept without an anticoagulant. Blood was centrifuged in a centrifugal machine for 10 min at 3000 rpm. The resultant product consisted of a topmost straw-colored layer consisting of acellular, PPP, PRF clot in the middle and sedimented red blood cells (RBCs) at the bottom. The uppermost layer was discarded with pipette. Fibrin clots were removed with a tweezer and transferred to sterile dappen dish [Figure 1] while the RBCs were gently scraped away and discarded.
Figure 1.
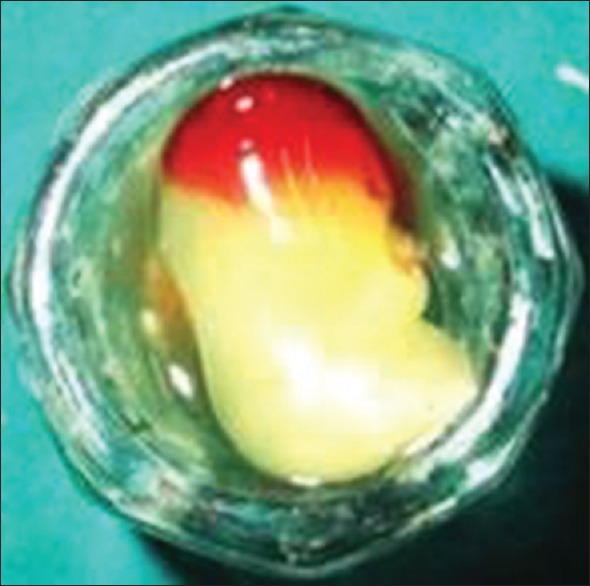
Platelet-rich fibrin in a sterile dappen dish
Surgical technique and postoperative management
Extraction of teeth was performed with emphasis on atraumatic extraction methods. Depending on the site involved, a nerve block was administered with 2% lignocaine with 1:200,000 adrenaline. A periosteal elevator was used to reflect the gingival tissues surrounding the tooth. Tooth was luxated from its socket using periotomes and/or luxators. Appropriate forceps were used depending on the availability of tooth structure to complete the extraction process in the maxilla or the mandible. The Group A sockets were debrided and sutured while Group B sockets were debrided and PRF was grafted [Figure 2] and were, then, sutured. Simple interrupted sutures were given to close the surgical wounds created. For postoperative management, medications were prescribed including 0.2% chlorhexidine mouthrinse to be used twice daily after 24 h for 7 days, capsule amoxicillin 500 mg TDS for 5 days and tablet Ibuprofen 400 mg + tablet paracetamol 325 mg TDS for 5 days. The patients were monitored postoperatively to observe for the healing and soft-tissue closure [Figures 3 and 4].
Figure 2.
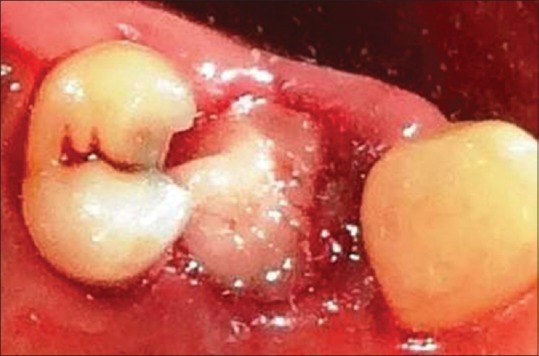
Extraction socket debrided and grafted with platelet-rich fibrin
Figure 3.
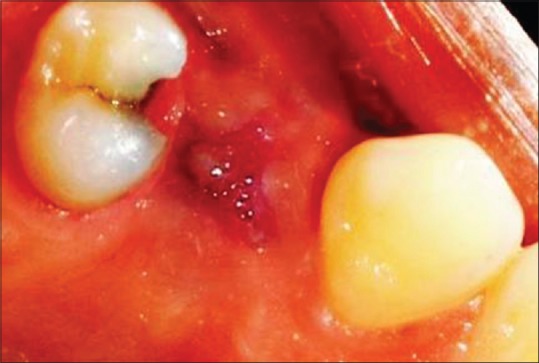
Soft-tissue healing after 1 week
Figure 4.

Soft-tissue healing after 1 week in another case
Postoperative soft-tissue assessment
One week after surgery, sutures were removed and the area was irrigated thoroughly with saline. Symptoms regarding discomfort, pain, and sensitivity were asked to the patient. Any signs of infection including pain, swelling, flap displacement, hematoma, and necrosis were noted and the patients were instructed again to rinse with chlorhexidine mouthrinse twice daily for another 1 week. During follow-up, the patients were evaluated clinically. Clinical assessment was repeated for both control and experimental sites similar to the previous presurgical measurement procedure. Wound healing was assessed using Landry, Turnbull, and Howley index, and a score was given ranging from 1 to 5 where 1 indicated very poor and 5 indicated excellent healing.
Initial cone beam computed tomography evaluation
A postoperative cone beam computed tomography (CBCT) was taken within 24 h of extraction followed by a CBCT 3 months after extraction. The CBCT at 24 h was done to study the density of healthy bone in the apical region of the extracted tooth socket and the socket height. This value obtained served as the baseline for further assessments. The density obtained was, then, compared with the bone formed at the end of 3 months in the extraction socket with and without PRF. The bone density was calculated by taking mean readings in the grayscale measurements from the periapical region.
Bone density and alveolar bone height in periapical region as evaluated on CBCT after 3 months: the readings were noted within 4 mm perimeter beyond the lamina dura/socket wall not including the same. Alveolar bone height was calculated [Figure 5] using stable landmarks including the anterior nasal spine, the infraorbital foramen, maxillary sinus, genial tubercle, mental foramen, and inferior alveolar nerve canal.
Figure 5.
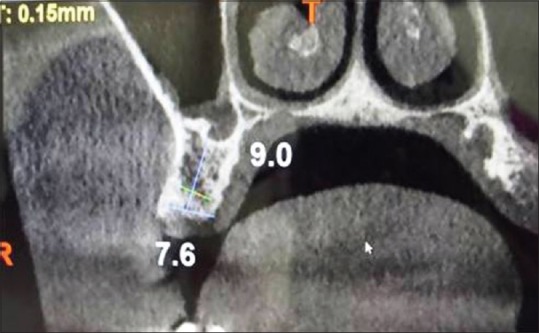
Bone density and alveolar bone height in periapical region as evaluated on cone beam computed tomography after 3 months
Statistical analysis used
Descriptive and analytical statistics were calculated using Statistical Package for Social Sciences (SPSS) version 19 (Chicago, USA). Chi-square test was used to assess wound healing score in the two groups while paired t-test was used to compare the bone density in the socket and periapical regions at different time intervals, and unpaired t-test was used for the intergroup comparisons. P < 0.05 was considered to be significant while P < 0.001 was considered highly significant.
RESULTS
The present study was carried out on 30 patients selected from the outpatient department over a period of 2½ years starting from May 2013 undergoing extraction of maxillary or mandibular teeth simultaneously to conduct a split-mouth study. Sixty sites were selected in 30 patients and were divided into Group A (control group) treated without PRF and Group B (experimental group) treated with PRF.
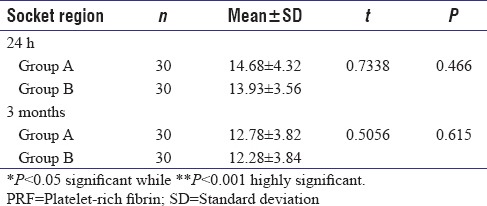
Significantly higher proportion of individuals in PRF group had better healing index when compared to without PRF group (P < 0.001) [Table 1]. The average 24 h and 3 months bone density in the socket region in Group A was found to be 194.82 and 295.87, respectively, while in Group B, similar values were found to be 319.79 and 564.76. Similar values in the periapical region were found to be 518.84 and 613.15 in Group A while 530.39 and 748.02 in Group B. The intra- and inter-group comparisons are shown in Tables 2a, b, 3a, b and Graphs 1a, b, 2a, b, 3a, b, 4a, b. The average 24 h and 3 months alveolar bone height did not differ significantly between Group A and Group B (P > 0.05) [Tables 2a, b, 3c and Graphs 1c, 2c, 5a, b]. Hence, in the present study, extraction sockets grafted with PRF showed statistically significant difference in wound healing and bone density whereas not much difference was seen in alveolar bone height in the two groups. There was a clear evidence, however, of clinical significance observed with respect to alveolar bone height in the experimental group with PRF grafting.
Table 1.
Intergroup comparison of wound healing score after 7 days
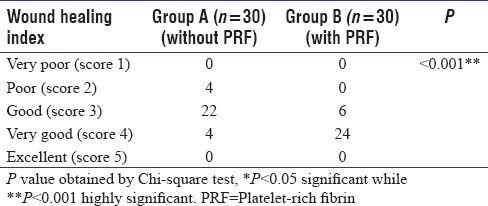
Table 2a.
Comparison of bone density and alveolar bone height in terms of mean±standard deviation in the socket and periapical regions at different time intervals in Group A using paired t-test
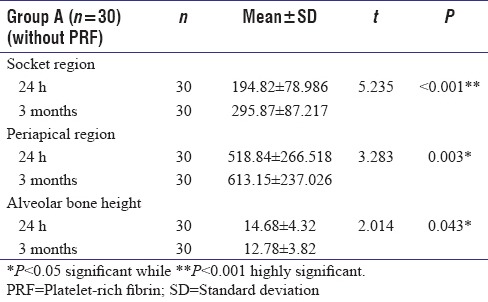
Table 2b.
Comparison of bone density and alveolar bone height in terms of mean±standard deviation in the socket and periapical regions at different time intervals in Group B using paired t-test
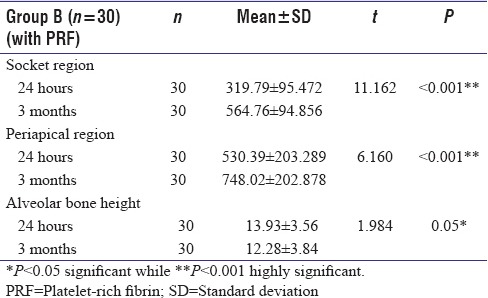
Table 3a.
Comparison of bone density in terms of mean±standard deviation in socket region at different time intervals in the two groups using unpaired t-test
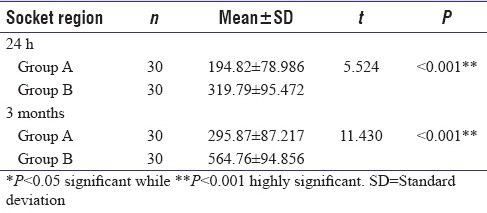
Table 3b.
Comparison of bone density in terms of mean±stanard deviation in periapical region at different time intervals in the two groups using unpaired t-test
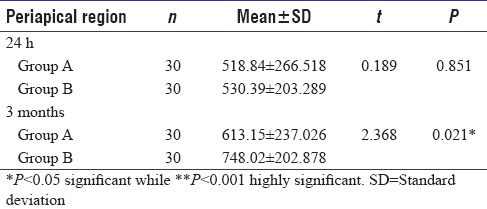
Graph 1.
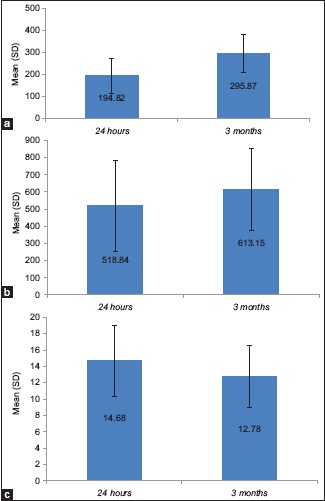
(a-c) Comparison of bone density and alveolar bone height in terms of mean (SD) in the socket and periapical regions at different time intervals in Group A using paired t-test. (a) socket region, (b) periapical region, (c) alveolar bone height
Graph 2.
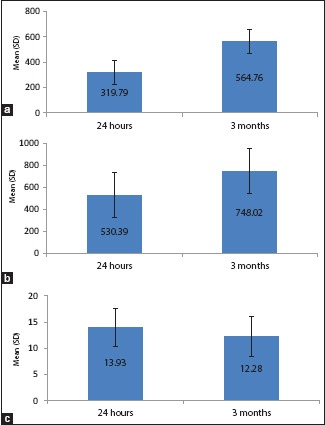
(a-c) Comparison of bone density and alveolar bone height in terms of Mean (SD) in the socket and periapical regions at different time intervals in Group B using paired t-test. (a) Socket region (b) periapical region (c) alveolar bone height
Graph 3.
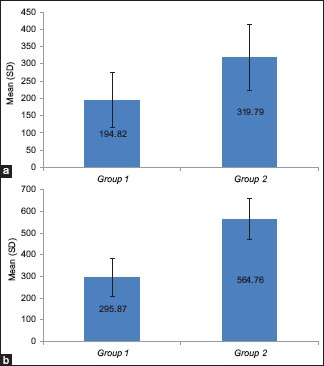
(a and b) Comparison of bone density in terms of mean (SD) in socket region at different time intervals in the two groups using unpaired t-test. (a) 24 h (b) 3 months
Graph 4.
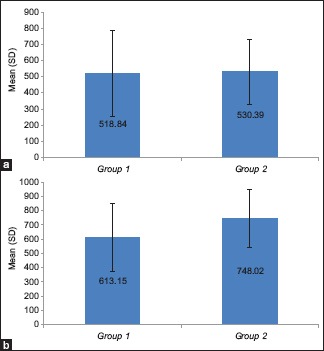
(a and b) Comparison of bone density in terms of mean (SD) in periapical region at different time intervals in the two groups using unpaired t-test. (a) 24 h (b) 3 months
Table 3c.
Comparison of alveolar bone height in terms of mean±standard deviation at different time intervals in the two groups using unpaired t-test
Graph 5.
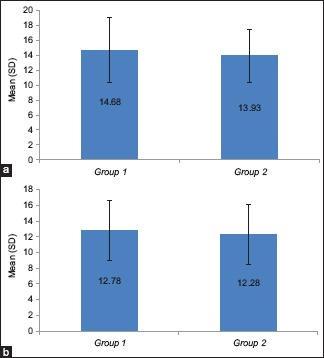
(a and b) Comparison of alveolar bone height in terms of mean (SD) in periapical region at different time intervals in the two groups using unpaired t-test. (a) 24 h (b) 3 months
DISCUSSION
Numerous studies and researches have been done on tooth socket healing processes; however, most of these are histological studies with less emphasis on radiographic evaluations. PRF is a platelet concentrate collected on a single fibrin membrane that contains all the constituents favorable for healing. The scientific rationale behind the use of platelet preparations lies in the fact that the platelet serves as a reservoir of many growth factors that are known to play a crucial role in hard- and soft-tissue healing process. PRF stimulates human osteoblastic proliferation, and histology has shown it to have an effect on neoangiogenesis. PRF is a second-generation platelet concentrate and is a gel-like matrix that contains high concentration of nonactivated, functional, intact platelets contained within a fibrin matrix that releases a relatively constant concentration of growth factors over a period of 7 days. In a membrane form, it can be used as fibrin bandage, serving as a matrix to accelerate the healing of wound edges. It is relatively inexpensive with chairside preparation which is quite easy and with processing being fast and simple. On filling of a tooth socket by PRF, neovascularization establishes through the PRF clot and an epithelial covering develops.[3] Despite the infectious and inflammatory potential of extraction sockets, rapid healing of the wound occurs without pain, swelling, and other attending signs of inflammation and infectious processes. Similar clinical results were found in the present study in which healing occurred without untoward symptoms. The results of the present study were in accordance with the results of the study conducted by Moya-Villaescusa and Sánchez-Pérez[5] which showed PRF to stimulate soft-tissue healing process seen clinically when applied to the fresh extraction sockets. In addition, it seemed to reduce alveolar ridge resorption following tooth extractions and to positively influence socket healing over a 3-month period.
An extraction socket contains both hard and soft tissues which heal concomitantly with a certain amount of lag in the healing processes. Toward the end of the 1st week, the clot retracts and breaks down as granulation tissue replaces the same. The granulation tissue covers the superior aspect of the alveolar bone ridge usually, and the epithelium proliferates along the soft-tissue wound margins. PRF compared with other platelet concentrates including PRP does not require any anticlotting or gelling agents, and the naturally forming PRF clot has a dense and complex three-dimensional architecture that contains not only platelets but also leukocytes.[6]
Healing index scores are based on the basis of existing erythema, presence of granulation tissue, bleeding, suppuration, and epithelialization. In the present study, during the postoperative follow-up visits, the surgical wounds created were evaluated using the Landry, Turnbull, and Howley index, and a score was given ranging from 1 to 5 where 1 indicated very poor and 5 indicated excellent healing.[7] The mean soft-tissue change assessment showed that significantly higher proportion of sites from PRF group at 7th postoperative day showed better healing index when compared to the sites from the non-PRF group.
Osteoid, in an extraction socket, is evident during a sound healing process at the apical portion (at the base) of the socket as uncalcified bony spicules after a vascular network are formed, and young connective tissue is formed at the end of the 1st week. The American Association of Oral and Maxillofacial Radiology recommends cross-sectional views for planning dental implants, and this in combination with the ease of accessibility, handling, and low radiation dose that the CBCT imaging offers has the potential for vertical scanning in a natural seated position in high resolution (e.g., bone trabeculae, periodontal ligament, and root formation imaging). Furthermore, it has additional advantages of offering lower dose of radiation than the multislice computed tomography (MSCT), less disturbance from the metal artifacts, reduced costs compared with MSCT, easier accessibility, in-office imaging, easier handling, small footprint, Digital Imaging and Communications in Medicine compatibility, being user friendly in postprocessing and viewing and better saving of energy when compared with MSCT.[8] The present study utilized the potential of CBCT in the evaluation of bone formed in extraction sockets. Gupta J and Ali SP,[8] also, found that the CBCT scans were more accurate than conventional radiography. Furthermore, Alhijazi and Mohammed[9] and Dohan et al.[10] in their study showed that the sites treated with PRF had complete osseous fill of the extraction sockets in 3 weeks, and similar observations were made in the present study, too, which showed faster bone healing in the form of bone density compared to the control group when evaluated on CBCT scans.
In the coronal portions of the socket, the width of the osseous walls is thin and internal resorption might lead to a reduction of the alveolar ridge after normal healing. The inflammatory or foreign body reaction might cause resorption of the internal walls of the socket. With PRF alone as the graft material, the healing process is more rapid and does not have an associated foreign body reaction adversely affecting the amount of bone formation. Lekovic et al.[11] quantified the changes in alveolar width and height and recorded a 0.38 mm (11.59%) loss of height after 4–6 months of healing. The results of the study conducted by Clozza et al.[12] reported a loss of crestal bone height and width which mainly occurred within the first 3 months after tooth extraction with no difference according to location (maxilla or mandible). Substantial vertical reduction was, also, noted by Agarwal et al.[13] in their study which was found to be close to 2 mm. The present study showed a mean radiographic measurement of alveolar bone height reduction of 0.06±0.25mm where in the average height did not reduce significantly at 3 month post-treatment follow-up with use of PRF. It, however, concurred with other studies as it did not obtain a statistical significance.
The density of bone in a normal socket achieves its maximum at 5 weeks in histological sections.[14] The density of bone was compared to the bone formed at the end of 3 months in the extraction socket with and without PRF and also, the influence of PRF, if any, in the apical area just adjacent to the placement of PRF which showed a comparable increase in density suggesting possible early rehabilitation in sockets with use of PRF. The radiographic results obtained in the present study indicated that a statistically significant bone fill was obtained in the experimental group compared to the baseline at 3 months postoperatively which were concurrent with the results from similar studies.[7,9,15,16,17]
CONCLUSION
The present study was designed to evaluate and compare wound healing and bone regeneration in extraction sockets with and without PRF utilizing the potential of the CBCT in determining the bone density and alveolar bone height as compared to the earlier methods for predictable outcomes with and without PRF. In the study, appreciable amount of bone regeneration was seen in the experimental group when compared to the control sites where no PRF was used substantiating the use of PRF as an inexpensive autologous material for socket preservation and future rehabilitation. The present study, also, showed that minimal operator expertise was required to conduct the procedure of PRF preparation and grafting when compared to bone harvesting from distant sites. The shorter duration between extractions and further rehabilitation obviates the need for a second procedure. The major limitation of the present study was with obtaining a statistical significance due to a limited number of individuals included.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cohen ES, editor. Atlas of Cosmetic and Reconstructive Periodontal Surgery. 1st ed. Philadelphia, PA: Lippincott Williams and Wilkins; 1988. Socket preservation. [Google Scholar]
- 2.Marrelli M, Tatullo M. Influence of PRF in the healing of bone and gingival tissues. Clinical and histological evaluations. Eur Rev Med Pharmacol Sci. 2013;17:1958–62. [PubMed] [Google Scholar]
- 3.Jiing HZ, Chung HT, Yu CC. Clinical and histologic evaluation of healing in an extraction socket filled with platelet-rich fibrin. J Dent Sci. 2011;6:116–22. [Google Scholar]
- 4.Chan HL, Lin GH, Fu JH, Wang HL. Alterations in bone quality after socket preservation with grafting materials: A systematic review. Int J Oral Maxillofac Implants. 2013;28:710–20. doi: 10.11607/jomi.2913. [DOI] [PubMed] [Google Scholar]
- 5.Moya-Villaescusa MJ, Sánchez-Pérez A. Measurement of ridge alterations following tooth removal: A radiographic study in humans. Clin Oral Implants Res. 2010;21:237–42. doi: 10.1111/j.1600-0501.2009.01831.x. [DOI] [PubMed] [Google Scholar]
- 6.Del Corso M, Mazor Z, Rutkowski JL, Dohan Ehrenfest DM. The use of leukocyte- and platelet-rich fibrin during immediate postextractive implantation and loading for the esthetic replacement of a fractured maxillary central incisor. J Oral Implantol. 2012;38:181–7. doi: 10.1563/AAID-JOI-D-12-CL.3802. [DOI] [PubMed] [Google Scholar]
- 7.Singh A, Kohli M, Gupta N. Platelet rich fibrin: A novel approach for osseous regeneration. J Maxillofac Oral Surg. 2012;11:430–4. doi: 10.1007/s12663-012-0351-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta J, Ali SP. Cone beam computed tomography in oral implants. Natl J Maxillofac Surg. 2013;4:2–6. doi: 10.4103/0975-5950.117811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alhijazi AY, Mohammed SA. Evaluation the effect of platelet rich fibrin matrix on bone healing. J Bagh Coll Dent. 2011;23:65–70. [Google Scholar]
- 10.Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e37–44. doi: 10.1016/j.tripleo.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Lekovic V, Milinkovic I, Aleksic Z, Jankovic S, Stankovic P, Kenney EB, et al. Platelet-rich fibrin and bovine porous bone mineral vs. Platelet-rich fibrin in the treatment of intrabony periodontal defects. J Periodontal Res. 2012;47:409–17. doi: 10.1111/j.1600-0765.2011.01446.x. [DOI] [PubMed] [Google Scholar]
- 12.Clozza E, Biasotto M, Cavalli F, Moimas L, Di Lenarda R. Three-dimensional evaluation of bone changes following ridge preservation procedures. Int J Oral Maxillofac Implants. 2012;27:770–5. [PubMed] [Google Scholar]
- 13.Agarwal G, Thomas R, Mehta D. Postextraction maintenance of the alveolar ridge: Rationale and review. Compend Contin Educ Dent. 2012;33:320–4. 326. [PubMed] [Google Scholar]
- 14.Amler MH. The time sequence of tissue regeneration in human extraction wounds. Oral Surg Oral Med Oral Pathol. 1969;27:309–18. doi: 10.1016/0030-4220(69)90357-0. [DOI] [PubMed] [Google Scholar]
- 15.Simon BI, Gupta P, Tajbakhsh S. Quantitative evaluation of extraction socket healing following the use of autologous platelet-rich fibrin matrix in humans. Int J Periodontics Restorative Dent. 2011;31:285–95. [PubMed] [Google Scholar]
- 16.Pagni G, Pellegrini G, Giannobile WV, Rasperini G. Postextraction alveolar ridge preservation: Biological basis and treatments. Int J Dent 2012. 2012 doi: 10.1155/2012/151030. 151030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kubilius M, Kubilius R, Gleiznys A. The preservation of alveolar bone ridge during tooth extraction. Stomatologija. 2012;14:3–11. [PubMed] [Google Scholar]


