Abstract
Aim:
The aim is to study the assessment of feasibility of medial sural artery perforator (MSAP) free flap for head and neck reconstruction at our center.
Materials and Methods:
Oral cancer patients with squamous cell carcinoma of the tongue, buccal mucosa, and floor of mouth cancer attending our center were reconstructed using MSAP flap after oncologic resection. Handheld 8 MHz Doppler was used to identify the perforator preoperatively.
Results:
We reconstructed 10 patients using MSAP flap. The flap was designed according to defect and donor site was primarily closed in all cases. Excellent results were seen in nine patients reconstructed with MSAP flap without any postoperative complication. Flap failure occurred in one patient due to venous thrombosis. The thickness of flap ranged from 4 to 8 mm. The vascular pedicle length ranged from 9 to 13 cm.
Conclusion:
The MSAP flap is appropriate for medium-sized oral defect reconstruction, with a long pedicle of matching caliber, adequate tissue volume, and minimal donor-site morbidity which makes it comparable to other microvascular free flaps such as radial artery free flap (RAFF) and anterolateral thigh flap.
Keywords: Free flap, head and neck reconstruction, medial sural artery perforator flap, perforator flap
INTRODUCTION
The medial sural artery perforator (MSAP) flap is a fasciocutaneous flap and it was first described by Cavadas et al. in 2001 as a refinement of the gastrocnemius flap.[1] Kao et al. established its use in head and neck reconstruction on anatomic basis and its versatility of application.[2] It is a useful alternative to radial forearm flap providing hairless tissue and less donor-site morbidity. Hallock in 2001 explained the perforator anatomy of MSAP flap.[3] Okamoto et al. in 2007 reported about the perforators present in MSAP flap.[4] For the medium-sized defect, MSAP flap is very reliable for soft-tissue defect. Nugent et al. used MSAP flap and reported its superiority to RAF flap for head and neck reconstruction.[5] The gastrocnemius muscle is supplied by medial and lateral sural arteries, which give off some myocutaneous perforators that supply the skin of the posterior calf. MSAP can be raised with this vessel without sacrificing gastrocnemius muscle.[1,6,7]
Vascular anatomy
The medial sural artery (MSA) arises from the popliteal artery, and after a few centimeters, the vessel enters and runs through the medial belly of the gastrocnemius muscle and some branches “perforate” through to the skin. The MSA usually divides into lateral and medial branches, and this usually occurs in the substance of the muscle (85%). Some surgeons prefer to use the lateral row of perforators because it is usually dominant. Muscle devascularization is not a major concern as there are other vascular supplies to the muscle apart from the MSA. There are usually 2–4 perforators of about 1 mm diameter that are concentrated at an area 4.5 cm from the midline and 8–12 cm from the popliteal fossa crease. The first perforator is usually 8 cm along a line drawn from the middle of the popliteal crease to the medial malleolus. Markings should be made with the patient standing straight [Figure 1]. The artery is about 2 mm in diameter at its origin. Depending on the perforator chosen and amount of retrograde dissection, the pedicle length ranges from 9 to 16 cm [Figure 2]. The posterior cutaneous nerve of the thigh can also be harvested in instances where a sensate flap is required.
Figure 1.

Marking of flap (patient 1)
Figure 2.

Flap harvest (patient 2)
MATERIALS AND METHODS
This is a prospective case series of the use of the free MSAP flap for intraoral soft-tissue reconstructions following cancer excision from a tertiary head and neck cancer center in India. The aim of the study was to report our experience of the flap for soft-tissue intraoral reconstructions. A total of 10 patients with squamous cell carcinoma (SCC) of oral cavity underwent excision of tumor along with neck dissection, and MSAP free flap was used for reconstruction. The patients’ lower limb was examined, in particular, for the pliability of the tissues by pinching the skin together to assess laxity to allow primary closure. Perforators were preoperatively identified by handheld Doppler (8 MHz). The size of the flap was designed according to the defect size [Figures 3 and 4]. We used a tourniquet in all cases to harvest flap. Initially, incision placed in the lateral side of the flap to locate the perforators of appropriate size. After getting appropriate perforator, flap design is adjusted and perforator is traced up to the main trunk. The vascular pedicle length, number of perforator, and flap size were recorded with calipers. The flap is inset into the intraoral defect, and the microvascular anastomoses are performed. Facial or superior thyroid artery was used for arterial anastomosis and one vein with bigger caliber was used for venous anastomosis. The donor site is closed primarily over a drain. Postoperative monitoring of the flap was done by clinical assessment, handheld Doppler, and prick test [Figures 5 and 6]. The patient is able to mobilize with full weight-bearing on the 1st postoperative day. Some challenges may encounter while harvest of this MSAP flap such as length and caliber of the pedicle is sometimes very small and anastomosis may be difficult. One may encounter very tiny skin perforator which is very difficult to dissect up to the feeder vessel, and extreme care is taken not to injure the perforator while dissection.
Figure 3.

Flap harvest (patient 1)
Figure 4.
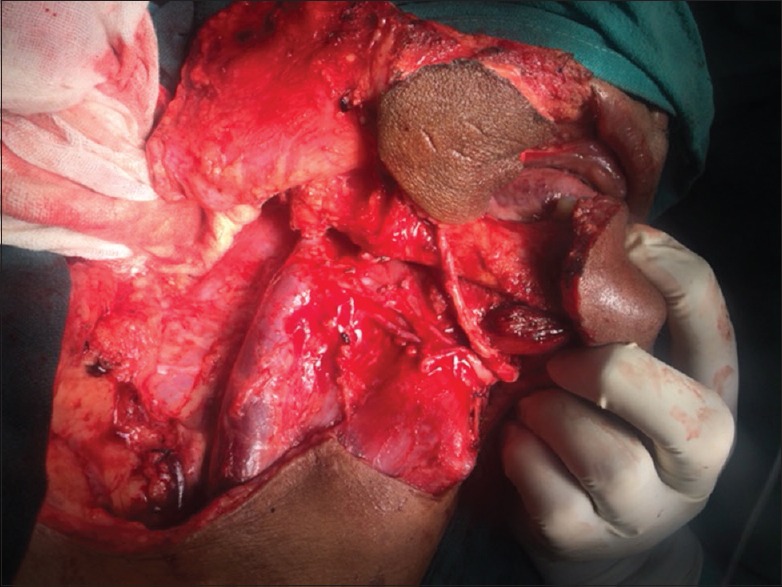
Flap insertion (patient 2)
Figure 5.

Prick test (patient 1)
Figure 6.

Prick test (patient 2)
RESULTS
Between August 2015 and December 2016, 10 free MSAP flaps were used to reconstruct intraoral soft-tissue defects [Table 1]. There were six male and four female patients with the median age of 37.6 years (from 22 to 55 years). All patients had oral SCC. The most common site of tumor resection was the tongue (5 cases), followed by buccal mucosa (3 cases) and floor of mouth (2 cases). Flap failed in one case due to venous thrombosis, rest all nine flaps survived. [Figures 7 and 8]. Failed flap was removed and defect was covered with split-thickness skin graft. The MSAP flap thickness was found from 4 to 7 mm (5.3 mm mean). The length of the vascular pedicle ranged from 8 to 13 cm (10.2 cm mean) which provides sufficient length during vessel anastomosis. Arterial diameter ranged from 1.1 to 2 mm and venous diameter of both veins in pedicle ranged from 1.5 to 3.5 mm in size. The number of perforators range from 1 to 3 and 70% flap was based on two perforators. Primary closure attained in all cases.
Table 1.
Result of our study
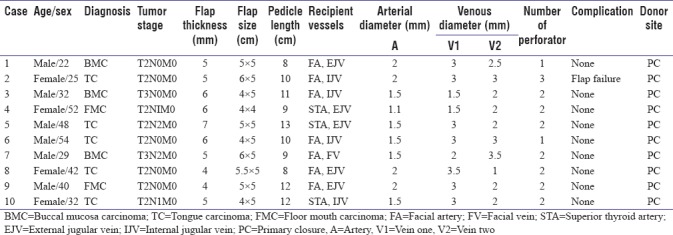
Figure 7.

Postoperative 6 months of medial sural artery perforator flap
Figure 8.

Postoperative 6 months (patient 2)
DISCUSSION
The use of free flaps in reconstructive surgery is now common. Perforator flaps have several advantages over traditional musculocutaneous flaps. First, as muscle is preserved rather than being incorporated into the flap, there is less donor-site weakness and morbidity.[1] There are various benefits of MSAP flap over RAF flap for oral reconstruction reported by Kao et al.[8,9,10] The disadvantage of RAFF is that it sacrifices the radial artery, and hence, the chances of donor-site morbidity increases.[8] MSAP flap is thin pliable flap, long vascular pedicle, less hair-bearing skin, and easy dissection with minimal donor-site morbidity. Sometimes, the removal of the gastrocnemius muscle results in weakness of the lower limb which affects the gait. About 10% morbidity was reported by Cavadas et al. by the removal of the gastrocnemius muscle.[1] In our study, the thickness of the flap was ranged from 4 to 8 mm, which gave satisfactory adaptation to the oral defect functionally and esthetically. Shen et al.[11] in a case reported that MSAP flap attained an acceptable appearance and it supplies enough skin for oral defects. He et al.[12] in their prospective study on tongue reconstruction reported that it gives minimal scarring and functional problem. According to our study, the length of the vascular pedicle is between 8 and 9 cm. Wong et al., on their clinical study on versatility of flap to cover defects around knee, concluded that MSAP flap was very efficient with long pedicle length, small volume, and left unsightly scar.[13] The main disadvantage of using anterolateral thigh flap is that it is bulky, so as to provide a taut surface for oral reconstruction, and patients also suffer from dark hair growth in oral cavity.[14,15]
According to our experience, handheld Doppler is very useful for the identification of main perforator at anatomical sites as it is easy and simple method for mapping. He et al. also supported Doppler sonography for mapping the perforators.[12] Shen et al. also reported that handheld Doppler is inexpensive and reliable device for perforator marking. Some other studies like Ensat et al. and Stekelenburg et al. shows opposite result and points that it is not a reliable technique as it shows variable results.[16,17] Yang et al. used computed tomography angiography (CTA) in anterolateral thigh perforator flap transplantation They reported significant reduction in complication of flap using CTA as comparison to conventional group.[18] Wolff et al. recommend the use of magnetic resonance angiograms to locate perforators preoperatively.[19]
Wong et al. proposed that sometimes, the located perforator does not have an artery with them.[20] Surgeon should be aware of the condition and flap can be harvested based on another perforator. If the graft size is wider than 5 cm, then the donor site is grafted with split-thickness graft.[13]
CONCLUSION
According to our experience, we believe that the MSAP flap is reliable flap for head and neck reconstruction. It is good alternative for tongue, buccal mucosa, and floor of mouth reconstruction. The advantages are its thin and pliable skin, good vascular pedicle length, and hairless flap with minimal donor-site morbidity making it comparable to RAFF and ALT flap. Handheld Doppler is a reliable device for mapping the perforator.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cavadas PC, Sanz-Giménez-Rico JR, Gutierrez-de la Cámara A, Navarro-Monzonís A, Soler-Nomdedeu S, Martínez-Soriano F, et al. The medial sural artery perforator free flap. Plast Reconstr Surg. 2001;108:1609–15. doi: 10.1097/00006534-200111000-00027. [DOI] [PubMed] [Google Scholar]
- 2.Kao HK, Chang KP, Chen YA, Wei FC, Cheng MH. Anatomical basis and versatile application of the free medial sural artery perforator flap for head and neck reconstruction. Plast Reconstr Surg. 2010;125:1135–45. doi: 10.1097/PRS.0b013e3181d180ac. [DOI] [PubMed] [Google Scholar]
- 3.Hallock GG. Anatomic basis of the gastrocnemius perforator-based flap. Ann Plast Surg. 2001;47:517–22. doi: 10.1097/00000637-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Okamoto H, Sekiya I, Mizutani J, Otsuka T. Anatomical basis of the medial sural artery perforator flap in Asians. Scand J Plast Reconstr Surg Hand Surg. 2007;41:125–9. doi: 10.1080/02844310601159972. [DOI] [PubMed] [Google Scholar]
- 5.Nugent M, Endersby S, Kennedy M, Burns A. Early experience with the medial sural artery perforator flap as an alternative to the radial forearm flap for reconstruction in the head and neck. Br J Oral Maxillofac Surg. 2015;53:461–3. doi: 10.1016/j.bjoms.2015.02.023. [DOI] [PubMed] [Google Scholar]
- 6.Chen SL, Chen TM, Lee CH. Free medial sural artery perforator flap for resurfacing distal limb defects. J Trauma. 2005;58:323–7. doi: 10.1097/00005373-200502000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Umemoto Y, Adachi Y, Ebisawa K. The sural artery perforator flap for coverage of defects of the knee and tibia. Scand J Plast Reconstr Surg Hand Surg. 2005;39:209–12. doi: 10.1080/02844310410004964. [DOI] [PubMed] [Google Scholar]
- 8.McMahon JD, MacIver C, Smith M, Stathopoulos P, Wales C, McNulty R, et al. Postoperative complications after major head and neck surgery with free flap repair – Prevalence, patterns, and determinants: A prospective cohort study. Br J Oral Maxillofac Surg. 2013;51:689–95. doi: 10.1016/j.bjoms.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 9.Avery CM. Review of the radial free flap: Is it still evolving, or is it facing extinction? Part one: Soft-tissue radial flap. Br J Oral Maxillofac Surg. 2010;48:245–52. doi: 10.1016/j.bjoms.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Kao HK, Chang KP, Wei FC, Cheng MH. Comparison of the medial sural artery perforator flap with the radial forearm flap for head and neck reconstructions. Plast Reconstr Surg. 2009;124:1125–32. doi: 10.1097/PRS.0b013e3181b457cf. [DOI] [PubMed] [Google Scholar]
- 11.Shen XQ, Lv Y, Shen H, Lu H, Wu SC, Lin XJ, et al. Endoscope-assisted medial sural artery perforator flap for head and neck reconstruction. J Plast Reconstr Aesthet Surg. 2016;69:1059–65. doi: 10.1016/j.bjps.2016.01.029. [DOI] [PubMed] [Google Scholar]
- 12.He Y, Jin SF, Zhang ZY, Feng SQ, Zhang CP, Zhang YX, et al. A prospective study of medial sural artery perforator flap with computed tomographic angiography-aided design in tongue reconstruction. J Oral Maxillofac Surg. 2014;72:2351–65. doi: 10.1016/j.joms.2014.05.019. [DOI] [PubMed] [Google Scholar]
- 13.Wong JK, Deek N, Hsu CC, Chen HY, Lin CH, Lin CH, et al. Versatility and “flap efficiency” of pedicled perforator flaps in lower extremity reconstruction. J Plast Reconstr Aesthet Surg. 2017;70:67–77. doi: 10.1016/j.bjps.2016.09.028. [DOI] [PubMed] [Google Scholar]
- 14.Kekatpure VD, Trivedi NP, Shetkar G, Manjula BV, Mathan Mohan A, Kuriakose MA, et al. Single perforator based anterolateral thigh flap for reconstruction of large composite defects of oral cavity. Oral Oncol. 2011;47:517–21. doi: 10.1016/j.oraloncology.2011.03.023. [DOI] [PubMed] [Google Scholar]
- 15.Kekatpure VD, Manjula BV, Mathias S, Trivedi NP, Selvam S, Kuriakose MA, et al. Reconstruction of large composite buccal defects using single soft tissue flap – Analysis of functional outcome. Microsurgery. 2013;33:184–90. doi: 10.1002/micr.22063. [DOI] [PubMed] [Google Scholar]
- 16.Ensat F, Babl M, Conz C, Fichtl B, Herzog G, Spies M, et al. Doppler sonography and colour doppler sonography in the preoperative assessment of anterolateral thigh flap perforators. Handchir Mikrochir Plast Chir. 2011;43:71–5. doi: 10.1055/s-0030-1255071. [DOI] [PubMed] [Google Scholar]
- 17.Stekelenburg CM, Sonneveld PM, Bouman MB, van der Wal MB, Knol DL, de Vet HC, et al. The hand held doppler device for the detection of perforators in reconstructive surgery: What you hear is not always what you get. Burns. 2014;40:1702–6. doi: 10.1016/j.burns.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 18.Yang JF, Wang BY, Zhao ZH, Zhou P, Pang F, Sun WD, et al. Clinical applications of preoperative perforator planning using CT angiography in the anterolateral thigh perforator flap transplantation. Clin Radiol. 2013;68:568–73. doi: 10.1016/j.crad.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 19.Wolff KD, Bauer F, Kunz S, Mitchell DA, Kesting MR. Superficial lateral sural artery free flap for intraoral reconstruction: Anatomic study and clinical implications. Head Neck. 2012;34:1218–24. doi: 10.1002/hed.21885. [DOI] [PubMed] [Google Scholar]
- 20.Wong MZ, Wong CH, Tan BK, Chew KY, Tay SC. Surgical anatomy of the medial sural artery perforator flap. J Reconstr Microsurg. 2012;28:555–60. doi: 10.1055/s-0032-1315778. [DOI] [PubMed] [Google Scholar]


