Abstract
To explore the prognostic related factors and mechanisms of gastric cancer (GC), we performed the systematic analysis with integrated bioinformatics tools based on multiple on-line datasets. With uni-variate COX analysis, we screened out 37 survival hazardous genes in GC. Further GO assays disclosed that the signatures related with extracellular matrix and structure, and the functions of “cell adhesion molecule binding” and “integrin binding” were the vital mechanisms of disease progression, and tissue inhibitor of metalloproteinase-2 (TIMP2) was the potential biomarker for prognosis. Based on GSEA, GSVA and GCN, TIMP2 was demonstrated to interact with multiple integrin pathways and involve in the regulation of EMT, cell adhesion, and angiogenesis of GC. The associations of TIMP2 expression with reduced OS and RFS of patients were declared by Kaplan-Meier analysis, and further confirmed by 1000 internal bootstrap replications and external KM plotter analysis. With multi-variate COX regression and time-dependent ROC analysis, we validated the prediction independency and capacity of TIMP2 for prognosis. The relationships of TIMP2 with clinicopathological characteristics were also uncovered. Taken together, our findings identify TIMP2 as the novel candidate biomarker for poorer outcome of GC patients, and revealed the underlying functions of TIMP2 and the potential mechanisms for GC progression.
Introduction
Gastric cancer (GC) is one of the most fetal diseases worldwide, and accounts for the fourth most common cancer and the second leading cause of cancer death1. High rate of advanced-stage diagnosis, treatment resistance, and later recurrence and metastasis greatly contribute to the poor prognosis of patients2. However, neither the traditional extensively used clinicopathological systems nor the novel molecular signatures could well interpret the malignant behavior and characteristics of GC, based on their limited accuracy and availability for the prognosis prediction in patients3,4. Therefore, much of the underlying mechanisms for GC development are still unclear, and more prognosis biomarkers of GC are awaiting uncovered.
High throughput genomic studies based on big cohort could present treasurable clues for the discovery of cancer development mechanisms and novel prognostic factors4. The data from the Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO) and Sequence Read Archive (SRA) involve dozens of cancer types and hundreds of cases for each cancer type, and have become the important study resources based on the great superiority of more variety and objectivity5. Moreover, mutual validations with different datasets and computational methods could be performed to reduce the false negative rate of big data assays6. Previously, multiple survival assays using online genomic data have been performed in GC7,8. However, most studies were more focused on data mining in a single dataset; lack of systematic and overall evaluation of related data; and absence of pre-analysis case selection according to clinicopathological information, thus provided the results with limited applicability and reliability.
In the current study, we systematically evaluated the prognosis related signatures and biomarkers of GC by combining integrated bioinformatics tools and mutual confirmation method based on multiple genomic-profiling datasets from TCGA and GEO. Using the whole mRNA expression profiles from 872 patients, 37 genes were filtered out to be related with worse outcomes of GC patients by COX assays. Based on further genetic ontology (GO) analysis, the extracellular matrix- related genes with the molecular functions of “cell adhesion molecule binding” and “integrin binding” might be vital for patients’ prognosis, and tissue inhibitor of metalloproteinase-2 (TIMP2) were supposed to be the potential key biomarker for GC progression. Moreover, TIMP2 was proved to increase the prediction accuracy of traditional clinicopathological characteristics (CPPs) for GC prognosis. Subsequent Gene Set Enrichment Analysis (GSEA), gene set variation analysis (GSVA) and co-expression network (GCN) assays shed light on the underlying functions of TIMP2 in GC. The results might enrich our knowledge on the tumorigenesis and development of GC, and also present more evidences to clarify the paradoxical role of TIMP2 in cancers.
Results
Basic characteristics of patients
The analysis procedure of the current study was shown in Supplementary Fig. 1, and the GC patients with the available data for the sequential analysis were selected (Supplementary Table 1). Among the 300 patients in GSE62554, most have tumors at T2 (62.4%), N1 (43.7%), M0 (91.0%), and TNM III (31.7%) stage. In GSE15459, most of the 192 tumors were intestinal (51.6%) type and stage III (37.5%). Most of the 380 patients in TCGA dataset have tumors with stage T3 (45.5%), N0 (30.8%), M0 (89.7%), and III (43.9%). The deaths occurred in GSE62254, GSE15459, and TCGA cohorts were135 (45%), 95 (49%), and 147(40%), respectively.
Identification of survival related genes and the key signatures
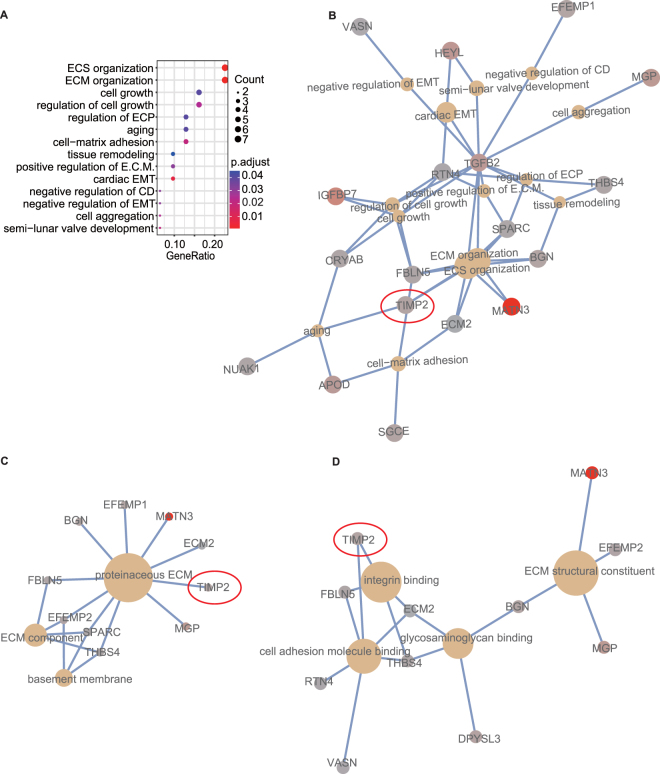
According to the uni-variate COX and KM plotter analysis, the 3 datasets shared totally 38 survival-related genes, including 1 protective (hazard ratio (HR) < 1, E2F2) and 37 hazardous (HR > 1) genes (Supplementary Table 2). In the GO analyses using the 37 hazardous genes, totally 14 biological process (BP) terms were significantly enriched, with “extracellular structure (ECS) organization” and “extracellular matrix (ECM) organization” as the most prominent signatures (Fig. 1A and B). In the GO analysis for cellular component (CC), ECM related signatures were found to be enriched (Fig. 1C). Moreover, GO-molecular function (MF) analysis identified “cell adhesion molecule binding” and “integrin binding” as the important functional signatures (Fig. 1D). Several genes, including ECM2, TGFB2, and TIMP2, were consistently found to be associated with the above key signatures in all three GO analyses.
Figure 1.
GO enrichment analyses for the 37 prognostic hazardous genes disclose the potential mechanisms of GC progression. (A) GO-BP pathways are significantly enriched. Each dot represents a specific GO-BP term, with the count number and the corresponding P value, respectively, indicated by the size and the color of the dot. The genes associated with the enriched GO-BP (B), GO-CC (C), and GO-MF (D) terms are illustrated by the cnetplots, with the size of each node representing the overlapped genes in each term. EMT: epithelial to mesenchymal transition, epithelial mesenchymal transition; E.C.M.: epithelial cell migration; ECP: epithelial cell proliferation; CD: cartilage development; ECM: extracellular matrix; ECS: extracellular structure.
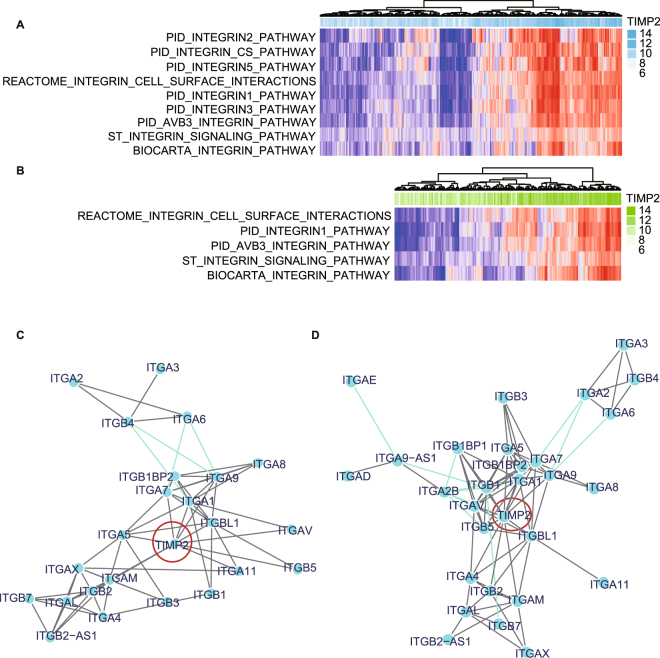
The relationship of TIMP2 with the integrin family
As integrin family have been reported to be important for ECS and ECM, and TIMP2 were currently found to be related with “integrin binding”, we further explored the relationship of TIMP2 with integrin-related signatures using GSVA, which allows to assess the underlying pathway activity variation via transforming the gene into a signature/gene set by sample matrix without the a priori knowledge of the experimental design. There were respective 9 and 5 integrin pathways associated with TIMP2 expression in GSE62254 (Fig. 2A) and GSE15459 (Fig. 2B). In GCN assays, TIMP2 was shown to respectively co-express with 10 genes in GSE62254 (Fig. 2C), and 14 genes in GSE15459 (Fig. 2D). The overlapped 9 genes were ITGA1, ITGA5, ITGA7, ITGA9, ITGAM, ITGAV, ITGB2, ITGB5, and ITGBL1.
Figure 2.
Sequential GSVA and GCN analysis uncover the correlation factors of TIMP2. There are respective 9 (A) and 5(B) integrin-related signatures enriched by high TIMP2 expression in the GSVA based on GSE62254 and GSE15459. GCN analysis declare 10 (C) and 14 (D) genes associated with high TIMP2 expression in GSE62254 and GSE15459, respectively.
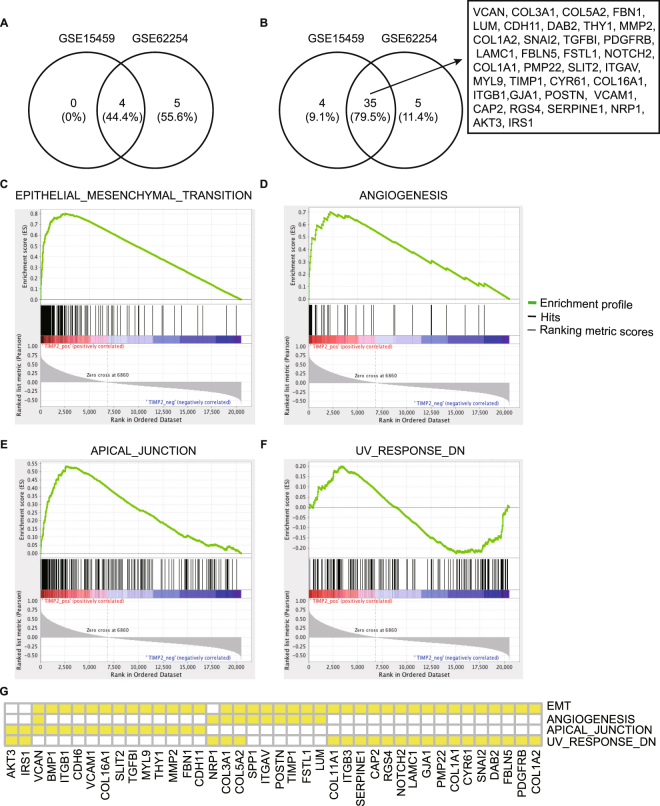
The potential functions of TIMP2 in cancers
To further disclose the potential functions of TIMP2 in cancers, we performed GSEA, a robust computational method to identify a-priori defined set of genes in a special phenotype. The most significant gene sets enriched in high TIMP2 phenotype were ordered by significance (false discovery rate (FDR) q- and P-values) and listed in Table 1. As shown in Fig. 3(A,C–F), four hallmark gene-sets, including “ANGIOGENESIS”, “APICAL_JUNCTION”, “EPITHELIAL_MESENCHYMAL_TRANSITION (EMT)” and “UV_RESPONSE_DN”, were shared by the both GSE datasets and supposed to be the vital signatures of high TIMP2 expression. As shown in Fig. 3B and G, GSE62254 and GSE15459 overlapped a number of leading-edge genes, such as cell adhesion molecule related genes including COL3A1, COL5A2, COL1A2, COL1A1, and COL16A1, and integrin family genes including ITGAV and ITGB1.
Table 1.
Gene set enrichment analysis (GSEA) and leading-edge gene assays according to the levels of TIMP-2 in GSE62254 and GSE15459.
| GSE62254 | GSE15459 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Size | ES | P | FDR.q. | Rankmax | Leading edge | ES | P | FDR.q. | Rankmax | Leading edge | |
| ANGIOGENESIS | 35 | 0.70 | 0.002 | 0.00 | 2167 | tags = 51%, list = 11%, signal = 57% | 0.69 | 0.004 | 0.07 | 3002 | tags = 57%, list = 15%, signal = 67% |
| APICAL_JUNCTION | 190 | 0.53 | 0.000 | 0.00 | 2746 | tags = 38%, list = 13%, signal = 44% | 0.48 | 0.002 | 0.08 | 3276 | tags = 40%, list = 16%, signal = 47% |
| COAGULATION | 135 | 0.60 | 0.002 | 0.00 | 2821 | tags = 40%, list = 14%, signal = 46% | — | ||||
| EMT | 196 | 0.80 | 0.000 | 0.00 | 2525 | tags = 73%, list = 12%, signal = 83% | 0.76 | 0.000 | 0.06 | 2375 | tags = 64%, list = 12%, signal = 72% |
| IR | 197 | 0.63 | 0.004 | 0.01 | 4572 | tags = 63%, list = 22%, signal = 81% | — | ||||
| KRAS_SIGNALING_UP | 193 | 0.54 | 0.000 | 0.01 | 3309 | tags = 45%, list = 16%, signal = 53% | — | ||||
| MYOGENESIS | 197 | 0.59 | 0.000 | 0.00 | 3377 | tags = 47%, list = 16%, signal = 56% | — | ||||
| TGF_BETA_SIGNALING | 53 | 0.55 | 0.004 | 0.02 | 2997 | tags = 40%, list = 15%, signal = 46% | — | ||||
| UV_RESPONSE_DN | 139 | 0.59 | 0.002 | 0.00 | 3269 | tags = 47%, list = 16%, signal = 56% | 0.64 | 0.000 | 0.08 | 4192 | tags = 61%, list = 20%, signal = 76% |
EMT: EPITHELIAL_MESENCHYMAL_TRANSITION; IR: INFLAMMATORY_RESPONSE.
Figure 3.
GSEA and LEGA declare the most significant pathways and genes related with TIMP-2 based on GSE62254 and GSE15459. GSE62254 and GSE15459 share 4 gene sets (A) and 35 (B) leading-edge genes that are related with TIMP-2 expression. The correlation of TIMP2 levels with the 4 hallmark gene-sets, including “EPITHELIAL_MESENCHYMAL_TRANSITION” (C), “ANGIOGENESIS” (D), “APICAL_JUNCTION” (E) and “UV_RESPONSE_DN” (F), are illustrated, and the overlapped leading-edge genes in GSE62254 are shown (G).
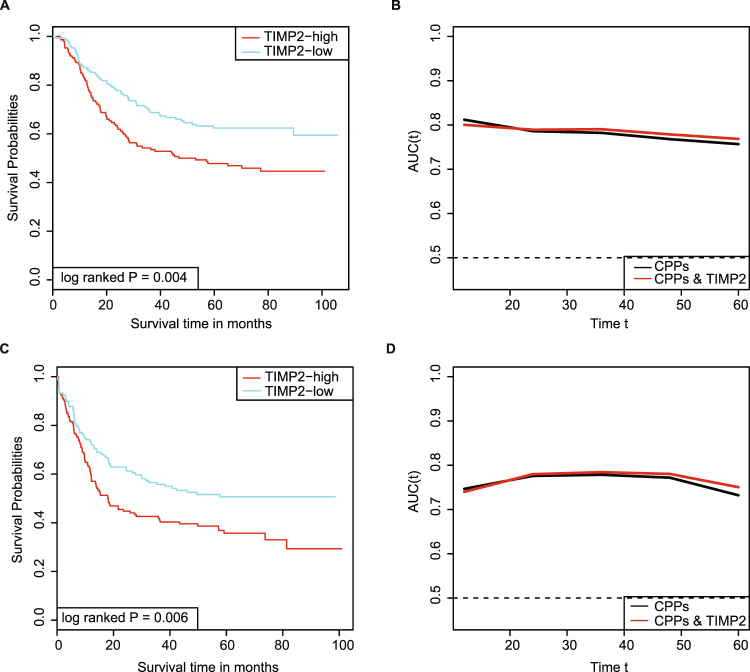
The survival prediction value of TIMP2 and the relationship with CPPs in GC
TIMP2 expression was demonstrated to predict shorter overall survival (OS) and recurrence free survival (RFS) of patients in the Kaplan-Meier (K-M) analysis (log-rank P = 0.004 and 0.006, respectively), and was further identified as the independent predictor for OS and RFS in the multi-variate COX analysis, respectively, using GSE62254 (Fig. 4A and C; Table 2) and GSE15459 (Supplementary Fig. 2A). The COX models based on the databases were both successfully validated by 1000 times bootstrapping (Table 2). Moreover, the inclusion of TIMP2 levels to the prognostic model using traditional CPPs slightly improved the prediction ability for OS and RFS (Fig. 4B and D, Supplementary Fig. 2B), as demonstrated by the increase of the resulting area under curve (AUC) values.
Figure 4.
High TIMP2 predicts poorer survival of GC patients in GSE62254. (A) K-M analysis identified the prognosis significance of TIMP2 for OS of patients in GC. (B) TIMP2 combining with CPPs increases the prediction accuracy of traditional CPPs for OS. (C) TIMP2 expression predicts reduced RFS of patients as demonstrated by K-M analysis. (D) The addition of TIMP2 to CPPs slightly improves the prediction capacity of CPPs for RFS.
Table 2.
Multivariate COX analysis for the independent predictors of overall survival and recurrence free survival of GC patients in GSE62254.
| OS | RFS | |||||||
|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | P - value | Bootstrapping 95% CI | HR | 95% CI | P - value | Bootstrapping 95% CI | |
| TIMP2 | 1.39 | 1.16–1.84 | 0.001 | 1.17–1.86 | 1.44 | 1.17–1.78 | <0.001 | 1.18–1.80 |
| Age | 1.02 | 1.01–1.04 | 0.003 | 1.01–1.04 | 1.02 | 1.01–1.04 | 0.002 | 1.01–1.04 |
| T-stage | 1.16 | 1.02–1.68 | 0.034 | 1.00–1.71 | — | — | — | — |
| N-stage | 1.77 | 1.59–2.41 | <0.001 | 1.61–2.42 | 1.82 | 1.52–2.19 | <0.001 | 1.54–2.20 |
| M-stage | 2.01 | 1.42–3.66 | <0.001 | 1.40–3.72 | 2.03 | 1.29–3.21 | 0.002 | 1.30–3.27 |
OS: overall survival; RFS: recurrence free survival.
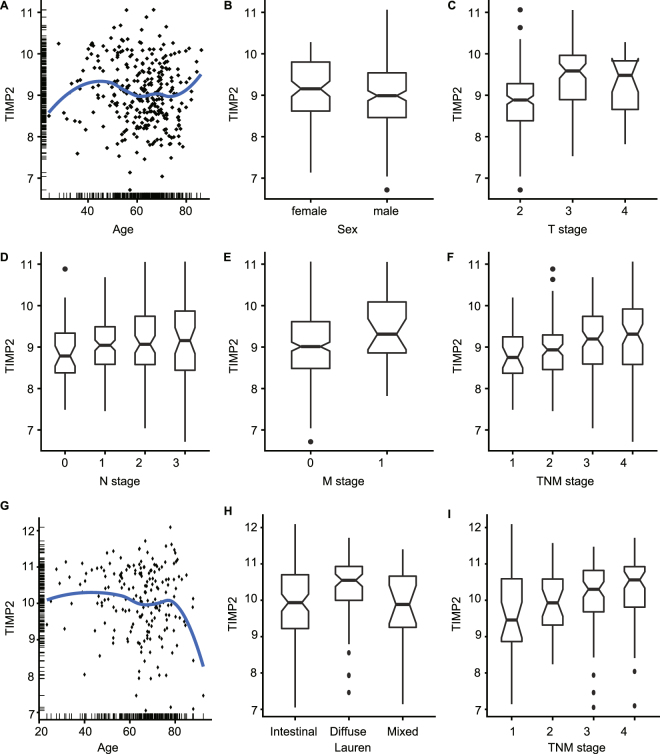
The associations of TIMP2 with CPPs were shown in Table 3, and Fig. 5. TIMP2 expression was significantly positively correlated with the age (P = 0.047), sex (P = 0.039), T stage (P < 0.001), M stage (P = 0.021), and TNM stage (P < 0.001) of patients in GSE62254, and the Lauren type (P = 0.020) and TNM stage (P = 0.002) of GC in GSE15459.
Table 3.
| Variable | GSE62254 | GSE15459 | ||||
|---|---|---|---|---|---|---|
| N (%) | TIMP-2 (median, IQR) | P | N (%) | TIMP-2 (median, IQR) | P | |
| Age (median, IQR) | 64 (55–70) | — | 0.047 | 67 (57–73) | — | 0.164 |
| Sex | 0.039 | 0.074 | ||||
| Female | 101 (33.9) | 9.16 (8.62–9.80) | 67 (34.9) | 10.37 (9.78–10.87) | ||
| Male | 197 (66.1) | 8.99 (8.46–9.54) | 125 (65.1) | 10.06 (9.26–10.75) | ||
| Lauren’s | — | 0.020 | ||||
| Intestinal | — | — | 99 (51.6) | 9.93 (9.22–10.70) | ||
| Diffused | — | — | 75 (39.1) | 10.55 (10.00–10.93) | ||
| Mixed | — | — | 18 (9.4) | 9.89 (9.25–10.66) | ||
| T stage | <0.001 | — | ||||
| T1 | — | — | — | — | ||
| T2 | 186 (62.4) | 8.89 (8.38–9.28) | — | — | ||
| T3 | 91 (30.5) | 9.59 (8.89–9.96) | — | — | ||
| T4 | 21 (7.0) | 9.48 (8.66–9.83) | — | — | ||
| N stage | 0.090 | — | ||||
| N0 | 38 (12.8) | 8.79 (8.38–9.34) | — | — | ||
| N1 | 130 (43.6) | 9.04 (8.58–9.49) | — | — | ||
| N2 | 79 (26.5) | 9.07 (8.58–9.74) | — | — | ||
| N3 | 51 (17.1) | 9.16 (8.44–9.87) | — | — | ||
| M stage | 0.021 | — | ||||
| M0 | 271 (90.9) | 9.01 (8.48–9.61) | — | — | ||
| M1 | 27 (9.1) | 9.31 (8.86–10.09) | — | — | ||
| TNM stage | <0.001 | 0.002 | ||||
| I | 30 (10.1) | 8.75 (8.37–9.25) | 31 (16.1) | 9.46 (8.87–10.59) | ||
| II | 96 (32.2) | 8.93 (8.46–9.29) | 29 (15.1) | 9.93 (9.32–10.58) | ||
| III | 95 (31.9) | 9.19 (8.59–9.74) | 72 (37.5) | 10.30 (9.68–10.82) | ||
| IV | 77 (25.8) | 9.31 (8.58–9.92) | 60 (31.2) | 10.56 (9.81–10.92) | ||
IQR, interquartile range.
Figure 5.
High TIMP2 is related with multiple CPPs involved in GC progression in GSE62254 and GSE15459. TIMP2 expression is significantly correlated with age (A), sex (B), T- (C), M- (E), and TNM-stage (F), and marginal related with N-stage (D) in GC cohort of GSE62254. High TIMP2 has no relationship with age (G), whereas statistically correlates with Lauren type (H) and TNM-stage (I) of cancer in GSE15459.
Discussion
With comprehensive bioinformatics analysis of 3 big GC datasets, we currently screened out 37 genes that could predict poorer outcome of patients, and further identified that TIMP2 might play a key role in the prognosis of GC through directly binding with integrin and working on cell adhesion, EMT, and angiogenesis of cancers.
TIMP2 is originally found to prohibit cell proliferation and migration in vitro via inhibiting the function of MMPs, but latterly disclosed indeed a factor full of puzzling paradox by multiple clinical studies. On one hand, TIMP2 was found to predict better prognosis in endometrial9 and pancreatic carcinomas10, whereas indicate poorer outcome in neuroblastoma, and head and neck, hepatocellular, Canine mammary, laryngeal, renal, colorectal, oral or tong squamous cell cancers11–18. On the other hand, conflicting evidences were present by different studies about the prognostic role of TIMP2 in the same type of cancer, such as breast19,20, lung4,21, cervical2,22,23, ovarian24–26, and bladder cancer27–29. In GC, TIMP2 was declared to express in cancer, mesenchymal or immune cells, with the clinical role still ambiguous. For example, TIMP2 was shown to predict disease progression30–32 in some studies, while demonstrated to have no relationship with CPPs33 or survival30,33,34 in others.
In the current study, we found that TIMP2 overexpression could predict poorer survival in GC, which is believed to be credible due to the following reasons. First, the clinical role of TIMP2 in GC was explored based on all the 3 biggest available on-line omics datasets of clinical patients, and further confirmed by 1000 internal bootstrap replications and external KM plotter analysis. Second, the independent prediction ability of TIMP2 for patients’ survival was constructed using COX regression model, and further validated by ROC analysis, which demonstrated that the addition of TIMP2 increased the prediction accuracy of the traditional prognostic model using CPPs. Third, the correlations of TIMP2 with Lauren type, and T, M, and TNM stage, were consistent with multiple previous reports, in which TIMP2 was significantly related with the Lauren classification in GC30, the distant metastasis in soft tissue sarcoma35, as well as gastric30,34,36, colorectal37, breast38, and Canine mammary cancer14, the local invasion in invasive prolactinomas39, and gastric32,40 and thyroid papillary cancer41, and the T or TNM stage in oral42,43, bladder29 and cervical cancer23. Besides, our further Oncomine analysis revealed significant higher TIMP2 in GC than non-cancer tissues, which indicates the potential key role of TIMP2 in the oncogenesis and development of GC (data not shown). Moreover, our explorations for the mechanisms of GC progression and TIMP2 functions might present more certifications for the current novel findings.
Consistent with previous reports, our analysis disclosed that TIMP2 involves in the regulation of EMT, cell adhesion, and angiogenesis, and interacts with cell adhesion molecular, and multiple integrin pathways and family members. Given the fact that TIMP2 was found to inhibit metastasis and angiogenesis in vitro on one hand, but on the other hand high TIMP2 correlates with malignant phenotype and unfavorable prognosis of cancer patients in lots of clinical assays44–47, our current study also encounters with the existing unsolved TIMP2 paradox and serves as another evidence for the paradoxical phenomenon. The potential explanations for the contradictions are as follows based on previous reports. First, the recorded concentrations of TIMP2 in tissues and biological fluids are much lower than the used concentrations in vitro experiments44. Second, TIMP2 is demonstrated to control cell fates through a proteolytic and a non-proteolytic mechanism44,48. In the non-proteolytic manner, TIMP2 was found to induce an intracellular ERK signaling cascade at the physiologically-relevant, low concentrations, and thus further disclosed to result in a burst in cancer cell migration48, as well as proliferation4. To solve the puzzling TIMP2 paradox, more in-vivo and high through-put data studies are expected.
The limitations of the current study are listed as follows. First, the role and the function of TIMP2 are conducted by bioinformatics methods based on on-line databases and need to be further validated by in-vitro and in-vivo experimental studies. Second, the ratios of MMPs/TIMP2 were considered meaningful markers for cancer studies but could not be evaluated currently49,50. Third, our current study did not evaluate the prognostic role of TIMP2 on the following respects, such as its genetic variations like SNP and methylation, the expression locations including cancer and mesenchymal cells, and the detection samples like tissues and serum31,37,51,52. Further studies are warranted for such topics.
In summary, we firstly uncover the significant prognostic role and the potential function of TIMP2 in GC with multiple datasets and integrated bioinformatics analysis-methods. TIMP2 is identified as a potential predictor for poorer outcome of patients, with the predictive accuracy and independency well demonstrated by both external and internal validations. Further GSEA, GSVA and GCN analysis declared the potential mechanisms for the progression of GC, such as cell adhesion; integrin networks, angiogenesis, and so on. Our findings present a novel candidate biomarker for patients’ prognosis in GC, shed lights on the underlying function of TIMP2, and indicate novel interesting topics for future studies.
Materials and Methods
Data preprocessing and summarization
The GC online datasets from Gene Expression Omnibus database (GEO, http://www.ncbi.nlm.nih.gov/geo/) were filtered according to the following criteria: 1) include more than 100 cases; 2) provide both clinicopathological and survival information (OS, and/or RFS); 3) use the universal high-throughput platform, such as affymetrix HGU133 plus2 (GPL570) or Illumina HiSeq 2000 instrument (GPL11154). The search strategy was as follows: (gastric cancer) AND ((GPL570) OR GPL11154) Filters: Series; DataSets, and totally 12 datasets were filtered out. After manual screening, two data sets including GSE62254 and GSE15459, were used in the current study. The raw data were preprocessed with Robust Multichip Average (RMA) methods in the default settings. The probe-level data were converted into the corresponding genetic symbols based on the annotation platform. As for a gene corresponding to a plurality of probes, average value was taken as the initial expression value. In addition, the TCGA RNASEQV2 data (level 3) of GC was downloaded from UCSC xena website (http://xena.ucsc.edu/), and cases with primary GC, no history of neo-adjuvant therapy, complete information of survival (OS and/or RFS) and mRNA profile, were included.
GSE62254 and GSE15459 were both performed on platform GPL570 and contained 300 cases from Korea and 192 cases from Singapore, respectively. Totally 20502 genes of each GEO dataset were analyzed for the relationship with the corresponding clinicopathological data, such as gender, age at diagnosis, histological subtypes, TNM stage, OS and/or RFS. According to TCGA, 380 out of 580 samples were selected currently. A total of 20564 genes were taken for the analysis. For the cohort in GSE62254, GSE15459 and TCGA, the median follow-up time, as calculated by the reverse KM method53, was respective 76.93, 74.33 and 23.07 months, and the median OS was respective 31.20 months, not reached, and 29.37 months. The CPPs of the 3 datasets were summarized in Supplementary Table 1.
Uni-variate COX, KM plotter and GO analysis
With each of the three selected datasets, including GSE62254, GSE15459, and TCGA, the prognostic value of each gene was calculated in the uni-variate COX analysis, and the genes with both P < 0.05 and betaOS * betaRFS > 0 were kept for further analysis. Genes were ranked based on the P values in the order from small to large, and the rank number based on POS and PRFS was, respectively, defined as rankOS and rankRFS. For each gene, the overall mean of rankOS and rankRFS was calculated and defined as rankave. The genes of the 3 datasets were, respectively, sorted based on the rankave in the order from small to large, and the top 1000 genes of each dataset were considered as significant. Then the gene with hazard ratio (HR) > 1 across the 3 datasets was considered survival hazardous, and the gene with HR < 1 across the 3 datasets was considered survival protective. The prognostic significance of the selected genes in GC were further confirmed using KM plotter. With the Bioconductor “clusterProfiler” package, GO-BP, -CC, and -MF were analyzed with the hazardous genes, using P- and FDR q-value < 0.05 as the standard for statistical significance.
GSVA and GCN construction
To infer specific activated pathways related with TIMP2 expression, we performed GSVA using the c2 curated signatures downloaded from the Molecular Signatures Database (MSigDB). The signatures whose name including “integrin” were chosen and applied to the correlation tests for the relationship between TIMP2 levels and the activation scores of the integrin-related signatures in GSE62254 and GSE15459, respectively. The signatures with Pearson correlation coefficients (PCC) higher than 0.6 were considered significant.
With R/igraph package and cytoscape V3.5.1, GCN was built on the correlation matrix of integrin family genes with TIMP2 in GSE62254 and GSE15459, respectively. PCC for every pair of genes were calculated, and the gene pairs with |PCC| > 0.4 and FDR q < 0.05 were retained.
GSEA, venn diagram and Leading-Edge Gene Analysis (LEGA)
For GSEA, 50 available hallmark gene sets from MSigDB were used, and the expression levels of TIMP2 were set to annotate the phenotypes of samples. After performing 1,000 permutations, the first 20 signatures with FDR q < 0.1 and P < 0.005 were considered to be significantly enriched. The overlapped enriched hallmark signatures in GSE62254 and GSE15459 were illustrated by venn diagram, and further applied to LEGA.
Correlation tests, K-M log-rank test, multi-variate COX analysis with bootstrapping, and ROC curve
Based on GSE62254 and GSE15459, spearman correlation tests were, respectively, performed to analyze the correlation of TIMP2 and CPPs, including age, sex, Lauren type, T-stage, N-stage, M-stage, and TNM stage. In the survival assays using K-M method and log-rank test, expression level of TIMP2 was dichotomized as high and low with median as the cutoff value. Multi-variate Cox PH models were used to estimate HR and 95% confidence interval (CI). The final multivariate model was constructed based on the Akaike information criterion (AIC) value using both “backward” and “forward” stepwise selection methods, and further internally validated by coefficients and 95% CIs using bootstrapping (1000 replications). Based on the risk scores, the AUC (t) curve was plotted to illustrate time dependent sensitivity and specificity of corresponding time-dependent receiver-operating characteristics (ROC) at each observed event time.
Electronic supplementary material
Acknowledgements
This study was supported by grants from the Special Clinical Foundation of Wujieping Medical Foundation Society (No. 320.6750.1281) and the Foundation for President of Liaoning Medical University (No. xzjj20130233).
Author Contributions
Wei Wang and YiFan Zhang were responsible for the acquisition of data, analysis and interpretation of data, drafting the article; Mingxing Liu, Yang Wang, Tao Yang, Dongsheng Li, and Feng Ding were responsible for the interpretation of data, revising the article; Qing Li and Guang Bai were responsible for the interpretation of data, conception and design of the study, critical revision.
Competing Interests
The authors declare no competing interests.
Footnotes
Wei Wang and Yifan Zhang contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-27897-x.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Guang Bai, Email: Baiguang69255@163.com.
Qing Li, Email: liqing610557@163.com.
References
- 1.Washington K. 7th edition of the AJCC cancer staging manual: stomach. Ann Surg Oncol. 2010;17:3077–3079. doi: 10.1245/s10434-010-1362-z. [DOI] [PubMed] [Google Scholar]
- 2.Braicu EI, et al. Role of serum concentration of VEGFR1 and TIMP2 on clinical outcome in primary cervical cancer: results of a companion protocol of the randomized, NOGGO-AGO phase III adjuvant trial of simultaneous cisplatin-based radiochemotherapy vs. carboplatin and paclitaxel containing sequential radiotherapy. Cytokine. 2013;61:755–758. doi: 10.1016/j.cyto.2013.01.013. [DOI] [PubMed] [Google Scholar]
- 3.Shah MA, et al. Molecular classification of gastric cancer: a new paradigm. Clin Cancer Res. 2011;17:2693–2701. doi: 10.1158/1078-0432.CCR-10-2203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cristescu R, et al. Molecular analysis of gastric cancer identifies subtypes associated with distinct clinical outcomes. Nat Med. 2015;21:449–456. doi: 10.1038/nm.3850. [DOI] [PubMed] [Google Scholar]
- 5.Dinh TA, et al. Comprehensive analysis of The Cancer Genome Atlas reveals a unique gene and non-coding RNA signature of fibrolamellar carcinoma. Sci Rep. 2017;7:44653. doi: 10.1038/srep44653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramasamy A, Mondry A, Holmes CC, Altman DG. Key issues in conducting a meta-analysis of gene expression microarray datasets. PLoS Med. 2008;5:e184. doi: 10.1371/journal.pmed.0050184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hou JY, Wang YG, Ma SJ, Yang BY, Li QP. Identification of a prognostic 5-Gene expression signature for gastric cancer. J Cancer Res Clin Oncol. 2017;143:619–629. doi: 10.1007/s00432-016-2324-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park C, et al. Host immune response index in gastric cancer identified by comprehensive analyses of tumor immunity. Oncoimmunology. 2017;6:e1356150. doi: 10.1080/2162402X.2017.1356150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Honkavuori-Toivola M, Talvensaari-Mattila A, Soini Y, Turpeenniemi-Hujanen T, Santala M. Immunoreactivity for TIMP-2 is associated with a favorable prognosis in endometrial carcinoma. Tumour Biol. 2012;33:935–941. doi: 10.1007/s13277-012-0321-7. [DOI] [PubMed] [Google Scholar]
- 10.Giannopoulos G, et al. The expression of matrix metalloproteinases-2 and -9 and their tissue inhibitor 2 in pancreatic ductal and ampullary carcinoma and their relation to angiogenesis and clinicopathological parameters. Anticancer Res. 2008;28:1875–1881. [PubMed] [Google Scholar]
- 11.Ara T, et al. Immunohistochemical expression of MMP-2, MMP-9, and TIMP-2 in neuroblastoma: association with tumor progression and clinical outcome. J Pediatr Surg. 1998;33:1272–1278. doi: 10.1016/S0022-3468(98)90167-1. [DOI] [PubMed] [Google Scholar]
- 12.Pietruszewska W, Bojanowska-Pozniak K, Kobos J. Matrix metalloproteinases MMP1, MMP2, MMP9 and their tissue inhibitors TIMP1, TIMP2, TIMP3 in head and neck cancer: an immunohistochemical study. Otolaryngol Pol. 2016;70:32–43. doi: 10.5604/00306657.1202546. [DOI] [PubMed] [Google Scholar]
- 13.Hsu KW, et al. Notch1 pathway-mediated microRNA-151-5p promotes gastric cancer progression. Oncotarget. 2016;7:38036–38051. doi: 10.18632/oncotarget.9342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Santos A, et al. Immunohistochemical evaluation of MMP-2 and TIMP-2 in canine mammary tumours: a survival study. Vet J. 2011;190:396–402. doi: 10.1016/j.tvjl.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Pietruszewska W, Kobos J, Gryczynski M, Durko T, Bojanowska-Pozniak K. Analysis of TIMP-1, TIMP-2 and TIMP-3 expression as a prognostic factor of laryngeal cancer progression. Otolaryngol Pol. 2008;62:380–387. doi: 10.1016/S0030-6657(08)70276-2. [DOI] [PubMed] [Google Scholar]
- 16.Kawata N, et al. Significant relationship of matrix metalloproteinase 9 with nuclear grade and prognostic impact of tissue inhibitor of metalloproteinase 2 for incidental clear cell renal cell carcinoma. Urology. 2007;69:1049–1053. doi: 10.1016/j.urology.2007.02.044. [DOI] [PubMed] [Google Scholar]
- 17.Oberg A, Hoyhtya M, Tavelin B, Stenling R, Lindmark G. Limited value of preoperative serum analyses of matrix metalloproteinases (MMP-2, MMP-9) and tissue inhibitors of matrix metalloproteinases (TIMP-1, TIMP-2) in colorectal cancer. Anticancer Res. 2000;20:1085–1091. [PubMed] [Google Scholar]
- 18.Katayama A, et al. Expressions of matrix metalloproteinases in early-stage oral squamous cell carcinoma as predictive indicators for tumor metastases and prognosis. Clin Cancer Res. 2004;10:634–640. doi: 10.1158/1078-0432.CCR-0864-02. [DOI] [PubMed] [Google Scholar]
- 19.Chen X, et al. miR-4443 Participates in the Malignancy of Breast Cancer. PLoS One. 2016;11:e0160780. doi: 10.1371/journal.pone.0160780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Remacle A, et al. High levels of TIMP-2 correlate with adverse prognosis in breast cancer. Int J Cancer. 2000;89:118–121. doi: 10.1002/(SICI)1097-0215(20000320)89:2<118::AID-IJC3>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 21.Zhu L, et al. Prognostic value of tissue inhibitor of metalloproteinase-2 expression in patients with non-small cell lung cancer: a systematic review and meta-analysis. PLoS One. 2015;10:e0124230. doi: 10.1371/journal.pone.0124230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Braicu EI, et al. Role of serum VEGFA, TIMP2, MMP2 and MMP9 in monitoring response to adjuvant radiochemotherapy in patients with primary cervical cancer–results of a companion protocol of the randomized NOGGO-AGO phase III clinical trial. Anticancer Res. 2014;34:385–391. [PubMed] [Google Scholar]
- 23.Davidson B, et al. MMP-2 and TIMP-2 expression correlates with poor prognosis in cervical carcinoma–a clinicopathologic study using immunohistochemistry and mRNA in situ hybridization. Gynecol Oncol. 1999;73:372–382. doi: 10.1006/gyno.1999.5381. [DOI] [PubMed] [Google Scholar]
- 24.Halon A, et al. Enhanced immunoreactivity of TIMP-2 in the stromal compartment of tumor as a marker of favorable prognosis in ovarian cancer patients. J Histochem Cytochem. 2012;60:491–501. doi: 10.1369/0022155412446978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davidson B, et al. The prognostic value of metalloproteinases and angiogenic factors in ovarian carcinoma. Mol Cell Endocrinol. 2002;187:39–45. doi: 10.1016/S0303-7207(01)00709-2. [DOI] [PubMed] [Google Scholar]
- 26.Davidson B, et al. High levels of MMP-2, MMP-9, MT1-MMP and TIMP-2 mRNA correlate with poor survival in ovarian carcinoma. Clin Exp Metastasis. 1999;17:799–808. doi: 10.1023/A:1006723011835. [DOI] [PubMed] [Google Scholar]
- 27.Vasala K, Kuvaja P, Turpeenniemi-Hujanen T. Low circulating levels of ProMMP-2 are associated with adverse prognosis in bladder cancer. Tumour Biol. 2008;29:279–286. doi: 10.1159/000156705. [DOI] [PubMed] [Google Scholar]
- 28.Gakiopoulou H, et al. Tissue inhibitor of metalloproteinase-2 as a multifunctional molecule of which the expression is associated with adverse prognosis of patients with urothelial bladder carcinomas. Clin Cancer Res. 2003;9:5573–5581. [PubMed] [Google Scholar]
- 29.Kanayama H, et al. Prognostic values of matrix metalloproteinase-2 and tissue inhibitor of metalloproteinase-2 expression in bladder cancer. Cancer. 1998;82:1359–1366. doi: 10.1002/(SICI)1097-0142(19980401)82:7<1359::AID-CNCR20>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 30.Alakus H, et al. Clinicopathological significance of MMP-2 and its specific inhibitor TIMP-2 in gastric cancer. Histol Histopathol. 2008;23:917–923. doi: 10.14670/HH-23.917. [DOI] [PubMed] [Google Scholar]
- 31.Lukaszewicz-Zajac M, et al. Matrix metalloproteinase 2 (MMP-2) and their tissue inhibitor 2 (TIMP-2) in gastric cancer patients. Adv Med Sci. 2013;58:235–243. doi: 10.2478/ams-2013-0018. [DOI] [PubMed] [Google Scholar]
- 32.Mroczko B, Lukaszewicz-Zajac M, Gryko M, Kedra B, Szmitkowski M. Clinical significance of serum levels of matrix metalloproteinase 2 (MMP-2) and its tissue inhibitor (TIMP-2) in gastric cancer. Folia Histochem Cytobiol. 2011;49:125–131. doi: 10.5603/FHC.2011.0018. [DOI] [PubMed] [Google Scholar]
- 33.Joo YE, et al. Expression of tissue inhibitors of metalloproteinases (TIMPs) in gastric cancer. Dig Dis Sci. 2000;45:114–121. doi: 10.1023/A:1005421713137. [DOI] [PubMed] [Google Scholar]
- 34.Alakus H, et al. Clinical impact of MMP and TIMP gene polymorphisms in gastric cancer. World J Surg. 2010;34:2853–2859. doi: 10.1007/s00268-010-0761-4. [DOI] [PubMed] [Google Scholar]
- 35.Yang HK, Jeong KC, Kim YK, Jung ST. Role of matrix metalloproteinase (MMP) 2 and MMP-9 in soft tissue sarcoma. Clin Orthop Surg. 2014;6:443–454. doi: 10.4055/cios.2014.6.4.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Park KS, Kim SJ, Kim KH, Kim JC. Clinical characteristics of TIMP2, MMP2, and MMP9 gene polymorphisms in colorectal cancer. J Gastroenterol Hepatol. 2011;26:391–397. doi: 10.1111/j.1440-1746.2010.06504.x. [DOI] [PubMed] [Google Scholar]
- 37.Groblewska M, et al. Serum levels and tissue expression of matrix metalloproteinase 2 (MMP-2) and tissue inhibitor of metalloproteinases 2 (TIMP-2) in colorectal cancer patients. Tumour Biol. 2014;35:3793–3802. doi: 10.1007/s13277-013-1502-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ree AH, et al. High levels of messenger RNAs for tissue inhibitors of metalloproteinases (TIMP-1 and TIMP-2) in primary breast carcinomas are associated with development of distant metastases. Clin Cancer Res. 1997;3:1623–1628. [PubMed] [Google Scholar]
- 39.Gultekin GD, Cabuk B, Vural C, Ceylan S. Matrix metalloproteinase-9 and tissue inhibitor of matrix metalloproteinase-2: Prognostic biological markers in invasive prolactinomas. J Clin Neurosci. 2015;22:1282–1287. doi: 10.1016/j.jocn.2015.02.021. [DOI] [PubMed] [Google Scholar]
- 40.Lin XD, et al. Association of polymorphism in matrix metalloproteinase-2 and tissue inhibitor of metalloproteinase-2 with genetic susceptibility of gastric cancer. Zhonghua Yu Fang Yi Xue Za Zhi. 2011;45:711–716. [PubMed] [Google Scholar]
- 41.Marecko I, et al. Expression of matrix metalloproteinase-2 and its tissue inhibitor-2 in fetal and neoplastic thyroid tissue and their significance as diagnostic and prognostic markers in papillary carcinoma. Cancer Biomark. 2011;11:49–58. doi: 10.3233/CBM-2012-0258. [DOI] [PubMed] [Google Scholar]
- 42.de Vicente JC, Fresno MF, Villalain L, Vega JA, Lopez Arranz JS. Immunoexpression and prognostic significance of TIMP-1 and -2 in oral squamous cell carcinoma. Oral Oncol. 2005;41:568–579. doi: 10.1016/j.oraloncology.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 43.Gao ZB, Duan YQ, Zhang L, Chen DW, Ding PT. Expression of matrix metalloproteinase 2 and its tissue inhibitor in oral squamous cell carcinoma. Int J Mol Med. 2005;16:599–603. [PubMed] [Google Scholar]
- 44.Strongin AY. Proteolytic and non-proteolytic roles of membrane type-1 matrix metalloproteinase in malignancy. Biochim Biophys Acta. 2010;1803:133–141. doi: 10.1016/j.bbamcr.2009.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang C, Chen Z, Li Z, Cen J. The essential roles of matrix metalloproteinase-2, membrane type 1 metalloproteinase and tissue inhibitor of metalloproteinase-2 in the invasive capacity of acute monocytic leukemia SHI-1 cells. Leuk Res. 2010;34:1083–1090. doi: 10.1016/j.leukres.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 46.Maatta M, Santala M, Soini Y, Turpeenniemi-Hujanen T, Talvensaari-Mattila A. Increased matrix metalloproteinases 2 and 9 and tissue inhibitor of matrix metalloproteinase 2 expression is associated with progression from vulvar intraepithelial neoplasia to invasive carcinoma. Acta Obstet Gynecol Scand. 2010;89:380–384. doi: 10.3109/00016340903555990. [DOI] [PubMed] [Google Scholar]
- 47.Christopoulos TA, et al. Expression of metalloproteinases and their tissue inhibitors in squamous cell laryngeal carcinoma. Oncol Rep. 2007;18:855–860. doi: 10.3892/or.18.4.855. [DOI] [PubMed] [Google Scholar]
- 48.D’Alessio S, et al. Tissue inhibitor of metalloproteinases-2 binding to membrane-type 1 matrix metalloproteinase induces MAPK activation and cell growth by a non-proteolytic mechanism. J Biol Chem. 2008;283:87–99. doi: 10.1074/jbc.M705492200. [DOI] [PubMed] [Google Scholar]
- 49.Shrestha B, Bajracharya D, Byatnal AA, Kamath A. & Radhakrishnan, R. May High MMP-2 and TIMP-2 Expressions Increase or Decrease the Aggressivity of Oral Cancer? Pathol Oncol Res. 2017;23:197–206. doi: 10.1007/s12253-016-0149-3. [DOI] [PubMed] [Google Scholar]
- 50.Ozden F, et al. Expression of MMP-1, MMP-9 and TIMP-2 in prostate carcinoma and their influence on prognosis and survival. J Cancer Res Clin Oncol. 2013;139:1373–1382. doi: 10.1007/s00432-013-1453-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thiefin G, et al. Beneficial influence of microsatellite instability on gelatinase-tissue inhibitors of metalloproteinase balance in colorectal cancer. Anticancer Res. 2007;27:583–588. [PubMed] [Google Scholar]
- 52.Furtado Y, et al. TIMP-2 gene methylation in cervical precursor and invasive lesions. Exp Mol Pathol. 2015;98:119–123. doi: 10.1016/j.yexmp.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 53.Schemper M, Smith TL. A note on quantifying follow-up in studies of failure time. Control Clin Trials. 1996;17:343–346. doi: 10.1016/0197-2456(96)00075-X. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.