Abstract
Background
As a marker of myocardial injury, troponin level correlates with adverse outcomes following myocardial infarction (MI). We hypothesized that patients with higher preoperative troponin level would have increased morbidity and mortality following CABG.
Methods
A total of 1,272 patients underwent urgent or emergent, isolated CABG and had preoperative troponin measurements at our institution (2002–2016). Logistic regression assessed the risk-adjusted impact of peak troponin level on morbidity and mortality. Long-term survival analysis was performed with Kaplan-Meier and Cox Proportional Hazards models.
Results
A total of 835 (65.6%) of patients had a positive preoperative troponin. The median peak troponin for this group was 3.2ng/mL [IQR;0.6-11.9] with a median time from peak troponin to surgery of 3 days (IQR;1-4). Positive troponin was associated with more significant comorbid conditions and more extensive coronary artery disease. Operative mortality (3.7 vs 1.1%, p=0.009), major morbidty (11.7 vs. 3.9%, p<0.001) and long-term mortality (median survival 12.5 vs. 13.6 years, p=0.01) were increased in the positive troponin group. After risk adjustment, positive troponin was not independently associated with increased operative mortality (OR 2.61; p=0.053). In both adjusted and unadjusted analysis, the peak preoperative troponin level did not independently predict mortality at any time point (all OR 1.0 and p>0.05).
Conclusions
While a positive preoperative troponin correlates with worse outcomes following CABG, risk adjustment eliminates much of the short term predictive value of this biomarker. Peak troponin level does not influence outcomes following CABG and is a poor predictor of events when STS predictive models are used.
Classifications: Cardiac Surgery, Coronary Artery Bypass Grafting, Troponin, Myocardial Infarction
Cardiac enzyme elevation is a surrogate for myocardial ischemia and cardiac specific troponin is important in the definition and diagnosis of myocardial infarction (MI) (1,2). Prior studies have shown that troponin level correlates with degree of myocardial injury and predicts adverse outcomes following myocardial infarction (1, 3–6). It is well established that acute preoperative MI increases the risk of adverse outcomes following coronary artery bypass grafting (CABG) and the optimal timing between MI and CABG has been debated (7,8). Although many surgeons consider the level of troponin elevation in operative timing decisions, the prognostic implications of troponin level prior to CABG remains unknown.
The Society for Thoracic Surgeons (STS) preoperative risk calculator is a highly accurate risk model that predicts both short-term mortality and postoperative complications. The STS risk calculation includes presence of acute MI, timing from MI to surgery, and the presence of a ST-segment elevation myocardial infarction (STEMI) versus non ST-segment myocardial infarction (NSTEMI). However, the degree of troponin elevation is not included in the assessment. Previously, the effect of positive troponin on outcomes has been evaluated, with the majority of studies demonstrating elevated risk of postoperative adverse events in patients an elevated troponin preoperatively (9,10,11–15). This is consistent whether CABG was performed as an elective operation or after presentation with an acute coronary syndrome (ACS). However, these studies have been limited by bias due to the inherent differences in baseline risk of patients who have preoperative positive troponin. Additionally, the implication of the peak level is less well established, and there is a lack of consensus as to its ability to predict postoperative morbidity or mortality.
In this study, we sought to determine if the level of the preoperative troponin is an independent risk factor for morbidity and mortality in a large cohort of patients who undergo CABG after presentation with ACS. Given that the preoperative troponin level is not included in preoperative risk assessments, we hypothesize that the level of this biomarker is an unaccounted risk factor in current STS risk models.
Patients and Methods
Patient Data
All patients who underwent urgent or emergent CABG at our institution between January 2002 and February 2016 were extracted from an institutional STS database. Exclusion criteria included missing troponin data and elective CABG. Preoperative troponin values were obtained via the institutional Clinical Data Repository (CDR). The peak preoperative troponin was measured using troponin I assays. Preoperative characteristics, intraoperative variables and postoperative outcomes were prospectively collected within the STS database. Long-term survival status was collected from the CDR, which obtains data from the Commonwealth of Virginia Department of Health. This study was approved by the University of Virginia Institutional Review Board (IRB) with a waiver of informed consent (IRB Protocol #19247).
Patients were stratified by positive preoperative troponin, defined as (troponin <0.08ng/mL vs. troponin ≥0.08ng/mL). The primary outcome of interest was operative mortality defined as in-hospital or 30-day mortality. Secondary outcomes included STS major morbidity and mortality (permanent stroke, renal failure, reoperation, deep sternal wound infection and prolonged ventilation). Standard STS definitions were used for all variables (16).
Statistical Analysis
Continuous variables are presented as median [interquartile range (IQR)] due to skewdness and categorical variables as count (percentage). For univariate comparisons continuous variables were analyzed by Mann-Whitney U test and for categorical variables by Chi-Square test. Multivariable logistic regression was used to analyze associations between preoperative troponin levels and outcomes of interest. Risk adjustment was performed using STS Predicted Risk of Mortality (PROM) and STS Predicted risk of Mortality or Morbidity (PROMM). Additionally, year was included to account for changing practices over time. To evaluate long-term survival, patients were stratified by positive troponin level for Kaplan-Meier survival analysis. Finally, risk adjusted long-term survival was performed using Cox Proportional Hazards with risk-adjustment performed using PROM and year. SAS version 9.4 (SAS Institute, Cary, NC) statistical software was used for analysis with a statistical threshold 0.05 set for significance.
Results
Baseline Characteristics
A total of 3,855 patients underwent isolated CABG during the study period at our institution. Of these, 1,357 had preoperative troponin levels available and of these, an additional 85 patients were excluded due to elective status. This resulted in 1,272 patients included in the final analysis who had undergone urgent or emergent isolated CABG during the study period and had preoperative troponin measurements available. Of which 835 (65.6%) had preoperative positive troponin (Table 1). The preoperative positive troponin group had a median peak of 3.2ng/mL [0.6-11.9]. Those with a preoperative positive troponin were more likely to have a history of previous myocardial infarction (63.1 vs. 31.1%, p<0.001) and a diagnosis of heart failure (35.8 vs. 15.6%, p<0.001). There was no significant difference between groups with respect to prior revascularization either with CABG (1.8 vs. 2.1%, p=0.743) or PCI (21.2 vs. 23.3%, p=0.380). The preoperative positive troponin group had an increased risk profile represented by both their STS PROM (1.9% vs. 1.1%, p<0.001) and their STS PROMM (16% vs. 10.9%, p<0.001).
Table 1.
Baseline Characteristics of patients with positive and negative troponin
| Troponin <0.08ng/mL | Troponin >0.08ng/mL | p-value | |
|---|---|---|---|
| Total | 437 (34.4%) | 835 (65.6%) | – |
| Age | 65 [57 – 73] | 65 [57 – 73] | 0. 34 9 |
| BMI | 29.1 [25. 3 – 32. 8] | 28.5 [25.4 – 33.2] | 0. 864 |
| EF | 57 [4 9 – 63] | 47 [3 7 – 5 8] | <0.001 |
| Female | 132 (30.2 %) | 228 (27.3%) | 0. 278 |
| Smoker | 40 (9.2 %) | 75 (9.0 %) | 0.92 0 |
| Heart Failure | 68 (15.6 %) | 299 (35.8%) | <0.001 |
| Hypertension | 354 (8 1 %) | 667 (79.9 %) | 0. 632 |
| DM | 185 (42. 3 %) | 383 (45. 9 %) | 0.2 29 |
| Chronic Lung Disease Moderate/Severe | 4 2 (9. 6 %) | 8 2 (9.8%) | 0.905 |
| Dialysis | 6 (1. 4 %) | 3 8 (4. 6 %) | 0.003 |
| Peripheral Arterial Disease | 68 (1 5. 6%) | 153 (18.3%) | 0.2 17 |
| Cerebral Vascular Disease | 78 (17.9 %) | 158 (1 8.9 %) | 0. 640 |
| Prior CVA | 29 (6.6 %) | 72 (8. 6 %) | 0. 213 |
| History of Prior MI | 136 (31 .1 %) | 527 (6 3.1 %) | <0.001 |
| Timing of Acute MI | <0.001 | ||
| 6h-24hr | 4 (0. 9 %) | 21 (2. 5 %) | |
| MI 1d-7d | 85 (19.5%) | 720 (8 6.2 %) | |
| MI 8-21 | 1 0 (2. 3 %) | 3 4 (4. 1 %) | |
| >21 | 121 (2 7.7 %) | 2 4 (2.9 %) | |
| Unknown timing | 0 (0 %) | 36 (4. 3 %) | |
| No recent acute MI | 217 (49.7%) | 0 (0%) | |
| Previous CABG | 9 (2. 1 %) | 15 (1. 8 %) | 0. 7433 |
| Prior PCI | 102 (2 3 .3%) | 177 (21. 2 %) | 0. 380 |
| Reoperation | 83 (1 9 %) | 103 (12. 3 %) | 0.001 |
| Preoperative IABP | 48 (1 1 %) | 161 (19. 3 %) | <0.001 |
| Peak Preoperative Troponin | 0.02 [0.02 – 0.06] | 3. 2 [0.6 – 11.9] | <0.001 |
| PROM | 1. 1 % [0.7 – 2.4] | 1.9% [1 – 4.4] | <0.001 |
| PROMM | 10.9 [7.9 – 18. 2] | 16. 0 % [10. 3 – 29. 7] | <0.001 |
n (%); median [IQR]
Operative Variables
The time from admission to surgery (3 vs. 3 days, p=0.178) was similar between groups (Table 2). Those with preoperative positive troponin were more likely to have three-vessel disease as compared to two- or one-vessel disease (3-vessel 77.6 vs. 71.2%, 2-vessel 19.4 vs. 25.6%, 1-vessel 3.0 vs. 3.2%, p=0.034). Operations on those with preoperative positive troponin required both longer cardiopulmonary bypass time (93 vs. 88 minutes, p<0.001) and longer cross clamp times (72 vs. 67 minutes, p<0.001).
Table 2.
Operative Variables
| Troponin <0.08ng/mL | Troponin <0.08ng/mL | p-value | |
|---|---|---|---|
| Days from Peak to Surgery | 2 [1 – 4] | 3 [1 – 4] | 0.1 70 |
| LOS Admission to Surgery | 3 [2 – 5] | 3 [2 – 5] | 0. 178 |
| Number of Diseased Vessels | 0.03 4 | ||
| 1-vessel | 14 (3.2 %) | 25 (3.0%) | |
| 2-vessel | 11 2 (2 5.6 %) | 162 (19.4 %) | |
| 3-vessel | 311 (71. 2 %) | 648 (77. 6 %) | |
| CPB Time | 88 [70 – 108] | 93 [75 – 11 6] | <0.001 |
| CC Time | 67 [52 – 86] | 7 2 [5 7 – 8 9] | 0.0 15 |
n (%); median [IQR]
Morbidity and Mortality
Postoperative adverse outcomes were significantly higher in the preoperative positive troponin group including operative mortality (3.7% vs. 1.1%, p=0.009) and major morbidity (11.4% vs. 4.3%, p=0.001; Table 3). One-year and five-year mortality was 11.4% vs. 4.3% (p=0.001) and 36.9% vs. 24.6% (p=0.006) respectively. Individual postoperative complications including post-operative atrial fibrillation (21.6% vs. 15.8%, p=0.014), cardiac arrest (3.1% vs. 0.9%, p=0.014), and pneumonia (4.4% vs. 1.4%, p=0.004) were all increased in the positive preoperative troponin group. These patients required more time in the intensive care unit (46 hours [24-88 hours] vs. 28 hours [22-60 hours], p<0.001) and greater number of hospital days post-operatively (6 days [5-8 days] vs. 5 days [4-6 days], p<0.001).
Table 3.
Outcomes of patients with positive and negative troponin
| Troponin <0.08ng/mL | Troponin <0.08ng/mL | p-value | |
|---|---|---|---|
| Operative Mortality | 5 (1.1%) | 31 (3. 7 %) | 0.009 |
| 1-year mortality | 1 2 (4.3 %) | 57 (11.4 %) | 0.001 |
| 5-year mortality | 42 (2 4.6 %) | 11 7 (3 6 .9%) | 0.0 06 |
| Major Morbidity | 17 (3.9 %) | 98 (11. 7 %) | <0.001 |
| Stroke | 5 (1.1%) | 21 (2. 5 %) | 0. 101 |
| Atrial Fibrillation | 69 (1 5.8 %) | 180 (21. 6 %) | 0.014 |
| Cardiac Arrest | 4 (0.9 %) | 26 (3 .1 %) | 0.014 |
| Pneumonia | 6 (1. 4 %) | 3 7 (4. 4 %) | 0.00 4 |
| Renal Failure | 6 (1. 4 %) | 49 (5.9%) | <0.001 |
| Need for Dialysis | 5 (1.1%) | 3 4 (4 .1 %) | 0.004 |
| DSWI | 0 | 1 (0.1%) | 0.4 69 |
| Reoperation Any Reason | 1 1 (2.5%) | 4 7 (5. 6 %) | 0.01 2 |
| Reoperation for Bleeding | 8 (1. 8 %) | 2 5 (3%) | 0.2 25 |
| LOS Surgery to Discharge | 5 [4 - 6] | 6 [5 – 8] | <0.001 |
| Total Hours in ICU | 2 7.5 [22 - 6 0] | 45.8 [24 – 88] | <0.001 |
| Discharge to Facility | 75 (17. 2 %) | 182 (2 1.8 %) | 0.0 51 |
n (%); median [IQR]
Risk Analysis
By regression analysis a positive troponin was correlated with operative and 1-year mortality as well as morbidity/mortality (Table 4). Additionally, median long-term survival was decreased in the preoperative positive troponin group (12.5 years vs. 13.6 years, p=0.01; Figure 1). After risk adjustment, however, a significant association between positive troponin and operative mortality no longer reaches statistical significance (OR 2.61, p=0.053), although it continues to independently predict increased odds of 1-year mortality (OR 2.59, p=0.007), morbidity/mortality (OR 2.26, p=0.001) and long term mortality (HR 1.37, p=0.028).
Table 4.
Positive Troponin and Risk for Adverse Outcomes
| Unadjusted | Risk Adjusted | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | |||
| Operative | ||||||||
| Mortality | 3.33 | 1. 29 | 8.63 | 0.013 | 2. 61 | 0. 99 | 6. 89 | 0. 053 |
| Morbidity or Mortality | 3.34 | 2.02 | 5.51 | <0.001 | 2. 51 | 1. 50 | 4.22 | 0.001 |
| 1 - year mortality | 2.84 | 1. 50 | 5.39 | 0.001 | 2. 33 | 1.2 0 | 4.52 | 0.012 |
| Long - term mortality | 1. 44 | 1.09 | 1. 90 | 0.011 | 1. 37 | 1.03 | 1. 83 | 0.028 |
Figure 1.
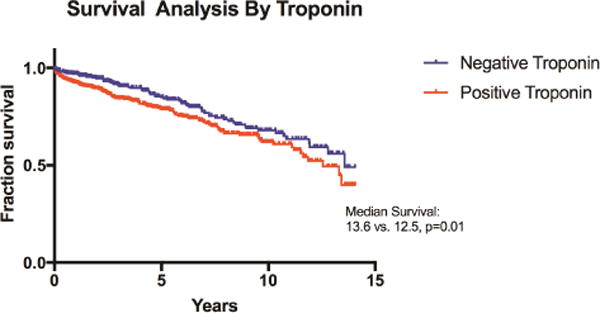
Kaplan-Meier Curves for long-term survival by positive and negative troponin.
As a continuous variable, the peak preoperative troponin level was not associated with a significantly increased risk of operative mortality (OR 1.00 per 1ng/mL rise, p=0.218), 1-year mortality (OR 1.00 per 1ng/mL rise, p=0.113) or long-term mortality (HR 1.00 per 1ng/mL rise, p=0.447), but was associated with morbidity/mortality (OR 1.01 per 1ng/mL rise, p=0.003; Table 5). After risk adjustment, troponin level continued to not be a predictor of operative mortality, one-year mortality, or long-term mortality, and was no longer a significant predictor of morbidity/mortality (OR 1.00, p=0.172).
Table 5.
Peak Troponin level and Risk for Adverse Outcomes
| Unadjusted | Risk Adjusted | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p - value | OR | 95% CI | p - value | |||
| Operative | ||||||||
| Mortality | 1.0 0 | 1.00 | 1.01 | 0. 218 | 1.00 | 1.00 | 1.01 | 0. 420 |
| Morbidity or Mortality | 1.01 | 1.00 | 1.01 | 0.003 | 1.00 | 1.00 | 1.01 | 0.1 72 |
| 1 - year mortality | 1.0 0 | 1.00 | 1.01 | 0. 113 | 1.00 | 1.00 | 1.01 | 0. 312 |
| Long - term mortality | 1.00 | 1.00 | 1.00 | 0.4 47 | 1.00 | 1.00 | 1.00 | 0. 788 |
Comment
We analyzed all patients at a quaternary care academic medical center that underwent urgent or emergent CABG and had preoperative troponin levels analyzed, of which 66% had a positive preoperative troponin. This cohort, with positive preoperative biomarkers, had a greater burden of comorbid conditions, more complex disease, and an increased rate of postoperative adverse events including early and late mortality. However, contrary to our primary hypothesis, the level of the peak preoperative troponin did not demonstrate independent predictive ability with regard to postoperative adverse events or long-term survival. Further, although a positive preoperative troponin predicted mortality and adverse events, after risk adjustment, a positive troponin was no longer an independent risk factor for operative mortality.
Elevated troponin levels have a strong association with adverse outcomes in coronary artery disease (1,4–6,17). In patients referred for surgical revascularization with CABG, preoperative positive troponin has been demonstrated to predict short-term adverse events (10,12) and operative mortality (9,11,13,14). In elective CABG operations, a positive troponin is associated with increased operative mortality, MACE, cardiac arrest, reoperation and length of ICU and hospital stays (9,10). Similarly, in non-elective CABG, 30-day mortality, major postoperative complications, postoperative length of stay is increased in the positive troponin cohorts (11–13). These studies utilized troponin cutoff levels that have ranged from 0.02ng/mL to 0.15ng/mL, depending on institutional laboratory definitions. Our results are consistent with the majority of retrospective studies and demonstrate an association between preoperative positive troponin and short-term mortality and morbidity. No prior study has utilized the STS PROM to risk adjust. A study by Petaja and colleagues did risk adjust with a validated model (Euroscore II) and found no additional predictive benefit of positive preoperative troponin to predict mortality in patients who underwent CABG (15). Given that presentation with myocardial infarction is included in the STS risk model, one would expect that a significant portion of the risk attributable to this clinical characteristic is accounted for in the model – which is consistent with the present analysis. Our study confirms that although preoperative positive troponin is a marker for increased postoperative mortality and morbidity there is little additional predictive utility of this biomarker above and beyond the STS risk model.
In addition to early postoperative events, positive preoperative troponin has been utilized as a predictive marker for mid- and long-term outcomes. Although there have been fewer reports of the impact of preoperative biomarkers on long term outcomes, the trends in longer-term follow-up appear to mirror those of short-term mortality – preoperative positive troponin portends a worse survival (11,12). Paparella et. al. previously showed that at six months, the mortality rate was increased (13% vs. 4%) in patients who had a positive preoperative troponin (12). In a similar study of isolated CABG, a positive preoperative troponin was associated with a five times increased odds of two-year mortality (11). We found a modest decrease in life expectancy for those with preoperative positive troponin with a 1-year decrease in overall life expectancy. In unadjusted analyses, operative, 1-year and long term mortality was associated with a positive preoperative troponin. However, in adjusted analysis the predictive power of positive troponin was not a significant predictor for operative mortality, but significance persisted for 1-year and long term mortality. This can be accounted for by the fact that we used STS PROM to risk adjust, and although PROM has been demonstrated to predict long term survival, the model is not well calibrated to do so, with decreased discriminatory power at longer follow up (18).
There is less clarity regarding the impact that the exact troponin level may have on outcomes, and its usefulness for risk stratification prior to CABG. Previous studies have analyzed the preoperative troponin level as both a continuous variable and in tiered groups and the preoperative troponin level has been found to correlate with increased morbidity and mortality (10,13,19). However, these studies were either performed in elective CABG populations or CABG after STEMI. In other analyses of non-elective revascularizations, the relationship between preoperative troponin level and mortality is not as clear. In a study of patients with acute myocardial infarction operated on within 21 days, the troponin level itself failed to predict 6-month mortality, despite increased mortality in those with positive biomarkers compared to those with negative biomarkers (12). Similarly, in a subgroup of patients presenting with NSTEMI who underwent revascularization with CABG, preoperative troponin levels did not correlate with rates of 2-year mortality (20). Our population was designed to include only those who underwent urgent or emergent operations, thus excluding elective case for which incremental increase in troponin level is known to correlate with adverse outcomes. In our cohort, the preoperative peak troponin level was not associated with either mortality or major morbidity in adjusted analyses. These results are consistent with previous studies and suggest the preoperative troponin level does not predict postoperative outcomes outside of the elective setting or those with STEMI.
While troponin level should not influence timing of CABG, the timing of surgery relative to MI diagnosis is included in the STS model and predicts postoperative morbidity and mortality (16). Approximately 30% of patients with NSTEMI that ultimately require CABG will undergo revascularization within 48 hours of admission (21). Several studies have demonstrated a higher risk of postoperative adverse outcomes in patients operated on soon after acute myocardial infarction (7,19,22). Although many analyses have suggested high complication rates in early surgery, there is a higher risk profile for those who undergo early revascularization, which is unaccounted for in a majority of studies (23). However, the decision to delay CABG must be weighed with the potential for ongoing ischemia or re-infarction. The ideal timing of CABG is yet to be elucidated, but current data suggests that it is safe, and likely beneficial, to allow for a waiting period of at least 6-48 hours prior to revascularization (7,24). Nevertheless, this correlation between early revascularization and increased mortality is not consistent in all studies. In fact, in an analysis specifically aimed at evaluating the risk of early vs. late (<48 hours post MI vs. >48 hours post MI) surgical revascularization after NSTEMI, no mortality difference was found (21). Similarly, there was no significant difference in 6 month mortality when patients were stratified based on whether they were operated on one, two and three weeks after NSTEMI (12).
This study is limited in its design by its retrospective nature that results in some element of selection bias. Additionally, this is a single institution study that may not be generalizable to all institutions. Further, the designation of urgent CABG includes a wide range of diagnoses and the limitations of the STS database prevent identification of the specific reason for labeling an operation as urgent. The negative troponin cohort may include a heterogeneous population as the urgent and emergent STS definitions can apply to a wide variety of indications, including high risk coronary lesions, unstable angina, or heart failure. Finally, because laboratory values were only collected from patients at our institution, troponin levels drawn prior to transfer were not captured in this dataset. However, sub-analyses excluding patients that were transferred from outside hospitals or had an unknown transfer status demonstrated similar results.
In conclusion, a positive preoperative troponin predicts adverse outcomes in urgent or emergent CABG patients. After risk adjustment with STS PROM, the short term mortality risk attributable to a positive preoperative troponin is largely accounted for. Importantly, and in contrast to our hypothesis, the peak preoperative troponin level does not provide independent predictive value in urgent or emergent CABG. Therefore, the level of peak preoperative troponin may not be critical in operative planning or risk assessment for CABG.
Abbreviations
- MI
Myocardial Infarction
- CABG
Coronary artery bypass grafting
- STS
Society for Thoracic Surgeons
- STEMI
ST-segment myocardial infarction
- NSTEMI
Non-ST segment myocardial infarction
- ACS
Acute Coronary syndrome
- PROM
Predicted Risk of Mortality
- PROMM
Predicted risk of Mortality or Morbidity
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Anderson JL, Adams CD, Antman EM, et al. 2011 ACCF/AHA Focused Update Incorporated Into the ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;123(18):e426–579. doi: 10.1161/CIR.0b013e318212bb8b. [DOI] [PubMed] [Google Scholar]
- 2.Brush JE, Jr, Kaul S, Krumholz HM. Troponin Testing for Clinicians. Journal of the American College of Cardiology. 2016;68(21):2365–2375. doi: 10.1016/j.jacc.2016.08.066. [DOI] [PubMed] [Google Scholar]
- 3.Antman EM, Tanasijevic MJ, Thompson B, et al. Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. The New England journal of medicine. 1996;335(18):1342–1349. doi: 10.1056/NEJM199610313351802. [DOI] [PubMed] [Google Scholar]
- 4.Giannitsis E, Muller-Bardorff M, Lehrke S, et al. Admission troponin T level predicts clinical outcomes, TIMI flow, and myocardial tissue perfusion after primary percutaneous intervention for acute ST-segment elevation myocardial infarction. Circulation. 2001;104(6):630–635. doi: 10.1161/hc3101.093863. [DOI] [PubMed] [Google Scholar]
- 5.Heidenreich PA, Alloggiamento T, Melsop K, McDonald KM, Go AS, Hlatky MA. The prognostic value of troponin in patients with non-ST elevation acute coronary syndromes: a meta-analysis. Journal of the American College of Cardiology. 2001;38(2):478–485. doi: 10.1016/s0735-1097(01)01388-2. [DOI] [PubMed] [Google Scholar]
- 6.Matetzky S, Sharir T, Domingo M, et al. Elevated troponin I level on admission is associated with adverse outcome of primary angioplasty in acute myocardial infarction. Circulation. 2000;102(14):1611–1616. doi: 10.1161/01.cir.102.14.1611. [DOI] [PubMed] [Google Scholar]
- 7.Lee DC, Oz MC, Weinberg AD, Lin SX, Ting W. Optimal timing of revascularization: transmural versus nontransmural acute myocardial infarction. The Annals of thoracic surgery. 2001;71(4):1197–1202. doi: 10.1016/s0003-4975(01)02425-0. discussion 1202–1194. [DOI] [PubMed] [Google Scholar]
- 8.Ngaage DL, Sogliani F, Tang A. Early and late prognostic implications of coronary artery bypass timing after myocardial infarction. European journal of cardio-thoracic surgery : official journal of the European Association for Cardiothoracic Surgery. 2013;43(3):549–554. doi: 10.1093/ejcts/ezs250. [DOI] [PubMed] [Google Scholar]
- 9.Buratto E, Conaglen P, Dimitriou J, et al. Predicting adverse outcomes in elective coronary artery bypass graft surgery using pre-operative troponin I levels. Heart, lung & circulation. 2014;23(8):711–716. doi: 10.1016/j.hlc.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 10.Carrier M, Pelletier LC, Martineau R, Pellerin M, Solymoss BC. In elective coronary artery bypass grafting, preoperative troponin T level predicts the risk of myocardial infarction. The Journal of thoracic and cardiovascular surgery. 1998;115(6):1328–1334. doi: 10.1016/S0022-5223(98)70216-8. [DOI] [PubMed] [Google Scholar]
- 11.Lyon WJ, Baker RA, Andrew MJ, Tirimacco R, White GH, Knight JL. Relationship between elevated preoperative troponin T and adverse outcomes following cardiac surgery. ANZ journal of surgery. 2003;73(1–2):40–44. doi: 10.1046/j.1445-2197.2003.02611.x. [DOI] [PubMed] [Google Scholar]
- 12.Paparella D, Scrascia G, Paramythiotis A, et al. Preoperative cardiac troponin I to assess midterm risks of coronary bypass grafting operations in patients with recent myocardial infarction. The Annals of thoracic surgery. 2010;89(3):696–702. doi: 10.1016/j.athoracsur.2009.11.072. [DOI] [PubMed] [Google Scholar]
- 13.Thielmann M, Massoudy P, Neuhauser M, et al. Risk stratification with cardiac troponin I in patients undergoing elective coronary artery bypass surgery. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2005;27(5):861–869. doi: 10.1016/j.ejcts.2005.01.043. [DOI] [PubMed] [Google Scholar]
- 14.Thielmann M, Massoudy P, Neuhauser M, et al. Prognostic value of preoperative cardiac troponin I in patients undergoing emergency coronary artery bypass surgery with non-ST-elevation or ST-elevation acute coronary syndromes. Circulation. 2006;114(1 Suppl):I448–453. doi: 10.1161/CIRCULATIONAHA.105.001057. [DOI] [PubMed] [Google Scholar]
- 15.Petaja L, Rosjo H, Mildh L, et al. Predictive value of high-sensitivity troponin T in addition to EuroSCORE II in cardiac surgery. Interactive cardiovascular and thoracic surgery. 2016;23(1):133–141. doi: 10.1093/icvts/ivw060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shahian DM, O’Brien SM, Filardo G, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 1–coronary artery bypass grafting surgery. The Annals of thoracic surgery. 2009;88(1 Suppl):S2–22. doi: 10.1016/j.athoracsur.2009.05.053. [DOI] [PubMed] [Google Scholar]
- 17.Morrow DA, Cannon CP, Rifai N, et al. Ability of minor elevations of troponins I and T to predict benefit from an early invasive strategy in patients with unstable angina and non-ST elevation myocardial infarction: results from a randomized trial. Jama. 2001;286(19):2405–2412. doi: 10.1001/jama.286.19.2405. [DOI] [PubMed] [Google Scholar]
- 18.Puskas JD, Kilgo PD, Thourani VH, et al. The society of thoracic surgeons 30-day predicted risk of mortality score also predicts long-term survival. The Annals of thoracic surgery. 2012;93(1):26–33. doi: 10.1016/j.athoracsur.2011.07.086. discussion 33–25. [DOI] [PubMed] [Google Scholar]
- 19.Thielmann M, Neuhauser M, Marr A, et al. Predictors and outcomes of coronary artery bypass grafting in ST elevation myocardial infarction. The Annals of thoracic surgery. 2007;84(1):17–24. doi: 10.1016/j.athoracsur.2007.03.086. [DOI] [PubMed] [Google Scholar]
- 20.Bagai A, Huang Z, Lokhnygina Y, et al. Magnitude of troponin elevation and long-term clinical outcomes in acute coronary syndrome patients treated with and without revascularization. Circulation Cardiovascular interventions. 2015;8(6):e002314. doi: 10.1161/CIRCINTERVENTIONS.115.002314. [DOI] [PubMed] [Google Scholar]
- 21.Parikh SV, de Lemos JA, Jessen ME, et al. Timing of in-hospital coronary artery bypass graft surgery for non-ST-segment elevation myocardial infarction patients results from the National Cardiovascular Data Registry ACTION Registry-GWTG (Acute Coronary Treatment and Intervention Outcomes Network Registry-Get With The Guidelines) JACC Cardiovascular interventions. 2010;3(4):419–427. doi: 10.1016/j.jcin.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 22.Weiss ES, Chang DD, Joyce DL, Nwakanma LU, Yuh DD. Optimal timing of coronary artery bypass after acute myocardial infarction: a review of California discharge data. The Journal of thoracic and cardiovascular surgery. 2008;135(3):503–511. 511.e501–503. doi: 10.1016/j.jtcvs.2007.10.042. [DOI] [PubMed] [Google Scholar]
- 23.Caceres M, Weiman DS. Optimal timing of coronary artery bypass grafting in acute myocardial infarction. The Annals of thoracic surgery. 2013;95(1):365–372. doi: 10.1016/j.athoracsur.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 24.Braxton JH, Hammond GL, Letsou GV, et al. Optimal timing of coronary artery bypass graft surgery after acute myocardial infarction. Circulation. 1995;92(9 Suppl):II66–68. doi: 10.1161/01.cir.92.9.66. [DOI] [PubMed] [Google Scholar]


