Abstract
Objective
Randomised controlled trials (RCTs) have shown tocilizumab (TCZ) administered intravenously or subcutaneously with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) to be superior to csDMARDs alone for improving rheumatoid arthritis (RA) disease activity. This study evaluated the effect of TCZ-intravenous and TCZ-subcutaneous on patient-reported outcomes (PROs) in three RCT populations.
Methods
OPTION (NCT00106548), BREVACTA (NCT01232569) and SUMMACTA (NCT01194414) were independent RCTs evaluating the efficacy and safety of TCZ-intravenous and/or TCZ-subcutaneous with csDMARDs in patients with RA. PROs included patient global assessment, pain, Health Assessment Questionnaire-Disability Index, Functional Assessment of Chronic Illness Therapy-Fatigue and Short Form-36. Study outcomes included the proportions of patients reporting changes from baseline in PRO scores ≥ minimum clinically important differences (MCID) and scores ≥ age and gender-matched normative values.
Results
In OPTION, more patients who received TCZ-intravenous reported improvements in PROs ≥MCID (50%–82% vs 31%–57%) and scores ≥ normative values (16%–44% vs 5%–28%) at week 16 compared with placebo. Similarly, a greater proportion of patients in BREVACTA who received TCZ-subcutaneous reported improvements ≥ MCID (54%–73% vs 42%–55%) and scores ≥ normative values (8%–34% vs 4%–25%) at week 12 compared with placebo. In SUMMACTA, 61%–84% of patients who received TCZ-subcutaneous and 64%–84% of those who received TCZ-intravenous reported improvements ≥ MCID and 14%–41% and 15%–24%, respectively, scores ≥ normative values at week 24.
Conclusions
TCZ-intravenous or TCZ-subcutaneous with csDMARDs resulted in more patients reporting clinically meaningful improvements and PRO scores ≥ normative values compared with placebo. These improvements were similar with TCZ-intravenous and TCZ-subcutaneous.
Keywords: biologic therapy, patient-reported outcomes, rheumatoid arthritis, tocilizumab
Key messages.
What is already known about this subject?
In randomised controlled trials (RCTs), tocilizumab (TCZ) administered intravenously or subcutaneously with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) has been shown to be superior to csDMARDs alone for improving disease activity in patients with active rheumatoid arthritis (RA); however, data are limited regarding the impact of TCZ-intravenous or TCZ-subcutaneous with csDMARDs vs csDMARDs alone on patient-reported outcomes (PROs).
What does this study add?
In this post hoc analysis of three RCT populations (OPTION, BREVACTA and SUMMACTA), patients with RA treated with TCZ-intravenous or TCZ-subcutaneous with csDMARDs or csDMARDs alone reported clinically meaningful improvements in PROs, including patient global assessment, pain, Health Assessment Questionnaire-Disability Index, Functional Assessment of Chronic Illness Therapy-Fatigue and Short Form-36.
TCZ-intravenous or TCZ-subcutaneous with csDMARDs resulted in greater mean improvements from baseline in PRO scores and more patients reporting clinically meaningful PRO improvements and PRO scores ≥ age and gender-matched normative values compared with csDMARDs alone, whereas treatment with TCZ-intravenous or TCZ-subcutaneous resulted in similar improvements in PROs.
How might this impact on clinical practice?
Treatment with TCZ-intravenous or TCZ-subcutaneous with csDMARDs was more effective overall than treatment with csDMARDs alone in improving PROs in patients with active RA.
The results of these analyses demonstrated that patients with RA are now able to attain PRO scores that more closely approach those reported by healthy populations.
Introduction
Rheumatoid arthritis (RA) is a chronic systemic autoimmune disorder characterised by joint tenderness and swelling and the progressive degradation of joint architecture. Due to the pain, stiffness, fatigue and impaired physical function that result from this disease, patients with RA often report decreased health-related quality of life (HRQOL).1–4 Patient-reported outcomes (PROs) are highly valuable measures when determining response to therapy,5–8 as patients may consider measures of HRQOL to be more important than traditional measures of clinical disease activity for assessing effectiveness of treatment.9 Thus, two key goals of treatment in patients with RA are to reduce disease activity and to improve patient HRQOL.
Among the currently available disease-modifying antirheumatic drugs (DMARDs), methotrexate (MTX) is recommended as the first-line treatment for patients with RA.10 In patients who do not achieve adequate or sustained responses to MTX (MTX-IR), the addition of a biologic therapy to MTX is recommended.10 11 While tumour necrosis factor inhibitors (TNFis) are often the first choice of biologic therapy, up to 80% of patients will have inadequate responses to TNFis (TNFi-IR).10 12 13 Switching to a biologic DMARD with a different mechanism of action may improve disease outcomes in TNFi-IR patients.
Tocilizumab (TCZ) is a monoclonal antibody that acts as an interleukin-6 receptor antagonist and is approved for the treatment of patients with moderately to severely active RA. TCZ can be administered intravenously or subcutaneously, with or without concomitant MTX or other conventional synthetic DMARDs (csDMARD).14 15 The efficacy of TCZ administered either intravenously or subcutaneously in improving RA disease activity has been demonstrated in randomised controlled trials (RCTs).16–18 Additionally, post hoc analyses of RCT populations have shown that TCZ administered as monotherapy improves HRQOL in patients with RA.19
The objective of these analyses was to evaluate the impact of TCZ administered intravenously or subcutaneously in combination with csDMARDs on HRQOL in patients with RA using post hoc analyses of three RCT populations (OPTION, BREVACTA and SUMMACTA).16–18
Methods
Study design and patient population
The study design, patient inclusion and exclusion criteria, and primary analyses of each RCT included in this analysis were previously described in detail and are summarised in online supplementary table 1. Briefly, OPTION (NCT00106548) was a phase 3, multicentre RCT that compared the efficacy of TCZ-intravenous versus placebo in MTX-IR patients with moderately to severely active RA.18 Patients received TCZ-intravenous 8 mg/kg, TCZ-intravenous 4 mg/kg or placebo every 4 weeks with MTX 10–25 mg/week. Those who had not achieved ≥20% improvement in both swollen and tender joint counts by week 16 received rescue therapy with TCZ-intravenous 8 mg/kg. For this post hoc analysis, only patients who received TCZ 8 mg/kg or placebo were included; PROs were assessed at week 16 before rescue therapy.
rmdopen-2017-000602supp001.docx (32.9KB, docx)
BREVACTA (NCT01232569) was a phase 3, multicentre RCT that compared the efficacy of TCZ-subcutaneous 162 mg vs placebo.17 Patients had moderately to severely active RA and previous inadequate responses to ≥1 DMARD (DMARD-IR), which may have included TNFis in up to 20% of patients. Study participants received TCZ-subcutaneous 162 mg or placebo every 2 weeks with stable doses of csDMARDs. Patients who had not achieved ≥20% improvement in both swollen and tender joint counts by week 12 received rescue therapy with TCZ-subcutaneous 162 mg weekly. For the purpose of these post hoc analyses, PROs were assessed at week 12 before initiation of rescue therapy.
SUMMACTA (NCT01194414) was a phase 3, multicentre RCT that compared the efficacy of TCZ-subcutaneous versus TCZ-intravenous in DMARD-IR patients (TNFi-IR in up to 20% of patients) with active RA.16 Patients received TCZ-intravenous 8 mg/kg every 4 weeks with placebo subcutaneously weekly or TCZ-subcutaneous 162 mg weekly with placebo intravenously every 4 weeks. Patients could receive concomitant csDMARDs at stable doses during the trial.
Patient-reported outcomes
HRQOL was evaluated at baseline in each study and at 16 weeks in OPTION, 12 weeks in BREVACTA and 24 weeks in SUMMACTA. PROs were assessed as previously described,19 and included patient global assessment of disease activity (PtGA; visual analogue scale 0–100 mm), pain (visual analogue scale 0–100 mm), Health Assessment Questionnaire-Disability Index (HAQ-DI; 0–3), Functional Assessment of Chronic Illness Therapy (FACIT)-Fatigue score (0–52; OPTION and BREVACTA only), Short Form-36 (SF-36) physical component score (PCS) and mental component score (MCS) (0–50), and SF-36 individual domain scores (physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional and mental health; 0–100). Outcomes included mean changes from baseline in PRO scores, the proportion of patients reporting improvements from baseline ≥ minimum clinically important differences (MCID) for each PRO,20 21 and the proportion of patients who reported scores ≥ to age and gender-matched normative values (table 1).20–22 Mean SF-36 domain scores were determined at baseline and 16, 12 or 24 weeks and compared with age and gender-matched normative values for each RCT population using spydergrams.23 To provide a reference for changes in disease activity, mean change from baseline in Clinical Disease Activity Index (CDAI) score was assessed at week 16, 12 or 24 for each trial population.
Table 1.
PRO age and gender-matched normative values in a US non-RA population without comorbid conditions
| OPTION | BREVACTA | SUMMACTA | |
| HAQ-DI, 0–3 | <0.5 | <0.5 | <0.5 |
| FACIT-Fatigue, 0–52 | ≥40 | ≥40 | ≥40 |
| SF-36 PCS (mean, 50; SD, 10) | ≥50 | ≥50 | ≥50 |
| SF-36 MCS (mean, 50; SD, 10) | ≥50 | ≥50 | ≥50 |
| SF-36 domains, 0–100 | |||
| Physical functioning | ≥78.7 | ≥79.4 | ≥79.0 |
| Role-physical | ≥79.1 | ≥80.0 | ≥79.6 |
| Bodily pain | ≥67.3 | ≥68.2 | ≥68.2 |
| General health | ≥68.3 | ≥69.6 | ≥69.4 |
| Vitality | ≥56.7 | ≥58.0 | ≥58.1 |
| Social functioning | ≥81.8 | ≥83.4 | ≥83.4 |
| Role-emotional | ≥85.1 | ≥86.7 | ≥86.5 |
| Mental health | ≥73.1 | ≥74.8 | ≥74.9 |
FACIT, Functional Assessment of Chronic Illness Therapy; HAQ-DI, Health Assessment Questionnaire-Disability Index; MCS, mental component summary; PCS, physical component summary; PRO, patient-reported outcome; RA, rheumatoid arthritis; SF-36, Short Form-36.
Statistical analysis
Analyses were performed in the patient populations used for the primary efficacy analysis in each trial. In OPTION, the primary efficacy hypothesis was to demonstrate superiority of TCZ-intravenous versus placebo in the intention-to-treat population (TCZ-intravenous, n=205; placebo, n=204). In BREVACTA, the primary efficacy hypothesis was to demonstrate superiority of TCZ-subcutaneous versus placebo in the intention-to-treat population (TCZ-subcutaneous, n=437; placebo, n=219). In SUMMACTA, the primary efficacy hypothesis was to demonstrate non-inferiority of TCZ-subcutaneous versus TCZ-intravenous in the per-protocol population (TCZ-subcutaneous, n=558; TCZ-intravenous, n=537). PROs, the proportions of patients reporting improvements ≥ MCID from baseline to week 16, 12 or 24 and the proportions of patients reporting scores ≥ age and gender-matched normative values at week 16, 12 or 24 were compared between TCZ-intravenous and placebo, TCZ-subcutaneous and placebo, or TCZ-subcutaneous and TCZ-intravenous in OPTION, BREVACTA and SUMMACTA, respectively. In OPTION and BREVACTA, p values were reported to demonstrate statistically significant differences between TCZ-intravenous and placebo and between TCZ-subcutaneous and placebo, respectively. In SUMMACTA, p values were not reported; rather, 95% CIs for the treatment difference (TCZ-subcutaneous − TCZ-intravenous) were calculated.
Least squares mean changes from baseline calculated using analysis of covariance were used to compare continuous endpoints. For each PRO and SF-36 domain, the proportions of patients reporting improvements from baseline ≥ MCID at 16, 12 or 24 weeks were analysed using a Cochran-Mantel-Haenszel χ2 test. All analyses were adjusted for site in OPTION and region, body weight category and baseline scores in BREVACTA and SUMMACTA.
Results
Study population and baseline patient characteristics
Details about the trial populations and patient characteristics have previously been described in detail.16–18 Patient demographics and baseline disease characteristics were generally comparable between treatment groups within each RCT (table 2). Overall, baseline PRO scores were comparable between treatment arms within each RCT and showed that patients were substantially impacted by disease activity (table 2). Baseline PRO scores were similar across the three RCTs (table 2).
Table 2.
Demographics, baseline disease characteristics and baseline PRO scores of patients in the OPTION, BREVACTA and SUMMACTA study populations
| Baseline characteristic* | OPTION | BREVACTA | SUMMACTA | |||
| TCZ-intravenous 8 mg/kg every 4 weeks (n=205) |
Placebo every 4 weeks (n=204) |
TCZ-subcutaneous 162 mg every 2 weeks (n=437) |
Placebo every 2 weeks (n=219) |
TCZ-subcutaneous 162 mg weekly (n=558) |
TCZ-intravenous 8 mg/kg every 4 weeks (n=537) |
|
| Age (years) | 50.8 (11.8) | 50.6 (12.1) | 52.1 (11.5) | 52.0 (11.7) | 52.4 (12.3) | 52.5 (12.5) |
| Female, n (%) | 175 (85) | 159 (78) | 375 (86) | 181 (83) | 461 (83) | 444 (83) |
| White, n (%) | 148 (72) | 149 (73) | 321 (74) | 152 (69) | 432 (77) | 403 (75) |
| Disease duration (years) | 7.5 (7.3) | 7.8 (7.2) | 11.1 (8.2) | 11.1 (8.4) | 8.7 (8.2) | 8.7 (7.9) |
| Number of prior csDMARDs/TNFis | 1.5 (1.4) | 1.7 (1.5) | 1.3 (0.7) | 1.4 (0.8) | 1.4 (0.7) | 1.4 (0.7) |
| CDAI | 43.4 (13.5) | 44.0 (12.0) | 41.0 (12.7) | 40.3 (12.4) | 39.3 (13.0) | 41.2 (13.9) |
| PtGA, VAS 0–100 mm | 64.8 (22.2) | 63.6 (21.8) | 63.6 (22.4) | 62.1 (20.8) | 67.3 (21.7) | 67.5 (21.6) |
| Pain, VAS 0–100 mm | 59.9 (22.4) | 57.3 (22.2) | 57.8 (22.8) | 56.8 (22.3) | 60.2 (22.5) | 61.8 (21.9) |
| HAQ-DI, 0–3 | 1.6 (0.6) | 1.5 (0.6) | 1.6 (0.6) | 1.6 (0.6) | 1.6 (0.6) | 1.7 (0.7) |
| FACIT-Fatigue, 0–52 | 27.7 (10.6) | 26.7 (11.1) | 27.0 (10.4) | 27.3 (10.2) | – | – |
| SF-36 PCS (mean, 50; SD, 10) |
32.1 (7.0) | 32.3 (7.0) | 31.7 (7.3) | 32.4 (6.9) | 30.2 (7.2) | 30.2 (7.5) |
| SF-36 MCS (mean, 50; SD, 10) |
40.8 (10.6) | 39.1 (11.0) | 38.6 (11.7) | 39.6 (11.0) | 39.7 (11.6) | 39.0 (12.1) |
| SF-36 domains, 0–100 | ||||||
| Physical functioning | 38.8 (22.6) | 39.8 (24.0) | 35.5 (22.5) | 37.1 (22.2) | 33.4 (21.3) | 33.2 (22.7) |
| Role-physical | 15.9 (29.0) | 14.0 (26.8) | 35.0 (22.4) | 37.2 (20.2) | 33.6 (22.4) | 32.8 (23.3) |
| Bodily pain | 28.9 (16.4) | 29.6 (17.3) | 30.2 (17.3) | 31.9 (16.3) | 27.3 (16.4) | 27.5 (17.6) |
| General health | 38.8 (18.3) | 36.1 (18.1) | 39.7 (18.2) | 41.5 (18.7) | 40.1 (18.6) | 38.7 (18.1) |
| Vitality | 39.1 (19.2) | 37.0 (18.9) | 39.4 (19.4) | 40.5 (19.4) | 36.1 (19.8) | 35.6 (20.0) |
| Social functioning | 53.4 (24.2) | 49.9 (23.8) | 48.2 (24.6) | 51.7 (23.7) | 48.2 (25.1) | 47.1 (25.5) |
| Role-emotional | 33.7 (41.0) | 30.3 (39.5) | 47.6 (27.7) | 49.9 (25.7) | 50.0 (28.1) | 48.1 (30.2) |
| Mental health | 55.8 (19.5) | 53.4 (20.6) | 54.0 (19.9) | 55.1 (19.3) | 56.5 (19.9) | 55.5 (20.0) |
*All values are presented as mean (SD) unless otherwise indicated.
CDAI, Clinical Disease Activity Index; csDMARD, conventional synthetic disease-modifying antirheumatic drug; FACIT, Functional Assessment of Chronic Illness Therapy; HAQ-DI, Health Assessment Questionnaire-Disability Index; MCS, mental component summary; PCS, physical component summary; PRO, patient-reported outcome; PtGA, patient global assessment; SF-36, Short Form-36; TCZ, tocilizumab; TNFi, tumour necrosis factor inhibitor; VAS, visual analogue scale.
Improvement in PROs
In OPTION, patients who received TCZ-intravenous every 4 weeks reported significantly greater improvements from baseline in all PRO scores at 16 weeks compared with placebo (table 3). Similarly, in BREVACTA, patients who received TCZ-subcutaneous every 2 weeks reported significantly greater improvements from baseline in all PRO scores at 12 weeks compared with placebo (table 3). In SUMMACTA, patients in the TCZ-subcutaneous weekly and TCZ-intravenous every 4 weeks groups reported similar improvements from baseline across all PRO scores at 24 weeks (table 3).
Table 3.
LSM changes from baseline in PRO scores at 16 weeks in OPTION, 12 weeks in BREVACTA and 24 weeks in SUMMACTA
| OPTION (week 16)* | BREVACTA (week 12)* | SUMMACTA (week 24)* | |||||||
| LSM change from baseline† | LSM change from baseline† | LSM change from baseline† | |||||||
| TCZ-intravenous every 4 weeks | Placebo every 4 weeks | Difference‡ (95% CI) |
TCZ-subcutaneous every 2 weeks | Placebo every 2 weeks | Difference‡ (95% CI) |
TCZ-subcutaneous weekly | TCZ-intravenous every 4 weeks | Difference (95% CI) |
|
| PtGA, VAS 0–100 mm | −28.4 | −12.0 | −16.4 (−21.6 to −11.3) | −23.4 | −11.7 | −11.6 (−15.4 to − 7.9) | −35.0 | −36.0 | 0.9 (−1.9 to 3.8) |
| Pain, VAS 0–100 mm | −27.1 | −10.0 | −17.1 (−22.4 to −11.8) | −18.5 | −8.1 | −10.5 (−14.2 to −6.7) | −29.2 | −31.1 | 1.9 (−0.9 to 4.7) |
| HAQ-DI, 0–3 | −0.5 | −0.2 | −0.4 (−0.5 to −0.2) | −0.4 | −0.2 | −0.2 (−0.3 to −0.1) | −0.6 | −0.6 | 0 (−0.1 to 0) |
| FACIT-Fatigue, 0–52 | 7.2 | 2.3 | 4.9 (2.8 to 7.0) | 6.0 | 3.2 | 2.8 (1.4 to 4.2) | – | – | – |
| SF-36 PCS (mean, 50; SD, 10) | 8.4 | 2.9 | 5.5 (3.7 to 7.3) | 4.9 | 2.3 | 2.6 (1.4 to 3.7) | 8.7 | 8.9 | −0.2 (−1.1 to 0.8) |
| SF-36 MCS (mean, 50; SD, 10) | 5.7 | 1.9 | 3.8 (1.5 to 6.1) | 5.5 | 2.3 | 3.2 (1.7 to 4.7) | 6.4 | 6.5 | −0.1 (−1.3 to 1.0) |
| SF-36 domains, 0–100 | |||||||||
| Physical functioning | 17.0 | 5.1 | 12.0 (7.3 to 16.7) | 8.9 | 2.8 | 6.0 (2.8 to 9.3) | 18.9 | 19.0 | −0.2 (−2.8 to 2.5) |
| Role-physical | 32.3 | 14.5 | 17.8 (9.9 to 25.8) | 14.9 | 7.7 | 7.2 (3.7 to 10.6) | 20.9 | 21.3 | −0.5 (−3.2 to 2.3) |
| Bodily pain | 26.8 | 10.3 | 16.5 (12.5 to 20.6) | 17.8 | 8.6 | 9.2 (6.0 to 12.4) | 25.5 | 27.5 | −1.9 (−4.4 to 0.5) |
| General health | 12.1 | 4.3 | 7.8 (4.5 to 11.1) | 8.5 | 4.2 | 4.3 (1.8 to 6.9) | 13.0 | 13.3 | −0.3 (−2.3 to 1.7) |
| Vitality | 16.0 | 6.1 | 9.9 (6.3 to 13.5) | 12.0 | 5.3 | 6.8 (4.0 to 9.5) | 16.1 | 14.8 | 1.4 (−0.7 to 3.5) |
| Social functioning | 16.8 | 3.1 | 13.7 (9.3 to 18.2) | 11.0 | 4.8 | 6.2 (2.7 to 9.6) | 20.0 | 20.4 | −0.4 (−2.8 to 2.1) |
| Role-emotional | 29.6 | 11.4 | 18.2 (9.6 to 26.8) | 12.2 | 4.6 | 7.6 (3.9 to 11.3) | 15.7 | 16.9 | −1.1 (−4.1 to 1.9) |
| Mental health | 11.3 | 3.8 | 7.5 (4.1 to 10.9) | 9.9 | 4.6 | 5.4 (2.7 to 8.0) | 10.7 | 10.9 | −0.3 (−2.2 to 1.7) |
| CDAI | −21.6 | −9.7 | −11.9 (−15.0 to –8.8) | −18.8 | −13.0 | −5.8 (−8.1 to –3.5) | −24.8 | −25.4 | 0.5 (−0.8 to 1.9) |
*Analyses were performed using the intention-to-treat population in OPTION (TCZ-intravenous, n=205; placebo, n=204), intention-to-treat population in BREVACTA (TCZ-subcutaneous, n=437; placebo, n=219) and per-protocol population in SUMMACTA (TCZ-subcutaneous, n=558; TCZ-intravenous, n=537). The amount of missing data varied by endpoint and ranged from 5% to 25% in OPTION, 3% to 5% in BREVACTA and 7% to 8% in SUMMACTA. No imputation for missing data was applied.
†Adjusted for site in OPTION and region, body weight category and baseline score in BREVACTA and SUMMACTA.
‡P≤0.001 for the difference in LSM change from baseline between the TCZ-intravenous (OPTION) or TCZ-subcutaneous (BREVACTA) group compared with placebo for all PROs.
CDAI, Clinical Disease Activity Index; FACIT, Functional Assessment of Chronic Illness Therapy; HAQ-DI, Health Assessment Questionnaire-Disability Index; LSM, least squares mean; MCS, mental component summary; PCS, physical component summary; PRO, patient-reported outcome; PtGA, patient global assessment; SF-36, Short Form-36; TCZ, tocilizumab; VAS, visual analogue scale.
Consistent with reported improvement in PROs, TCZ-treated patients in OPTION and BREVACTA experienced significantly greater improvements from baseline in CDAI scores at 16 and 12 weeks, respectively, compared with placebo (table 3). Patients in the TCZ-subcutaneous weekly and TCZ-intravenous every 4 weeks arms of SUMMACTA experienced similar improvements from baseline in CDAI scores at 24 weeks (table 3).
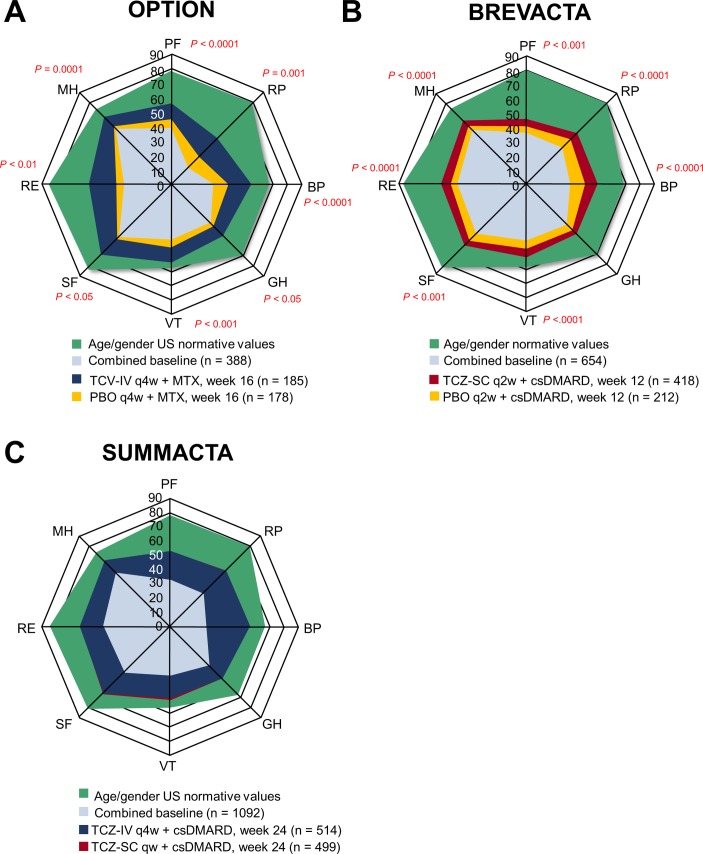
In all three RCT populations, patients who received TCZ-intravenous or TCZ-subcutaneous reported higher mean scores across all SF-36 domains, which more closely approached age and gender-matched normative values, at the study endpoints compared with baseline scores. Patients in OPTION who received TCZ-intravenous every 4 weeks reported significantly higher mean scores across all SF-36 domains at 16 weeks compared with placebo (figure 1A), with greatest improvements from baseline in TCZ-intravenous-treated patients in role-physical, role-emotional and bodily pain (table 3). Similarly, patients in BREVACTA who received TCZ-subcutaneous every 2 weeks reported significantly higher mean scores across all SF-36 domains at week 12 compared with placebo (figure 1B), with greatest improvements in TCZ-subcutaneous-treated patients in bodily pain, role-physical and role-emotional (table 3). Patients in the TCZ-subcutaneous weekly and TCZ-intravenous every 4 weeks groups in SUMMACTA reported similar mean scores across all SF-36 domains at 24 weeks (figure 1C), with greatest improvements in both TCZ-treated groups in bodily pain, role-physical and social functioning (table 3).
Figure 1.
SF-36 domain scores at baseline and at (A) 16 weeks in OPTION, (B) 12 weeks in BREVACTA and (C) 24 weeks in SUMMACTA compared with age and gender-matched normative values. Analyses were performed using the intention-to-treat population in OPTION (TCZ-intravenous, n=205; PBO, n=204), intention-to-treat population in BREVACTA (TCZ-subcutaneous, n=437; PBO, n=219) and per-protocol population in SUMMACTA (TCZ-subcutaneous, n=558; TCZ-intravenous, n=537). BP, bodily pain; csDMARD, conventional synthetic disease-modifying antirheumatic drug; GH, general health; IV, intravenous; MH, mental health; MTX, methotrexate; PBO, placebo; PF, physical functioning; qw, weekly; q2w, every 2 weeks; q4w, every 4 weeks; RE, role-emotional; RP, role-physical; SC, subcutaneous; SF, social functioning; SF-36, Short Form-36; TCZ, tocilizumab; VT, vitality.
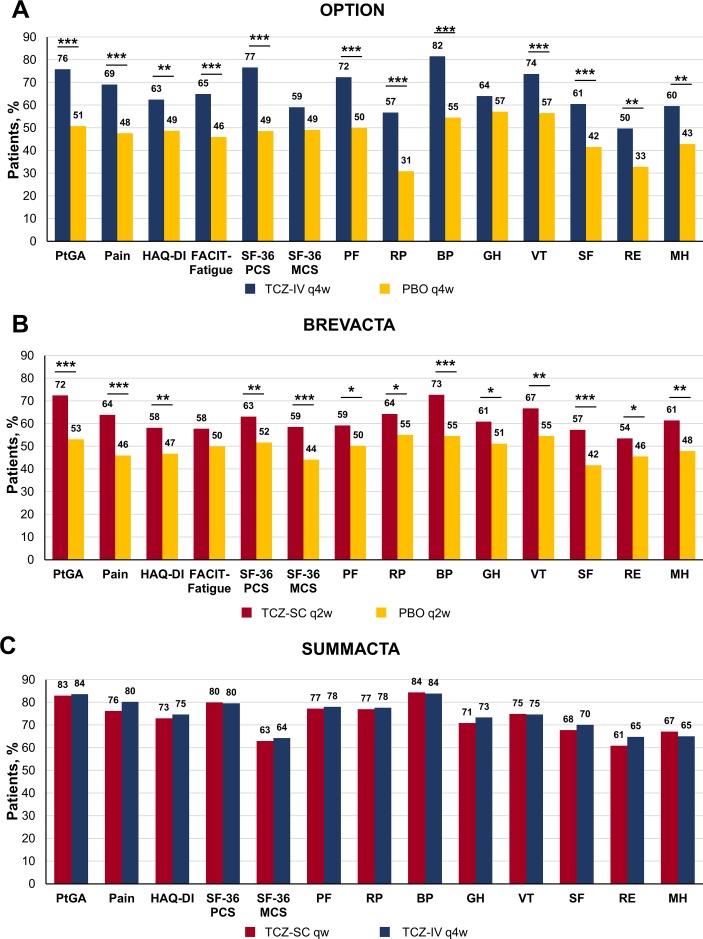
Patients reporting improvement greater than or equal to MCID
In OPTION, 50%–82% of patients who received TCZ-intravenous every 4 weeks reported improvements from baseline ≥ MCID in PRO and SF-36 domain scores at week 16, compared with 31%–57% of those who received placebo (figure 2A). The proportion of patients in the TCZ-intravenous every 4 weeks group that reported improvements ≥ MCID was significantly greater compared with placebo for all PROs (p<0.01; number needed to treat (NNT) 3.6–7.2), except SF-36 MCS and general health scores (supplementary table 2). In BREVACTA, 54%–73% of patients who received TCZ-subcutaneous every 2 weeks reported improvements from baseline ≥ MCID in PRO scores at week 12 compared with 42%–55% of those who received placebo (figure 2B). The proportion of patients in the TCZ-subcutaneous every 2 weeks group who reported improvements ≥ MCID was significantly greater compared with placebo for all PROs (p<0.05; NNT 5.2–12.5), except FACIT-Fatigue scores (supplementary table 2). In SUMMACTA, 61%–84% of patients who received TCZ-subcutaneous weekly reported improvements from baseline ≥ MCID in PROs at 24 weeks compared with 64%–84% of those who received TCZ-intravenous every 4 weeks, with no significant differences between groups (figure 2C).
Figure 2.
Proportion of patients reporting improvements from baseline in patient-reported outcomes (PROs) ≥ the MCID at (A) 16 weeks in OPTION, (B) 12 weeks in BREVACTA and (C) 24 weeks in SUMMACTA. The MCID for PROs were defined as follows: HAQ-DI: ≥0.22; PtGA: ≥10; patient pain: ≥10; FACIT-Fatigue: ≥4; SF-36 PCS/MCS: ≥2.5; and SF-36 domains: ≥5.0. Analyses were performed using the intention-to-treat population in OPTION (TCZ-intravenous, n=205; PBO, n=204), intention-to-treat population in BREVACTA (TCZ-subcutaneous, n=437; PBO, n=219) and per-protocol population in SUMMACTA (TCZ-subcutaneous, n=558; TCZ-intravenous, n=537). *P<0.05; **P<0.01; ***P<0.001. BP, bodily pain; FACIT, Functional Assessment of Chronic Illness Therapy; GH, general health; HAQ-DI, Health Assessment Questionnaire-Disability Index; IV, intravenous; MCID, minimum clinically important difference; MCS, mental component score; MH, mental health; PBO, placebo; PCS, physical component score; PF, physical functioning; PtGA, patient global assessment; qw, weekly; q2w, every 2 weeks; q4w, every 4 weeks; RE, role-emotional; RP, role-physical; SC, subcutaneous; SF, social functioning; SF-36, Short Form-36; TCZ, tocilizumab; VT, vitality.
With respect to SF-36 domains, improvements ≥ MCID were most frequently reported in bodily pain in the TCZ treatment arms of all trials, followed by vitality and physical functioning among TCZ-intravenous-treated patients in OPTION, vitality and role-physical in TCZ-subcutaneous-treated patients in BREVACTA, and physical functioning and role-physical in both TCZ-treated groups in SUMMACTA (figure 2).
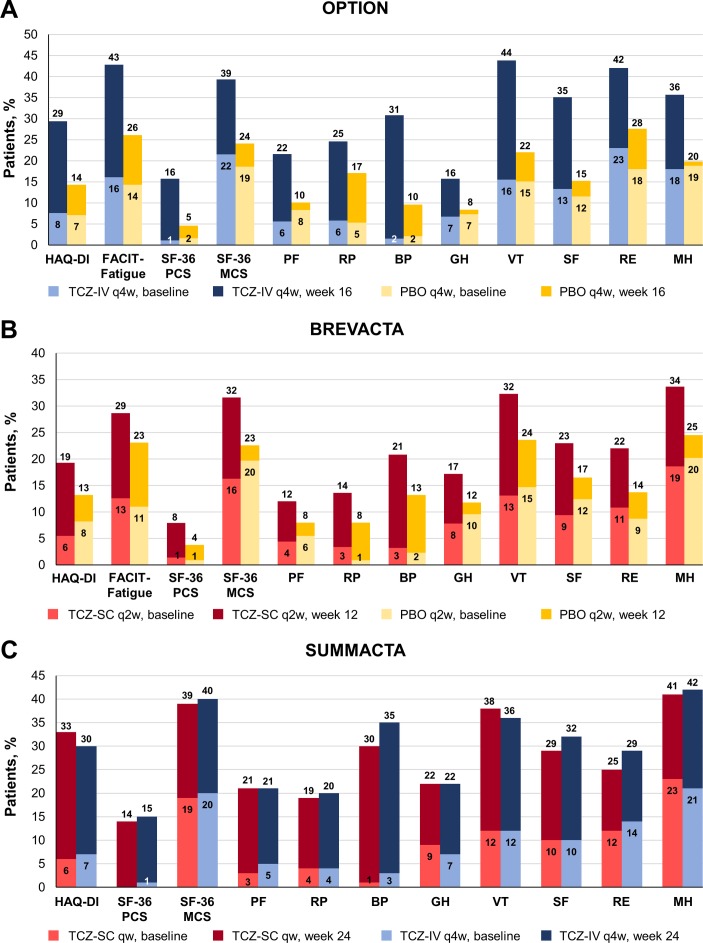
Patients reporting PRO scores greater than or equal to age and gender-matched normative values
The proportions of patients with PRO scores ≥ age and gender-matched normative values at baseline were comparable between treatment arms within each RCT (figure 3). In OPTION, this proportion ranged from 1% and 2% (SF-36 PCS; TCZ-intravenous every 4 weeks and placebo, respectively) to 22% and 19% (SF-36 MCS; TCZ-intravenous every 4 weeks and placebo, respectively), with a similar range across SF-36 domains: 2% (bodily pain; both groups) to 23% (role-emotional; TCZ-intravenous every 4 weeks) and 19% (mental health; placebo). In BREVACTA, this proportion ranged from 1% (SF-36 PCS; both groups) to 16% and 20% (SF-36 MCS; TCZ-subcutaneous every 2 weeks and placebo, respectively), with a similar range across SF-36 domains: 8% and 4% (role-physical; TCZ-subcutaneous every 2 weeks and placebo, respectively) to 19% and 20% (mental health; TCZ-subcutaneous every 2 weeks and placebo, respectively). In SUMMACTA, the proportion of patients with normative scores at baseline ranged from 0% and 1% (SF-36 PCS; TCZ-subcutaneous weekly and TCZ-intravenous every 4 weeks, respectively) to 19% and 20% (SF-36 MCS; TCZ-subcutaneous weekly and TCZ-intravenous every 4 weeks, respectively), with a similar range across SF-36 domains: 1% and 3% (bodily pain; TCZ-subcutaneous weekly and TCZ-intravenous every 4 weeks, respectively) to 23% and 21% (mental health, TCZ-subcutaneous weekly and TCZ-intravenous every 4 weeks, respectively).
Figure 3.
Proportion of patients reporting scores ≥ age and gender-matched normative patient-reported outcome values at (A) 16 weeks in OPTION, (B) 12 weeks in BREVACTA and (C) 24 weeks in SUMMACTA. Analyses were performed using the intention-to-treat population in OPTION (TCZ-intravenous, n=205; PBO, n=204), intention-to-treat population in BREVACTA (TCZ-subcutaneous, n=437; PBO, n=219) and per-protocol population in SUMMACTA (TCZ-subcutaneous, n=558; TCZ-intravenous, n=537). BP, bodily pain; FACIT, Functional Assessment of Chronic Illness Therapy; GH, general health; HAQ-DI, Health Assessment Questionnaire-Disability Index; IV, intravenous; MCS, mental component score; MH, mental health; PBO, placebo; PCS, physical component score; PF, physical functioning; PtGA, patient global assessment; qw, weekly; q2w, every 2 weeks; q4w, every 4 weeks; RE, role-emotional; RP, role-physical; SC, subcutaneous; SF, social functioning; SF-36, Short Form-36; TCZ, tocilizumab; VT, vitality.
The proportions of patients with scores ≥ age and gender-matched normative values at 16, 12 or 24 weeks in OPTION, BREVACTA and SUMMACTA, respectively, increased from baseline in all treatment groups across all PROs and indicated clinically important improvements in TCZ-treated patients (figure 3). In OPTION, 16%–43% of patients treated with TCZ-intravenous every 4 weeks reported scores ≥ normative values across HAQ-DI, FACIT-Fatigue and SF-36 PCS/MCS and 16%–44% across SF-36 domains at week 16 compared with 5%–19% and 8%–28% of placebo-treated patients, respectively. In BREVACTA, the proportion of patients treated with TCZ-subcutaneous every 2 weeks reporting scores ≥ normative values ranged from 8% to 32% for HAQ-DI, FACIT-Fatigue and SF-36 PCS/MCS and from 12% to 34% across SF-36 domains at week 12 compared with 4%–23% and 8%–25% in placebo, respectively. In SUMMACTA, 14%–39% of patients treated with TCZ-subcutaneous weekly and 15%–40% receiving TCZ-intravenous every 4 weeks reported scores ≥ normative values across HAQ-DI and SF-36 PCS/MCS scores at week 24; 19%–44% of patients treated with TCZ-subcutaneous weekly and 20%–42% of patients treated with TCZ-intravenous every 4 weeks reported scores ≥ normative values across SF-36 domains.
With respect to SF-36 domains, the greatest increases from baseline in proportions of patients reporting scores ≥ normative values among TCZ-treated patients were observed in bodily pain, vitality and social functioning in TCZ-intravenous-treated patients in OPTION; vitality, bodily pain and mental health in TCZ-subcutaneous-treated patients in BREVACTA; and bodily pain, vitality and social functioning in both TCZ-treated groups in SUMMACTA (figure 3).
Discussion
In the OPTION, BREVACTA and SUMMACTA trial populations, TCZ administered intravenously or subcutaneously with concomitant csDMARDs was effective in improving PROs in MTX-IR or TNFi-IR patients with RA. Improvements in PRO scores were consistent with CDAI responses. Treatment with either TCZ-intravenous every 4 weeks or TCZ-subcutaneous every 2 weeks in OPTION and BREVACTA, respectively, resulted in significantly greater improvements in all PRO scores at 16 and 12 weeks, respectively, compared with placebo; higher proportions of patients reported improvements from baseline ≥ MCID as well as scores ≥ age and gender-matched normative values, indicative of clinically meaningful changes, than those who received placebo. In SUMMACTA, TCZ-subcutaneous weekly and TCZ-intravenous every 4 weeks resulted in similar improvements across all PRO scores at 24 weeks, with similar proportions of patients reporting clinically meaningful improvements and scores ≥ normative values.
Mean baseline PRO scores for patients in all RCT populations were below normative values, with <25% of patients reporting scores ≥ normative values for any PRO, indicating that patients in all RCT populations were substantially impacted by RA at baseline. Treatment with TCZ-intravenous or TCZ-subcutaneous resulted in clinically meaningful improvements across all PRO scores in all three trial populations. In OPTION, clinically meaningful NNTs (≤10) favouring TCZ-intravenous every 4 weeks versus placebo were observed for all PROs except SF-36 MCS and general health domain scores. In BREVACTA, clinically meaningful NNTs favouring TCZ-subcutaneous every 2 weeks versus placebo were observed for PtGA, pain, HAQ-DI score, and SF-36 PCS, MCS, and four of eight domain scores (bodily pain, vitality, social functioning and mental health). In all three RCTs, mean scores in SF-36 individual domains more closely approached normative values, and higher proportions of patients reported scores ≥ normative values across all PROs compared with baseline. Thus, these data suggest that attainment of PRO scores similar to those reported by healthy populations is an achievable goal for RA treatment.
The results of this study are consistent with those reported in a post hoc analysis of the RADIATE study (NCT00106522) that evaluated changes in PROs in TNFi-IR patients with RA.24 25 In the RADIATE population, patients who received TCZ-intravenous 8 mg/kg every 4 weeks with MTX reported significantly greater improvements in PtGA, pain, HAQ-DI, FACIT-Fatigue, SF-36 PCS and all SF-36 domain scores at 24 weeks compared with placebo.25 In addition, a higher proportion of patients who received TCZ-intravenous 8 mg/kg reported improvements ≥ MCID in PtGA, pain, HAQ-DI, FACIT-Fatigue, and SF-36 PCS and MCS scores at 24 weeks than placebo.25 Patients who received TCZ-intravenous 8 mg/kg also reported mean scores in all SF-36 individual domains that more closely matched age and gender-matched normative values at 24 weeks.25 Taken together, the results of RADIATE and the present analyses indicate that treatment with TCZ can substantially improve HRQOL in both csDMARD-IR and TNFi-IR patients with RA.
These analyses are limited by the evaluation of improvements in PROs up to only 16, 12 and 24 weeks, before rescue of placebo-treated patients was offered. Longer studies are needed to examine PROs in patients with RA receiving longer term therapy with TCZ-intravenous or TCZ-subcutaneous in combination with csDMARDs. Additionally, longitudinal analyses were not performed for these analyses. Due to the active comparator trial design without the need for rescue of non-responders, patients in SUMMACTA were treated with TCZ longer (24 weeks) than those in OPTION (16 weeks) or BREVACTA (12 weeks) at the time of PRO assessment. Longer exposure to TCZ in patients in SUMMACTA may contribute to the apparent differences in the magnitude of improvements and proportions of patients reporting changes ≥ MCID or scores ≥ normative values between patients who received TCZ-intravenous in SUMMACTA versus OPTION or TCZ-subcutaneous in SUMMACTA versus BREVACTA. Trials evaluating PROs are inherently limited by the potential for patient anticipation of improvements due to initiation of new therapy, which may introduce bias, particularly in an active comparator trial such as SUMMACTA. However, across these trials, reported improvements in PROs correlated with significant improvements in CDAI scores.
In these post hoc analyses of three RCT populations, treatment with TCZ-intravenous or TCZ-subcutaneous with concomitant csDMARDs resulted in statistically significant and clinically meaningful, and important, improvement in PROs in MTX-IR or TNFi-IR patients with RA. TCZ-intravenous or TCZ-subcutaneous with concomitant csDMARDs was more effective than csDMARDs alone in improving PROs, whereas treatment with TCZ-intravenous or TCZ-subcutaneous resulted in similar improvements in PROs. The results of these analyses indicate that achievement of PRO scores that more closely approach those reported by healthy populations is now an attainable goal in patients with RA.
Acknowledgments
The authors acknowledge Kathy Lampl for her critical appraisal of the manuscript. Support for third-party writing assistance, furnished by Elizabeth Ohneck, PhD, of Health Interactions, was provided by F Hoffmann-La Roche/Genentech.
Footnotes
Contributors: All authors were involved in the study design and/or collection, analysis and interpretation of data, provided critical revision of the manuscript and approved the final version to be submitted for publication.
Funding: The study was funded by F Hoffmann-La Roche/Genentech.
Competing interests: VS has received consulting fees from AbbVie, Amgen, AstraZeneca, Biogen, Boehringer Ingelheim, Celltrion, Crescendo Bioscience, F Hoffmann-La Roche/Genentech, GSK, Janssen, Eli Lilly, Merck, Novartis, Pfizer, Regeneron, Samsung, Sanofi and UCB. MM, CB, JP and KT are employees of Genentech. RF is an employee and shareholder of F Hoffmann-La Roche. AJK has received consulting fees from Genentech, Novartis, Pfizer, Sanofi-Regeneron and UCB; JSS has received grants from AbbVie, Janssen, Lilly, MSD, Pfizer and Roche and has provided expert advice to and/or had speaking engagements for AbbVie, Amgen, AstraZeneca, Astro, Celgene, Celtrion, GlaxoSmithKline, ILTOO, Janssen, Lilly, MedImmune, MSD, Novartis-Sandoz, Pfizer, Roche, Samsung, Sanofi and UCB. GRB has received grants and honoraria for consulting and lectures from Roche.
Patient consent: Not required.
Ethics approval: The OPTION, BREVACTA and SUMMACTA study protocols were approved by an ethics committee or institutional review board at each participating centre before the start of the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. Austad C, Kvien TK, Olsen IC, et al. Sleep disturbance in patients with rheumatoid arthritis is related to fatigue, disease activity, and other patient-reported outcomes. Scand J Rheumatol 2017;46:95–103. 10.3109/03009742.2016.1168482 [DOI] [PubMed] [Google Scholar]
- 2. Strand V, Khanna D. The impact of rheumatoid arthritis and treatment on patients' lives. Clin Exp Rheumatol 2010;28:S32–40. [PubMed] [Google Scholar]
- 3. van Vilsteren M, Boot CR, Knol DL, et al. Productivity at work and quality of life in patients with rheumatoid arthritis. BMC Musculoskelet Disord 2015;16:107 10.1186/s12891-015-0562-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wan SW, He HG, Mak A, et al. Health-related quality of life and its predictors among patients with rheumatoid arthritis. Appl Nurs Res 2016;30:176–83. 10.1016/j.apnr.2015.07.004 [DOI] [PubMed] [Google Scholar]
- 5. Deshpande PR, Rajan S, Sudeepthi BL, et al. Patient-reported outcomes: a new era in clinical research. Perspect Clin Res 2011;2:137–44. 10.4103/2229-3485.86879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Her M, Kavanaugh A. Patient-reported outcomes in rheumatoid arthritis. Curr Opin Rheumatol 2012;24:327–34. 10.1097/BOR.0b013e3283521c64 [DOI] [PubMed] [Google Scholar]
- 7. Kalyoncu U, Dougados M, Daurès JP, et al. Reporting of patient-reported outcomes in recent trials in rheumatoid arthritis: a systematic literature review. Ann Rheum Dis 2009;68:183–90. 10.1136/ard.2007.084848 [DOI] [PubMed] [Google Scholar]
- 8. Strand V, Singh JA. Newer biological agents in rheumatoid arthritis: impact on health-related quality of life and productivity. Drugs 2010;70:121–5. 10.2165/11531980-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 9. Kirwan JR, Hewlett SE, Heiberg T, et al. Incorporating the patient perspective into outcome assessment in rheumatoid arthritis--progress at OMERACT 7. J Rheumatol 2005;32:2250–6. [PubMed] [Google Scholar]
- 10. Singh JA, Saag KG, Bridges SL, et al. 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Rheumatol 2016;68:1–26. 10.1002/art.39480 [DOI] [PubMed] [Google Scholar]
- 11. Smolen JS, Landewé R, Bijlsma J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis 2017;76:960–77. 10.1136/annrheumdis-2016-210715 [DOI] [PubMed] [Google Scholar]
- 12. Keystone EC, Kavanaugh AF, Sharp JT, et al. Radiographic, clinical, and functional outcomes of treatment with adalimumab (a human anti-tumor necrosis factor monoclonal antibody) in patients with active rheumatoid arthritis receiving concomitant methotrexate therapy: a randomized, placebo-controlled, 52-week trial. Arthritis Rheum 2004;50:1400–11. 10.1002/art.20217 [DOI] [PubMed] [Google Scholar]
- 13. Klareskog L, van der Heijde D, de Jager JP, et al. Therapeutic effect of the combination of etanercept and methotrexate compared with each treatment alone in patients with rheumatoid arthritis: double-blind randomised controlled trial. Lancet 2004;363:675–81. 10.1016/S0140-6736(04)15640-7 [DOI] [PubMed] [Google Scholar]
- 14. Genentech, Inc. Actemra® [package insert]. South San Francisco, CA: Genentech, Inc, 2016. [Google Scholar]
- 15. European Medicines Agency. RoActemra [European public assessment report]. London, UK: European Medicines Agency, 2016. [Google Scholar]
- 16. Burmester GR, Rubbert-Roth A, Cantagrel A, et al. A randomised, double-blind, parallel-group study of the safety and efficacy of subcutaneous tocilizumab versus intravenous tocilizumab in combination with traditional disease-modifying antirheumatic drugs in patients with moderate to severe rheumatoid arthritis (SUMMACTA study). Ann Rheum Dis 2014;73:69–74. 10.1136/annrheumdis-2013-203523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kivitz A, Olech E, Borofsky M, et al. Subcutaneous tocilizumab versus placebo in combination with disease-modifying antirheumatic drugs in patients with rheumatoid arthritis. Arthritis Care Res 2014;66:1653–61. 10.1002/acr.22384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Smolen JS, Beaulieu A, Rubbert-Roth A, et al. Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): a double-blind, placebo-controlled, randomised trial. Lancet 2008;371:987–97. 10.1016/S0140-6736(08)60453-5 [DOI] [PubMed] [Google Scholar]
- 19. Strand V, Michalska M, Birchwood C, et al. Impact of tocilizumab monotherapy on patient-reported outcomes in patients with rheumatoid arthritis from two randomised controlled trials. RMD Open 2017;3:e000496 10.1136/rmdopen-2017-000496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Strand V, Boers M, Idzerda L, et al. It’s good to feel better but it’s better to feel good and even better to feel good as soon as possible for as long as possible. Response criteria and the importance of change at OMERACT 10. J Rheumatol 2011;38:1720–7. 10.3899/jrheum.110392 [DOI] [PubMed] [Google Scholar]
- 21. Webster K, Cella D, Yost K. The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health Qual Life Outcomes 2003;1:79 10.1186/1477-7525-1-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Krishnan E, Tugwell P, Fries JF. Percentile benchmarks in patients with rheumatoid arthritis: Health Assessment Questionnaire as a quality indicator (QI). Arthritis Res Ther 2004;6:R505–13. 10.1186/ar1220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Strand V, Crawford B, Singh J, et al. Use of "spydergrams" to present and interpret SF-36 health-related quality of life data across rheumatic diseases. Ann Rheum Dis 2009;68:1800–4. 10.1136/ard.2009.115550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Emery P, Keystone E, Tony HP, et al. IL-6 receptor inhibition with tocilizumab improves treatment outcomes in patients with rheumatoid arthritis refractory to anti-tumour necrosis factor biologicals: results from a 24-week multicentre randomised placebo-controlled trial. Ann Rheum Dis 2008;67:1516–23. 10.1136/ard.2008.092932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Strand V, Burmester GR, Ogale S, et al. Improvements in health-related quality of life after treatment with tocilizumab in patients with rheumatoid arthritis refractory to tumour necrosis factor inhibitors: results from the 24-week randomized controlled RADIATE study. Rheumatology 2012;51:1860–9. 10.1093/rheumatology/kes131 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2017-000602supp001.docx (32.9KB, docx)