Abstract
Background and Objective
Many countries require hospitals to implement medication reconciliation for accreditation, but the process is resource-intensive, thus adherence is poor. We report on the impact of prepopulating and aligning community and hospital drug lists with data from population-based and hospital-based drug information systems to reduce workload and enhance adoption and use of an e-medication reconciliation application, RightRx.
Methods
The prototype e-medical reconciliation web-based software was developed for a cluster-randomized trial at the McGill University Health Centre. User-centered design and agile development processes were used to develop features intended to enhance adoption, safety, and efficiency. RightRx was implemented in medical and surgical wards, with support and training provided by unit champions and field staff. The time spent per professional using RightRx was measured, as well as the medication reconciliation completion rates in the intervention and control units during the first 20 months of the trial.
Results
Users identified required modifications to the application, including the need for dose-based prescribing, the role of the discharge physician in prescribing community-based medication, and access to the rationale for medication decisions made during hospitalization. In the intervention units, both physicians and pharmacists were involved in discharge reconciliation, for 96.1% and 71.9% of patients, respectively. Medication reconciliation was completed for 80.7% (surgery) to 96.0% (medicine) of patients in the intervention units, and 0.7% (surgery) to 82.7% of patients in the control units. The odds of completing medication reconciliation were 9 times greater in the intervention compared to control units (odds ratio: 9.0, 95% confidence interval, 7.4-10.9, P < .0001) after adjusting for differences in patient characteristics.
Conclusion
High rates of medication reconciliation completion were achieved with automated prepopulation and alignment of community and hospital medication lists.
Keywords: medication reconciliation, medical informatics, medication systems, patient safety
BACKGROUND
Many countries recommend or require hospitals to implement medication reconciliation at admission, transfer, and discharge for accreditation as a means of reducing medication errors and avoidable morbidity, and improving patient safety.1,2 Discharge reconciliation has been given the highest priority, as it is expected to reduce the risk of adverse events caused by the failure to reconcile and communicate changes made in the community drug regimen during hospitalization. Indeed, inadvertent discrepancies in community and hospital medications may increase the risk of adverse events.3
In compliance with accreditation standards, hospitals have instituted medication reconciliation, with most using a paper-based process. However, the paper-based process is cumbersome and resource-intensive, leading to poor adherence, with medication reconciliation conducted in <20% of patients at risk.4–16 Several hospitals have developed software tools to reduce inefficiencies in the medication reconciliation process by curtailing repetitive manual recording of medication lists. The result has been an improvement in completion rates to 40%.17
One of the most challenging and time-consuming aspects of medication reconciliation is accurately and reliably documenting the community drug list.18,19 In an effort to improve efficiencies, several creative solutions have been implemented.19–21 Partners Healthcare (Boston, MA, USA), through its Pre-Admission Medication List tool, displays medications that were recently prescribed in the community and during previous hospitalizations.20 Using a drag-and-drop function, clinicians can build the current community drug list in consultation with patients. An alternate approach was instituted at the US Veterans Administration, where patients themselves use computer kiosks to enter information about their current medications.21 Both initiatives have had a positive impact on completion of the community drug list,20,21 and in the case of the Pre-Admission Medication List tool, it almost doubled the completion of medication reconciliation at discharge to 75%.
Many countries have invested in the creation of regional clinical data repositories to facilitate data exchange among different providers, an approach that can support continuity across transitions in care. These regional repositories provide data about drugs dispensed in the community and, in theory, these data could prepopulate a community drug list that could then be validated by clinicians. Our team developed a web-based software application, RightRx, to semi-automate the medication reconciliation process by prepopulating the community and hospital medication lists using a regional clinical data repository and the local hospital pharmacy system. System development followed user-centered design and an agile development process, with a focus on features and functions to enhance patient safety and improve efficiency. We evaluated whether use of the RightRx system increased medication reconciliation completion rates and report on the technical, professional, and medicolegal issues encountered in its deployment and use.
Context
RightRx was developed for use in a clinical trial designed to determine whether electronic medication reconciliation would reduce preventable adverse drug events, emergency department visits, and readmissions.22 The RightRx trial was conducted at the McGill University Health Centre (MUHC), a consortium of 5 tertiary hospitals for adults and children in Montreal, Quebec, with >1000 beds, 36 730 admissions per year, 12 000 nurses and hospital staff, >500 residents and 1500 physicians, dentists, and pharmacists.23 The MUHC has a clinical information system that provides an integrated display of patient-specific inpatient information including drugs, labs, imaging, and prior admissions. However, most clinical notes and physician orders remain paper-based, and these documents are printed, scanned, and archived in a nonsearchable format as part of the electronic chart. By 2017, the hospital was expected to have implemented medication reconciliation at admission, discharge, and transfer to receive accreditation. At the time of RightRx development, medical units used an electronic form (fillable Portable Document Format [PDF]), which replicated a previously used paper form that was used to perform and document medication reconciliation. Supplementary Appendix S1 summarizes the paper-based medication reconciliation process. On surgical units, medication reconciliation was rarely performed.
METHODS
Development approach
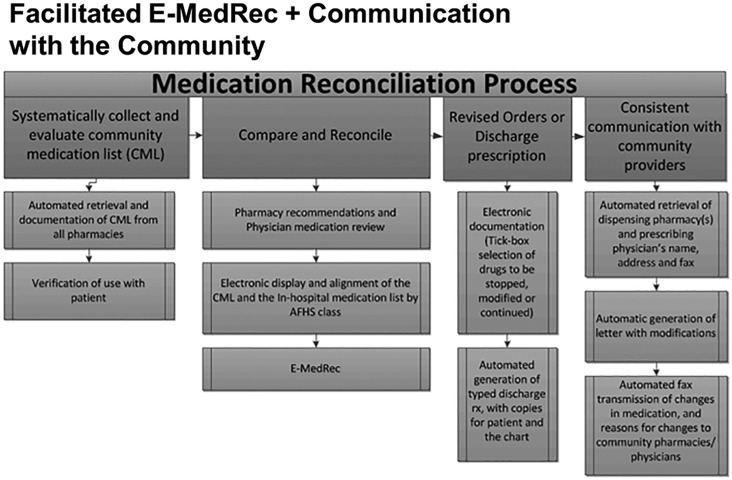
User-centered design and agile development processes were used to develop the RightRx application.24–26 A group of “champion” users, comprising a geriatrician, a general surgeon, a general internist, a pharmacist, and a nurse, worked with a business analyst and a development team to define requirements. Requirements were grouped into 3-week development sprints; the output was tested internally, debugged, and then implemented in the production environment. As the production environment with its real-time data feeds from systems could not be replicated exactly in the test environment, an additional round of testing was done in production, initially by the field research team, and then by champion clinicians within the medical and surgical units. After core functionality was developed, feedback from clinical users (including residents, attending staff physicians, and pharmacists) generated subsequent requirements. Entry into the software development queue of all new requests for features or functionality was prioritized accordingly, based on the impact on patient safety enhancement, improvements in process efficiency, and, finally, other clinically utility. Figure 1 summarizes the changes made to automate an e-medication reconciliation process. Table 1 summarizes the major components that were involved in developing and implementing the e-medication reconciliation RightRx software, as well as the changes and features that were added based on feedback from users in the field.
Figure 1.
Electronic medication reconciliation process.
Table 1.
Components of RightRx development and implementation
| Component | Preliminary Plan | Adaptations |
|---|---|---|
| Baseline assessment | ||
| 1. Workflow and gap analysis | Estimation of the amount of missing information in the documented community drug list at admission compared to population-based dispensing data22 | Workflow analysis of the number of tasks and time per task required for medication reconciliation among different units to address opportunities for improvement in efficiency 18 |
| Data feeds | ||
| 2. External integration to obtain provincial dispensing data, prescribers, and pharmacist information |
|
A system monitoring and alert system was added to detect breaks in the RAMQ web service and hospital data feeds and a protocol to communicate with end users |
| 3. Communication with community-based prescribers and pharmacies | Contact information was obtained by linking the provincial data to the licensing rosters of the College of Physicians and Order of Pharmacists for the community-based prescribers and pharmacies to facilitate communication of changes in community-based medication |
|
| 4. Drug knowledge module requirements | A commercial drug knowledge database was used to map drug identification numbers in the community drug list to generic molecules, and text strings in the hospital drug information to standardized text strings for the name of the same molecule | Frequent drug sentence orders for dose-based prescribing were incorporated to improve the efficiency of data entry |
| Interface development | ||
| 5. Role-based workflow and user interface | Different profile settings were set up for various types of clinicians to tailor to their specific workflow needs and the provincial and hospital legal and professional regulatory requirements |
|
| 6. User-centered design and feedback |
|
|
| Functionalities development | ||
| 7. Prior to admission functionalities |
|
Change from product-based prescribing to generic molecule and dose-per-administration prescribing to improve ease of prescribing and patient safety |
| 8. In-hospital/transfer medication reconciliation functionalities |
|
|
| 9. Discharge functionalities |
|
|
| Deployment, implementation, and adoption | ||
| 10. System deployment |
|
|
| 11. Implementation model/strategy |
|
|
| 12. Adoption |
|
|
Integration of hospital and community-based drug-dispensing data
Community drug list: Real-time data on dispensed community drugs came from the provincial health administrative databases managed by the Régie de l'assurance-maladie du Québec (RAMQ). The RAMQ is the public health insurer for the 8.5 million people in the province of Quebec. A secure web service was established with the RAMQ data warehouse27 that retrieves, for a consenting patient, data on all drugs dispensed. Each drug record includes a unique identification number (which specifies the chemical entity, manufacturer, strength, and form), the date and quantity dispensed, the duration of the prescription, the name and address of the dispensing pharmacy, and the name and license number of the prescribing physician. These data have been previously validated for clinical and research uses.28–31 We prepopulated the RightRx community drug list using all drugs that were dispensed within the last 3 months to account for variation between patients in medication adherence and renewals, using an algorithm that has been previously described.22 For each medication, the algorithm used the last dispensing record to represent the current medication strength (eg, oxycodone 20 mg). The address and phone and fax numbers of dispensing pharmacies and prescribing physicians were obtained by linking the RAMQ data to the licensing rosters of the provincial College of Physicians and Order of Pharmacists. All of these data were inserted into patients’ RightRx records.
Hospital inpatient active drug list: Data were extracted from the hospital pharmacy system (GE Centricity) by using the built-in report generator. A list of all drugs dispensed, stopped, or placed on hold for all patients admitted to the study units was generated daily at 06:00. A new report on changes was generated every 15 min between 06:00 and 24:00. The plain-text report files were automatically parsed to extract drug name, dose per administration, frequency, route, and additional comments. Data were then inserted into patients’ RightRx records.
RightRx features
Alignment and display of medication
An essential requirement to optimize patient safety is aligning the community and hospital drug lists to reduce cognitive load in reconciliation.32–34 Our unique approach departs from the usual practice of sorting community and hospital drug lists alphabetically, where 2 medications that are the same or similar can appear in very different orders on the 2 lists. In addition, to facilitate reconciliation and adjudication, the American Hospital Formulary Classification System was used to group drugs by pharmacologic class, and classes were then ordered by clinical importance based on expert opinion. This approach provides more clinical coherence as medications are reviewed and considered within a group with consistent therapeutic intent (eg, cardiovascular medications, anticoagulants). Drug records in the hospital and community had to be mapped to their generic molecules, then by dose per administration, frequency, and route in order for this matching and ordering to be achieved. This required the use of a monthly updated commercial drug knowledge database, Vigilance Santé,35 to map drug identification numbers in the community drug list to generic molecules, and text strings in the hospital drug information to standardized text strings for the name of the same molecule.
Organization of medication reconciliation action tabs and business logic to support workflow and accreditation requirements
Canadian hospital accreditation requires that each patient have medication reconciliation completed at admission, transfer, and discharge.2,34 The application was designed to support each of these processes, in accordance with the National Institute of Safe Medication Practices requirements for e-medication reconciliation,2 with tabs that allow clinicians to easily switch from admission to transfer and discharge activities. The business logic supports and constrains the actions in each specific activity. For example, at discharge, the reference medication list is the community drug list, so that medications appearing only in the hospital list that are to be continued at discharge are automatically classified as new medications, whereas during transfer between hospital units, these in-hospital medications are classified as continued medications. Many clinicians, including pharmacy technicians, pharmacists, medical students, residents, nurses, and attending physicians, are involved in many different steps in the medication reconciliation process, including validating the community drug list and generating the best possible medication history; reconciling, reviewing, and revising medication orders; and generating the discharge prescription. A combination of role-based permissions, embedded business logic, screen design, and application ergonomics were used to align hospital policy and provincial legal and professional regulatory requirements, along with the various task completion workflows by all the different contributors.22 For example, learners are authorized to enter data and start a task, but only a licensed professional can finalize that task. Using agile development cycles, the application was refined to optimize the user experience and to constrain actions and activities in support of patient safety. For example, most fields are completed using dropdown lists, and free-text entries are limited to fields with less direct patient-care impact.
Prior to admission tab
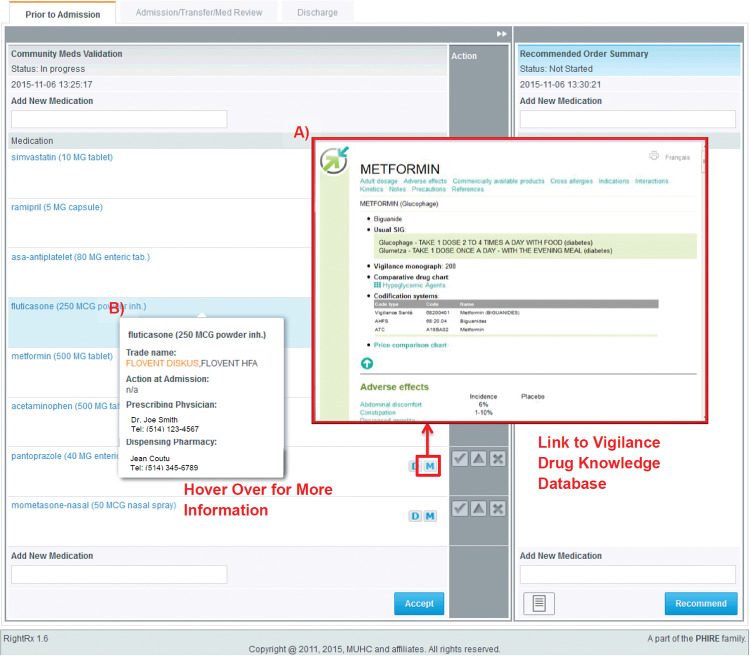
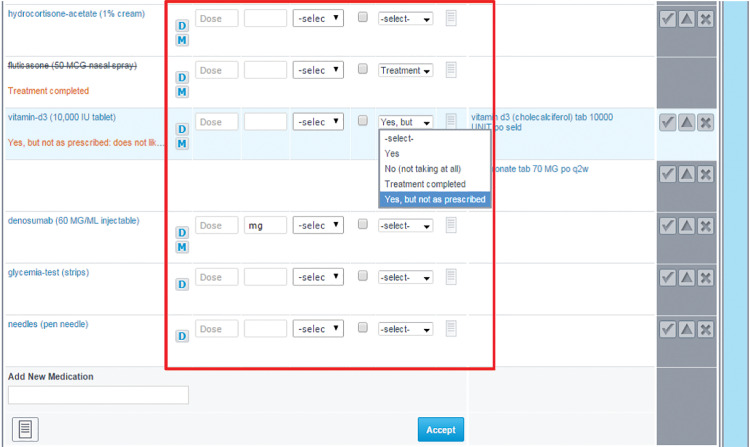
The displayed community drug list is prepopulated with dispensed medication records extracted from the RAMQ system (Figures 1 and 2). To provide a reference for users, each medication is linked to its drug monograph using a commercial drug knowledge base (Figure 2A). Information pertaining to the dispensing pharmacies and prescribing physicians is extracted from the RAMQ system, linked to regulatory body databases for physicians and pharmacists to obtain contact information that is displayed with each medication (Figure 2B). Since the dispensed medication data from the RAMQ do not include medication administration directives (eg, take 2 tablets twice a day), the medication validation entry screen allows documentation of the dose per administration and frequency, as well as patient-reported adherence to prescribed therapy, reasons for nonadherence, and free-text comments to be recorded for each medication (Figure 3).
Figure 2.
Prior to Admission tab. (A) Hover-over option to display more drug, prescribing physician, and dispensing pharmacy information; (B) link to open Vigilance Drug Knowledge Database in a new tab.
Figure 3.
Expanded view for modification or addition of drug information.
Admission/transfer/medication review tab
As medication reconciliation is often done after the patient has been admitted to the hospital, the Admission/Transfer/Med Review tab enables the clinical team to conduct a retrospective review and reconciliation of medications ordered at admission as well as during transfer.2 To avoid flipping between tabs to validate and reconcile medications, the community drug list screen can be pulled across and expanded to enable validation to be done on the Admission/Transfer/Med Review or Discharge tab.
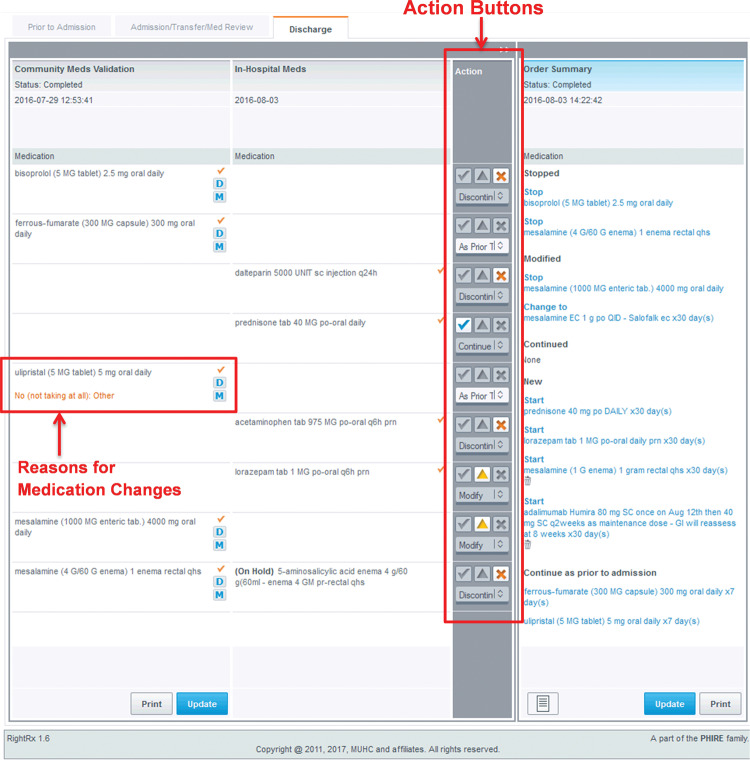
Discharge tab
The Discharge tab functions in the same way as the Admission/Transfer/Med Review tab. The left panel displays the original community drug list against which the current hospital medications list (center panel, Figure 4) is reconciled and reviewed to generate the final discharge prescription (right panel, Figure 4). Hospital-only medications that were stopped are not recorded in the discharge prescription. All other changes, additions, and discontinuations are recorded in the discharge prescription, along with the reasons for those changes. The discharge prescription organizes the medications into bins according to the action taken, starting with the most important, stopped and modified medications, followed by continued and new medications. The finalized discharge prescription is printed, signed, and given to the patient, and a copy is scanned into the hospital chart. A letter summarizing the changes made to the patient’s community drug list is faxed to each of the community-based dispensing pharmacies and prescribing physicians identified from the dispensing data (Figure 1).
Figure 4.
Alignment of the community medication list and the in-hospital medications in the Discharge tab.Action buttons are for users to indicate status of medications at discharge, which are organized into bins (eg, continue, modify, stop). Reasons for any medication change to the community medications can be found in orange text below the community medication.
Functionalities to improve patient safety and medication reconciliation process efficiency
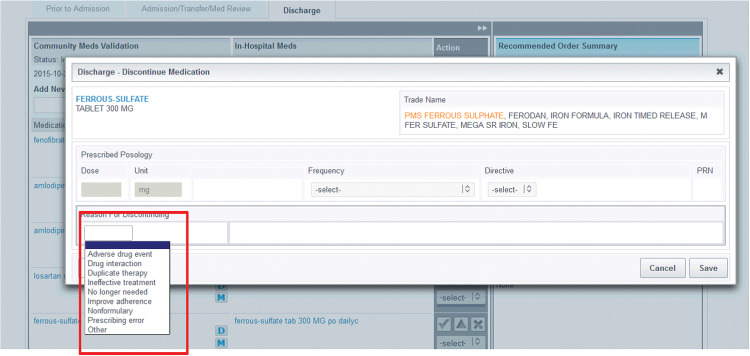
A combination of visual cues, alignment of same and similar drugs, adjacencies of action buttons, hover-over information bubbles, and reminder messages is used to assist in the safe and efficient completion of medication reconciliation tasks. To avoid unintended errors of omission and commission, users must record an action for each medication before the reconciliation activity and frame can be finalized. The action radio buttons beside each medication in both the hospital and community drug lists change to a “disabled” appearance once a selection is made (Figure 4). New medications can be added through an electronic prescriber at the bottom of the review window. As decisions are made and actions recorded, the results appear in the right-most summary pane, with medications organized into bins according to the action taken. For each decision to change a medication, the clinician is required to record a reason from a dropdown list (Figure 5), with a free-text option for exceptional cases. The reasons for changes are printed with the order, for both in-hospital orders and discharge prescriptions. All new medications prescribed through RightRx also include a mandatory field indicating the therapeutic intent, via a dropdown list containing on-label and off-label uses of a drug. An optional free-text entry is available for exceptional cases.
Figure 5.
List of reasons for discontinuing medications are available to be selected in a drop-list format when discontinuing a medication.
RightRx implementation
The implementation process was multifaceted. First, overall support for the implementation of the RightRx solution was sought and received from the MUHC senior management team. Second, unit directors were engaged to gain their support and leadership in the best strategy for staged implementation, including the engagement and support of unit staff. Some of the additional software requirements were identified at this stage, and implementation was delayed until critical requirements for adoption were met. Dedicated computers and printers were purchased for each unit to maximize ease of access. Field staff first trained the champion users on the unit, usually those with the primary responsibility for medication reconciliation, then gradually expanded training and support for primary users: residents, pharmacists, nurse practitioners, medical and pharmacy students, and pharmacy technicians, and eventually staff physicians and nurses who played a smaller role in the day-to-day process. The analysis team monitored weekly admissions, discharges, and usage for discussion at bimonthly implementation review meetings.
Medication reconciliation completion rate
The RightRx medication reconciliation solution was implemented in 2 hospital units, general internal medicine and cardiac surgery, and medication reconciliation completion rates were compared with 2 control units, general internal medicine and thoracic surgery, in the first 20 months of the trial. To measure medication reconciliation rates, we first retrieved the files of all patients admitted to and discharged from the intervention and control units from the hospital information system. Each patient’s community drug list, for both intervention and control units, was retrieved from the RAMQ medication database. Medication reconciliation completion was determined by chart review, and by documentation in the RightRx software. Medication reconciliation was defined as completed if the disposition of each of the community drugs (ie, continue, stop, or modify dose) was documented in the chart at discharge. Medication reconciliation was defined as “not attempted” if there was no documentation on the disposition of any of the community medications at discharge. Partial documentation of some but not all community medications was considered partially completed reconciliation, divided into major incomplete if >25% of medications were not reconciled and minor if ≤25% medications were not adjudicated.
Analysis
Patient characteristics were summarized using descriptive characteristics. Differences in the proportion of patients with completed, partial, or no medication reconciliation in the intervention and control groups were tested using a chi-square test. Multivariate logistic regression was used to determine if there were significant differences in medication completion rates in the intervention and control groups after adjusting for differences in patient age, sex, number of medications, and number of community-based prescribing physicians and pharmacies, overall and for medical and surgical units separately.
Ethics approval
This study was approved by the MUHC Ethics Board (10-180 GEN). All patients provided written consent to be included in this study.
RESULTS
Challenges in implementation and solutions
The Clinical Adoption Framework was used to classify challenges encountered in implementation, as it allows the sociotechnical aspects of health care organizations to be considered in evaluating health IT adoption at the macro, meso, and micro levels.36 The main challenges arose in the macro-governance, meso-people, and micro–net benefits and quality of health IT dimensions. The additional user requirements and development needed to resolve these issues are summarized in Table 1.
Macro-governance and meso-people dimensions
Legal and professional issues
Discharging physician’s role in prescribing community-based medication: In the initial workflow model, the physician discharging the patient took full responsibility for prescribing all medications at discharge after the reconciliation process was completed. However, many physicians were concerned about renewing or modifying community medications they did not start, for which they did not know the indication, where they may have disagreed with the medication’s use but did not want to stop it, or where they did not want to be the physician on record as the last prescriber for a chronic medication that would require refills. As a result, surgeons commonly wrote “continue all previous home medications” on the paper discharge prescription.
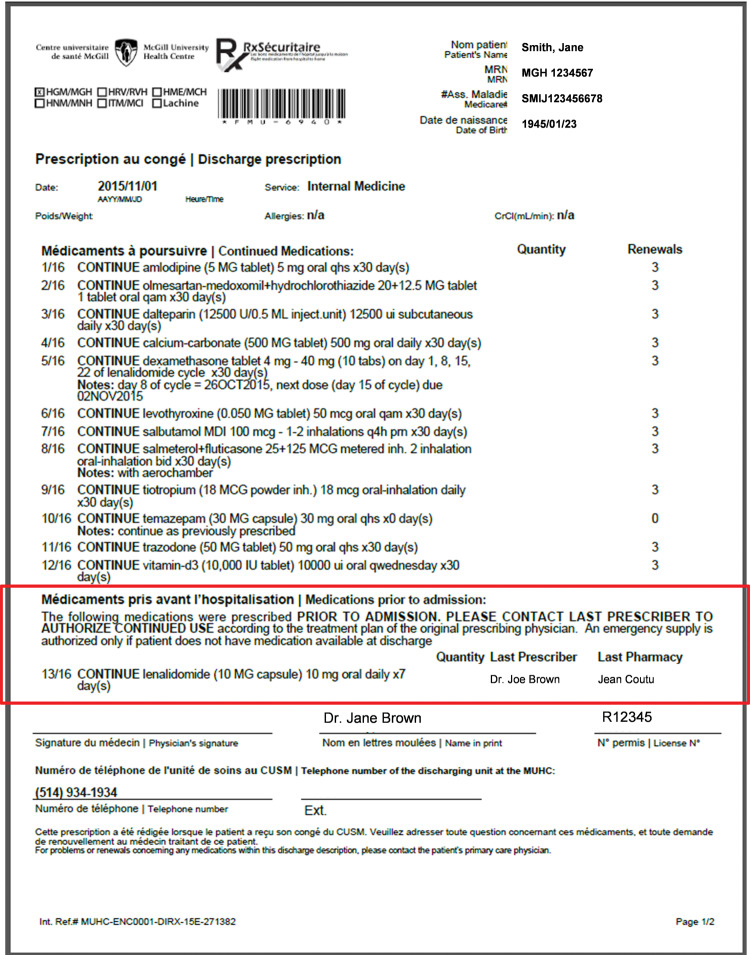
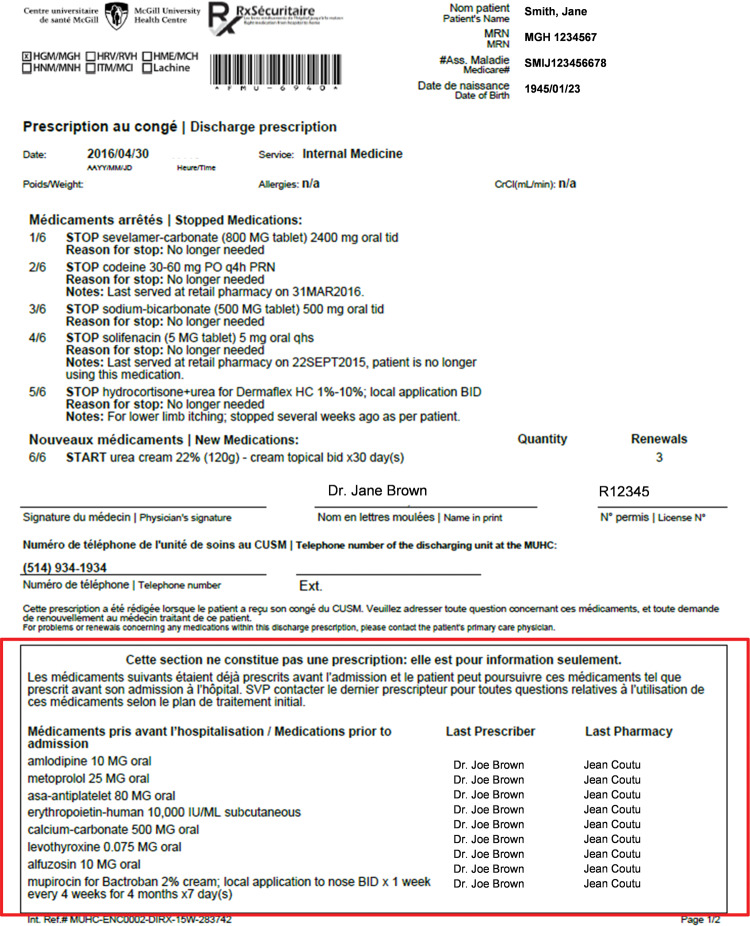
Due to the lack of a pan-Canadian consensus regarding the legal responsibilities of the discharging physician, 2 versions of the software were developed. In both versions, a fourth action button, labeled “continue as previous,” was added. In a legal environment where the physician is expected to be the prescriber for all discharge medications, the “continue as previous” action button allocates these medications into a fifth bin, Medications Prior to Admission (Figure 6A). The community-based prescribing physician and dispensing pharmacy and their contact information are listed, and a 7-day emergency supply is prescribed, with the message that the prescription is to be filled only if the patient does not have medication available at discharge. In an environment where the discharging physician is not mandated to prescribe all community-based medication, a second version of the software implements the business rule that use of the “continue as previous” button groups those selected medications into an information box, indicating that the printout is not a prescription and that those medications should be continued by the original community-based pharmacy and prescribing physician listed (Figure 6B).
Figure 6.
(A) “Continue as previous” medications on the discharge prescription (version 1).
Please note that the patient, physician, and pharmacist information are simulated examples.
Pharmacist review recommendations and physician orders: Clinical pharmacists frequently complete the community drug list validation, medication review, and reconciliation. Although pharmacists are not authorized in Quebec to prescribe in the hospital setting, their scope of practice emphasizes making medication recommendations to improve safety and efficacy. In the early versions of RightRx, if the physician made changes to the pharmacist-recommended orders (that only the physician had the right to approve), there was no official record of the pharmacist’s recommendations. To adhere to the pharmacist’s professional and legal responsibility for medication review, a new “consult” document was created that allows pharmacists to save their recommended order summaries so that they can be scanned into patient records. Scopes of practice are changing, and the use of role-based rules enables the application to accommodate differences between jurisdictions and changes over time.
Micro-net benefits of health IT dimension
Exposing prior clinical reasoning details: Since many different clinicians may be involved in medication management during a patient’s hospital stay, we needed to adapt the RightRx solution to display the reasons documented for any changes to the community medications as well as the pharmacists’ notes on medication adherence (Figure 4). The last change and reason are now shown, and the user can, with a single click, optionally access all historical data. This feature was needed for the discharging physician, who often was not involved in a patient’s previous care.
Generic molecule dose–basedvs product-based prescribing: In keeping with the Quebec provincial policy of product-based prescribing for electronic prescribing solutions, the initial design of the RightRx prescriber module required physicians to choose a drug product from a dropdown list (eg, Apo-Ciproflox 250 mg) and calculate and enter the number of tablets/capsules/ml per administration to obtain the dose required per administration and the frequency of administrations per day. However, product-based prescribing is not congruent with physician training, and additional cognitive load is involved in calculating the dose per administration (eg, 5 mg/day = 2 × 2.5 mg/tab), which creates a potential source of error. Indeed, an incident occurred early in the course of implementation where the units/administration field was used to enter the intended daily dose of 5 mg of warfarin, resulting in a prescription of 5× warfarin (2.5 mg/tab), for a total of 12.5 mg being prescribed. The RightRx prescribing module was subsequently modified to support dose-based prescribing, whereby physicians select the generic molecule they wish to prescribe and enter the dose per administration and frequency per day. The community pharmacist then determines which product to dispense.
Micro-quality of health IT
Unstructured data and missing medication administration directives: The RAMQ community dispensed medication data, which were used to prepopulate the community drug list, do not include the dose per administration and frequency. The clinician validating the community drug list with the patient has to complete these fields.
The hospital pharmacy reports sometimes contain text strings, which cannot be easily parsed into a structured format to yield drug dose and frequency with which to compare against the corresponding community drug. In these instances, where there is uncertainty and the clinician continues the drug at discharge, the business rules conservatively assume that the dose may have been changed and allocates the prescribed medication into the “modified” bin, indicating that the original community drug was stopped and that same drug is now prescribed at a specified dose.
RightRx use-intervention units
Pharmacists, physicians, and pharmacy students were the professionals involved with the community drug list validation and post-admission reconciliation for 88.4%, 20.2%, and 13.0% of patients, respectively (Table 2). At discharge, physicians completed medication reconciliation and generated discharge prescriptions for 96.1% of patients. Pharmacists were also heavily involved in the discharge process, contributing to recommended discharge prescriptions for 74.7% of patients. The overall mean (Sd) time during each RightRx session was 10.9 min (10.9 min) for pharmacists and 5.8 min (7.8 min) for physicians. On average, during each patient stay, a pharmacist accessed each patient’s files 3.3 (2.5) times, and a physician accessed them 1.9 (1.4) times (Table 2). Usage between the medical and surgical RightRx units was similar, with the general internal medicine unit having slightly higher rates of access by physicians and pharmacists.
Table 2.
Use of the RightRx application by different health professionals for patients in medical and surgical units
| Role | Patient files accessed for admission reconciliation (%) | Patient files accessed for discharge reconciliation (%) | Overall |
Internal Medicine |
Cardiac Surgery |
|||
|---|---|---|---|---|---|---|---|---|
| Average no. of accesses per patient stay, mean ± SD | Mean time spent per access (min), mean ± SD | Average no. of accesses per patient stay, mean ± SD | Mean time spent per access (min), mean ± SD | Average no. of accesses per patient stay, mean ± SD | Mean time spent per access (min), mean ± SD | |||
| Physician | 21.4 | 96.1 | 1.9 ± 1.4 | 5.8 ± 7.8 | 2.2 ± 1.7 | 5.8 ± 7.2 | 1.5 ± 1.0 | 5.7 ± 8.8 |
| Pharmacist | 85.6 | 71.9 | 3.3 ± 2.5 | 10.9 ± 10.9 | 3.5 ± 2.8 | 10.8 ± 10.6 | 2.9 ± 1.9 | 11.1 ± 11.5 |
| Pharmacy Studenta | 13.5 | 3.0 | 2.4 ± 1.5 | 12.3 ± 11.7 | 2.4 ± 1.5 | 12.3 ± 11.7 | ||
| Medical Student | 5.9 | 12.2 | 1.9 ± 2.8 | 6.9 ± 7.9 | 1.4 ± 1.2 | 7.3 ± 6.7 | 2.4 ± 3.7 | 6.6 ± 8.6 |
| Nurse Practitionerb | 2.6 | 4.5 | 1.4 ± 0.6 | 11.3 ± 11.9 | 1.4 ± 0.6 | 11.3 ± 11.9 | ||
| Nurse | 1.0 | 0.5 | 1.1 ± 0.3 | 0.37 ± 0.3 | 1.1 ± 0.3 | 0.37 ± 0.3 | ||
aPharmacy students were only available in the internal medicine unit.
bNurse practitioners only worked in the cardiac surgery unit.
Medication reconciliation: intervention vs control units
Patient characteristics
Among the 2916 patients admitted to the intervention and control units, 41.6% were female, and the mean age was 69.6 years (Table 3). Intervention unit patients were slightly older, and there was a higher proportion of male patients, mainly attributable to a higher proportion of male patients being admitted to the cardiac surgery unit. While 14.5% of patients had no prescription medication prior to admission, 15.8% in the control units and 13.0% in the intervention units had ≥16 prescribed medications. The majority of patients had 2–4 community-based prescribing physicians and 1 pharmacy from which their medications were dispensed.
Table 3.
Characteristics of the 2916 study patients in the RightRx intervention and control units
| Characteristics | Overall | Control | Intervention |
|---|---|---|---|
| (N = 2916) | (N = 1506) | (N = 1410) | |
|
Mean (SD) |
Mean (SD) |
Mean (SD) |
|
| Age | 69.0 (15.3) | 68.1 (16.4) | 70.0 (14.0) |
| Sex |
N (%) |
N (%) |
N (%) |
| Female | 1213 (41.6) | 691 (45.9) | 522 (37.0) |
| Male | 1703 (58.4) | 815 (54.1) | 888 (63.0) |
|
Community-based medication use at admission | |||
| Number of medications | |||
| 0 medications | 424 (14.5) | 200 (13.3) | 224 (15.9) |
| 1–5 medications | 632 (21.7) | 346 (23.0) | 286 (20.3) |
| 6–10 medications | 828 (28.4) | 391 (26.0) | 437 (31.0) |
| 11–15 medications | 610 (20.9) | 331 (22.0) | 279 (19.8) |
| ≥16 medications | 422 (14.5) | 238 (15.8) | 184 (13.0) |
| Number of prescribing physiciansa | |||
| 0 physicians | 424 (14.5) | 200 (13.3) | 224 (15.9) |
| 1 physician | 467 (16.0) | 241 (16.0) | 226 (16.0) |
| 2–4 physicians | 1386 (47.5) | 703 (46.7) | 683 (48.4) |
| ≥5 physicians | 639 (21.9) | 362 (24.0) | 277 (19.6) |
| Number of pharmacies | |||
| 0 pharmacies | 424 (14.5) | 200 (13.3) | 224 (15.9) |
| 1 pharmacy | 1979 (67.9) | 1006 (66.8) | 973 (69.0) |
| ≥2 pharmacies | 513 (17.6) | 300 (19.9) | 213 (15.1) |
aPrescribing physicians include specialists as well as general practitioners.
Medication reconciliation status: interventionvs control units
The overall medication reconciliation completion rate was 88.1% in the RightRx intervention units compared to 46.3% in the control units (χ2: 569.7, P < .0001) (Table 4). The rates of incomplete medication reconciliation and failure to conduct any medication reconciliation were also was significantly lower in the intervention units. Medication reconciliation completion rates differed for the medical and surgical units, with the most marked impact of the intervention being in the surgical units, with completion rates of 80.7% in the intervention unit compared to 0.7% in the control units. However, even on the medical units that had a tradition of undertaking medication reconciliation, there was a significantly higher rate of medication reconciliation completion in the intervention unit (96.0%) compared to the control unit (82.7%).
Table 4.
Medication reconciliation status in the RightRx intervention and control units for the 2916 patients enrolled in the study in the first 20 months
| Medication reconciliation | Overall |
|||
|---|---|---|---|---|
| Control | Intervention | Chi-square | ||
| (N = 1506) |
(N = 1410) |
|||
| N (%) | N (%) | Value | P-value | |
| Completea | ||||
| Yes | 698 (46.3) | 1242 (88.1) | 569.7 | <.0001 |
| No | 808 (53.7) | 168 (11.9) | ||
| Major incompleteb | ||||
| Yes | 395 (26.2) | 52 (3.7) | 285.1 | <.0001 |
| No | 1111 (73.8) | 1358 (96.3) | ||
| Minor incompletec | ||||
| Yes | 228 (15.1) | 67 (4.8) | 86.4 | <.0001 |
| No | 1278 (84.9) | 1343 (95.2) | ||
| Not attemptedd | ||||
| Yes | 98 (6.5) | 3 (0.2) | 86.3 | <.0001 |
| No | 1408 (93.5) | 1407 (99.8) | ||
|
Internal medicine units |
||||
| Completea | ||||
| Yes | 693 (82.7) | 652 (96.0) | 66.3 | <.0001 |
| No | 145 (17.3) | 27 (4.0) | ||
| Major incompleteb | ||||
| Yes | 20 (2.4) | 4 (0.6) | 7.8 | .005 |
| No | 818 (97.6) | 678 (99.4) | ||
| Minor incompletec | ||||
| Yes | 114 (13.6) | 3 (0.4) | 91.3 | <.0001 |
| No | 724 (86.4) | 676 (99.6) | ||
| Not attemptedd | ||||
| Yes | 12 (1.4) | 1 (0.1) | 7.3 | .007 |
| No | 826 (98.6) | 678 (99.9) | ||
|
Surgical units |
||||
| Completea | ||||
| Yes | 5 (0.7) | 590 (80.7) | 913.1 | <.0001 |
| No | 663 (99.3) | 141 (19.3) | ||
| Major incompleteb | ||||
| Yes | 375 (56.1) | 48 (6.6) | 406.6 | <.0001 |
| No | 293 (43.9) | 683 (93.4) | ||
| Minor incompletec | ||||
| Yes | 114 (17.1) | 64 (8.8) | 21.7 | <.0001 |
| No | 554 (82.9) | 667 (91.2) | ||
| Not attemptedd | ||||
| Yes | 86 (12.9) | 2 (0.3) | 94.0 | <.0001 |
| No | 582 (87.1) | 729 (99.7) | ||
aPatients with electronic discharge prescriptions or paper medication reconciliation forms.
bPatients with ≥25% of community medications that were NOT acted upon during hospitalization.
cPatients with <25% of community medications that were NOT acted upon during hospitalization.
dPatients without electronic prescriptions OR paper medication reconciliation forms, or who had all of their drugs NOT acted upon.
Overall medication reconciliation completion rates, adjusting for patient characteristics
After adjusting for patient characteristics, the odds of medication reconciliation being completed in the intervention units were 9 times greater than in the control units (odds ratio [OR]: 9.0, 95% confidence interval [CI], 7.4-10.9, P < .0001) (Table 5). The odds of medication reconciliation being completed increased with patient age and with higher numbers of community-based medications. However, the odds of medication reconciliation being completed decreased by 16% (OR: 0.84, 95% CI, 0.73-0.98, P = .03) if patients used 2 or more community-based pharmacies, as hospital-based pharmacists typically only request information from 1 pharmacy and thus have incomplete information.
Table 5.
Comparison of overall medication reconciliation completion rates between the RightRx intervention and control units, adjusting for patient characteristics
| Patient characteristics | MedRec completion rate (%) | Odds of aMedRec completion | P-value |
|---|---|---|---|
| (95% CI) | |||
| Intervention group | |||
| Control | 46.3 | Reference | |
| Intervention | 88.1 | 9.01 | <.0001 |
| (7.41-10.95) | |||
| Age (increase per 10 years) | – | 1.09 | .003 |
| (1.03-1.16) | |||
| 18–34 | 62.1 | – | – |
| – | |||
| 35–49 | 65.2 | – | – |
| – | |||
| 50–64 | 61.9 | – | – |
| – | |||
| ≥65 | 68.3 | – | – |
| – | |||
| Sex | |||
| Female | 65.5 | Reference | |
| Male | 67.3 | 0.91 | .30 |
| (0.76-1.09) | |||
| Number of medications | – | 1.05 | <.0001 |
| (1.03-1.07) | |||
| 0 medications | 66.3 | – | – |
| 1–5 medications | 58.9 | – | – |
| 6–10 medications | 65.8 | – | – |
| 11–15 medications | 67.9 | – | – |
| ≥16 medications | 77.7 | – | – |
| Number of prescribing physiciansb | – | 1.01 (0.96-1.07) | .65 |
| 0 physicians | 66.3 | – | – |
| 1 physician | 62.2 | – | – |
| 2–4 physicians | 67.0 | – | – |
| ≥5 physicians | 68.9 | – | – |
| Number of pharmacies | – | 0.84 (0.73-0.98) | .03 |
| 0 pharmacies | 66.3 | – | – |
| 1 pharmacy | 67.1 | – | – |
| ≥2 pharmacies | 64.5 | – | – |
aAdjusted for age, sex, number of medications, number of prescribing physicians, and number of pharmacies. Intercept of the model was found to be −0.9565.
bPrescribing physicians include specialists as well as general practitioners.
DISCUSSION
To our knowledge, RightRx, the computer-assisted medication reconciliation solution described in this study, is the first to use a population-based administrative data warehouse containing dispensed medication records to prepopulate a community drug list and automatically align it with hospital-based medications. We achieved medication reconciliation completion rates of 80%–96% in the intervention, a 9-fold increase compared to the control units, even in surgery, where there was little to no prior activity to reconcile medications.17 There are several factors that we believe contributed to our success. Support was provided by senior hospital and clinical unit leadership, clinical champions existed at the unit level, field staff provided ongoing training and feedback to the scientific and development team about technical, usability, and professional issues, weekly adoption rates were analyzed, and the development team responded to modify the application and system to address priority issues.
Increasingly, population-based clinical data repositories are being put in place in different regions.37 Integrating these data into the medication reconciliation process should enable improvements that were seen in this study in both the efficiency and completeness of the process. RightRx was developed with federal research and innovation funding, with the expectation that this software could be tested at the McGill University Health Centre and, if successful, would be available for deployment in other hospitals. With this in mind, we developed the solution to meet the Canadian Institute of Safe Medication Practices for electronic medication reconciliation as well as Accreditation Canada standards for medication reconciliation. The transferability of RightRx to other institutions is unknown and will likely depend on local leadership, the extent of integration of health informatics into care in the outpatient and inpatient areas, and preexisting medication reconciliation practices.
The efficiency and effectiveness of a computer-assisted medication reconciliation solution could be further improved by addressing remaining challenges. First, there could be enormous gains in efficiency and safety if medication administration directives and instructions were standardized according to existing national or international standards.38–40 Structured data on drug, dose, frequency, and route could be achieved by parsing text strings from hospital and community-dispensed medication using current or future advances in this area41 or instituting standards within source systems. Doing so would eliminate repetitive data entry and would provide an accurate method of assessing intended and unintended dose changes at transitions in care.
Second, to enhance the safety and efficiency of dose-based prescribing, order sentences could be incorporated into e-prescribing systems. The physician, when prescribing a drug, would select from complete orders that would specify the drug, dose per administration, frequency, route, quantity, and duration when relevant. Order sentences should also incorporate the therapeutic intent, as knowledge of the therapeutic indication would facilitate medication review and the discontinuation of unnecessary therapy, and would provide an additional safeguard to prevent errors in dispensing.42
Consistent with recommended best practice,43,44 physicians and pharmacists involved in medication management in the community were all sent letters with information about changes made during hospitalization. An important asset in facilitating communication was the automated retrieval of the contact information and names of all prescribing physicians and dispensing pharmacies, particularly when most patients had 2–4 prescribing physicians. However, there is evidence that providing the same information to patients may be essential to reduce misunderstandings in medication changes at discharge.43,45 One study found a reduction in medication nonadherence for cardiac patients when patient-specific information on changes in community-based medication was provided at discharge.43 Future computer-assisted medication reconciliation solutions should generate a “patient-friendly” information sheet on the changes made to a patient’s medication regimen during the hospital stay, and provide it either with the printed discharge prescription or electronically through a patient portal.45
There are limitations that need to be considered in the interpretation of results. The high rates of adherence in the intervention units may be partially attributable to the Hawthorne effect.46 The research field team was highly visible on both control and intervention units in order to obtain consent from patients, they actively sought feedback from the users on the intervention units, and their attention may have contributed to higher completion rates. The study was conducted in one tertiary academic facility, and the reproducibility of these improvements in medication reconciliation completion rates in other settings will need to be evaluated.
In conclusion, we achieved high levels of medication reconciliation completion through the use of a computer-assisted tool, even in units that had not previously conducted medication reconciliation. Automated prepopulation of drug data, the use of a clinician-focused medication sort order, and a combination of business rules, software design, and ergonomics contributed to an easy-to-use application that supported this improvement. Professional, legal, and technical issues were identified and resolved during implementation. Future development should focus on standardization of medication administration data, order sentences to support dose-based prescribing, and patient-friendly information about medication changes.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGEMENTS
We wish to acknowledge André Bonnici, Dr Laurence Green, and Dr Renzo Cecere for their continued support throughout the project, as well as all the users for their valuable feedback and participation in this project.
References
- 1. Leotsakos A, Zheng H, Croteau R et al. , Standardization in patient safety: the WHO High 5s project. Int J Qual Health Care. 2014;262:109–16. [DOI] [PubMed] [Google Scholar]
- 2. Accreditation Canada, the Canadian Patient Safety Institute, and the Institute for Safe Medication Practices Canada. Medication Reconciliation in Canada: Raising the Bar. Progress to date and the course ahead. Ottawa, ON: Accreditation Canada; 2012. [Google Scholar]
- 3. Bell CM, Brener SS, Gunraj N et al. , Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;3068:840–47. [DOI] [PubMed] [Google Scholar]
- 4. Miller SL, Miller S, Balon J, Helling TS. Medication reconciliation in a rural trauma population. Ann Emerg Med. 2008;525:483–91. [DOI] [PubMed] [Google Scholar]
- 5. van den Bemt PM, van den Broek S, van Nunen AK, Harbers JB, Lenderink AW. Medication reconciliation performed by pharmacy technicians at the time of preoperative screening. Ann Pharmacother. 2009;435:868–74. [DOI] [PubMed] [Google Scholar]
- 6. Lubowski TJ, Cronin LM, Pavelka RW, Briscoe-Dwyer LA, Briceland LL, Hamilton RA. Effectiveness of a medication reconciliation project conducted by PharmD students. Am J Pharm Educ. 2007;715:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Paparella S. Medication reconciliation: doing what's right for safe patient care. J Emerg Nurs. 2006;326:516–20. [DOI] [PubMed] [Google Scholar]
- 8. Schwarz M, Wyskiel R. Medication reconciliation: developing and implementing a program. Crit Care Nurs Clin North Am. 2006;184:503–07. [DOI] [PubMed] [Google Scholar]
- 9. Haig K. Medication reconciliation. Am J Med Qual. 2006;215:299–303. [DOI] [PubMed] [Google Scholar]
- 10. Saufl NM. Reconciliation of medications. J Perianesth Nurs. 2006;212:126–27. [DOI] [PubMed] [Google Scholar]
- 11. Bayley K, Savitz L, Maddalone T, Stoner S, Hunt J, Wells R. Evaluation of patient care interventions and recommendations by a transitional care pharmacist. Therapeutics Clin Risk Manag. 2007;34:695–703. [PMC free article] [PubMed] [Google Scholar]
- 12. Varkey P, Resar RK. Medication reconciliation implementation in an academic center. Am J Med Qual. 2006;215:293–95. [DOI] [PubMed] [Google Scholar]
- 13. Kemp LO, Narula P, McPherson ML, Zuckerman I. Medication reconciliation in hospice: a pilot study. Am J Hosp Palliat Care. 2009;263:193–99. [DOI] [PubMed] [Google Scholar]
- 14. Ledger S, Choma G. Medication reconciliation in hemodialysis patients. CANNT J. 2008;184:41–43. [PubMed] [Google Scholar]
- 15. Gleason KM, Groszek JM, Sullivan C, Rooney D, Barnard C, Noskin GA. Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients. Am J Health-Sys Pharm. 2004;6116:1689–95. [DOI] [PubMed] [Google Scholar]
- 16. Weingart SN, Cleary A, Seger A et al. , Medication reconciliation in ambulatory oncology. Jt Comm J Qual Patient Saf. 2007;3312:750–57. [DOI] [PubMed] [Google Scholar]
- 17. Marien S, Krug B, Spinewine A. Electronic tools to support medication reconciliation: a systematic review. J Am Med Inform Assoc. 2017;241:227–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Meguerditchian AN, Krotneva S, Reidel K, Huang A, Tamblyn R. Medication reconciliation at admission and discharge: a time and motion study. BMC Health Services Res 2013;13:485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Poon EG, Blumenfeld B, Hamann C et al. , Design and implementation of an application and associated services to support interdisciplinary medication reconciliation efforts at an integrated healthcare delivery network. J Am Med Inform Assoc. 2006;136:581–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schnipper JL, Hamann C, Ndumele CD et al. , Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Int Med. 2009;1698:771–80. [DOI] [PubMed] [Google Scholar]
- 21. Lesselroth BJ, Felder RS, Adams SM et al. , Design and implementation of a medication reconciliation kiosk: the Automated Patient History Intake Device (APHID). J Am Med Inform Assoc. 2009;163:300–04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tamblyn R, Huang AR, Meguerditchian AN et al. , Using novel Canadian resources to improve medication reconciliation at discharge: study protocol for a randomized controlled trial. Trials. 2012;13:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McGill University Health Centre. Partnerships Moving Forward Together: The MUHC 2015–2016 Annual Report. 2016:1–19. [Google Scholar]
- 24. Manifesto for Agile Software Development. 2001. http://agilemanifesto.org/ Accessed August 28, 2017. [Google Scholar]
- 25. Lee G, Xia W. Toward agile: an integrated analysis of quantitative and qualitative field data on software development agility. MIS Quarterly. 2010;341:87–114. [Google Scholar]
- 26. Dingsøyr T, Nerur S, Balijepally V, Moe NB. A decade of agile methodologies: towards explaining agile software development. J Syst Software. 2012;856:1213–21. [Google Scholar]
- 27. Tamblyn R, Huang A, Perreault R et al. , The medical office of the 21st century (MOXXI): effectiveness of computerized decision-making support in reducing inappropriate prescribing in primary care. CMAJ. 2003;1696:549–56. [PMC free article] [PubMed] [Google Scholar]
- 28. Wilchesky M, Tamblyn RM, Huang A. Validation of diagnostic codes in medical services claims data. Can J Clin Pharmacol. 2001;81:39. [DOI] [PubMed] [Google Scholar]
- 29. Tamblyn R, Reid T, Mayo N, McLeod P, Churchill-Smith M. Using medical services claims to assess injuries in the elderly: sensitivity of diagnostic and procedure codes for injury ascertainment. J Clin Epidemiol. 2000;532:183–94. [DOI] [PubMed] [Google Scholar]
- 30. Levy AR, Tamblyn RM, Fitchett D, McLeod PJ, Hanley JA. Coding accuracy of hospital discharge data for elderly survivors of myocardial infarction. Can J Cardiol. 1999;1511:1277–82. [PubMed] [Google Scholar]
- 31. Tamblyn R, Lavoie G, Petrella L, Monette J. The use of prescription claims databases in pharmacoepidemiological research: the accuracy and comprehensiveness of the prescription claims database in Quebec. J Clin Epidemiol. 1995;488:999–1009. [DOI] [PubMed] [Google Scholar]
- 32. Plaisant C, Chao T, Wu J et al. , Twinlist: novel user interface designs for medication reconciliation. AMIA Annu Symp Proc. 2013;2013:1150–59. [PMC free article] [PubMed] [Google Scholar]
- 33. Markowitz E, Bernstam EV, Herskovic J et al. , Medication reconciliation: work domain ontology, prototype development, and a predictive model. AMIA Annu Symp Proc. 2011;2011:878–87. [PMC free article] [PubMed] [Google Scholar]
- 34. The Electronic Medication Reconciliation Group. Paper to Electronic MedRec Implementation Toolkit. ISMP Canada and Canadian Patient Safety Institute; 2014. [Google Scholar]
- 35. Vigilance Santé, Quebec, Canada: www.vigilance.ca/ 2013. Accessed July 7, 2017. [Google Scholar]
- 36. Craven CK, Doebbeling B, Furniss D, Holden RJ, Lau F, Novak LL. Evidence-based health informatics frameworks for applied use. Stud Health Technol Inform. 2016;222:77–89. [PubMed] [Google Scholar]
- 37. Groseclose SL, Buckeridge DL. Public health surveillance systems: recent advances in their use and evaluation. Annu Rev Public Health. 2017;38:57–79. [DOI] [PubMed] [Google Scholar]
- 38. National Health Service. NHS Dose Syntax Recommendations 2015. UK: National Health Service; 2015. [Google Scholar]
- 39. ISMP. ISMP’s Guidelines for Standard Order Sets. Canada: Institute for Safe Medication Practices; 2010. [Google Scholar]
- 40. Schiff G. Standardized pill imprint codes: a pharma fantasy. J Med Syst. 2004;281:1–7. [DOI] [PubMed] [Google Scholar]
- 41. Jiang M, Wu Y, Shah A, Priyanka P, Denny JC, Xu H. Extracting and standardizing medication information in clinical text – the MedEx-UIMA system. AMIA Jt Summits Transl Sci Proc. 2014;2014:37–42. [PMC free article] [PubMed] [Google Scholar]
- 42. Schiff GD, Klass D, Peterson J, Shah G, Bates DW. Linking laboratory and pharmacy: opportunities for reducing errors and improving care. [Review] [106 refs]. Arch Int Med. 2003;1638:893–900. [DOI] [PubMed] [Google Scholar]
- 43. Hohmann C, Neumann-Haefelin T, Klotz JM, Freidank A, Radziwill R. Providing systematic detailed information on medication upon hospital discharge as an important step towards improved transitional care. J Clin Pharm Ther. 2014;393:286–91. [DOI] [PubMed] [Google Scholar]
- 44. Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;25:314–23. [DOI] [PubMed] [Google Scholar]
- 45. Heyworth L, Paquin AM, Clark J et al. , Engaging patients in medication reconciliation via a patient portal following hospital discharge. J Am Med Inform Assoc. 2014;21(e1):e157–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Berthelot JM, Le Goff B, Maugars Y. The Hawthorne effect: stronger than the placebo effect? Joint Bone Spine. 2011;784:335–36. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.