Abstract
Background
Schizophyllum commune, a basidiomycetous fungus, is a common invader of rotten wood. This fungus rarely causes mycotic disease in humans, especially cutaneous infection. In this paper, we describe the first case of cutaneous granuloma caused by S. commune in a Chinese woman.
Case presentation
A 25-year-old female with a two-year history of erythema, papules, nodules, and scales on her sole of left foot was presented to our outpatient center. Samples were obtained by the scraping of lesion and for light microscopy. Hyphae were observed by microscopic examination. We carried out a skin tissue biopsy, which showed multiple granulomatous nodules. Biopsy specimens were also inoculated onto media. After being cultured on SDA at 27 °C for 7 days, spreading-woolly-white colonies grew on the inoculation sites of media containing chloramphenicol only and there,s no other colonies grew. S. commune was identified by morphology methods, biochemical tests, and PCR sequencing. Pathological findings also aided in diagnosing cutaneous fungal granuloma. Oral itraconazole was applied. After 1 month of therapy, rashes on her left foot and pain were improved.
Conclusion
We describe the first case of cutaneous granuloma caused by Schizophyllum commune, which illustrates the importance of recognizing uncommon pathogenic fungal infections.
Keywords: Cutaneous granulomas, Itraconazole, Schizophyllum commune
Background
Schizophyllum commune is a common fungal species, which belongs to Eukaryota, Opisthokonta, Fungi, Dikarya, Basidiomycota, Agaricomycotina, Agaricomycetes, Agaricomycetidae, Agaricales, Schizophyllaceae, Schizophyllum. This fungus colonizes diverse trees and rotting woods worldwide [1–3]. S. commune has also long been regarded as nonpathogenic to humans [4, 5]. Recently, an increasing number of cases related to S. commune infection has been reported. Most reports are associated with allergic bronchopulmonary mycosis (ABPM) after inhaling the spores of S. commune [1, 2, 6]. Infection in deep tissues, such as the sphenoid sinus, maxillary sinus, and brain, has also been recently reported [2, 7–9]. To our knowledge, the cutaneous infection caused by S. commune has not been reported yet.
Case presentation
A 25-year-old female with a two-year history of erythema, papules, nodules, and scales on her sole of left foot was presented to our outpatient center. She has no history of autoimmue disease and untreated with immunosuppressive therapy. Considering her pregnancy, she was not given treatments for 1 year. The left foot skin lesion on the medial and lateral margins and on the fourth toe dorsum became enlarged with evident pain after more than 1 year (Fig. 1a and b). Approximately 1 month before visiting our department, she received treatment ineffectively in a local clinic, and the diagnosis was unclear.
Fig. 1.

(a, b) Sole of left foot exhibits erythema, papules, nodules, and scales. The fourth toe dorsum is also infected. (c, d) Foot lesions regressed after 1 month of treatment
Samples were obtained by the scraping of lesion and for light microscopy. Hyphae were observed by microscopic examination (Fig. 2).
Fig. 2.
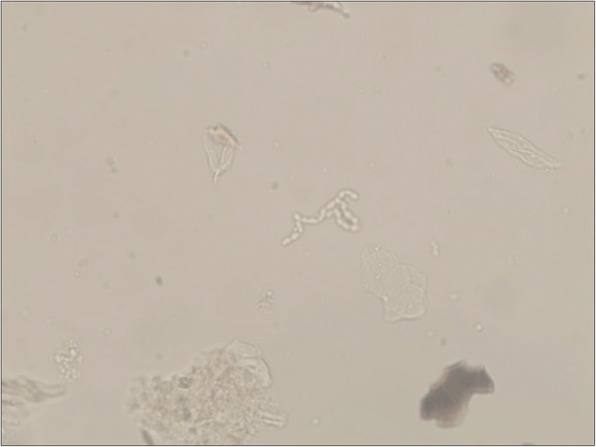
Hyphae were observed by microscopic examination (400×)
We carried out a skin tissue biopsy, which showed multiple granulomatous nodules (Fig. 3a). The Ziehl–Neelsen stain was negative. Periodic acid–Schiff (PAS) and Grocott methenamine silver (GMS) staining were carried out two times. Results were also negative. Biopsy specimens were also inoculated onto two kinds of media: Sabouraud’s dextrose agar (SDA), where one of which contained chloramphenicol and cycloheximide, and the other one contained chloramphenicol only. After being cultured on SDA at 27 °C for 7 days, spreading-woolly-white colonies grew on the inoculation sites of media containing chloramphenicol only and there,s no other colonies grew (Fig. 3b). The colonies produced an unpleasant smell like biogas. No colony was observed on the media with chloramphenicol and cycloheximide. Clamp connections, spicules, tear-like secretions, and medusa-like isomers were observed on the slide culture at 27 °C after 3 days (Fig. 3c and d). Urease activity tests were also performed. Trichophyton rubrum standard strain and the isolated strain were cultured on urease media at 27 °C for 7 days. The T. rubrum standard strain was negative, whereas the isolated strain turned red (Fig. 3e and f).
Fig. 3.
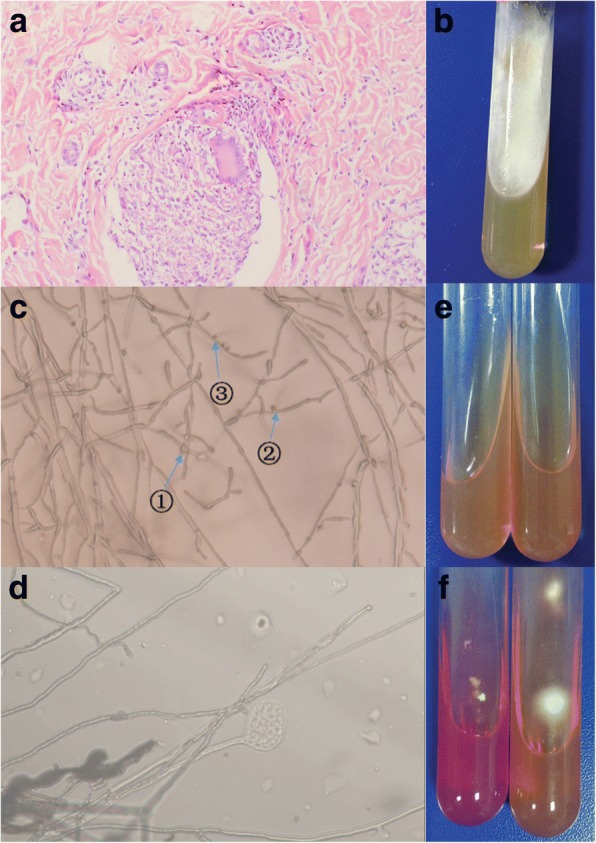
a Hematoxylin-eosin (H&E) stain for pathology study showed multiple granulomatous nodules (× 200). b When cultured on Sabouraud’s dextrose agar, spreading-woolly-white colonies grew on the media containing chloramphenicol only. c, d Clamp connections (①), spicules (②), tear-like secretions(③), and medusa-like isomers were observed on the slide culture at 27 °C after 3 days (400×). e, f Urease activity test before and after cultivation: isolated strain (+), Trichophyton rubrum standard strain (−)
Sequencing of large subunit rDNA was performed by using the E.Z.N.A.™ Fungal DNA Mini Kit (Omega Biotek, USA). We utilized set primers for the region of internal transcribed spacer (ITS) and performed PCR. The PCR primers were ITS1: 5′-TCCGTAGGTGAACCTGCGG-3′ and ITS4: 5′-TCCTCCGCTTATTGATATGC-3′. The PCR-amplified DNA was matched with that of S. commune (Nos. KP 326677.1 and KP 004975.1) with a homology of 100%. After identification, the sequence was submitted to the GenBank (MF 495704).
Pathological finding and mycological examination indicated a cutaneous granuloma caused by S. commune. Oral itraconazole (100 mg) was applied twice a day. The rashes on the left foot and the pain regressed after 1 month of treatment (Fig. 1c and d). Follow-up is currently under way.
Discussion and conclusions
To our knowledge, fungal granuloma is caused by a wide variety of fungi, such as Coccidioides, Histoplasma, Blastomyces, Cryptococcus, T. rubrum, and T. mentagraphytes, but some less known fungi have been recently documented as causes of fungal granuloma [10]. In the past, S. commune was regarded as a rare human pathogen. Since 1950 when Kligman reported the first case of onychomycosis caused by S. commune, this fungus has emerged as an increasingly important pathogen for clinical disease [11]. We conducted a literature review through PubMed and found that S. commune is an opportunistic pathogenic fungus that can cause sinusitis and ABPM mostly [3, 12], as well as rarely isolated from patients with onychomycosis, palate ulceration [11, 13]. Table 1 shows the clinical spectrum of fungal disease caused by S. commune and country-wise distribution of clinical cases. Cutaneous and subcutaneous infections caused by S. commune have not been previously reported.
Table 1.
Clinical spectrum of disease due to Schizophyllum commune and country-wise distribution of clinical cases (n = 99)
| Mycosis (No. of case) | Country (No. of cases) | References |
|---|---|---|
| Sinusitis (34) | Austria (5) | [14, 15] |
| USA(3) | [8, 16] | |
| Colombia(3) | [17–19] | |
| France (3) | [20–22] | |
| Serbia (2) | [23, 24] | |
| India(2) | [25, 26] | |
| U.K. (1) | [27] | |
| Japan (7) | [28–30] | |
| Australia (1) | [31] | |
| New Zealand(2) | [5, 32] | |
| South Korea(3) | [2, 33] | |
| China(2) | [34, 35] | |
| ABPM (30) | Japan(29) | [3, 5, 36–49] |
| India(1)a | [50] | |
| Bronchial mucoid impaction (8) | Japan(8) | [38, 45, 51–56] |
| Pulmonary fungal ball (2) | North America(1) | [57] |
| India(1) | [50] | |
| Schizophyllum asthma(2) | Japan(2) | [58] |
| Pulmonary infiltrate plus eosinophilia (1) | Japan(1) | [38] |
| Chronic eosinophilic pneumonia (1) | Japan(1) | [59] |
| Honeycomb lung (1) | Japan(1) | [60] |
| Bronchogenous cyst (1) | Serbia (1) | [61] |
| Pulmonary nodules (1) | Taiwan (1) | [62] |
| Other pulmonary mycoses (11) | Iran (7) | [63] |
| Japan (3) | [38] | |
| Italy (1) | [64] | |
| Brain abscess (2) | USA (1) | [9] |
| Austria (1) | [15] | |
| Ulceration of the palate (1) | Colombia (1) | [13] |
| Otitis externa (1) | Slovenia (1) | [65] |
| Fatal Empyema Thoracis (1) | Hong Kong (1) | [66] |
| Onychomycosis (1) | USA (1) | [11] |
| Meningitis (1) | Brazil (1) | [67] |
ainclude only one case, but the patient has the allergic broncho-pulmonary mycosis and bronchial mucoid impaction at the same time
In our case, colonies grew on the inoculation sites of media with no other colonies grew and antifungal therapy only was effective, which can be excluded the possibility of contamination. We describe the first case of cutaneous granuloma caused by S. commune, which illustrates the importance of recognizing uncommon pathogenic fungal infections.
Acknowledgments
We thank Prof. Lin Wang from West China Hospital of Sichuan University for pathologic diagnosis assistance.
Fundings
This work was supported by local city-school cooperation project (NSMC20170418) and the Project Q15005 of Youth innovation in medical research of Sichuan Province.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- ABPM
Allergic bronchopulmonary mycosis
- GMS
Grocott methenamine silver
- ITS
Internal transcribed spacer
- PAS
Periodic acid–Schiff
- PCR
Polymerase chain reaction
- S. commune
Schizophyllum commune
- SDA
Sabouraud’s dextrose agar,
- T. mentagraphytes
Trichophyton mentagraphytes
- T. rubrum
Trichophyton rubrum
Authors’ contributions
LT and YM conceptualized, collected and interpreted the clinical data, and wrote the manuscript. HZ designed, interpreted the clinical data and wrote the manuscript. XcS, CY, and XzS revised the manuscript critically for important content. DQ carried out the microbiological examination and nucleotide sequencing. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the individual patient described in this report. A copy of the written consent is available by request.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Lidi Tian and Yunzhu Mu contributed equally to this work.
Contributor Information
Lidi Tian, Email: 349357797@qq.com.
Yunzhu Mu, Email: hymyz@126.com.
Hao Zhang, Email: dr.zhanghao@126.com.
Xiaocui Su, Email: 1062879876@qq.com.
Chuan Yang, Email: 745337001@qq.com.
Xianzhu Shu, Email: 1475061304@qq.com.
Defu Qing, Email: 156106173@qq.com.
References
- 1.Ren Q, Wan L, Ju Y, et al. Animal experimental study of the pathogenicity of Schizophyllum commune. J Clin Dermatol. 2011;40(10):587–91.
- 2.Won EJ, Shin JH, Sang CL, et al. Molecular identification of Schizophyllum commune as a cause of allergic fungal sinusitis. Ann Lab Med. 2012;32(5):375–379. doi: 10.3343/alm.2012.32.5.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kobayashi H, Taira T, Wakuda K, et al. A favorable clinical effect of an expectorant in allergic bronchopulmonary mycosis caused by Schizophyllum commune. Respiratory Med Case Rep. 2016;19:54–57. doi: 10.1016/j.rmcr.2016.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Unno H, Kamei K, Honda A, et al. A murine model of pulmonary basidiomycosis by Schizophyllum commune. J Infect Chemother. 2005;11(3):136–140. doi: 10.1007/s10156-005-0382-2. [DOI] [PubMed] [Google Scholar]
- 5.Kamei K, Unno H, Nagao K, et al. Allergic bronchopulmonary mycosis caused by the basidiomycetous fungus Schizophyllum commune. Clin Infect Dis. 1994;18(3):305–309. doi: 10.1093/clinids/18.3.305. [DOI] [PubMed] [Google Scholar]
- 6.Tanaka H, Takizawa K, Baba O, et al. Basidiomycosis: Schizophyllum commune osteomyelitis in a dog. J Vet Med Sci. 2008;70(11):1257–1259. doi: 10.1292/jvms.70.1257. [DOI] [PubMed] [Google Scholar]
- 7.Roh ML, Tuazon CU, Mandler R, et al. Sphenocavernous syndrome associated with Schizophyllum commune infection of the sphenoid sinus. Ophthalmic Plast Reconstr Surg. 2005;21(1):71–74. doi: 10.1097/01.IOP.0000148407.34784.6E. [DOI] [PubMed] [Google Scholar]
- 8.Kern ME, Uecker FA. Maxillary sinus infection caused by the homobasidiomycetous fungus Schizophyllum commune. J Clin Microbiol. 1986;23(6):1001–1005. doi: 10.1128/jcm.23.6.1001-1005.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rihs JD, Padhye AA, Good CB. Brain abscess caused by Schizophyllum commune: an emerging basidiomycete pathogen. J Clin Microbiol. 1996;34(7):1628. doi: 10.1128/jcm.34.7.1628-1632.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li G. The research progress of fungal granuloma. Chin J Mycol. 2014;9(6):373–376. [Google Scholar]
- 11.Kligman AM. A Basidiomycete causing onychomycosis. illust. 1950;14(1):67–70. [DOI] [PubMed]
- 12.Seki M, Ohno H, Gotoh K, et al. Allergic bronchopulmonary mycosis due to co-infection with aspergillus fumigatus, and Schizophyllum commune. Idcases. 2014;1(1):5–8. doi: 10.1016/j.idcr.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Restrepo A, Greer DL, Robledo M, et al. Ulceration of the palate caused by a basidiomycete Schizophyllum commune. Sabouraudia. 1973;11(3):201. doi: 10.1080/00362177385190431. [DOI] [PubMed] [Google Scholar]
- 14.Buzina W, Lang-Loidolt D, Braun H, Freudenschuss K, Stammberger H. Development of molecular methods for identification of Schizophyllum commune from clinical samples. J Clin Microbiol. 2001;39:2391–2396. doi: 10.1128/JCM.39.7.2391-2396.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoenigl M, Aspeck E, Valentin T, et al. Sinusitis and frontal brain abscess in a diabetic patient caused by the basidiomycete Schizophyllum commune: case report and review of the literature. Mycoses. 2013;56(3):389–393. doi: 10.1111/myc.12040. [DOI] [PubMed] [Google Scholar]
- 16.Rosenthal J, Katz R, DuBois DB, Morrissey A, Machicao A. Chronic maxillary sinusitis associated with the mushroom Schizophyllum commune in a patient with AIDS. Clin Infect Dis. 1992;14:46–48. doi: 10.1093/clinids/14.1.46. [DOI] [PubMed] [Google Scholar]
- 17.Sigler L, Estrada S, Montealegre NA, et al. Maxillary sinusitis caused by Schizophyllum commune and experience with treatment. J Med Vet Mycol. 1997;35(5):365–370. doi: 10.1080/02681219780001431. [DOI] [PubMed] [Google Scholar]
- 18.Jiménez R, Rodríguez C, Arango M, et al. Sinusitis por Schyzophyllum commune: informe de nueve casos. Infectio. 2002;6:108.
- 19.Castro LÁ, Álvarez MI, Martínez E. Case report of Schizophyllum commune sinusitis in an immunocompetent patient. Colombia Med. 2010;41(1):71–75. [Google Scholar]
- 20.Marlier S, De Jaureguiberry JP, Aguilon P, et al. Chronic sinusitis caused by Schizophyllum commune in AIDS. Presse Med. 1993;22(23):1107. [PubMed] [Google Scholar]
- 21.Baron O, Cassaing S, Percodani J, et al. Nucleotide sequencing for diagnosis of sinusal infection by Schizophyllum commune, an uncommon pathogenic fungus. J Clin Microbiol. 2006;44(8):3042–3043. doi: 10.1128/JCM.00211-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lorentz C, Rivier A, Debourgogne A, et al. Ethmoido-maxillary sinusitis caused by the basidiomycetous fungus Schizophyllum commune. Mycoses. 2012;55(2):8–12. doi: 10.1111/j.1439-0507.2011.02060.x. [DOI] [PubMed] [Google Scholar]
- 23.Pekic S, Arsenijevic VA, Gazibara MS, et al. What lurks in the sellar? Lancet. 2010;375(9712):432. doi: 10.1016/S0140-6736(09)61835-3. [DOI] [PubMed] [Google Scholar]
- 24.Perić A, Vojvodić D, Zolotarevski L, et al. Nasal polyposis and fungal Schizophyllum commune infection: a case report. Acta Med Austriaca. 2011;54(2):83–86. doi: 10.14712/18059694.2016.25. [DOI] [PubMed] [Google Scholar]
- 25.Premamalini T, Ambujavalli B T, Anitha S, et al. Schizophyllum commune a causative agent of fungal sinusitis: a case report. Case Rep Infect Dis. 2011;(10):821259. [DOI] [PMC free article] [PubMed]
- 26.Adhikary R, Joshi S. Comment on: Schizophyllum commune sinusitis in an immunocompetent host. Indian J Med Microbiol. 2012;30(2):249. doi: 10.4103/0255-0857.96717. [DOI] [PubMed] [Google Scholar]
- 27.Clark S, Campbell CK, Sandison A, et al. Schizophyllum commune: an unusual isolate from a patient with allergic fungal sinusitis. J Infect. 1996;32(2):147. doi: 10.1016/S0163-4453(96)91436-X. [DOI] [PubMed] [Google Scholar]
- 28.Taguchi K, Oharaseki T, Yokouchi Y, et al. Allergic fungal sinusitis caused by Bipolaris spicifera and Schizophyllum commune. Med Mycol. 2007;45(6):559. doi: 10.1080/13693780701487813. [DOI] [PubMed] [Google Scholar]
- 29.Matsuwaki Y, Ogawa H, Iwasaki H, et al. Allergic fungal rhinosinusitis (AFRS) caused by the basidiomycetous fungus Schizophyllum commune. Oto-Rhino-Laryngology Tokyo. 2013;56(6):8–18. [Google Scholar]
- 30.Ahmed MK, Ishino T, Takeno S, et al. Bilateral allergic fungal rhinosinusitis caused by Schizophillum commune and aspergillus Niger. A case report. Rhinology. 2009;47(2):217–221. [PubMed] [Google Scholar]
- 31.Shaw CL, Mccleave M, Wormald PJ. Unusual presentations of isolated sphenoid fungal sinusitis. J Laryngol Otol. 2000;114(114):385–388. doi: 10.1258/0022215001905643. [DOI] [PubMed] [Google Scholar]
- 32.Sigler L, Bartley JR, Parr DH, et al. Maxillary sinusitis caused by medusoid form of Schizophyllum commune. J Clin Microbiol. 1999;37(10):3395–3398. doi: 10.1128/jcm.37.10.3395-3398.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sa HS, Ko KS, Woo KI, et al. A case of sino-orbital infection caused by the Schizophyllum commune. Diagn Microbiol Infect Dis. 2012;73(4):376–377. doi: 10.1016/j.diagmicrobio.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 34.Liu X, Zou H, Chen Q-J, et al. Allergic fungal sinusitis caused by Schizophyllum commune. World J Otorhinolary-Head Neck Surg. 2017;3(1):59–63. doi: 10.1016/j.wjorl.2017.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yin X, Liang Y, Zeng L, et al. A case of sinusitis caused by Schizophyllum commune and Bacteria in acute Myelocytic leukemia. Clin Lab. 2015;61(11):1799. doi: 10.7754/clin.lab.2015.150418. [DOI] [PubMed] [Google Scholar]
- 36.Tomita K, Hashizume I, Kasamatsu N, et al. Allergic bronchopulmonary mycosis caused by Schizophyllum commune. Nihon Kyobu Shikkan Gakkai Zasshi. 1996;34(7):804–809. [PubMed] [Google Scholar]
- 37.Yamashina S. Case of allergic bronchopulmonary mycosis caused by Schizophyllum commune. Jpn J Antibiot. 1997;50(1):51–53. [PubMed] [Google Scholar]
- 38.Kamei K, Unno H, Ito J, et al. Analysis of the cases in which Schizophyllum commune was isolated. Nihon Ishinkin Gakkai zasshi. 1999;40(3):175–181. doi: 10.3314/jjmm.40.175. [DOI] [PubMed] [Google Scholar]
- 39.Yamasaki A, Nishimura K, Sano H, et al. A case of allergic bronchopulmonary mycosis caused by Schizophyllum commune. Allergy. 2002;51(5):439. [PubMed] [Google Scholar]
- 40.Kawano T, Matsuse H, Iida K, et al. Two cases of allergic bronchopulmonary mycosis caused by Schizophyllum commune in young asthmatic patients. Nihon Kokyūki Gakkai zasshi. 2003;41(3):233. [PubMed] [Google Scholar]
- 41.Amemiya Y, Shirai R, Tokimatsu I, et al. Allergic bronchopulmonary mycosis induced by Schizophyllum commune--case report and review of the literature. Nihon Kokyuki Gakkai zasshi. 2009;47(8):692. [PubMed] [Google Scholar]
- 42.Masunaga A, Morimoto K, Ando T, et al. Three cases of allergic bronchopulmonary mycosis due to Schizophyllum commune. Nihon Kokyuki Gakkai zasshi. 2010;48(12):912. [PubMed] [Google Scholar]
- 43.Ishiguro T, Takayanagi N, Saito A, et al. Allergic bronchopulmonary mycosis due to Schizophyllum commune and aspergillus fumigatus. Nihon Kokyuki Gakkai zasshi. 2011;49(8):612–618. [PubMed] [Google Scholar]
- 44.Ogawa H, Fujimura M, Takeuchi Y, et al. The definitive diagnostic process and successful treatment for ABPM caused by Schizophyllum commune: a report of two cases. Allergol Int. 2012;61(1):163–169. doi: 10.2332/allergolint.11-CR-0325. [DOI] [PubMed] [Google Scholar]
- 45.Uruga H, Imafuku A, Hanada S, et al. A case of allergic bronchopulmonary mycosis caused by Schizophyllum commune presenting with hyperattenuated mucoid impaction. Nihon Kokyuki Gakkai Zasshi. 2010;48(10):749–754. [PubMed] [Google Scholar]
- 46.Ikushima S. Case of allergic bronchopulmonary mycosis caused by Schizophyllum commune. Jpn J Antibiot. 1997;50:47–49. [PubMed] [Google Scholar]
- 47.Nishimura K. Allergic bronchopulmonary mycosis caused by the Basidiomycetous fungus Schizophyllum commune[J] Clin Infect Dis. 1994;18(3):305–309. doi: 10.1093/clinids/18.3.305. [DOI] [PubMed] [Google Scholar]
- 48.Tomita K, Hashizume I. Kasamatsu N, et al. [allergic bronchopulmonary mycosis caused by Schizophyllum commune][J] Nihon Kyōbu Shikkan Gakkai Zasshi. 1996;34(7):804–809. [PubMed] [Google Scholar]
- 49.Seki M, Ohno H, Gotoh K, et al. Allergic bronchopulmonary mycosis due to co-infection with aspergillus fumigatus, and Schizophyllum commune[J] Idcases. 2014;1(1):5–8. doi: 10.1016/j.idcr.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chowdhary A, Randhawa HS, Gaur SN, et al. Schizophyllum commune, as an emerging fungal pathogen: a review and report of two cases. Mycoses. 2013;56(1):1. doi: 10.1111/j.1439-0507.2012.02190.x. [DOI] [PubMed] [Google Scholar]
- 51.Amitani R, Nishimura K, Niimi A, et al. Bronchial mucoid impaction due to the Monokaryotic mycelium of Schizophyllum commune. Clin Infect Dis. 1996;22(1):146–148. doi: 10.1093/clinids/22.1.146. [DOI] [PubMed] [Google Scholar]
- 52.Miyazaki Y, Sakashita H, Tanaka T, et al. Mucoid impaction caused by monokaryotic mycelium of Schizophyllum commune in association with bronchiectasis. Intern Med. 2000;39(2):160–162. doi: 10.2169/internalmedicine.39.160. [DOI] [PubMed] [Google Scholar]
- 53.Itou Y, Sasaki S, Watanabe S, et al. A case of mucoid impaction of bronchi (MIB) due to Schizophyllum commune. Nihon Kokyuki Gakkai Zasshi. 2001;39:266–270. [PubMed] [Google Scholar]
- 54.Ishiguro T, Takayanagi N, Tokunaga D, et al. Pulmonary Schizophyllum commune infection developing mucoid impaction of the bronchi. Yale J Biol Med. 2007;80(3):105–111. [PMC free article] [PubMed] [Google Scholar]
- 55.Ishiguro T, Takayanagi N, Harasaw K, et al. Mucoid impaction of the bronchi caused by Schizophyllum commune which developed after discontinuation of itraconazole administration. Nihon Kokyuki Gakkai zasshi. 2009;47(4):296. [PubMed] [Google Scholar]
- 56.Kato F, Kasamaatsu N, Kasai H, et al. A case of mucoid impaction of bronchi caused by Schizophyllum commune. J Jpn Soc Bronchology. 2012;34:38–43. [Google Scholar]
- 57.Sigler L, Maza LMDL, Tan G, et al. Diagnostic difficulties caused by a nonclamped Schizophyllum commune isolate in a case of fungus ball of the lung. J Clin Microbiol. 1995;33(8):1979–1983. doi: 10.1128/jcm.33.8.1979-1983.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ogawa H, Fujimura M, Takeuchi Y, et al. Two cases of Schizophyllum asthma: is this a new clinical entity or a precursor of ABPM? Pulm Pharmacol Ther. 2011;24(5):559–562. doi: 10.1016/j.pupt.2011.04.030. [DOI] [PubMed] [Google Scholar]
- 59.Kawayama T, Fujiki R, Rikimaru T, et al. Chronic eosinophilic pneumonia associated with, Schizophyllum commune. Respirology. 2003;8(4):529–531. doi: 10.1046/j.1440-1843.2003.00504.x. [DOI] [PubMed] [Google Scholar]
- 60.Iizasa T, Kamei K, Chiyo M, et al. Colonization with Schizophyllum commune of localized honeycomb lung with mucus. Respiration. 2001;68(2):201–203. doi: 10.1159/000050493. [DOI] [PubMed] [Google Scholar]
- 61.Bulajic N, Cvijanovic V, Vukojevic J, et al. Schizophyllum commune, associated with bronchogenous cyst. Mycoses. 2006;49(4):343–345. doi: 10.1111/j.1439-0507.2006.01247.x. [DOI] [PubMed] [Google Scholar]
- 62.Roan JN, Hsieh HY, Tsai HW, et al. Pulmonary nodules caused by Schizophyllum commune, after cardiac transplantation. J Infect. 2009;58(2):164–167. doi: 10.1016/j.jinf.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 63.Chadeganipour M, Bonerje G, Nilipour S. Detection of antibodies in immunocompromised patients affected with pulmonary Schizophyllum infection. Clin Immunol. 2010;135(1):S75. doi: 10.1016/j.clim.2010.03.224. [DOI] [Google Scholar]
- 64.Tullio V, Mandras N, Banche G, et al. Schizophyllum commune: an unusual of agent bronchopneumonia in an immunocompromised patient. Med Mycol. 2009;46(46):735–738. doi: 10.1080/13693780802256091. [DOI] [PubMed] [Google Scholar]
- 65.Matos T, Tomazin R, Battelino S. First report of otitis externa caused by Schizophyllum commune and review of the literature. Wien Klin Wochenschr. 2016;128(9–10):387–390. doi: 10.1007/s00508-015-0898-0. [DOI] [PubMed] [Google Scholar]
- 66.Chan JFW, Teng JLL, Li IWS, et al. Fatal empyema Thoracis caused by Schizophyllum commune with cross-reactive Cryptococcal Antigenemia. J Clin Microbiol. 2014;52(2):683. doi: 10.1128/JCM.02770-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chavez-Batista A, Maica JA, Singer R. Basidio-neuromycosis on man. Anals da Sociedade de Biologia de Pernambuco. 1955;13:52–60. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.


