Abstract
Background
Little is known about patterns of end-of-life care for patients with advanced kidney disease not treated with maintenance dialysis.
Study Design
Case series.
Setting & Participants
A sample of 14,071 patients with a sustained estimated glomerular filtration rate <15 ml/min/1.73m2 treated in the US Veterans Affairs (VA) health care system who died during 2000–2011. Prior to death, 12,756 of these patients had been treated with dialysis, 503 had been discussing and/or preparing for dialysis, and, for 812, there had been a decision not to pursue dialysis.
Outcomes
Hospitalization and receipt of an intensive procedure during the final month of life, in-hospital death, and palliative care consultation and hospice enrollment prior to death.
Results
Compared with decedents treated with dialysis, those for whom a decision not to pursue dialysis had been made were less often hospitalized (57.3% vs. 76.8%; OR, 0.40 [95% CI, 0.34–0.46]), were less often the recipient of an intensive procedure (3.5% vs. 24.6%; OR, 0.15 [95% CI, 0.10–0.22]), more often the recipient of a palliative care consultation (52.6% vs. 21.6%; OR, 4.19 [95% CI, 3.58–4.90]), more often used hospice services (38.7% vs. 18.2%; OR, 3.32 [95% CI, 2.83–3.89]) and died less frequently in a hospital (41.4% vs. 57.3%; OR, 0.78 [95% CI, 0.74–0.82]). Hospitalization (55.5%; OR, 0.39 [95% CI, 0.32–0.46]), receipt of an intensive procedure (13.7%; OR, 0.60 [95% CI, 0.46–0.77]), and in-hospital death (39.0%; OR, 0.47 [95% CI, 0.39–0.56]) were also less common among decedents who had been discussing and/or preparing for dialysis, but their utilization of palliative care and hospice services were similar.
Limitations
Findings may not be generalizable to groups not well-represented in the VA health care system.
Conclusions
Among decedents, patients not treated with dialysis prior to death received less intensive patterns of end-of-life care than those treated with dialysis. Decedents for whom there had been a decision not to pursue dialysis prior to death were more likely to receive palliative care and hospice.
Index words: chronic kidney disease (CKD), kidney failure, dialysis, conservative care, palliative care, hospice, end-of-life care, intensive treatment, health care intensity
Although advances in medical science and technology have led to improvements in population health and longevity, the potential benefits of interventions intended to prolong life tend to diminish as patients approach the end of life. For patients with advanced chronic kidney disease (CKD), potential gains in longevity with maintenance dialysis are sometimes offset by the challenges that can be associated with this treatment such as more frequent interaction with the healthcare system,1,2 and loss of employment, independence, and physical and social function,3–5 especially given the uncertain affect of dialysis on symptom burden.6,7
In other developed countries, there is growing experience with models of conservative care intended to support patients with advanced CKD who do not plan to pursue dialysis. Several observational studies conducted in Europe and Asia suggest that older patients (75 years or older) with a high burden of comorbidity and poor functional status who opt for conservative management may have a life expectancy8–12 and quality of life13,14 comparable to those who initiate dialysis. Based on data from outside the United States, patients with advanced CKD opting for conservative management also spend less time in the hospital toward the end of life,2,11 are less likely to receive invasive procedures11 and to die in the hospital,2,10,11,15,16 and are more likely to receive palliative care and hospice.10,11,16
Concerted efforts to establish conservative care programs as a therapeutic alternative to maintenance dialysis in the United States lag considerably behind some other developed countries. Older patients with advanced CKD are far more likely to be treated with dialysis in the United States than in other developed countries,17 and qualitative data suggest that US patients seem to view maintenance dialysis as a treatment that will inevitably be “needed” rather than as a distinct treatment “choice.”18–20 To our knowledge, no prior studies have compared patterns of end-of-life care among US patients with advanced CKD treated and not treated with dialysis.
Methods
Study Population
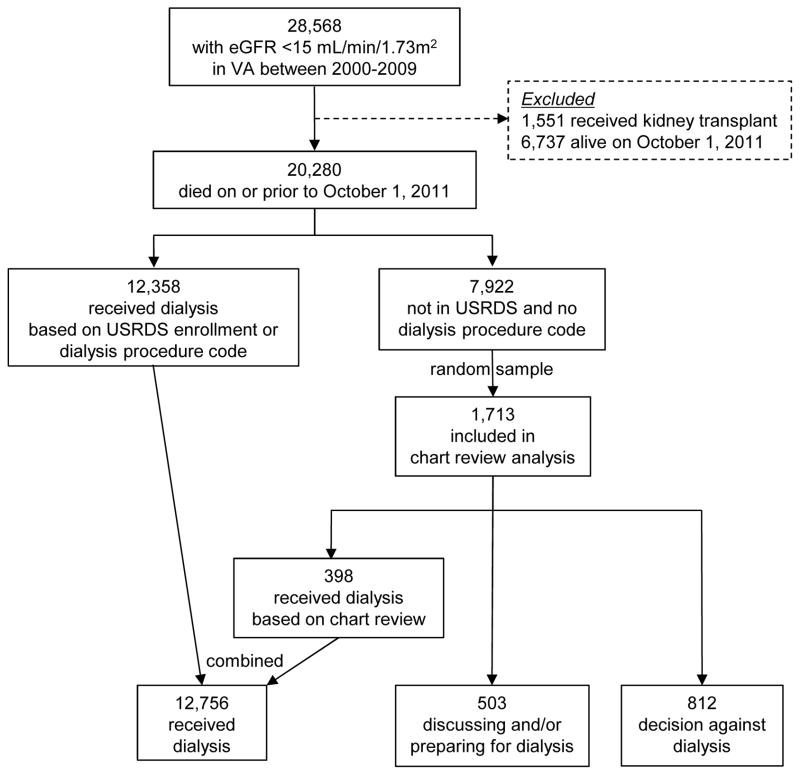
We conducted a retrospective review of patterns of end-of-life care among decedents of a previously assembled national cohort of 28,568 adults with at least two outpatient measures of an estimated glomerular filtration rate (eGFR) <15 ml/min/1.73m2 drawn at least 90 days apart within the US Veterans Affairs (VA) health care system during the period 2000–2009.17 As previously described,17 we used a combination of administrative and clinical data from VA data sources, the US Renal Data System (USRDS)—a national registry for treated end-stage renal disease—and Medicare claims to define and characterize the original study cohort. Patients entered the cohort on the date of their second eGFR <15 ml/min/1.73m2 and were followed up through their date of death or October 1, 2011, whichever came first. The current case series excludes cohort members who received a kidney transplant (n=1,551) and is restricted to cohort members who died during follow-up (n=20,280) (Figure 1).
Figure 1. Derivation of decedent sample.
Note: a flow chart of the full cohort derivation is provided in Wong et al.17 (Abbreviations: eGFR, estimated glomerular filtration rate; VA, Veterans Affairs; USRDS, United Stated Renal Data System)
As described previously,17 we categorized patients according to their treatment status with respect to dialysis. Briefly, we considered patients who were enrolled in USRDS or had at least one dialysis procedure code in VA or Medicare files prior to death as having been treated with dialysis (n=12,358). We performed a detailed review of the VA-wide electronic medical record for a random sample of the remaining 7,922 patients in order to confirm that they had not received dialysis and to characterize their treatment status closest to the time of death. Of the 1,713 patients selected for chart review, 398 had in fact received dialysis prior to death (for analytic purposes, these patients were included in the aforementioned group treated with dialysis), 503 were discussing and/or preparing for dialysis but had not initiated dialysis prior to death, and, in 812, an implicit or explicit decision was made by the patients themselves, their family members and/or providers not to pursue dialysis prior to death (Figure 1).
End-of-Life Care
We ascertained whether decedents had been hospitalized and had received an intensive procedure (cardiopulmonary resuscitation, mechanical ventilation or artificial enteral nutrition) during the final month of life, had died in the hospital, and had received a palliative care consultation and/or hospice care prior to death from VA and Fee-Basis administrative files (which include information on care received both within the VA and outside the VA but paid for by the VA) and Medicare Institutional and Physician Supplier claims. We also ascertained the number of days spent in the hospital during the final month of life and the timing of first palliative care consultation and hospice enrollment in relation to death.
Decedent Characteristics
We used the VA Decision Support System Laboratory Results File to ascertain outpatient serum creatinine measurements and calculated each patient’s eGFR using the MDRD (Modification of Diet in Renal Disease) Study equation. We obtained information on race (categorized as white, black and other), sex and age (categorized as <65, 65–74, 75–84 and ≥85 years) at the time of each patient’s second eGFR <15 ml/min/1.73m2 from the VA Vital Status File. We used both VA administrative data and Medicare claims to obtain information on nephrology clinic visits (categorized as no prior visits, 1–3 clinic visits, and ≥4 visits) and the following co-morbidities based on the presence of relevant diagnostic codes on at least two claims during the year prior to the date of the second eGFR <15 ml/min/1.73m2: coronary artery disease, congestive heart failure, chronic obstructive pulmonary disease, cirrhosis, peripheral artery disease, hypertension, diabetes, dementia, cancer, and stroke. We also categorized patients by tertile of Gagne comorbidity score21 as having low (scores< 4), moderate (score = 4–6) or high (score >6) comorbid burden based on diagnostic codes in VA administrative files and Medicare claims during the year before their second eGFR <15 ml/min/1.73m2.
Analytical Approach
We compared characteristics of decedents categorized according to their treatment status at the time of death using chi-square tests and ANOVA as appropriate. We tested for differences in patterns of end-of-life care between treatment groups using logistic or linear regression models, as appropriate, and included all measured patient characteristics and calendar year of death.
We used SAS, version 9 (SAS Institute Inc., Cary, NC) to construct the analytic dataset, and SPSS version 19 (IBM SPSS, Somers, NY) to conduct statistical analyses.
Results
Decedent Characteristics
Median time from the date of the second eGFR <15 ml/min/1.73m2 to death was 32.0 (interquartile range [IQR], 16.0–53.8) months for decedents who had received dialysis, 6.8 (IQR, 2.2–16.6) months for those who had been discussing and/or preparing for dialysis, and 5.7 (IQR, 1.1–17.2) months for those in whom there had been a decision against dialysis (p-value <0.001). The mean value of the second eGFR <15 ml/min/1.73m2 was 11.3±2.6 ml/min/1.73m2 for decedents who had been treated with dialysis, 12.0±2.3 ml/min/1.73m2 for those who had been discussing and/or preparing for dialysis, and 11.7±2.5 ml/min/1.73m2 for those in whom there had been a decision against dialysis (p-value <0.001). As compared with decedents who had received dialysis, those who were discussing and/or preparing for dialysis and those in whom there was a decision against dialysis tended to be older, less often black, and to have a higher burden of comorbidity and less nephrology care (Table 1). Most comorbidities were also more prevalent among decedents not treated with dialysis.
Table 1.
Characteristics of decedents with advanced kidney disease
| Received dialysis (n=12,756) | Discussing and/or preparing for dialysis (n=503) | Decision against dialysis (n=812) | p-value | |
|---|---|---|---|---|
| Age | <0.001 | |||
| <65 y | 4767 (37.4) | 172 (34.2) | 145 (17.9) | |
| 65–74 y | 3984 (31.2) | 145 (28.8) | 173 (21.3) | |
| 75–84 y | 3572 (28.0) | 149 (29.6) | 351 (43.2) | |
| ≥85 y | 433 (3.4) | 37 (7.4) | 143 (17.6) | |
| Race | <0.001 | |||
| White | 7941 (62.3) | 293 (58.3) | 542 (66.8) | |
| Black | 3596 (28.2) | 99 (19.7) | 156 (19.2) | |
| Other | 1219 (9.6) | 111 (22.1) | 114 (14.0) | |
| Sex | 0.9 | |||
| Female | 159 (1.3) | 6 (1.2) | 9 (1.1) | |
| Male | 12597 (98.8) | 497 (98.8) | 803 (98.9) | |
| Burden of comorbidity | <0.001 | |||
| Low | 4579 (35.9) | 130 (25.8) | 175 (21.6) | |
| Moderate | 5088 (39.9) | 205 (40.8) | 278 (34.2) | |
| High | 3025 (23.7) | 167 (33.2) | 350 (43.1) | |
| Missing | 64 (0.5) | 1 (0.2) | 9 (1.1) | |
| Comorbidities | ||||
| Hypertension | 11875 (93.1) | 466 (92.6) | 722 (88.9) | <0.001 |
| Coronary artery disease | 5412 (42.4) | 240 (47.7) | 374 (46.1) | 0.01 |
| Congestive heart failure | 4268 (33.5) | 188 (37.4) | 344 (42.4) | <0.001 |
| Diabetes mellitus | 8101 (63.5) | 275 (54.7) | 428 (52.7) | <0.001 |
| Peripheral artery disease | 1976 (15.5) | 83 (16.5) | 137 (16.8) | 0.5 |
| Cancer | 2381 (18.7) | 143 (28.4) | 261 (32.1) | <0.001 |
| Chronic obstructive pulmonary disease | 2326 (18.2) | 132 (26.2) | 234 (28.8) | <0.001 |
| Dementia | 226 (1.8) | 18 (3.6) | 73 (9.0) | <0.001 |
| Stroke | 1097 (8.6) | 51 (10.1) | 106 (13.1) | <0.001 |
| Cirrhosis | 162 (1.3) | 15 (3.0) | 17 (2.1) | 0.001 |
| Nephrology care in year prior | <0.001 | |||
| None | 3039 (23.8) | 174 (34.6) | 380 (46.8) | |
| 1–3 clinic visits | 5095 (39.9) | 196 (39.0) | 285 (35.1) | |
| ≥4 clinic visits | 4622 (36.2) | 133 (26.4) | 147 (18.1) |
Note: Values are given as number (percentage). Characteristics were ascertained at date of second eGFR <15 ml/min/1.73 m2.
End-of-Life Care
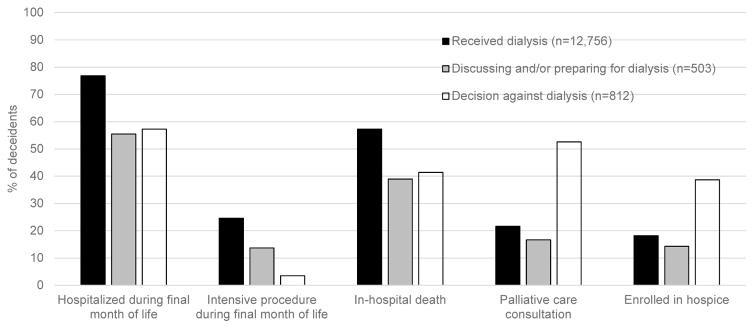
As compared with decedents who had been treated with dialysis, those for whom there had been a decision not to pursue dialysis were less likely to have been hospitalized during the final month of life (57.3% vs. 76.8%; odds ratio [OR], 0.40; 95% confidence interval [CI], 0.34–0.46), were less likely to have received an intensive procedure during the final month of life (3.5% vs. 24.6%; OR, 0.15 [95% CI, 0.10–0.22]) and to have died in the hospital (41.4% vs. 57.3%; OR, 0.78 [95% CI, 0.74–0.82]), and were more likely to have received a palliative care consultation (52.6% vs. 21.6%; OR, 4.19 [95% CI, 3.58–4.90]) and hospice care (38.7% vs. 18.2%; OR, 3.32 [95% CI, 2.83–3.89]) (Figure 2). Decedents in whom there had been a decision not to pursue dialysis also spent fewer days in the hospital during the last month of life (median of 10.0 [IQR, 4.0–24.0] vs. 14.0 [IQR, 6.0–28.0] days; p-value <0.001), and received longer periods of palliative care (median of 27.0 [IQR, 5.0–81.0] vs. 7.0 [IQR, 3.0–29.0] days; p-value <0.001) and hospice services (median of 14.0 [IQR, 1.0–68.0] vs. 6.0 [IQR, 2.0–32.0] days; p-value <0.001) than those treated with dialysis (Table 2). Hospitalization (55.5%; OR, 0.39 [95% CI, 0.32–0.46]) and receipt of an intensive procedure (13.7%; OR, 0.60 [95% CI, 0.46–0.77]) during the final month of life and in-hospital death (39.0%; OR, 0.47 [95% CI, 0.39–0.56]) were also less common among decedents discussing and/or preparing for dialysis as compared with those treated with dialysis. However, their utilization of palliative care (16.7%; OR, 0.78 [95% CI, 0.61–1.01]) and hospice services (14.3%; OR, 0.86 [95% CI, 0.67–1.12]) was no different than for those treated with dialysis.
Figure 2.
End-of-life care among decedents with advanced kidney disease
Table 2.
End-of-life care among decedents with advanced kidney disease
| Received dialysis (n=12,756) | Discussing and/or preparing for dialysis (n=503) | Decision against dialysis (n=812) | |||
|---|---|---|---|---|---|
| median [IQR] | median [IQR] | p-valuea | median [IQR] | p-valuea | |
| Days hospitalized during final month of life | 14.0 [6.0–28.0] | 8.0 [3.0–21.0] | <0.001 | 10.0 [4.0–24.0] | <0.001 |
| Days prior to death of first palliative care encounter | 7.0 [3.0–29.0] | 8.0 [3.0–27.8] | 0.3 | 27.0 [5.0–81.0] | <0.001 |
| Days enrolled in hospice | 6.0 [2.0–32.0] | 8.0 [2.0–27.8] | 0.5 | 14.0 [1.0–68.0] | 0.07 |
Abbreviation: IQR, interquartile range
reference group is patients who received dialysis; linear regression models adjusted for age, race, sex, comorbidity burden, comorbidities, prior nephrology care, and year of death
Discussion
We believe this study providing information on patterns of end-of-life care among US patients with advanced CKD not treated with dialysis is novel. Consistent with prior studies conducted outside the United States,2,10,11,15,16 patients with advanced CKD not treated with dialysis prior to death—especially those for whom there was a decision not to pursue dialysis—received less intensive patterns of inpatient care near the end of life than those treated with dialysis. They were less likely to be hospitalized and to receive invasive procedures intended to prolong life, spent less time in the hospital, and were less likely to die in the hospital than patients who received dialysis prior to death. However, only the subgroup of patients for whom there had been an implicit or explicit decision not to pursue dialysis prior to death were more likely than those treated with dialysis to have received a palliative care consultation and hospice, and tended to receive these services for longer periods of time before death.
Hospice utilization under Medicare is known to be low among patients treated with maintenance dialysis and is often accompanied by discontinuation of diaysis.22 The strong association between hospice utilization and dialysis discontinuation among patients on dialysis is often attributed to barriers to reimbursement for concurrent receipt of dialysis and hospice care under the Medicare Program, which can have the effect of forcing patients to choose between these two benefits.23 Nevertheless, hospice use among members of this veteran sample treated with dialysis prior to death (18.2%)—for whom there are theoretically fewer regulatory barriers to concurrent receipt of dialysis and hospice services—was comparable to that reported for Medicare beneficiaries on dialysis who died during the same time frame (17.9%).22 Furthermore, rates of palliative care consultation (for which there are no such regulatory barriers under Medicare or within the VA) and hospice enrollment were only higher for patients not treated with dialysis when there had been an implicit or explicit decision not to pursue dialysis prior to death. Rates of hospice and palliative care utilization for patients discussing and/or preparing for dialysis at the time of death were no different than for those treated with dialysis. These findings suggest that unless there is a concrete decision not to pursue dialysis, utilization of palliative care and hospice services may be as limited for patients with advanced CKD not on dialysis as for those already receiving dialysis.
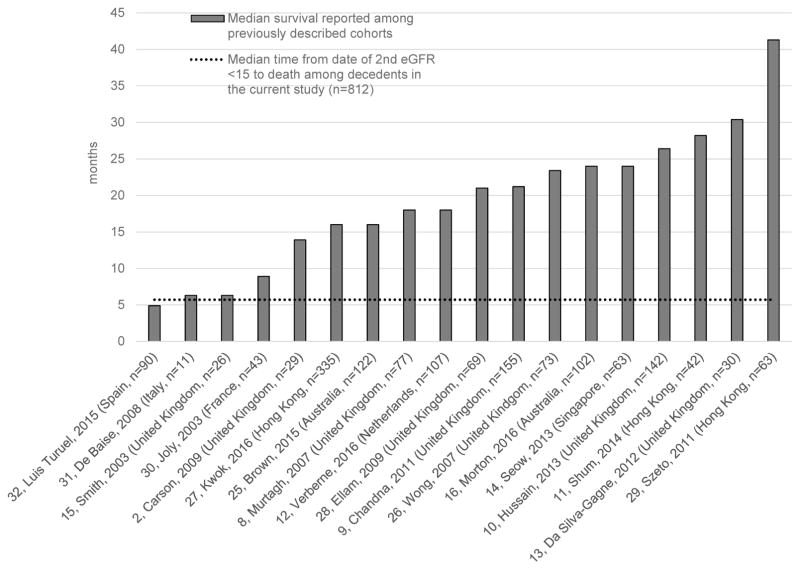
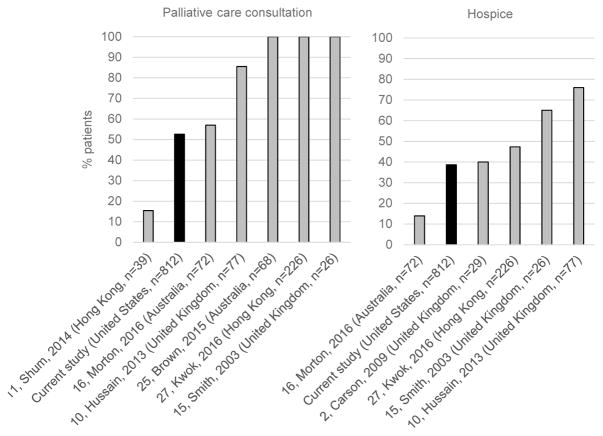
In other countries with established conservative care pathways for patients with advanced CKD, the decision not to pursue dialysis tends to be a proactive choice to enter a multidisciplinary supportive care program that integrates palliative care and hospice services early in the course of advanced CKD.2,8–10,13,15,24–27 In the current study, median time from date of the second eGFR <15ml/min/1.73m2 to death among patients in whom there had been a decision not to pursue dialysis was only 5.7 months and is considerably shorter than the median survival reported for most conservatively managed cohorts described in the literature (4.9–30.4 months) (Figure 3),2,8–16,25–32 likely reflecting that this decision occurred among patients with an extremely poor prognosis and/or relatively late in their illness trajectory. While some patients in the current study did decide not to pursue dialysis (or their family members and/or providers made this decision for them) prior to death, it is noteworthy that the frequency of palliative care consultation (52.6%) and hospice use (38.7%) among these patients were far lower than for most conservatively managed cohorts previously described in the literature (Figure 4).2,10,11,15,16,25,27 Levels of healthcare intensity near the end of life were also quite high for patients in our study for whom there had been a decision not to pursue dialysis prior to death; most (57.3%) were hospitalized during their final month of life, and half spent more than a third of their last month of life in the hospital. Most likely, these findings suggest that the transition to palliative care and hospice services for patients in whom there was a decision not to pursue dialysis tended to occur only after an initial trial of more aggressive care near the end of life.
Figure 3. Survival among patients in whom there was a decision not to pursue maintenance dialysis reported in the literature.
(the dashed line indicates median time from date of second eGFR <15ml/min/1.73m2 to death among decedents for whom there was a decision not to pursue dialysis in the current study; data limited to studies published in English; studies are indicated by following: reference number, first author, year of publication (country, study size)).
Figure 4. Utilization of palliative care consultation and hospice services among patients for whom there was a decision not to pursue maintenance dialysis prior to death.
(data limited to studies published in English; studies are indicated by following: reference number, first author, year of publication (country, total number of decedents)).
The VA is the largest integrated healthcare system in the United States and affords a unique window on the care of patients with advanced CKD not treated with dialysis—a group not captured in national registry data. Nevertheless, our results must be interpreted with the following considerations in mind. First, findings may not be generalizable to nonveterans, women, and other groups not well represented in the VA. Second, we relied solely on the VA electronic medical record to assign treatment status, leaving open the possibility for misclassification among patients who were receiving care outside the VA. Because their treatment status was known, we also did not review the medical records for the large majority of patients treated with dialysis. Third, the medical record and administrative data provide only limited insight into patients’ treatment preferences, their experience of the decision-making process for dialysis and the quality of end-of-life care. Fourth, categorization of patients in the current study was based on the most recent documented treatment plan in the medical record at the time of death, which enabled us to distinguish those for whom there had been a decision not to pursue dialysis and those who did not receive dialysis but were discussing and/or preparing for it prior to death. This may limit literature comparisons because most prior studies followed up patients prospectively from the time of their initial documentation of treatment preference and consequently included large numbers (15.2%–72.1%) of patients in the dialysis group who did not go on to initiate dialysis during follow-up as well as a smaller number of patients who elected for conservative treatment but went on to initiate dialysis.8–12,15,16 Both methods of categorization miss some of the complexity of decision-making for dialysis in which patients’ treatment preferences can change over time.17,19 Last but not least, the results of this retrospective review is limited to decedents and cannot support inferences about prognosis or downstream care for patients approaching decisions about dialysis.
In this national sample of veterans with advanced CKD who died during the period 2000–2011, those not treated with dialysis prior to death—especially those for whom there had been a decision not to pursue dialysis—received less intensive patterns of end-of-life care than those treated with dialysis. Conversely, utilization of palliative care and hospice services seemed to be strongly tied to the decision not to pursue dialysis and, as compared with reports from conservatively managed cohorts outside the United States, seemed to have occurred in a less proactive fashion among relatively sicker patients and/or later in the course of illness. Collectively, our findings highlight opportunities for better integration of hospice and palliative care services into contemporary models of care for patients with advanced CKD.
Acknowledgments
Support: This work was supported by grants from National Institutes of Health (1K23DK107799-01A1, principal investigator [PI] Wong) and the VA Health Services Research and Development (IIR 09-094, PI Hebert; and IIR 12-126, PI O’Hare). The funding organizations had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review, or approval of the manuscript.
We thank Jeffrey Todd-Stenberg for his assistance with data programming, and Christine Sulc and Whitney Showalter for their assistance with study coordination.
Footnotes
Authors’ Contributions: Research idea and study design: SPYW; data acquisition: SPYW, MKY, C-FL, PLH, AMO; data analysis/interpretation: SPYW, MKY, PKG, C-FL, PLH, AMO; statistical analysis: SPYW, PKG, AMO; supervision or mentorship: AMO. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Financial Disclosure: AMO receives royalties from UpToDate. The other authors declare that they have no other relevant financial interests.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position or policy of the VA.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Susan P. Y. Wong, Assistant Professor of Medicine, Health Service Research and Development Center of Innovation, VA Puget Sound Health Care System, Department of Medicine, University of Washington, 1660 S. Columbian Way, Building 100, Renal Dialysis Unit, Seattle, WA 98108
Margaret K. Yu, Clinical Assistant Professor of Medicine, Department of Medicine, Stanford University
Pamela K. Green, Research Health Science Specialist, Health Service Research and Development Center of Innovation, VA Puget Sound Health Care System
Chuan-Fen Liu, Research Professor, Health Service Research and Development Center of Innovation, VA Puget Sound Health Care System, Department of Health Services, University of Washington
Paul L. Hebert, Research Associate Professor, Health Service Research and Development Center of Innovation, VA Puget Sound Health Care System, Department of Health Services, University of Washington
Ann M. O’Hare, Professor of Medicine, Department of Medicine, VA Puget Sound Healthcare System and University of Washington
References
- 1.Wong SP, Kreuter W, O’Hare AM. Healthcare intensity at initiation of chronic dialysis among older adults. J Am Soc Nephrol. 2014;25(1):143–9. doi: 10.1681/ASN.2013050491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carson RC, Juszczak M, Davenport A, Burns A. Is maximum conservative management an equivalent treatment option to dialysis for elderly patients with significant comorbid disease? Clin J Am Soc Nephrol. 2009;4(10):1611–9. doi: 10.2215/CJN.00510109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Purnell TS, Auguste P, Crews DC, et al. Comparison of life participation activities among adults treated by hemodialysis, peritoneal dialysis and kidney transplantation: a systematic review. Am J Kidney Dis. 2013;62(5):953–73. doi: 10.1053/j.ajkd.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jassal SV, Chui E, Hiadunewich M. Loss of independence in patients starting dialysis at 80 years of age and older. N Engl J Med. 2009;361(16):1612–3. doi: 10.1056/NEJMc0905289. [DOI] [PubMed] [Google Scholar]
- 5.Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE. Functional status of elderly adults before and after initiation of dialysis. N Engl J Med. 2009;361(16):1539–47. doi: 10.1056/NEJMoa0904655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abdel-Kader K, Unruh ML, Weisbord SD. Symptom burden, depression, and quality of life in chronic and end-stage kidney disease. Clin J Am Soc Nephrol. 2009;4(6):1057–64. doi: 10.2215/CJN.00430109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rivara MB, Robinson-Cohen C, Kestenbaum B, et al. Changes in symptom burden and physical performance with initiation of dialysis in patients with chronic kidney disease. Hemodial Int. 2015;19(1):147–50. doi: 10.1111/hdi.12244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murtagh FE, Marsh JE, Donohoe P, Ekbal NJ, Sheerin NS, Harris FE. Dialysis or not? A comparative survival study of patients over 75 years with chronic kidney disease stage 5. Nephrol Dial Transplant. 2007;22(7):1955–62. doi: 10.1093/ndt/gfm153. [DOI] [PubMed] [Google Scholar]
- 9.Chandna SM, Da Silva-Gane M, Marshall C, Warwicker P, Greenwood RN, Farrington K. Survival of elderly patients with stage 5 CKD: comparison of conservative management and renal replacement therapy. Nephrol Dial Transplant. 2011;26(5):1608–14. doi: 10.1093/ndt/gfq630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hussain JA, Mooney A, Russon L. Comparison of survival analysis and palliative care involvement in patients aged over 70 years choosing conservative management or renal replacement therapy in advanced chronic kidney disease. Palliat Med. 2013;27(9):829–939. doi: 10.1177/0269216313484380. [DOI] [PubMed] [Google Scholar]
- 11.Shum CK, Tam KF, Chak WL, Chan TC, Mak YF, Chau KF. Outcomes in older adults with stage 5 chronic kidney disease: comparison of peritoneal dialysis and conservative management. J Gerontol A Biol Sci Med Sci. 2014;69(3):308–14. doi: 10.1093/gerona/glt098. [DOI] [PubMed] [Google Scholar]
- 12.Verberne WR, Tom Geers ABM, Jellea WT, Vincent HH, van Delden JJM, Bos WJW. Comparative survival among older adults with advanced kidney disease managed conservatively versus with dialysis. Clin J Am Soc Nephrol. 2016;11(4):633–40. doi: 10.2215/CJN.07510715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Da Silva-Gane M, Wellsted D, Greenshields H, Norton S, Chandna SM, Farrington K. Quality of life and survival in patients with advanced kidney failure managed conservatively or by dialysis. Clin J Am Soc Nephrol. 2012;7(12):2002–9. doi: 10.2215/CJN.01130112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seow YY, Cheung YB, Qu LM, Yee ACP. Trajectory of quality of life for poor prognosis stage 5D chronic kidney disease with and without dialysis. Am J Nephrol. 2013;37(3):231–8. doi: 10.1159/000347220. [DOI] [PubMed] [Google Scholar]
- 15.Smith C, Da Silva-Gane M, Chandna S, Warwicker P, Greenwood R, Farrington K. Choosing not to dialyse: evaluation of planned non-dialytic management in a cohort of patients with end-stage renal failure. Nephron Clin Pract. 2003;95(2):c40–6. doi: 10.1159/000073708. [DOI] [PubMed] [Google Scholar]
- 16.Morton RL, Webster AC, McGeechan K, et al. Conservative management and end of life care in an Australian cohort with ESRD. Clin J Am Soc Nephrol. 2016;11(12):2195–2203. doi: 10.2215/CJN.11861115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong SP, Hebert PL, Laundry RJ, et al. Decisions about renal replacement therapy in patients with advanced kidney disease in the US Department of Veterans Affairs, 2000–2011. Clin Am J Soc Nephrol. 2016;11(10):1825–33. doi: 10.2215/CJN.03760416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaufman SR, Shim JK, Russ AJ. Old age, life extension and the character of medical choice. J Gerontol B Psychol Sci Soc Sci. 2006;61(4):S175–84. doi: 10.1093/geronb/61.4.s175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Song MK, Lin FC, Gilet CA, Arnold RM, Bridgman JC, Ward SE. Patient perspectives on informed decision-making surrounding dialysis initiation. Nephrol Dial Transplant. 2013;28(11):2815–23. doi: 10.1093/ndt/gft238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong SP, Vig EK, Taylor JS, et al. Timing of initiation of maintenance dialysis: a qualitative analysis of the electronic medical records of a national cohort of patients form the Department of Veterans Affairs. JAMA Intern Med. 2016;176(2):228–35. doi: 10.1001/jamainternmed.2015.7412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol. 2011;64(7):749–59. doi: 10.1016/j.jclinepi.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.USRDS. 2016 Annual Data Report, Atlas of End Stage Renal Disease in the United States. Bethesda, Md: National Institutes of Health, National Institutes of Diabetes and Digestive and Kidney Diseases; Jun, [Google Scholar]
- 23.Grubbs V, Moss AH, Cohen LM, et al. Dialysis Advisory Group of the American Society of Nephrology. A palliative approach to dialysis care: A patient-centered transition to the end of life. Clin J Am Soc Nephrol. 2014;9(12):2203–9. doi: 10.2215/CJN.00650114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okamato I, Tonkin-Crine S, Rayner H, et al. Conservative care for ESRD in the United Kingdom: a national survey. Clin J Am Soc Nephrol. 2015;10(1):120–6. doi: 10.2215/CJN.05000514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brown MA, Collett GK, Josland EA, Foote C, Li Q, Brennan FP. CKD in elderly patients managed without dialysis: survival, symptoms and quality of life. Clin J Am Soc Nephrol. 2015;10(2):260–8. doi: 10.2215/CJN.03330414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wong CF, McCarthy M, Howse MLP, Williams PS. Factors affecting survival in advanced chronic kidney disease patients who choose not to receive dialysis. Ren Fail. 2007;29(6):653–9. doi: 10.1080/08860220701459634. [DOI] [PubMed] [Google Scholar]
- 27.Kwok AO, Yuen SK, Yong DS, Tse DM. The symptoms prevalence, medical interventions and health care service needs for patients with end-stage renal disease in a renal palliative care program. Am J Hosp Palliat Care. 2016;33(10):952–8. doi: 10.1177/1049909115598930. [DOI] [PubMed] [Google Scholar]
- 28.Ellam T, El-Kossi M, Prasanth KC, El-Nahas M, Khwaja A. Conservatively managed patients with stage 5 chronic kidney disease--outcomes from a single center experience. Q J Med. 2009;102(8):547–54. doi: 10.1093/qjmed/hcp068. [DOI] [PubMed] [Google Scholar]
- 29.Szeto CC, Kwan BC, Chow KM, et al. Life expectancy of Chinese patients with chronic kidney disease without dialysis. Nephrology (Carlton) 2011;16(8):715–9. doi: 10.1111/j.1440-1797.2011.01504.x. [DOI] [PubMed] [Google Scholar]
- 30.Joly D, Alnglicheau D, Alberti C, et al. Octogenerians reaching end-stage renal disease: cohort study of decisions-making and clinical outcomes. J Am Soc Nephrol. 2003;14(4):12–21. doi: 10.1097/01.asn.0000054493.04151.80. [DOI] [PubMed] [Google Scholar]
- 31.De Baise V, Tobaldini O, Coaretti C, et al. Prolonged conservative treatment for frail elderly patients with end-stage renal disease: the Verona experience. Nephrol Dial Transplant. 2008;23(4):1313–7. doi: 10.1093/ndt/gfm772. [DOI] [PubMed] [Google Scholar]
- 32.Luis Tereul J, Burguera Vion V, Gomis Couto A, et al. Choosing conservative therapy in chronic kidney disease. Nefrologia. 2015;35(3):273–9. doi: 10.1016/j.nefro.2015.05.005. [DOI] [PubMed] [Google Scholar]