Abstract
Objectives
The individual burden of caring for one’s relatives not only depends on care characteristics but is also related to contextual factors. The objective of this study is to determine whether regional formal long-term care provision is linked to the well-being of spousal caregivers introducing the concept of “control” as central pathway to explain this link.
Method
We applied multilevel analysis using data from the Survey of Health, Ageing and Retirement in Europe (SHARE) from over 29,000 Europeans and 1,800 spousal caregivers located in 138 regions in 11 countries to analyze the effects of regional contexts on caregiver well-being. The provision of formal care in a region was measured by the number of long-term care beds in nursing and residential homes among the older population.
Results
We found that spousal caregivers’ well-being, measured in terms of life satisfaction, loneliness, and depression, was positively linked to the regional availability of formal care, which is partly due to higher perceived control in regions with more formal care provision.
Discussion
Our results suggest that formal care supply is essential not only for care recipients but also for caregivers: perceived alternatives to the private care arrangement go along with greater well-being of informal caregivers.
Keywords: Depression, Loneliness, Multilevel models, Personal control, Satisfaction with life
Aging populations are an unprecedented challenge for Western societies, leading to a rise in the number of older people in need of long-term care (LTC) and expected gaps in LTC provision (Agree & Glaser, 2009). In Europe, the majority of care is provided by families (Genet, Boerma, Kroneman, Hutchinson, & Saltman, 2013) and this can be a burdensome experience (Pinquart & Sörensen, 2003). The potential for family care is expected to decrease in the future due to lower fertility rates, higher mobility of younger generations, and higher female labor force participation. At the same time, LTC systems are undergoing reforms to counteract the rising costs of formal care (Deusdad, Pace, & Anttonen, 2016; Ranci & Pavolini, 2013). Governments argue about adequate strategies for organizing formal care and how to support family carers (Colombo, Llena-Nozal, Mercier, & Tjadens, 2011). It is crucial to understand how formal care arrangements should be designed to counteract the expected drop in informal care. With its immense variation in LTC options, Europe is the perfect setting to study the connections between LTC availability and caregivers’ well-being.
The caregiver stress model (Pearlin, Mullan, Semple, & Skaff, 1990) explains how formal care options affect the emergence of informal caregivers’ stress. According to the model, formal care options are part of the care context which influences all the dimensions of the stress process: First, it affects primary stressors that are directly related to the care situation—such as the hours of care provided. It also affects secondary stressors that stem from the challenges due to fulfilling several roles beyond being a caregiver, for example that of an employee, a partner, or a parent. That way, formal care options help reducing intrapsychic strain which ultimately leads to stress.
In this article, we will concentrate on the availability of support by formal LTC providers as a macro contextual factor. We will elaborate how exactly the care context in terms of formal care may affect well-being of caregivers. Therefore, we distinguish between a behavioral and a cognitive-emotional pathway: First, the availability of LTC services may lead to an uptake of the latter so the care recipient receives additional help from a professional caregiver. This is likely to affect the care-related primary stressors and stressors that stem from role strain (Pearlin et al., 1990). We call this the “behavioral pathway” as the formal LTC availability is supposed to affect the uptake and intensity of family care via the uptake of (additional) formal care.
Second, formal LTC availability might not only affect informal caregiver behavior but also the way caregivers think and feel about the care situation via the “cognitive-emotional pathway”. When caregivers are able to choose between providing care themselves and/or (paying for) professional care, they gain control and can thus cope better with the care situation. In general, control is defined as “the extent to which a person feels capable of producing desired and preventing undesired events” (Patrick, Skinner, & Connell, 1993, p. 782). Psychological theory states that if a person is convinced that an (adverse) event occurred due to his/her own behavior, s/he will experience less stress than someone who is convinced that the occurrence of the event was out of his/her own control (Rotter, 1966). Within the caregiver stress model (Pearlin et. al, 1990) role captivity—or how strongly someone feels obliged to fulfill the caregiver role—constitutes an example of a secondary stressor.
For both mechanisms, it is crucial that LTC offers are actually known and available. Otherwise, family caregivers can neither utilize them (behavioral pathway) nor experience control over the care situation (cognitive-emotional pathway). However, the availability of LTC services differs greatly due to regional characteristics in a country (Genet et al., 2011). For example, in poorer regions, financial resources may be spent on public core tasks other than LTC services. In urban regions with higher population densities, the allocation of LTC services is more cost-efficient than in rural regions where for example, home care providers must travel longer distances from one client to another (Coburn, 2002). Therefore, the regional availability of LTC services may be a decisive factor in individual attitudes toward and decisions about formal LTC uptake.
Our study adds to existing research by studying how regional formal care availability affects spousal caregivers’ well-being within several European countries. In addition, we use three different dimensions—life satisfaction, loneliness and depression—to obtain a comprehensive picture of caregivers’ well-being within different regional contexts. Moreover, we introduce the concept of “control” as an important mediator of the link between formal care and spousal caregiver well-being. We will first describe the relevant empirical background for our hypotheses before we introduce our analytical approach, data and methods. We then present our multilevel results and discuss our findings, as well as the limitations of this study, in the concluding section.
Empirical Background and Hypotheses
Various studies indicate that informal caregivers have lower well-being than noncaregivers in terms of physical and mental health (Pinquart & Sörensen, 2003, 2007; Schulz, Visintainer, & Williamson, 1990), quality of life (George & Gwyther, 1986), and loneliness (Beeson, 2003).
Several empirical studies linked the context in terms of formal LTC options to caregivers’ well-being. At the country level, there is evidence that the provision of LTC services is associated with caregivers’ quality of life. Verbakel (2014) compared 18 European countries and showed that the difference in well-being between caregivers and noncaregivers was lower in countries with more formal LTC options. She argued that professional support in difficult situations and the possibility of completely turning over the care duty to professional caregivers may relieve the individual burden. In line with that, Wagner and Brandt (2015) showed that caregiver loneliness was linked to the availability of LTC services comparing 15 European countries. Dujardin and colleagues (2011) found that self-rated health was better among caregivers in Great Britain compared to Belgium, which was in part explained by better targeted LTC services for intensive home care in Great Britain than in Belgium. Ruppanner and Bostean (2014) found differences in well-being between caregivers and noncaregivers in 22 European countries related to the percentage of gross domestic product (GDP) spending on old-age and family related issues. These studies showed the connection between formal LTC options and well-being on the country level, but did not explicitly analyze possible pathways that may explain the results.
Regarding the behavioral pathway, research showed that when formal long-term care options were available, care tasks differed in character and intensity because informal caregivers took over the less intense and spontaneous support tasks (voluntarily) and formal caregivers fulfilled the more demanding and regular duties (Brandt, Haberkern, & Szydlik, 2009). Verbakel, Metzelthin, and Kempen (2016) found that instrumental support from professional home care services was connected to caregivers’ well-being by reducing the hours spent providing care. Furthermore, research found that formal home care does not substitute for informal care but that the relationship is often complementary (Bolin, Lindgren, & Lundborg, 2008; Bonsang, 2009; Chappell & Blandford, 1991) and that the welfare state context affects the amount of informal care provided (Suanet, Broese van Groenou, & van Tilburg, 2012).
Concerning the cognitive-emotional pathway, experimental research showed that experiencing a sense of control had a positive effect on health and well-being, especially in old age (Rodin, 1986). Schulz and Brenner (1977), for example, found that relocation to a nursing home was experienced as less stressful when the older people had control over the move. So far, few studies have explicitly focused on the role of control in caregivers’ well-being: Schulz et al. (2012) showed that freedom in the decision whether to take over care was linked to higher caregiver well-being. A second study showed that perceived control over the care situation was directly related to higher life satisfaction and less depression and indirectly related to lower stress of caregivers (Wallhagen, 1992).
All in all, there is a limited body of research on contextual effects on caregivers’ well-being on the country level and, to the best of our knowledge, no analyses on the regional level. Studies tend to focus on the behavioral pathway whereas there is little research analyzing the cognitive-emotional pathway (perceived control) in the care context. We will thus focus on the cognitive-emotional pathway by analyzing the concept of “control” as an important mediator of the links between contexts and caregiver well-being. We expect that the well-being of spousal caregivers is higher in regions with many formal care services than in regions with low formal care provision, partly due to higher perceived control. We will analyze whether the connection between LTC context and well-being is affected by caregivers’ perceived control, and whether the extent of control that caregivers perceive is linked to the LTC availability in a region.
Method
Data Sources and Sample
We analyze data from the Survey of Health, Ageing and Retirement in Europe (SHARE), a panel study that started in 2004 with representative samples of individuals aged 50 and older across Europe and Israel (Börsch-Supan et al., 2013; Börsch-Supan, 2015). The respondents were resurveyed biannually by interviewers who visited them at home. We analyzed information from over 29,000 respondents from 138 European regions that were collected in 2013 during the fifth wave. Time-invariant information was partly given only once in the baseline interview and thus forwarded. We concentrate on spousal caregivers (n = 1,806) who make up the majority of cohabiting informal caregivers (Stuifenbergen, van Delden, & Dykstra, 2008) and are most likely to experience negative care outcomes due to the care setting (Kaschowitz & Brandt, 2016; Tennstedt, Crawford, & McKinlay, 1993). Typically, partners live under the same roof, provide many hours of care, are relatively old, and very important network members (Broese van Groenou, de Boer, & Iedema, 2013; Pinquart & Sörensen, 2011).
For our analyses, these micro data were combined with macro data on the regional level using the NUTS (Nomenclature of Territorial Units for Statistics) classification. The NUTS-2 level comprises basic regions with 800,000 to 3,000,000 inhabitants. Regional macro indicators were retrieved from EUROSTAT (2016). Indicators from the year 2012, one year prior to the collection of the SHARE data, were used. Additional regional data were collected from national statistical offices in Germany (Federal Statistical Office Germany, 2016), Switzerland (Federal Statistical Office Switzerland, 2016), and Denmark (Statistics Denmark, 2016). For Germany, only data from 2011 were available.
We restricted our analyses to respondents for whom data linkage with regional information on the NUTS-2 level was possible. Israel does not use the NUTS classification, and the Netherlands, Slovenia, and Sweden did not provide data that could be used as an indicator for LTC availability and therefore were eliminated from the analyses. Finally, data from eleven countries (Austria, Belgium, the Czech Republic, Denmark, Estonia, France, Germany, Italy, Luxembourg, Spain, and Switzerland) were available. Another 5% of the respondents were excluded because of item nonresponse on any of the variables used in the analyses. The net sample comprised 29,458 individuals from 138 European regions in eleven countries spanning Europe from North to South and West to East.
Measures at the Individual Level
As outcome variables, three different measures of subjective well-being were used: Life satisfaction, loneliness, and depression. Well-being is a broad concept that comprises emotional aspects as well as evaluations of one’s satisfaction with life in general and with domains such as family, health, and work (Diener, Suh, Lucas, & Smith, 1999). Life satisfaction is often used interchangeably with subjective well-being and was taken as a general measure of well-being, assessed by a single item asking how satisfied respondents were with their lives. Loneliness is defined as “the unpleasant feeling of lacking certain relationships or missing a certain level of quality in one’s contacts with other people” (de Jong Gierveld & Havens, 2004) and covers social aspects of caregiver well-being. Loneliness was measured by the revised three-item version of the UCLA loneliness scale (Russell, Peplau, & Cutrona, 1980). Depression captures mental health and emotional aspects of well-being and was assessed using the EURO-D 16-item scale, which was designed to measure depressive symptoms among the older European population (Prince et al., 1999).
The main explanatory variable was partner care. It was measured by one item asking “Is there someone living in this household whom you have helped regularly during the last twelve months with personal care, such as washing, getting out of bed, or dressing?” If the respondent answered in the affirmative, a follow-up question was asked about the relationship between the caregiver and the cared-for person. Partners and spouses were coded as one; all other caregivers (such as children or siblings) were set to missing, which applied to one third of all caregivers. Since SHARE does not allow measuring care intensity—a prerequisite for analyzing the behavioral pathway—we will focus on the cognitive-emotional pathway in our analyses. To investigate whether sense of control might be a mediator in the relation of LTC availability and well-being of the spousal caregiver, we used the three-item subscale “control” from the broader CASP quality of life scale (von dem Knesebeck, Hyde, Higgs, Kupfer, & Siegrist, 2005) and applies to general control at older ages, not to the care situation only. The exact wording of all the measures can be found in the supplementary materials section.
Following previous research, we included gender, age, years of education, ability to make ends meet, being employed or not, number of children, household size, physical health, religiosity, having access to public services, and living in a rural or urban area (for details, see Table 1) as controls.
Table 1.
Sample Characteristics of Spousal Caregivers and Noncaregivers in 138 European Regions (n = 29,458)
| Spousal caregivers (n = 1,807) | Noncaregivers (n = 27,651) | |||
|---|---|---|---|---|
| Variable | Definition (range) | Mean (SD) | Mean (SD) | p value |
| Life satisfaction | Overall satisfaction with life (0–10) | 7.05 (2.0) | 7.76 (1.71) | .00 |
| Loneliness | Three-item UCLA loneliness scale (3–9) | 3.95 (1.4) | 3.58 (1.11) | .00 |
| Depression | EURO-D scale of depressive symptoms (0–12) | 3.40 (2.5) | 2.18 (2.12) | .00 |
| Control | Subscale Control from CASP quality of life scale (3–12) | 8.17 (2.5) | 9.10 (2.22) | .00 |
| Female | 1 = female; 0 = otherwise | 0.56 (0.5) | 0.50 (0.50) | .00 |
| Age | Respondent’s age in years (30–95) | 69.50 (9.9) | 64.40 (9.40) | .00 |
| Education | Years of education (0–25) | 10.30 (4.3) | 11.17 (4.50) | .00 |
| Making ends meet | 1 = making ends meet fairly easily or easily; 0 = making ends meet with some or great difficulty | 0.58 (0.5) | 0.71 (0.46) | .00 |
| Working | 1 = paid work (employed or self-employed); 0 = retired, unemployed, permanently sick, or a homemaker | 0.15 (0.4) | 0.31 (0.46) | .00 |
| Children | Number of children (0–13) | 2.30 (1.4) | 2.20 (1.20) | .03 |
| Household size | Number of household members (2–11) | 2.27 (0.7) | 2.44 (0.84) | .00 |
| Physical health | Number of limitations on instrumental activities of daily living (0–7) | 0.55 (1.2) | 0.22 (0.80) | .00 |
| Religiosity | 1 = praying once a week or more often; 0 = praying less than once a week | 0.43 (0.5) | 0.38 (0.49) | .00 |
| Public services | Access to bank, grocery shop, doctor, and pharmacy (4–16) | 11.79 (3.4) | 12.96 (2.78) | .00 |
| Rural | 1 = living in a small town or village; 0 = living in a city, the suburbs of a city or a large town | 0.60 (0.5) | 0.63 (0.48) | .04 |
Note: SE = Standard error. Source: SHARE Wave 5 release 5.0.0.
Measures at the Regional Level
In our study, formal care provision on the regional level was assessed by the number of institutionalized LTC beds in nursing homes or residential care facilities per 100 people aged 65 or older by NUTS-2 region in 2012—or, more briefly, LTC beds. This was taken as a proxy for formal LTC provision in general, as regions with many LTC beds usually also have a greater variety of LTC facilities, such as day care centers or formal home care. As a control variable on the regional level, we included the economic wealth of a region which was measured as GDP in Euro per capita at current market prices in 2012 per region.
Analytic Approach
We applied a multilevel design with individuals on the first level who were clustered in NUTS-2 regions (Level 2), which were clustered in countries (Level 3). We used a random-intercept model with individual- and regional-level variables, including cross-level interactions. All the metric variables were centered. In the main analysis, we used the three well-being measures as outcome variables. Life satisfaction was taken as an overall measure of well-being, and loneliness and depression were used to capture the social and mental aspects of caregivers’ well-being. In an additional analysis focusing on the cognitive-emotional pathway, we used control as outcome variable.
In addition to the regional context being the relevant area for LTC decisions within the local family, there is a strong methodological argument for using the regional variation within Europe: Multilevel analysis with country data may lead to biased results, as the country level typically comprises a small number of observations compared to the number of explanatory variables (Bryan & Jenkins, 2015)—we fall well above the prominent threshold of 30 observations per level to estimate contextual effects (Maas & Hox, 2004).
Results
Descriptive Results
Table 1 provides an overview of the sample and differences between spousal caregivers and noncaregivers regarding our outcome variables life satisfaction, loneliness, and depression, as well as the sociodemographic characteristics included in the multivariate models.
Six percent of the sample cared for their spouse or partner. In line with previous research, spousal caregivers reported lower life satisfaction and higher scores for loneliness and depression than noncaregivers. Moreover, we found that spousal caregivers experienced less control over their lives than noncaregivers. As in other studies, we found more women among the spousal caregivers. Spousal caregivers were older than noncaregivers, less educated, and less often able to “make ends meet”. Furthermore, they were less likely to be working and had more physical limitations. Spousal caregivers were likely to have more children, lived in smaller households, and were more religious. They more often lived in rural areas and had less access to public services (all variables p < .05 in t test). Taken together, caregivers were in worse positions than their counterparts concerning many characteristics that may affect well-being in addition to caring and LTC context.
The regional variation in formal LTC services and GDP is shown in Table 2. The number of LTC beds for older people was higher in Northern, Western, and Central European countries, whereas it was lower in Eastern and Southern European countries. In addition to marked differences among countries, we see strong differences in the numbers of LTC beds across regions (with the exception of Estonia and Luxembourg, where the NUTS-2 level comprises the entire country). In Italy, one region provided almost no formal care services (0.3 beds for 100 older inhabitants), whereas in another Italian region this number went up to 4.6 beds for 100 inhabitants. The same was true for GDP, which differed among countries but also varied considerably within them—in almost all the countries, the richest region had a GDP at least twice as high as that of the poorest (correlation between regional GDP and LTC beds r = .3, n = 138).
Table 2.
Descriptive Overview of Regional Variations in Formal Long-term Care Supply and Gross Domestic Product Among 11 Countries
| LTC beds per 100 persons aged 65 or older in 2012 | GDP in Euro per capita at current market prices in 2012 | ||||
|---|---|---|---|---|---|
| Country | Number of NUTS-2 regions | Country mean | Range between NUTS-2 regions | Country mean | Range between NUTS-2 regions |
| Austria | 9 | 4.4 | 2.8–6.0 | 36,400 | 25,582–47,623 |
| Belgium | 11 | 6.9 | 4.5–9.9 | 34,000 | 22,755–60,707 |
| Czech Republic | 8 | 4.2 | 2.2–5.9 | 14,600 | 11,675–32,021 |
| Denmark | 5 | 4.7 | 3.7–5.0 | 43,900 | 30,752–56,036 |
| Estonia | 1 | 3.9 | 3.9 | 13,000 | 13,000 |
| France | 21 | 5.6 | 4.2–7.7 | 31,100 | 23,722–52,294 |
| Germany | 38 | 5.2 | 4.0–6.5 | 32,600 | 22,978–54,071 |
| Italy | 19 | 1.8 | 0.3–4.6 | 25,700 | 16,038–39,975 |
| Luxembourg | 1 | 5.7 | 5.7 | 80,700 | 80,700 |
| Spain | 18 | 4.4 | 1.9–7.5 | 22,300 | 15,409–30,916 |
| Switzerland | 7 | 6.9 | 5.3–8.0 | 61,900 | 56,989–80,194 |
Note: GDP = Gross domestic product; LTC = Long-term care; NUTS = Nomenclature of territorial units for statistics. Sources: EUROSTAT, Federal Statistical Office Germany, Federal Statistical Office Switzerland, Statistics Denmark.
Multilevel Results
To determine whether the availability of LTC services was positively related to the well-being of informal caregivers and whether feelings of “control” mediate this relation, we calculated nested models for each of the well-being variables life satisfaction, loneliness, and depression. The results for the well-being measure life satisfaction are presented in Table 3.
Table 3.
Caregivers’ Life Satisfaction and Individual and Regional Influences
| Outcome variable | Life satisfaction | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| M1a | M1b | M1c | M1d | M1e | ||||||
| Estimate | (SE) | Estimate | (SE) | Estimate | (SE) | Estimate | (SE) | Estimate | (SE) | |
| Partner care | –0.38*** | (0.038) | –0.38*** | (0.038) | –0.38*** | (0.038) | –0.28*** | (0.036) | ||
| LTC beds | –0.03 | (0.021) | –0.03 | (0.021) | –0.04* | (0.019) | ||||
| Partner care * LTC beds | 0.07** | (0.022) | 0.04* | (0.020) | ||||||
| Sense of control | 0.24*** | (0.004) | ||||||||
| Regional GDP | 0.06 | (0.029) | 0.06 | (0.029) | 0.05* | (0.026) | ||||
| Control variablesa | (+) | (+) | (+) | (+) | ||||||
| ICC country | 0.105 | (0.044) | 0.072 | (0.033) | 0.056 | (0.028) | 0.056 | (0.030) | 0.052 | (0.026) |
| ICC country in region | 0.125 | (0.043) | 0.090 | (0.032) | 0.074 | (0.030) | 0.074 | (0.030) | 0.067 | (0.026) |
| AIC | 112,142 | 108,996 | 108,995 | 108,987 | 105,991 | |||||
Note: Observations: 29,458 respondents, 138 regions; (+) = variables included but coefficients not shown; AIC = Aikaike Information Criterion; ICC = Intraclass Correlation; GDP = Gross domestic product; LTC = Long-term care.
aControl variables: female, age, education, making ends meet, working, children, household size, physical health, religiosity, access to public services, rural.*p < .05; **p < .01; ***p < .001. Sources: SHARE Wave 5 release 5.0.0, EUROSTAT, Federal Statistical Office Germany, Federal Statistical Office Switzerland, Statistics Denmark.
The empty Model 1a shows how much of the variation in life satisfaction can be attributed to the different levels of analysis by examining the intraclass correlation (ICC). The variance in life satisfaction (M1a) that could be attributed to the country level was eleven percent. The “ICC region in country” is the Level 2 intraclass correlation at the region-within-country level, and the unexplained variance in life satisfaction in the same region and country was 13%. The decrease of the ICC in the following models compared to in the intercept-only model indicates the extent to which the variables included in the analysis reduced the unexplained variance at the country and regional levels.
Model 1b is a random intercept model that includes partner care as the explanatory variable and the individual control variables. The results replicate the well-known finding that spousal caregivers have reduced well-being. Life satisfaction (M1b) was significantly lower (minus 0.38 points on the life satisfaction score) than for people who did not provide informal care—independent of the relevant sociodemographic characteristics.
Model 1c adds the contextual variable “LTC beds” as a regional measure of LTC availability and regional wealth as a control variable. As expected, LTC beds as such were not related to peoples’ life satisfaction. In the following Model 1d, we added the interaction term of partner care and LTC beds. We found a significant interaction effect of partner care and number of LTC beds, meaning that the relation between formal care services and life satisfaction is more positive for spousal caregivers than for noncaregivers. Spousal caregivers were more satisfied with life when LTC services were available—compared to noncaregivers. Among spousal caregivers, each additional nursing home bed per 100 people aged 65 years and over (with LTC beds ranging from 0.3 to 9.9 in our sample) diminishes the negative effect of partner care by roughly 10%.
In the last Model 1e, we added perceived control to test whether it influences caregiver well-being and whether the interaction between LTC and caregiver well-being was diminished and thus possibly linked to a sense of control. First, individual control was positively connected to life satisfaction and the effect of partner care was lower (−0.28 in M1e) compared to the former model (−0.38 in M1d) indicating caregiver well-being was influenced by perceived control. Second, GDP was positively and LTC beds were negatively related to life satisfaction of noncaregivers. Third, the interaction of partner care and LTC beds remained positive and significant, but diminished and had higher error probability (0.07*** vs 0.04*). The relation between formal care services and life satisfaction is still more positive for spousal caregivers than for noncaregivers when controlling for perceived control, but the latter seems to be an important channel for the influence of LTC on caregiver well-being connection.
Subsequent models were calculated for the outcome measures loneliness and depression.
M2b in Table 4 shows that spousal caregivers felt lonelier, with loneliness scores on average 0.20 higher than for noncaregivers. When analyzing depression as a measure of mental health (see M3b in Table 5), carers reported on average 0.75 more depressive symptoms than noncaregivers.
Table 4.
Caregivers’ Loneliness and Individual and Regional Influences
| Outcome variable | Loneliness | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| M2a | M2b | M2c | M2d | M2e | ||||||
| Estimate | (SE) | Estimate | (SE) | Estimate | (SE) | Estimate | (SE) | Estimate | (SE) | |
| Partner care | 0.20*** | (0.026) | 0.20*** | (0.026) | 0.21*** | (0.027) | 0.12*** | (0.025) | ||
| LTC beds | –0.01 | (0.011) | –0.01 | (0.011) | –0.01 | (0.008) | ||||
| Partner care × LTC beds | –0.03* | (0.015) | –0.01 | (0.014) | ||||||
| Sense of control | –0.19*** | (0.003) | ||||||||
| Regional GDP | –0.02 | (0.014) | –0.02 | (0.015) | –0.02 | (0.011) | ||||
| Control variablesa | (+) | (+) | (+) | (+) | ||||||
| ICC country | 0.033 | (0.018) | 0.025 | (0.011) | 0.023 | (0.010) | 0.023 | (0.011) | 0.014 | (0.007) |
| ICC country in region | 0.046 | (0.015) | 0.033 | (0.011) | 0.031 | (0.011) | 0.031 | (0.011) | 0.017 | (0.007) |
| AIC | 89,686 | 87,747 | 87,748 | 87,745 | 83,768 | |||||
Note: Observations: 29,458 respondents, 138 regions; (+) = variables included but coefficients not shown; AIC = Aikaike Information Criterion; ICC = Intraclass Correlation; GDP = Gross domestic product; LTC = Long-term care.
aControl variables: female, age, education, making ends meet, working, children, household size, physical health, religiosity, access to public services, rural.*p < .05; **p < .01; ***p < .001. Sources: SHARE Wave 5 release 5.0.0, EUROSTAT, Federal Statistical Office Germany, Federal Statistical Office Switzerland, Statistics Denmark.
Table 5.
Caregivers’ Depression and Individual and Regional Influences
| Outcome variable | Depression | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| M3a | M3b | M3c | M3d | M3e | ||||||
| Estimate | (SE) | Estimate | (SE) | Estimate | (SE) | Estimate | (SE) | Estimate | (SE) | |
| Partner care | 0.75*** | (0.048) | 0.75*** | (0.048) | 0.76*** | (0.048) | 0.60*** | (0.045) | ||
| LTC beds | 0.04 | (0.027) | 0.05 | (0.027) | 0.05* | (0.027) | ||||
| Partner care * LTC beds | –0.08** | (0.027) | –0.04 | (0.025) | ||||||
| Sense of control | –0.34*** | (0.005) | ||||||||
| Regional GDP | –0.07* | (0.034) | –0.07** | (0.034) | –0.05 | (0.034) | ||||
| Control variablesa | (+) | (+) | (+) | (+) | ||||||
| ICC country | 0.025 | (0.013) | 0.018 | (0.009) | 0.015 | (0.008) | 0.016 | (0.008) | 0.014 | (0.008) |
| ICC country in region | 0.060 | (0.013) | 0.043 | (0.010) | 0.040 | (0.009) | 0.049 | (0.009) | 0.046 | (0.009) |
| AIC | 127,939 | 122,850 | 122,848 | 122,842 | 118,876 | |||||
Note: Observations: 29,458 respondents, 138 regions; (+) = variables included but coefficients not shown; AIC = Aikaike Information Criterion; ICC = Intraclass Correlation; GDP = Gross domestic product; LTC = Long-term care.
aControl variables: female, age, education, making ends meet, working, children, household size, physical health, religiosity, access to public services, rural. *p < .05; **p < .01; ***p < .001. Sources: SHARE Wave 5 release 5.0.0, EUROSTAT, Federal Statistical Office Germany, Federal Statistical Office Switzerland, Statistics Denmark.
As expected, LTC beds were neither related to loneliness nor to depression among the general population (see M2c and M3c). For both loneliness and depression a significant interaction effect between LTC beds and partner caregiving was found, meaning that the relation between loneliness or depression and formal LTC services was significantly more negative for spousal caregivers than for noncaregivers. Thus, spousal caregivers benefit from the regional availability of LTC services—they feel less depressed and less lonely—compared to noncaregivers (see M2d and M3d). This interaction effect was no longer significant after adding perceived control to the Models 2e and 3e, respectively. Thus, for all well-being measures, there was indication that control is an important mechanism by which the availability of LTC services and caregivers’ well-being are connected.
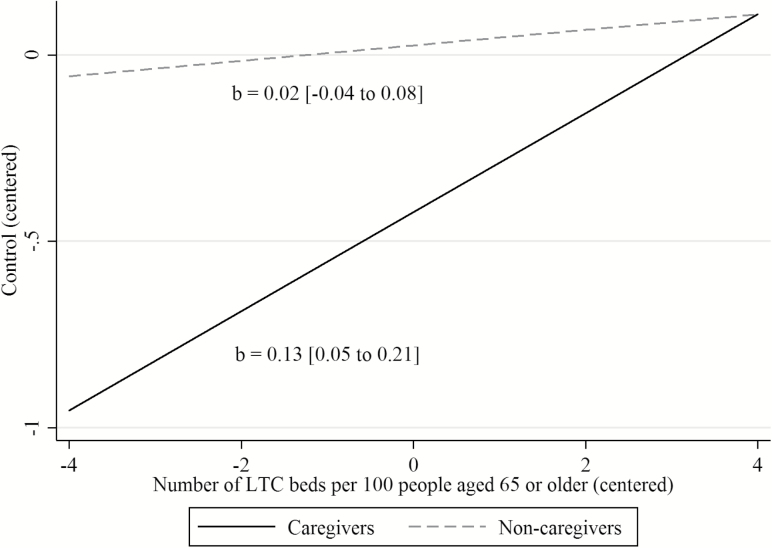
To further investigate this mechanism, we additionally checked whether the extent of control that caregivers generally perceived was linked to the LTC availability in a region. We regressed perceived control on an interaction of partner care and LTC availability again controlling for socioeconomic characteristics and general wealth of a region (results not displayed). Spousal caregivers felt that they had less control over their lives than noncaregivers, which was the main effect of partner care (b = −0.45; SE = 0.05). The main effect of LTC availability was insignificant; therefore, LTC availability as such was not related to the respondents’ sense of control. However, a highly significant interaction was found (b = 0.11; SE = 0.028), indicating that spousal caregivers and noncaregivers differ in their relation between control and LTC availability. When calculating the margins for caregivers and noncaregivers we found that caregivers’ perceived control over their lives was connected to the LTC availability in a region, but not so for noncaregivers. The result is displayed in Figure 1.
Figure 1.
Control of caregivers and non-caregivers varies with the availability of formal LTC services.
Discussion
In a time of an expected rise in care-dependency and a drop in informal care potentials, it is critical to understand how regional contexts are related to the caregiver well-being to inform evidence-based policies. Regarding formal care, trends toward deinstitutionalization, privatization, and marketization are favored in many European countries to counteract the rising costs of formal care (Deusdad et al., 2016) and the legal responsibility for LTC is shifted toward communities and local governments (Ranci & Pavolini, 2013). This article analyzed whether and how regional formal LTC provision is linked to the well-being of spousal caregivers. We theoretically differentiated two possible causal pathways and included a measure of perceived control as a basic test of the cognitive-emotional pathway into our analyses. Our baseline result showed that spousal caregivers’ well-being is related to the availability of formal care in a region which is not the case for noncaregiving spouses.
Our findings are in line with previous research that examined the relation of country differences in formal care to caregivers’ quality of life (Ruppanner & Bostean, 2014; Verbakel, 2014), self-rated health (Dujardin et al., 2011), and loneliness (Wagner & Brandt, 2015). By using data from 138 regions across 11 European countries we additionally exploited the enormous variation in LTC contexts across European countries and regions. The trend of decentralization of LTC contributes to more regional variation in formal care availability. So by analyzing the regional level, we are actually closer to where the decisions on how to arrange LTC take place, which is the community or even the neighborhood. Methodologically, we overcame the shortcoming from previous studies that had to deal with a very low number of observations at the contextual level which can lead to spurious significant effects (Maas & Hox, 2004). Moreover, the ICC at the region-within-country level showed slightly more variation in well-being within European regions which we would have missed in a country comparison only. Taken together, regional data may be better suited than country comparisons only to measure contextual effects on caregiver well-being.
Our second result showed that the significant interaction of caregiving and regional LTC availability vanished for loneliness and depression when adding a measure of perceived control to the analyses implying that the link between LTC and well-being of caregivers was mediated by perceived control. For overall life satisfaction, a significant interaction remained. One possible explanation is that overall life satisfaction as a more comprehensive measure of well-being may be less strongly related to the care situation than loneliness or depression. We further investigated this possible mechanism and found that for caregivers, perceived control over one’s life was linked to the regional LTC availability, but not so for noncaregivers. We conclude that a higher sense of control is an important mechanism through which LTC availability is beneficial for caregivers, consistent with the limited previous research on cognitive pathways (e.g., Schulz et al., 2012; Wallhagen, 1992).
When communities and local governments become increasingly responsible for the organization of LTC services, they should thus focus not only on care supply but also on the suppliers and arrange formal support services that unburden informal caregivers—and by that may in turn even lead to a higher informal care supply (Brandt, 2013). Based on our findings, local governments can actively influence the conditions for healthy aging of a growing number of informal caregivers and receivers: When people are forced to become caregivers, it will come at the expense of their well-being and possibly also at the expense of the quality of care. Perceived control over life in general and the care situation in particular seems to be an important mechanism here. Our results suggest that offering alternatives to informal care is a key factor to improve caregiver well-being. Low-threshold assistance is necessary, especially for partner caregivers, who are most burdened by providing care (Kaschowitz & Brandt, 2016; Tennstedt et al., 1993). According to the state of research (also see, e.g., Da Roit, 2013; Glendinning, 2013), the trend of cutting back on formal LTC options is expected to have negative influences on informal care.
Limitations and Suggestions for Future Research
Several limitations of the current analysis are worth noting. Although we laid down theoretical arguments supporting the cognitive-emotional pathway leading from LTC availability via a higher sense of control to better well-being of caregivers, our results do not allow for causal interpretations. Even after controlling for many socioeconomic factors, selection effects cannot be ruled out completely. For example, regional differences in care couples that are confounded with our measures, for example, due to caregiving norms, female labor participation, or conjugal duties could play a role. Along with that, we could not analyze the behavioral pathway to check whether the actual uptake of additional care support is beneficial for caregivers as it requires longitudinal data collected in short intervals and a measure of care intensity which was not available. Thus, we cannot ascertain whether caregivers who live in regions with more LTC offers actually do less demanding care tasks and therefore, have higher well-being. As a result, we might overestimate the importance of control. Further research could analyze both pathways jointly to find an answer to this question.
By using regional information on LTC availability, we were able to get closer to where the decisions on LTC arrangements actually take place. However, the NUTS-2 classification may still be too broad as it comprises region with 800,000 to 3,000,000 inhabitants. Measures at the level of the municipality might be better suited for our analysis but this data was neither available in the SHARE dataset nor in international databases on LTC. Such data may be available for single countries.
Our indicator of the availability of LTC beds is a proxy; however, beds in nursing homes are not the only way of providing formal LTC. Some countries have placed a stronger emphasis on nursing homes, whereas others have focused more on the provision of home care services (Ranci & Pavolini, 2013). Alternative measures such as LTC expenditure or formal LTC provided at home are unfortunately not available in all countries and regions. As a robustness check, we calculated a regional measure of the share of people using formal home care services based on SHARE (problematic due to small sample sizes in some regions, possible autocorrelation when both partners were interviewed, and missing weights). The results (not shown, available upon request) were very similar to the results obtained with the official macro data. Still, once there are comparable data available on the regional level, it will be important to investigate other measures of formal care arrangements.
The validity of our LTC indicator in measuring the amount of alternatives and control that spousal caregivers perceive might be reduced when many spousal caregivers do not actually consider formal LTC services as an option—in that case we present a rather conservative estimation of the links between LTC and caregivers’ well-being. Further research could also extend the study to more care relations and analyze whether the links found can be generalized to other caregiving relations in addition to spouses—and perhaps, following the above considerations, identify even stronger links due to a lower private care obligation.
Limitations also comprise our measure of control and possible unobserved variables that may influence the control over the care situation. First, the measure includes control over life in general, not control over the care situation and might therefore be not specific enough. Second, the extent to which caregivers’ sense of control might be related to the availability of LTC services could also vary due to different normative expectations about caregiving in different European countries (Saraceno, 2010) and possibly also regions. Norms on caregiving are likely to shape one’s expectations regarding caregiving and thus affect the perceived control over the care situation. For example, Oudijk, Woittiez, and de Boer (2011) found that caregivers in familialistic societies felt less obliged to take over care than potential caregivers in individualistic societies. Future research should measure caregivers’ experienced control and shed light on differences in caregivers’ feelings of control as related to social norms and expectations.
All these considerations however do not challenge our main conclusion that formal care services are an important means of improving the situations of not only care receivers but also informal caregivers today—and they will become ever more important with rising care needs and fewer informal care resources in aging societies.
Funding
This article uses data from SHARE Waves 1, 2, 4 and 5 (DOIs: 10.6103/SHARE.w1.500, 10.6103/SHARE.w2.500, 10.6103/SHARE.w4.500, 10.6103/SHARE.w5.500), see Börsch-Supan et al., (2013) for methodological details. The SHARE data collection has been primarily funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006–062193), and FP7 (SHARE-PREP: N°211909, SHARE-LEAP: N°227822, SHARE M4: N°261982). Additional funding from the German Ministry of Education and Research, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064) and from various national funding sources is gratefully acknowledged (see www.share-eric.org).
Author Contributions
M. Wagner planned the study, performed the statistical analysis, and wrote the paper. M. Brandt supervised the planning of the study and the data analysis, and revised the manuscript.
Conflict of Interest
None reported.
Supplementary Material
Acknowledgments
We are grateful to Candace Kemp, to the anonymous reviewers and to our colleague Thorsten Kneip for helpful comments and suggestions. We want to thank Theresa Faber and Maximilian Scherer for their research assistance during various stages of the project.
References
- Agree E. M., & Glaser K (2009). Demography of informal caregiving. In Uhlenberg P. (Ed.), International handbook of population aging (pp. 647–668). Dordrecht, Netherlands: Springer. doi:10.1007/978-1-4020-8356-3_29 [Google Scholar]
- Beeson R. A. (2003). Loneliness and depression in spousal caregivers of those with Alzheimer’s disease versus non-caregiving spouses. Archives of Psychiatric Nursing, 17, 135–143. doi:10.1016/s0883-9417(03)00057-8 [DOI] [PubMed] [Google Scholar]
- Bolin K., Lindgren B., & Lundborg P (2008). Informal and formal care among single-living elderly in Europe. Health Economics, 17, 393–409. doi:10.1002/hec.1275 [DOI] [PubMed] [Google Scholar]
- Bonsang E. (2009). Does informal care from children to their elderly parents substitute for formal care in Europe?Journal of Health Economics, 28, 143–154. doi:10.1016/j.jhealeco.2008.09.002 [DOI] [PubMed] [Google Scholar]
- Börsch-Supan A., Brandt M., Hunkler C., Kneip T., Korbmacher J., Malter F., … Zuber S; SHARE Central Coordination Team (2013). Data resource profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). International Journal of Epidemiology, 42, 992–1001. doi:10.1093/ije/dyt088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Börsch-Supan A. (Ed.). (2015). Survey of health, ageing and retirement in Europe (SHARE) Wave 5: Release version: 5.0.0 http://www.share-project.org/data-documentation/waves-overview/wave-5.html
- Brandt M., Haberkern K., & Szydlik M (2009). Intergenerational help and care in Europe. European Sociological Review, 25, 585–601. doi:10.1093/esr/jcn076 [Google Scholar]
- Brandt M. (2013). Intergenerational help and public assistance in Europe. European Societies, 15, 26–56. doi:10.1080/14616696.2012.726733 [Google Scholar]
- Broese van Groenou M. I., de Boer A., & Iedema J (2013). Positive and negative evaluation of caregiving among three different types of informal care relationships. European Journal of Ageing, 10, 301–311. doi:10.1007/s10433-013-0276-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan M. L., & Jenkins S. P (2015). Multilevel modelling of country effects: A cautionary tale. European Sociological Review, 32, 3–22. doi:10.1093/esr/jcv059 [Google Scholar]
- Chappell N., & Blandford A (1991). Informal and formal care: Exploring the complementarity. Ageing and Society, 11, 299–317. doi:10.1017/S0144686X00004189 [Google Scholar]
- Coburn A. F. (2002). Rural long-term care: What do we need to know to improve policy and programs?The Journal of Rural Health, 18, 256–269. doi:10.1111/j.1748-0361.2002.tb00935.x [DOI] [PubMed] [Google Scholar]
- Colombo F., Llena-Nozal A., Mercier J., & Tjadens F (Eds.). (2011). Help wanted? Providing and paying for long-term care. Paris: OECD Publishing; Retrieved from http://www.oecd.org/els/health-systems/help-wanted-9789264097759-en.htm. [Google Scholar]
- Da Roit B. (2013). Long-term care reforms in the Netherlands. In Ranci C. & Pavolini E. (Eds.), Reforms in long-term care policies in Europe (pp. 97–115). doi:10.1007/978-1-4614-4502-9_5 [Google Scholar]
- de Jong Gierveld J., & Havens B (2004). Cross-national comparisons of social isolation and loneliness: Introduction and overview. Canadian Journal on Aging = La revue canadienne du vieillissement, 23, 109–113. doi:10.1353/cja.2004.0021 [DOI] [PubMed] [Google Scholar]
- Deusdad B. A., Pace C., & Anttonen A (2016). Facing the challenges in the development of long-term care for older people in Europe in the context of an economic crisis. Journal of Social Service Research, 42, 144–150. doi:10.1080/01488376.2015.1133147 [Google Scholar]
- Diener E., Suh E. M., Lucas R. E., & Smith H. L (1999). Subjective well-being: Three decades of progress. Psychological Bulletin, 125, 276–302. doi:10.1037/0033-2909.125.2.276 [Google Scholar]
- Dujardin C., Farfan-Portet M. I., Mitchell R., Popham F., Thomas I., & Lorant V (2011). Does country influence the health burden of informal care? An international comparison between Belgium and Great Britain. Social Science & Medicine (1982), 73, 1123–1132. doi:10.1016/j.socscimed.2011.07.016 [DOI] [PubMed] [Google Scholar]
- EUROSTAT (2016). Database Retrieved from http://ec.europa.eu/eurostat/data/database.
- Federal Statistical Office Germany (2016). Regionaldatenbank Deutschland Retrieved from https://www.regionalstatistik.de/.
- Federal Statistical Office Switzerland.(2016). Regionale Indikatoren Retrieved from http://www.bfs.admin.ch/bfs/portal/de/index/themen/04/02/05.html.
- Genet N., Boerma W. G., Kringos D. S., Bouman A., Francke A. L., Fagerström C., … & Devillé W (2011). Home care in Europe: A systematic literature review. BMC Health Services Research, 11, 207. doi:10.1186/1472-6963-11-207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genet N., Boerma W. G. W., Kroneman M., Hutchinson A., & Saltman R. B (2013). Home care across Europe: Case studies. European Observatory on Health Systems and Policies London. [PubMed] [Google Scholar]
- Garms-Homolova V., Naiditch M., Fagerström C., … Hutchinson A (2013). Clients in focus. In:Genet N., Boerma W., Kroneman M., Hutchinson A., Saltman R.B. (Eds): Home care across Europe. Current structure and future challenges. Brussels: European Observatory on Health Systems and Policies, Copenhagen, Denmark: (pp. 55–70). [Google Scholar]
- George L. K., & Gwyther L. P (1986). Caregiver well-being: A multidimensional examination of family caregivers of demented adults. The Gerontologist, 26, 253–259. doi:10.1093/geront/26.3.253 [DOI] [PubMed] [Google Scholar]
- Glendinning C. (2013). Long term care reform in England: A long and unfinished story. In Ranci C. & Pavolini E. (Eds.), Reforms in long-term care policies in Europe. New York, NY: Springer; (pp. 179–200). doi:10.1007/978-1-4614-4502-9_9 [Google Scholar]
- Kaschowitz J., & Brandt M (2016). Health effects of informal caregiving across Europe: A longitudinal approach. Social Science & Medicine, 173, 72–80. doi:10.1016/j.socscimed.2016.11.036 [DOI] [PubMed] [Google Scholar]
- Maas C. J. M., & Hox J. J (2004). Robustness issues in multilevel regression analysis. Statistica Neerlandica, 58, 127–137. doi:10.1046/j.0039-0402.2003.00252.x [Google Scholar]
- Oudijk D., Woittiez I., & de Boer A (2011). More family responsibility, more informal care? The effect of motivation on the giving of informal care by people aged over 50 in the Netherlands compared to other European countries. Health policy (Amsterdam, Netherlands), 101, 228–235. doi:10.1016/j.healthpol.2011.05.004 [DOI] [PubMed] [Google Scholar]
- Patrick B. C., Skinner E. A., & Connell J. P (1993). What motivates children’s behavior and emotion? Joint effects of perceived control and autonomy in the academic domain. Journal of Personality and Social Psychology, 65, 781–791. doi:10.1037/0022-3514.65.4.781 [DOI] [PubMed] [Google Scholar]
- Pearlin L. I., Mullan J. T., Semple S. J., & Skaff M. M (1990). Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist, 30, 583–594. doi:10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Pinquart M., & Sörensen S (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging, 18, 250–267. doi:10.1037/0882-7974.18.2.250 [DOI] [PubMed] [Google Scholar]
- Pinquart M., & Sörensen S (2007). Correlates of physical health of informal caregivers: A meta-analysis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 62, P126–P137. doi:10.1093/geronb/62.2.P126 [DOI] [PubMed] [Google Scholar]
- Pinquart M., & Sörensen S (2011). Spouses, adult children, and children-in-law as caregivers of older adults: A meta-analytic comparison. Psychology and Aging, 26, 1–14. doi:10.1037/a0021863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince M. J., Reischies F., Beekman A. T., Fuhrer R., Jonker C., Kivela S. L., … Copeland J. R (1999). Development of the EURO-D scale–a European, Union initiative to compare symptoms of depression in 14 European centres. The British Journal of Psychiatry: The Journal of Mental Science, 174, 330–338. doi:10.1192/bjp.174.4.330 [DOI] [PubMed] [Google Scholar]
- Ranci C., & Pavolini E (2013). Institutional change in long-term care: Actors, mechanisms and impacts. In Ranci C. & Pavolini E. (Eds.), Reforms in long-term care policies in Europe: Investigating institutional change and social impacts, New York, NY: Springer; (pp. 269–314). doi:10.1007/978-1-4614-4502-9_13 [Google Scholar]
- Rodin J. (1986). Aging and health: Effects of the sense of control. Science (New York, N.Y.), 233, 1271–1276. doi:10.1126/science.3749877 [DOI] [PubMed] [Google Scholar]
- Rotter J. B. (1966). Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs, 80, 1–28. doi:10.1037/h0092976 [PubMed] [Google Scholar]
- Ruppanner L., & Bostean G (2014). Who cares? Caregiver well-being in Europe. European Sociological Review, 30, 655–669. doi:10.1093/esr/jcu065 [Google Scholar]
- Russell D., Peplau L. A., & Cutrona C. E (1980). The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology, 39, 472–480. [DOI] [PubMed] [Google Scholar]
- Saraceno C. (2010). Social inequalities in facing old-age dependency: A bi-generational perspective. Journal of European Social Policy, 20, 32–44. doi:10.1177/0958928709352540 [Google Scholar]
- Schulz R., & Brenner G (1977). Relocation of the aged: A review and theoretical analysis. Journal of Gerontology, 32, 323–333. doi:10.1093/geronj/32.3.323 [DOI] [PubMed] [Google Scholar]
- Schulz R., Visintainer P., & Williamson G. M (1990). Psychiatric and physical morbidity effects of caregiving. Journal of Gerontology, 45, P181–P191. doi:10.1093/geronj/45.5.P181 [DOI] [PubMed] [Google Scholar]
- Schulz R., Beach S. R., Cook T. B., Martire L. M., Tomlinson J. M., & Monin J. K (2012). Predictors and consequences of perceived lack of choice in becoming an informal caregiver. Aging & Mental Health, 16, 712–721. doi:10.1080/13607863.2011.651439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Denmark (2016). Living conditions Retrieved from http://www.statbank.dk/10048.
- Stuifenbergen M. C., van Delden J. J. M., & Dykstra P. A (2008). The implications of today’s family structures for support giving to older parents. Ageing and Society, 28, 413–434. doi:10.1017/S0144686X07006666 [Google Scholar]
- Suanet B., Broese van Groenou M., & van Tilburg T (2012). Informal and formal home-care use among older adults in Europe: Can cross-national differences be explained by societal context and composition?Ageing and Society, 32, 491–515. doi:10.1017/S0144686X11000390 [Google Scholar]
- Tennstedt S. L., Crawford S., & McKinlay J. B (1993). Determining the pattern of community care: Is coresidence more important than caregiver relationship?Journal of Gerontology, 48, S74–S83. [DOI] [PubMed] [Google Scholar]
- Verbakel E. (2014). Informal caregiving and well-being in Europe: What can ease the negative consequences for caregivers?Journal of European Social Policy, 24, 424–441. doi:10.1177/0958928714543902 [Google Scholar]
- Verbakel E., Metzelthin S. F., & Kempen G. I (2016). Caregiving to older adults: Determinants of informal caregivers’ subjective well-being and formal and informal support as alleviating conditions. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 1–13. doi:10.1093/geronb/gbw047 [DOI] [PubMed] [Google Scholar]
- von dem Knesebeck O., Hyde M., Higgs P., Kupfer A., & Siegrist J (2005). Quality of life and well-being. In Börsch-Supan A.,Brugiavini A.,Jürges H.,Mackenbach J.,Siegrist J., & Weber G. (Eds.), Health, ageing and retirement in Europe – First results from the Survey of Health, Ageing and Retirement in Europe (pp. 199–203). Mannheim: Mannheim Research Institute for the Economics of Aging (MEA). [Google Scholar]
- Wagner M., Brandt M (2015). Loneliness among informal caregivers aged 50+. In Boersch-Supan A., Brandt M., Litwin H., Weber G (Eds.), Ageing in Europe – Supporting policies for an inclusive society (pp. 179–188). Berlin/Boston: De Gruyter. [Google Scholar]
- Wallhagen M. I. (1992). Perceived control and adaptation in elder caregivers: Development of an explanatory model. International Journal of Aging & Human Development, 36, 219–237. doi:10.2190/ba90-aqx3-t6ce-abek [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.