Abstract
背景与目的
国内外目前已有多篇现场细胞学应用于经支气管镜针吸活检(transbronchial needle aspiration, TBNA)的报道,但专门针对肺癌患者的研究很少。本研究的目的是探讨TBNA联合现场细胞学在肺癌诊断中的作用。
方法
回顾性分析2012年12月-2013年12月在滨州市人民医院行TBNA并最终确诊为肺癌的69例患者,其中行现场细胞学者37例,未行现场细胞学者32例。比较现场细胞学结果与最终HE染色结果的一致性,同时比较两组患者的诊断率、每个淋巴结穿刺针数、并发症发生率及细胞学诊断费用。
结果
现场细胞学与HE染色一致性为94.1%(32/34)。现场细胞学组诊断率与非现场细胞学组相比无统计学差异(91.9% vs 78.1%, P=0.20);但平均穿刺针数及并发症发生率,现场细胞学组少于非现场细胞学组(t=29.5, P < 0.05; χ2=4.4, P < 0.05),现场细胞学组患者细胞学诊断费用低于非现场细胞学组(t=10.9, P < 0.05)。
结论
TBNA联合现场细胞学诊断肺癌,与HE染色一致性好,且能减少穿刺针数及并发症,节省细胞学诊断费用,值得推广。
Keywords: 经支气管镜针吸活检, 现场细胞学, 肺肿瘤
Abstract
Background and objective
There have been several studys about transbronchial needle aspiration (TBNA) combined with rapid on-site evaluation (ROSE) so far at home and abroad, yet few studys were especially for patients with lung cancer. The aim of our study is to investigate the effect of TBNA combined with ROSE in the diagnosis of lung cancer.
Methods
The data of the patients from December 2012 to December 2013, who were performed with TBNA and ultimately diagnosed with lung cancer in the People's Hospital of Binzhou City, were retrospectively analyzed. The patients were divided into two groups, ROSE group (rapid on-site evaluation group) and no-ROSE group (the group without rapid on-site evaluation). Among these patients, 37 patients were in the ROSE group and 32 patients were in the no-ROSE group. The result of ROSE and HE stain, the diagnostic yields and needle passes of each lymph node, the complication and cytology diagnostic cost of TBNA with ROSE and without ROSE were compared.
Results
The coherence of ROSE and HE stain was 94.1% (32/34). The diagnostic yields of TBNA were 91.9% (34/37) and 78.1% (25/32) in ROSE group and no-ROSE group respectively, no significant differences were found. But the median number of needle passes of each lymph node and the percentage of the complication in ROSE group and no-ROSE group was significantly lower (t=29.5, P < 0.05 and χ2=4.4, P < 0.05, respectively). The cytopathological diagnostic cost of ROSE group was significantly lower compared with no-Rose group (t=10.9, P < 0.05).
Conclusion
TBNA combined with ROSE has good concordance with HE stain in the diagnosis of lung cancer, and could reduce the needle passes, cytopathological diagnostic cost and complication, worthy of popularized.
Keywords: Transbronchial needle aspiration (TBNA), Rapid on-site evaluation (ROSE), Lung neoplasms
在临床工作中经常遇到肺内占位合并肺门和/或纵隔淋巴结肿大,以及单纯肺门和/或纵隔淋巴结肿大患者,这种情况下单纯依靠胸部CT不能确诊,因为很多疾病可以有类似影像学表现,如肺癌、转移性肿瘤、淋巴瘤、结节病、淋巴结结核等。支气管镜粘膜活检或刷检能明确镜下有新生物或粘膜有浸润表现的部分患者,但对镜下无新生物及粘膜正常的患者,常规支气管镜检查却难以明确诊断。这种情况往往需要依靠经支气管镜针吸活检(transbronchial needle aspiration, TBNA)、超声支气管镜引导下经支气管镜针吸活检(endobronchial ultrasound-guided transbronchial needle aspiration, EBUS-TBNA)或纵隔镜才能明确诊断。其中纵隔镜仍是目前纵隔淋巴结活检的“金标准”[1]。但标准纵隔镜在很多地方不能常规开展,且需要在全麻下进行、费用昂贵、需要住院,并发症和死亡率在1.4%-2.3%[2],目前往往在TBNA和EBUS-TBNA结果阴性时才考虑行纵隔镜。由于经济因素,国内开展EBUS-TBNA的医院很少,因此在大多数医院TBNA仍是明确纵隔或肺门肿大淋巴结性质的首选方法。
由于TBNA系“盲穿”,操作时不能直接看到气管或支气管壁外的结构[3],因此操作过程中不能确定是否穿刺到目标淋巴结。很多临床医生由于阳性率低或害怕由此引起的风险而放弃该项检查。为了解决这个问题,现场细胞学(rapid on-site evaluation, ROSE)开始应用于临床[4]。现场细胞学检查是在支气管镜检查过程中,由细胞病理学家现场对穿刺标本进行制片和染色,并进行快速评价,向操作者反馈穿刺是否成功,并提供初步诊断的一种方法[5]。国内外目前已有多篇[4, 6-10]现场细胞学用于TBNA的报道,但专门针对肺癌患者的研究很少。我们对行TBNA并最终确诊为肺癌的患者进行回顾性分析,旨在对TBNA联合现场细胞学在肺癌诊断中的作用进行评价。
1. 研究对象与方法
1.1. 对象
2012年12月-2013年12月共有74例患者在滨州市人民医院支气管镜室行TBNA,最终诊断为肺癌的69例患者纳入本研究。全部患者胸部强化CT示至少有1组纵隔或肺门淋巴结肿大(淋巴结短经大于10 mm)伴有或不伴有肺内肿块,但支气管镜检查镜下未见明显新生物及肿瘤浸润改变。
1.2. TBNA及现场细胞学检查过程
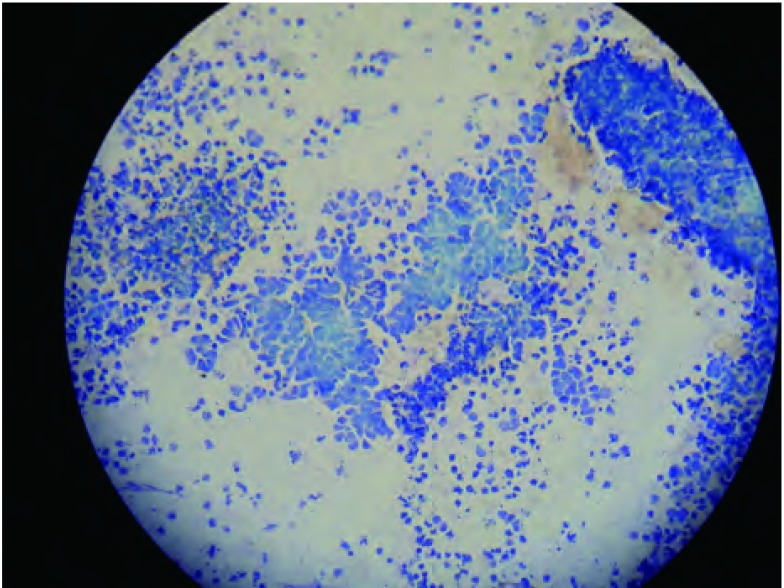
根据第七版肺癌TNM分期系统[11]和WANG氏分区定位法[12]明确穿刺淋巴结的位置。麻醉成功后,用标准的可弯曲支气管镜(BF-260,奥林巴斯),按文献所述方法[13, 14]以王氏122针(Conmed Corprotion, USA)行TBNA,优先选择最易穿刺到的淋巴结,如第7组和4R组淋巴结。每次穿刺完毕后取出穿刺针,并将抽得穿刺液快速打到载玻片上,快速推片。行现场细胞学者由细胞病理学医师以甲苯胺蓝按文献[4]所述方法进行染色并现场阅片,如现场细胞学检查结果阳性(图 1),则停止TBNA操作,如检查结果阴性则由术者在原部位或另选穿刺点再次穿刺,每个部位穿刺次数最多不超过7次[15],操作结束后所有涂片送病理科脱色后行HE染色,由2名高年资病理科医师阅片并确定最终诊断,作为“金标准”。不行现场细胞学者穿刺结束所有涂片置95%乙醇固定后常规送HE染色。非现场细胞学组按文献[16, 17]推荐穿刺3针-5针,由操作者根据穿刺抽吸的效果决定。全部69例TBNA操作由同一名医师完成,操作全程监测心电、血压、指脉氧。
1.
现场细胞学甲苯胺蓝染色(×200)肿瘤细胞胞浆稀少,呈裸核状,核深染,不规则(小细胞肺癌)。
Rapid on-site evaluation with Toluidine blue stain (×200). Tumor cells with little cytoplasm, naked nucleus, and the nucleus were hyperchromatic and irregular (small cell lung caner).
1.3. TBNA结果判读
涂片中如果可见多个淋巴细胞团,或较多癌细胞,认为TBNA穿刺成功;如果为大量红细胞或有核细胞很少,则认为TBNA穿刺失败。如涂片中发现癌细胞则认为穿刺结果阳性,如涂片中未发现癌细胞,则认为穿刺结果阴性。每例患者任何一个部位TBNA结果阳性,则认为TBNA总结果阳性;全部部位TBNA结果阴性,则认为TBNA总结果阴性[18]。
1.4. 现场细胞学组与非现场细胞学组相关指标比较
比较现场细胞学结果与最终的HE染色结果的一致性,同时比较TBNA在现场细胞学组及非现场细胞学组的诊断率(现场细胞学组诊断率以HE染色结果为准)、每个淋巴结穿刺针数、并发症发生率及细胞病理学诊断费用。TBNA最常见的并发症为出血,出血量由支气管镜医师根据镜下表现估计。按文献所述[19]分为极少量出血、轻度出血、中度出血及重度出血。极少量出血定义为 < 5 mL,轻度出血定义为5 mL-20 mL,中度出血定义为 > 20 mL-100 mL,重度出血定义 > 100 mL。极少量出血不列为并发症范畴。
1.5. 统计学分析
以SPSS 17.0统计软件进行统计学分析。计量资料采用t检验,组间率的比较采χ2检验,以P < 0.05认为有统计学差异。
2. 结果
2.1. 患者一般资料及TBNA穿刺淋巴结分布
结果见表 1、表 2。现场细胞学组37例患者中,男25例,女12例,年龄最大76岁,最小35岁,平均(56.8±11.2)岁,肿大淋巴结的短径为(1.8±0.2)cm。非现场细胞学组32例患者中,男性22例,女性10例,年龄最大74岁,最小38岁,平均(57.5±10.8)岁,肿大淋巴结的短径为(1.7±0.5)cm,上述资料两组相比差异无统计学意义。
1.
患者一般资料
General data of patients
| Variables | ROSE group | No-ROSE group | P |
| ROSE: rapid on-site evaluation; No-ROSE group: group without rapid on-site evaluation. | |||
| Age (yr) | 56.8±11.2 | 57.5±10.8 | 0.8 |
| Sex (male/female) | 25/12 | 21/11 | 0.9 |
| Short axis of lymph node (cm) | 1.8±0.2 | 1.7±0.5 | 0.3 |
2.
淋巴结分布
Location of lymph nodes
| Lymph node station | ROSE group (n) | No-ROSE group (n) |
| 10R | 4 | 1 |
| 10L | 2 | 3 |
| 11R | 2 | 1 |
| 11L | 1 | 0 |
| 4L | 5 | 4 |
| 4R | 8 | 10 |
| 7 | 22 | 20 |
| Total | 44 | 39 |
2.2. TBNA穿刺结果
现场细胞学组37例患者共穿刺44个部位,106针,穿刺成功98针(92.5%)。非现场细胞学组32例患者共穿刺39个部位,179针,穿刺成功154针(86.0%)。现场细胞学组37例肺癌患者中,甲苯胺蓝染色共确诊肺癌32例,其中小细胞肺癌16例,鳞癌6例,腺癌10例,其余5例中有2例系现场细胞学阴性,经HE染色证实分别为鳞癌和腺癌,另外3例甲苯胺蓝及HE染色均为阴性,经至上级医院行EBUS-TBNA确诊。非现场细胞学组由TBNA确诊小细胞肺癌12例,鳞癌5例,腺癌8例,其余7例通过经支气管肺活检、EBUS-TBNA确诊,其中鳞癌3例,腺癌4例(表 3)。
3.
TBNA穿刺结果
Results of TBNA
| Diagnosis | ROSE group (n=37)* | No-ROSE group (n=32)** |
|
| Toluidine blue stain |
HE stain | ||
| *Among the 37 patients,there patients got the negative result by TBNA and were diagnosed by EBUS-TBNA; ** Among the 32 patients,two patients were diagnose by transbronchial lung biopsy and five patients were diagnosed by EBUS-TBNA. | |||
| Small cell lung cancer | 16 | 16 | 12 |
| Squamous cell cancer | 6 | 7 | 5 |
| Adenocarcinoma | 10 | 11 | 8 |
| Total | 32 | 34 | 25 |
2.3. 现场细胞学与HE染色一致性
现场细胞学组甲苯胺蓝染色诊断肺癌32例,且均经HE染色证实,未出现假阳性结果,2例现场细胞学检查阴性,经HE染色分别诊断为鳞癌和腺癌,两者一致性为94.1%(32/34)。
2.4. 两组诊断率对比
现场细胞学组TBNA对肺癌诊断率为91.9%(34/37),非现场细胞学组TBNA诊断率为78.1%(25/32),两者相比差异无统计学意义(χ2=1.63, P=0.20)。
2.5. 非现场细胞学结果
非现场细胞学组每个淋巴结穿刺针数、镜下出血率、细胞学诊断相关费用均高于现场细胞学组,两者相比有统计学差异(表 4)。其中现场细胞学组和非现场细胞学组分别有4例和10例出现轻度出血,无中度和重度出血及纵隔气肿、纵隔血肿等并发症发生。
4.
现场细胞学组与非现场细胞学组相关指标对比
Comparison of index between Rose-group and no-Rose group
| Needle passes (n) | Bleeding rate (n) | Cytology diagnostic cost (RMB) | |
| No-ROSE group (n=32) | 4.6±0.4 | 10/32 | 140.3±4.6 |
| Rose group (n=37) | 2.4±0.2 | 4/37 | 130.8±2.5 |
| t=29.5 | χ2=4.4 | t=10.9 | |
| P | P < 0.001 | P=0.035 | P < 0.001 |
3. 讨论
TBNA是一种获取气道壁、肺实质以及邻近支气管树纵隔内病变部位的细胞学、组织学或微生物学标本的技术。有研究[20]将此技术应用于可弯曲支气管镜,目前已在临床广泛开展,在纵隔及肺门肿大淋巴结的诊断及鉴别诊断、肺癌的早期诊断和分期、纵隔及管外型病灶的活检等方面发挥着独特的重要作用。国内荣福教授最早开展该项技术,并逐步在全国范围内推广。目前TBNA已经成为肺癌诊断和分期的有力工具,文献[21]报道TBNA阳性率20%-90%,很多医师由于阳性率太低而放弃该项检查。为提高穿刺成功率,我院呼吸科自2012年联合病理科引入现场细胞学技术,并取得了较理想的结果,刚刚开展TBNA的医院可借鉴。
行TBNA时每个淋巴结穿刺几次能获得较高的阳性率,文献报道差异较大。有研究[16, 22]推荐3次,有研究[17]建议当穿刺仅仅是为了明确诊断,且在一个以上淋巴结穿刺取材或有其他的取材手段时,3针较合适,而当穿刺目的是肺癌的分期时应至少穿刺4针-5针。最近一篇系统性回顾中推荐3针-5针[23]。但上述研究均不是专门针对肺癌患者。主要针对肺癌患者的一项前瞻性研究[15]中发现穿刺4针-7针可获得最好的诊断率,穿刺7次诊断率达到一个平台,再增加穿刺次数阳性率无明显增加。同时该研究中发现现场细胞学组的平均穿刺次数为(2.5±2.0)次,非现场细胞学组穿刺次数为(3.7±1.6)次,两者相比差异有统计学意义,因此得出现场细胞学能减少穿刺针数的结论。我们的研究中现场细胞学组平均穿刺次数为(2.4±0.2)次、非现场细胞学组平均穿刺次数为(4.6±0.4)次,所得结论与上述研究相一致。同时我们的研究中发现因穿刺针数减少,病理科医师阅片张数减少,因此细胞学诊断费用下降,同样因为穿刺针数减少,应用现场细胞学组出血发生率较未应用现场细胞学组减少,这与Trisolini等[9]的研究结论一致。
早期的研究[4, 7, 8]发现,与未行现场细胞学检查组相比,现场细胞学组获得不满意标本(定义为没有淋巴细胞或诊断性的/恶性肿瘤细胞)的例数减少,对恶性肿瘤的诊断率高,因此推断现场细胞学能提高诊断率。2011年的发表的两项研究[9, 10],主要评估现场细胞学对胸部CT表现为肺门/纵隔淋巴结肿大患者的诊断价值,这些患者未经筛选,既有肺癌患者,也有淋巴瘤、结节病、结核患者。这两项随机对照研究发现应用现场细胞学组与未应用现场细胞学组相比诊断率无统计学差异,因此考虑早期研究结果可能与选择偏倚有关。我们的研究中现场细胞学组诊断率为91.9%,非现场细胞学组诊断率为78.1%,两组诊断率无统计学差异,与上述两项研究结论相一致。本研究与之前研究对比,优势是研究对象是专门针对肺癌患者,潜在缺陷之一是未使用随机对照,因此上述结论尚需专门针对肺癌的大样本、随机对照研究进一步证实。
文献[24, 25]报道第4组和第7组淋巴结穿刺阳性率较高,因此我们在穿刺时大多首选这两组淋巴结。本研究最终对肺癌的诊断阳性率(以HE染色为准)为91.9%(34/37),略高于国内文献[18, 26, 27]所报道,考虑除与应用现场细胞学有关外,也与所选择穿刺部位多为第4和第7组淋巴结有关。
我们的研究中现场细胞学对小细胞肺癌的诊断率为100%(16/16),对腺癌和鳞癌的诊断率相对偏低,这与李香菊等[28]的报道一致。文献[23]报道小细胞肺癌穿刺阳性率较高可能是因为小细胞肺癌生物学侵袭性高、黏附性低,且容易侵犯4R组淋巴结。刚开展TBNA的医院可以从临床疑诊小细胞肺癌的患者开始练习穿刺,以提高自信心。通过我们的观察发现,以甲苯胺蓝行现场细胞学与HE染色相比一致性为94.1%(32/34)。有2例患者现场细胞学阴性,而HE染色证实分别为鳞癌和腺癌,这提示我们现场细胞学所提供诊断为临时诊断,最终诊断仍应以常规HE染色为准。
现场细胞学检查需要细胞病理学家的参与,但国内的现状是病理科医生日常工作非常繁忙,很难抽出专门的人员参与现场细胞学检查,因此国内很少有医院开展这项工作。但最近Chest上发表的一项研究[29]有望改变这种局面。在这项研究中肺科医师经过3个月的细胞病理学知识培训后行现场细胞学检查,准确率可达80%,与细胞病理学家相比(准确率92%)无统计学差异。因此我们有理由相信将来会有越来越多的肺科医师参与现场细胞学检查,这将大大推进这项技术的普及。
总之,TBNA联合现场细胞学诊断肺癌,与HE染色一致性好,且能减少穿刺针数及并发症,节省细胞学诊断费用,值得推广。
Funding Statement
本研究受山东省科学技术发展计划医药卫生项目(No.2009GG10002061)资助
The study was supported by the grant from Scientific and Technological Development Plan Projets of Shandong Province, China (to Shujuan JIANG)(No.2009GG10002061)
References
- 1.Lerut T, De Leyn P, Coosemans W, et al. Cervical videomediastinoscopy. Thorac Surg Clin. 2010;20(2):195–206. doi: 10.1016/j.thorsurg.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Reich JM, Brouns MC, O' Connor EA, et al. Mediastinoscopy in patients with presumptive stage I sarcoidosis: a risk/benefit, cost/benefit analysis. Chest. 1998;113(1):147–153. doi: 10.1378/chest.113.1.147. [DOI] [PubMed] [Google Scholar]
- 3.Yarmus L, Van der Kloot T, Lechtzin N, et al. A randomized prospective trial of the utility of rapid on-site evaluation of transbronchial needle aspirate specimens. J Bronchol Interv Pulmonol. 2011;18(2):121–127. doi: 10.1097/LBR.0b013e31821707ee. [DOI] [PubMed] [Google Scholar]
- 4.Davenport RD. Rapid on-site evaluation of transbronchial aspirates. Chest. 1990;98(1):59–61. doi: 10.1378/chest.98.1.59. [DOI] [PubMed] [Google Scholar]
- 5.Wohlschläger J, Darwiche K, Ting S, et al. Rapid on-site evaluation (ROSE) in cytological diagnostics of pulmonary and mediastinal diseases. Pathologe. 2012;33(4):308–315. doi: 10.1007/s00292-012-1578-8. [DOI] [PubMed] [Google Scholar]
- 6.Diette GB, White P Jr, Terry P, et al. Utility of on-site cytopathology assessment for bronchoscopic evaluation of lung masses and adenopathy. Chest. 2000;117(4):1186–1190. doi: 10.1378/chest.117.4.1186. [DOI] [PubMed] [Google Scholar]
- 7.Baram D, Garcia RB, Richman PS. Impact of rapid on-site cytologic evaluation during transbronchial needle aspiration. Chest. 2005;128(2):869–875. doi: 10.1378/chest.128.2.869. [DOI] [PubMed] [Google Scholar]
- 8.Diacon AH, Schuurmans MM, Theron J, et al. Utility of rapid on-site evaluation of transbronchial needle aspirates. Respiration. 2005;72(2):182–188. doi: 10.1159/000084050. [DOI] [PubMed] [Google Scholar]
- 9.Trisolini R, Cancellieri A, Tinelli C, et al. Rapid on-site evaluation of transbronchial aspirates in the diagnosis of hilar and mediastinal adenopathy: a randomized trial. Chest. 2011;139(2):395–401. doi: 10.1378/chest.10-1521. [DOI] [PubMed] [Google Scholar]
- 10.Yarmus L, Van der Kloot T, Lechtzin N, et al. A randomized prospective trial of the utility of rapid on-site evaluation of transbronchial needle aspirate specimens. J Bronchol Interv Pulmonol. 2011;18(2):121–127. doi: 10.1097/LBR.0b013e31821707ee. [DOI] [PubMed] [Google Scholar]
- 11.Kligerman S, Abbott G. A radiologic review of the new TNM classification for lung cancer. AJR Am J Roentgenol. 2010;194(3):562–573. doi: 10.2214/AJR.09.3354. [DOI] [PubMed] [Google Scholar]
- 12.Wang KP. Staging of bronchogenic carcinoma by bronchoscopy. Chest. 1994;106(2):588–593. doi: 10.1378/chest.106.2.588. [DOI] [PubMed] [Google Scholar]
- 13.Patelli M, Lazzari Agli L, Poletti V, et al. Role of fiberscopic transbronchial needle aspiration in the staging of N2 disease due to non-small cell lung cancer. Ann Thorac Surg. 2002;73(2):407–411. doi: 10.1016/S0003-4975(01)03447-6. [DOI] [PubMed] [Google Scholar]
- 14.Rong F, Guo S, Zuo LE, et al. Transbronchial needle aspiration in diagnosing mediastinal and hilar tuberculous lymphadenopathy. http://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_zhjhhhx200206003. Zhonghua Jie He He Hu Xi Za Zhi. 2002;25(6):330–332. [PubMed] [Google Scholar]; 荣 福, 郭 苏, 左 六二, et al. 经支气管针吸活检在纵隔及肺门淋巴结结核诊断中的作用. http://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_zhjhhhx200206003. 中华结核和呼吸杂志. 2002;25(6):330–332. [PubMed] [Google Scholar]
- 15.Chin R Jr, McCain TW, Lucia MA, et al. Transbronchial needle aspiration in diagnosing and staging lung cancer: how many aspirates are needed? http://www.ncbi.nlm.nih.gov/pubmed/12153974. Am J Respir Crit Care Med. 2002;166(36):377–381. doi: 10.1164/rccm.2106153. [DOI] [PubMed] [Google Scholar]
- 16.Schenk DA, Bryan CL, Bower JH, et al. Transbronchial needle aspiration in the diagnosis of bronchogenic carcinoma. Chest. 1987;92(1):83–85. doi: 10.1378/chest.92.1.83. [DOI] [PubMed] [Google Scholar]
- 17.Diacon AH, Schuurmans MM, Theron J, et al. Transbronchial needle aspirates: how many passes per target site? https://www.ncbi.nlm.nih.gov/pubmed/17005579. Eur Respir J. 2007;29(1):112–116. doi: 10.1183/09031936.00055506. [DOI] [PubMed] [Google Scholar]
- 18.Wang MZ, Chen Y, Zhong W, et al. Transbronchial needle aspiration in the diagnosis of bronchogenic carcinoma with enlarged mediastinal and/or hilar lymph nodes. http://med.wanfangdata.com.cn/Paper/Detail/PeriodicalPaper_zhzl200607014. Zhonghua Zhong Liu Za Zhi. 2006;28(7):533–535. [PubMed] [Google Scholar]; 王 孟昭, 陈 勇, 钟 巍, et al. 经支气管镜淋巴结针吸活检对肺癌的诊断意义. http://med.wanfangdata.com.cn/Paper/Detail/PeriodicalPaper_zhzl200607014. 中华肿瘤杂志. 2006;28(7):533–535. [PubMed] [Google Scholar]
- 19.Carr IM, Koegelenberg CF. Blood loss during flexible bronchoscopy: a prospective observational study. Respiration. 2012;84(4):312–318. doi: 10.1159/000339507. [DOI] [PubMed] [Google Scholar]
- 20.Rong F, Li Q, Wang KP. The practical application of transbronchial needle aspiration on pulmonary disease. http://d.wanfangdata.com.cn/Periodical_zhjhhhx200801003.aspx. Zhonghua Jie He He Hu Xi Za Zhi. 2008;31(1):6–7. [PubMed] [Google Scholar]; 荣 福, 李 强, Wang Ko Pen. 经支气管针吸活检术在呼吸系统疾病诊治中的应用. http://d.wanfangdata.com.cn/Periodical_zhjhhhx200801003.aspx. 中华结核和呼吸杂志. 2008;31(1):6–7. [PubMed] [Google Scholar]
- 21.Rakha EA, Naik V, Chaudry Z. Cytological assessment of conventional transbronchial fine needle aspiration of lymph nodes. Cytopathology. 2010;21(1):27–34. doi: 10.1111/j.1365-2303.2008.00590.x. [DOI] [PubMed] [Google Scholar]
- 22.Wang KP, Brower R, Haponik EF, et al. Flexible transbronchial needle aspiration for staging of bronchogenic carcinoma. Chest. 1983;84(5):571–576. doi: 10.1378/chest.84.5.571. [DOI] [PubMed] [Google Scholar]
- 23.Bonifazi M, Zuccatosta L, Trisolini R, et al. Transbronchial needle aspiration: a systematic review on predictors of a successful aspirate. Respiration. 2013;86(2):123–134. doi: 10.1159/000350466. [DOI] [PubMed] [Google Scholar]
- 24.Soja J, Szlubowski A, Kocoń P, et al. Usefulness of transbronchial needle aspiration for initial lung cancer staging. http://www.ncbi.nlm.nih.gov/pubmed/20693956. Pol Arch Med Wewn. 2010;120(7-8):264–269. [PubMed] [Google Scholar]
- 25.Stoll LM, Yung RC, Clark DP, et al. Cytology of endobronchial ultrasound-guided transbronchial needle aspiration versus conventional transbronchial needle aspiration. Cancer Cytopathol. 2010;118(5):278–286. doi: 10.1002/cncy.20103. [DOI] [PubMed] [Google Scholar]
- 26.Wang MZ, Wan XB, Chen Y, et al. The results of transbronchial needle aspiration in 164 cases with enlarged mediastinal and/or hilar lymph nodes. http://d.wanfangdata.com.cn/Periodical_zhnk200902016.aspx. Zhonghua Nei Ke Za Zhi. 2009;48(2):133–135. [PubMed] [Google Scholar]; 王 孟昭, 万 小兵, 陈 勇, et al. 经支气管淋巴结针吸活检164例结果分析. http://d.wanfangdata.com.cn/Periodical_zhnk200902016.aspx. 中华内科杂志. 2009;48(2):133–135. [PubMed] [Google Scholar]
- 27.Wang D, Ma WX, Jiang SJ, et al. Diagnostic value of endobronchial ultrasound-guided transbronchial needle aspiration in paratracheal mediastinal lesions. Zhonghua Yi Xue Za Zhi. 2013;93(20):1563–1566. doi: 10.3760/cma.j.issn.0376-2491.2013.20.013. [DOI] [PubMed] [Google Scholar]; 王 栋, 马 卫霞, 姜 淑娟. 经支气管镜超声引导针吸活检术在纵隔病变诊断中的应用价值. 中华医学杂志. 2013;93(20):1563–1566. doi: 10.3760/cma.j.issn.0376-2491.2013.20.013. [DOI] [PubMed] [Google Scholar]
- 28.Li XJ, Zhao J, Wang P, et al. Comparative analysis of cytopathologic and histopathologic diagnosis in the transbronchial needle aspiration specimens. http://www.airitilibrary.com/Publication/alDetailedMesh?docid=zhblx201206009. Zhonghua Bing Li Xue Za Zhi. 2012;41(6):400–404. doi: 10.3760/cma.j.issn.0529-5807.2012.06.009. [DOI] [PubMed] [Google Scholar]; 李 香菊, 赵 军, 王 萍, et al. 经支气管针吸活检标本的细胞与组织病理比较分析. http://www.airitilibrary.com/Publication/alDetailedMesh?docid=zhblx201206009. 中华病理学杂志. 2012;41(6):400–404. doi: 10.3760/cma.j.issn.0529-5807.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 29.Bonifazi M, Sediari M, Ferretti M, et al. The role of the pulmonologist in rapid on-site cytological evaluation of transbronchial needle aspiration: a prospective study. Chest. 2014;145(1):60–65. doi: 10.1378/chest.13-0756. [DOI] [PubMed] [Google Scholar]