Abstract
A past history of pulmonary tuberculosis (TB) is a risk factor for long-term respiratory impairment. Post-TB lung dysfunction often goes unrecognised, despite its relatively high prevalence and its association with reduced quality of life. Importantly, specific host and pathogen factors causing lung impairment remain unclear. Host immune responses probably play a dominant role in lung damage, as excessive inflammation and elevated expression of lung matrix-degrading proteases are common during TB. Variability in host genes that modulate these immune responses may determine the severity of lung impairment, but this hypothesis remains largely untested. In this review, we provide an overview of the epidemiological literature on post-TB lung impairment and link it to data on the pathogenesis of lung injury from the perspective of dysregulated immune responses and immunogenetics.
Short abstract
Host factors driving lung injury in TB likely contribute to variable patterns of pulmonary impairment after TB http://ow.ly/a3of30hBsxB
Introduction
A third of the world's population is infected with Mycobacterium tuberculosis (MTB), and over 9 million new cases of tuberculosis (TB) are reported annually [1]. Treatment of drug-susceptible pulmonary TB is highly effective, with 85% (66 million cases) of reported cases estimated to have been successfully treated between 1995 and 2015 [1]. However, up to half of TB survivors have some form of persistent pulmonary dysfunction despite microbiologic cure [2–5]. Pulmonary dysfunction, ranging from minor abnormalities to severe breathlessness, can increase the risk of death from respiratory causes [6–9]. Furthermore, treated TB patients appear to contribute substantially to the growing worldwide burden of chronic obstructive pulmonary disease (COPD) [10–12]. These findings call for strategies to address pulmonary impairment after TB (PIAT).
A notable feature of lung involvement in TB is its striking heterogeneity. This is observed on formal lung function testing in terms of the magnitude of pulmonary function, ranging from no impairment to severe dysfunction [3, 7, 8] and the specific types of ventilatory defects [3, 11, 13]. Patients may present with cavitation, fibrosis or nodular infiltrates, or have a mix of these pulmonary pathologies [14, 15]. This immense variability may relate to host–pathogen interactions and the diverse immunological events that can follow. We also hypothesise that heterogeneity in lung damage may be partially attributed to variation in genes coding for or regulating host immune responses. Elucidating the immune pathways and genetic risk factors for TB-associated lung injury could inform therapies that specifically target immunological factors responsible for lung injury.
This review summarises the epidemiology of PIAT, examines TB-associated lung pathology potentially linked to lung dysfunction, and reviews the immunological and plausible genetic correlates of lung tissue damage in TB. We also describe several processes, such as pulmonary cavitation, fibrosis and bronchiectasis, which probably contribute collectively to lung remodelling in TB and PIAT. These terms are defined in table 1.
TABLE 1.
Definitions for processes contributing to lung remodelling during pulmonary tuberculosis (TB) and pulmonary impairment after TB
| Term | Definition |
| Pulmonary cavitation | Process by which normal pulmonary tissue is obliterated, becoming gas-filled spaces or cavities in the lung. This process initially involves caseous necrosis of lipid pneumonia lesions, producing caseous pneumonia. During caseation, alveolar cells and septa are destroyed along with neighbouring vessels and bronchi. Cavities form when these regions of caseous pneumonia liquefy, fragment and are released upon coughing. |
| Pulmonary fibrosis | Results from long-term lung tissue injury that is characterised by excessive extracellular matrix deposition in the lung. Replacement of normal lung parenchyma with collagenous tissue results in architectural changes in the lung, such as thickening and stiffening of the lung walls. |
| Bronchiectasis | Manifests as irreversible bronchial dilatation and thickening of the bronchial wall. Elastic and muscular components of the bronchial wall are destroyed in bronchiectasis. Bronchial dilatation associated with bronchiectasis in TB may be due to multiple factors, including traction from surrounding tissue fibrosis, caseous necrosis that makes its way into the bronchi, and elevated luminal pressure due to coughing. Bronchiectasis can also predispose to recurrent exacerbations of purulent sputum production and possibly bacterial pneumonia in subsequent years. |
| Pulmonary impairment after TB | A broad term we use in this review to refer to lung dysfunction that includes airflow obstruction, restrictive ventilatory defects and impaired gas exchange. Pulmonary impairment after TB is probably downstream of a wide variety of lung remodelling events, some of which are described above. Given the lung's considerable reserve, these structural changes may manifest as symptoms and pulmonary disability over a period of time. |
Search strategy
For this review we identified references in PubMed that were published up to May 2017. We specifically searched for studies describing the epidemiology of impaired lung function post-TB treatment using the search terms “epidemiology”, “pulmonary tuberculosis”, “pulmonary function”, “obstruction AND/OR restrictive”, “bronchiectasis”, “fibrosis”, “cavitation” and “TB treatment”. For studies on lung pathology and mediators of inflammation in TB we used the terms “pulmonary tuberculosis”, “lung pathology”, “immunopathology”, “matrix metalloproteinase”, “inflammatory biomarkers OR inflammation”, “neutrophils” and “CD4 T cells”. Genetic studies were queried using the terms “pulmonary tuberculosis”, “genetics”, “COPD” and “idiopathic pulmonary fibrosis”. Relevant articles published in English that resulted from the searches, and references cited therein, were reviewed.
PIAT
Epidemiology
Initial studies conducted among untreated or incompletely treated TB patients highlighted that lung disability was a relatively common outcome [16, 17]. Many studies since have reported on lung impairment at TB treatment completion [5, 7, 8, 18], with persistence of defects several years post cure (table 2) [2, 4, 13]. For example, a South African study observed airflow obstruction in 68% of patients with a history of TB treated up to 16 years (mean 5.6 years) prior to assessment [13]. Although longitudinal studies have shown improvement in pulmonary function with TB treatment, a considerable proportion of patients have irreversible and often progressive pulmonary defects [3, 4, 7, 8, 20]. In a prospective study of 74 hospitalised patients with newly diagnosed TB, 54% had improved lung function with treatment and the rest had either no change or worsening pulmonary function [3]. Even in the outpatient setting, where patients are presumably healthier than those who are hospitalised, a quarter [7] to one-third [8] of the patients had moderate-to-severe airway limitation at treatment completion. Other groups have corroborated these findings in multiple other settings [5, 19, 22, 23]. A limitation of many of the studies described above, however, was their small-to-moderate sample size (study-specific limitations are described in table 2).
TABLE 2.
Summary of epidemiological studies investigating pulmonary impairment after tuberculosis (TB)
| First author [ref.] | Type of study | Setting | Sample size n | Exposure | Outcome | Association/finding | Major limitation |
| Akkara [ 18 ] | Cross-sectional | India | 257 | Treated TB (2 weeks post-treatment completion) |
Airflow obstruction measured by FEV1 and FVC | Airflow obstruction in 86.8% of patients | Lung impairment before TB treatment initiation was not measured to relate to lung impairment after treatment completion and determine causality. Long-term lung disability was not assessed.# |
| Willcox [ 13 ] | Cross-sectional | South Africa | 71 | History of TB (up to age 16 years) |
Airflow obstruction defined as RV >120% pred and/or FEV1/FVC ratio <70% pred with TLC >80% of pred | Obstruction in 68% of patients Obstruction with some restriction in 20% Non-obstructive decrease in lung volume in 17% |
Lung impairment before TB treatment initiation was not measured to relate to lung impairment after treatment completion and determine causality. Lung function was evaluated only in patients who could be traced after several years of attending a TB clinic. Selection of patients in this way may have contributed to survivor bias and underestimated lung dysfunction. |
| Manji [ 19 ] | Cross-sectional | Tanzania | 501 | Treated TB (20 weeks of anti-TB therapy) | Airflow defects measured by FEV1 and FVC | Lung impairment in 74% of patients Obstruction in 42% Restriction in 13% Mixed pattern in 19% | Lung impairment before TB treatment initiation was not measured to relate to lung impairment after treatment completion and determine causality. Long-term lung disability was not assessed.# |
| Hnizdo [ 2 ] | Retrospective | South Africa | 27 660 | History of 1, 2 or ≥3 episodes of TB | Airflow obstruction defined as FEV1 <80% | Prevalence of airflow obstruction after 1 episode of TB (18.4%), 2 episodes of TB (27.1%) and ≥3 episodes of TB (35.2%) Lung impairment is greatest in the first 6 months following TB diagnosis and stabilises 6 months post-TB treatment completion |
Only male mine workers were assessed. |
| Ross [ 4 ] | Matched retrospective | South Africa | 185 TB cases versus 185 age-matched controls without history of TB | History of TB | Lung function loss over time measured by FEV1 and FVC | History of TB was associated with an adjusted mean loss of 40.3 mL·year−1 in FEV1 (95% CI 25.4–55.1) and 42.7 mL·year−1 in FVC (95% CI 27–58.5) compared to controls |
Only male mine workers were assessed. Patients were included in the study only if they were still working in the mines at follow-up, nearly 4.5 years after baseline measures. Several subjects had left the mines by follow-up. Selecting only those still working at the mines may have contributed to survivor bias and underestimated lung function. |
| Rhee [ 20 ] | Retrospective | Republic of Korea | 595 | Destroyed lung resulting from a past history of TB | Lung function loss measured by FEV1 and FVC | Lung impairment after TB in 76.8% of patients | Cohort consisted of hospitalised TB patients with destroyed lungs, thereby limiting the generalisability of findings to less advanced patients. PFTs were not standardised. |
| Plit [ 3 ] | Prospective cohort | South Africa | 74 | TB treatment | Lung function at the end of TB treatment | 54% of patients had an improvement in lung function 28% of patients had obstructed airflow 24% of patients had restricted airflow Only study to date that has investigated an association between inflammation and lung function: elevated C-reactive protein correlated with decreased FEV1 % after TB treatment completion, independent of smoking |
Cohort consisted of hospitalised patients with severe TB, thereby limiting the generalisability of findings to less advanced patients. Long-term lung disability was not assessed.# |
| Maguire [ 7 ] | Prospective cohort | Indonesia | 69 | TB treatment | Lung function over the course of TB treatment | Lung function improved over the course of TB treatment; however, 25% of the patients had residual moderate-to-severe TB (FEV1 <60%) at treatment completion | Study was restricted to 69 of 115 patients who attended all follow-up visits. Those included were more likely to have been cured and had better lung function at diagnosis compared to those not included. This may have underestimated the extent of lung dysfunction among patients with a history of TB. Long-term lung disability was not assessed.# |
| Ralph [ 8 ] | Prospective cohort | Indonesia | 200 | TB treatment | Lung function over the course of treatment and at treatment completion | 47% of TB patients had moderate-to-severe pulmonary impairment at baseline 27% of TB patients had residual moderate-to-severe pulmonary impairment at the end of treatment |
Long-term lung disability was not assessed.# |
| Pasipanodya [ 5 ] | Case–control | USA | 107 active TB cases versus 210 latent TB controls | Treated TB (20 weeks of anti-TB therapy) | Airway obstruction defined as FEV1/FVC <70% pred and FVC >80% pred | TB patients on anti-TB therapy have significantly higher odds of pulmonary impairment versus controls with latent TB, OR 5.4 (95% CI 2.98–9.68) | Lung impairment before TB treatment initiation was not measured to relate to lung impairment at treatment completion and determine causality. Long-term lung disability was not assessed.# |
| Amaral [ 10 ] | Cross-sectional, population-based study of adults | 18 high and low-/middle-income countries | 14 050 | History of TB | Airflow defects: obstruction defined as post-bronchodilator FEV1/FVC less than LLN; restriction defined as post-bronchodilator FVC less than LLN | Obstruction: adjusted OR 2.51 (95% CI 1.8–3.42) Restriction: adjusted OR 2.31 (95% CI 1.42–3.19) |
Self-report of TB was used to determine association with airflow obstruction. This approach may have resulted in recall bias. |
| Menezes [ 12 ] | Cross-sectional, population-based | 5 Latin American cities | 5571 patients; 132 with a diagnosis of TB | History of TB | COPD | Prevalence of COPD in 30.7% versus 13.9% comparing those with and without history of TB, respectively Smoking adjusted OR 2.33 (95% CI 1.5–3.62) |
History of TB was not confirmed by medical records. Lung function was not measured |
| Lee [ 21 ] | Retrospective | Taiwan | 3176 pulmonary TB cases versus 15 880 matched controls | History of TB | COPD | History of TB is an independent risk factor of COPD (HR 2.05, 95% CI 1.77–2.39) | Patients were considered to have a history of TB and COPD based on medical treatment records. Lung function was not measured. |
| Byrne [ 11 ] | Systematic review and meta-analysis | Multiples countries | History of TB | COPD | History of TB was significantly associated with COPD in adults over 40 years (pooled OR 3.05, 95% CI 2.42–3.85) | All studies included in the meta-analysis were cross-sectional. Thus, precluding determination of a temporal and causal effect of TB on COPD. |
FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity; RV: residual volume; TLC: total lung capacity; PFT: pulmonary function test; LLN: lower limit of normal; COPD: chronic obstructive pulmonary disease. #: the study by Hnizdo et al. [2] demonstrated that lung impairment peaks 6 months after diagnosis, but improves 6 months post-treatment completion before stabilising to become chronic. These studies determined lung function at treatment completion, thus their findings may not represent residual lung impairment.
An increasing number of population-based studies have demonstrated that a history of TB increases risk for airflow obstruction and COPD [10–12, 22]. A study of 14 050 patients from 18 countries revealed that a history of TB increased risk for obstructive airway disease by 2.5-fold independent of smoking and other clinical factors [10]. Another study (n=5571) showed a higher prevalence of COPD in those with a history of TB (30.7%) versus those without (13.9%) [12]. In a large study of 13 522 adults aged ≥40 years set in South Korea, a history of TB and lesions on chest radiographs were associated with 4.47 increased odds of airflow obstruction (95% CI 3.07–6.51) after adjusting for age, smoking, body mass index (BMI) and other confounders [24]. Furthermore, a meta-analysis demonstrated that a history of treated TB was a risk factor for COPD (pooled OR 3.05, 95% CI 2.42–3.85) independent of smoking and age [11].
Risk factors associated with PIAT have not been fully elucidated and the relationships are probably complicated. It has been suggested that smoking, which is an established risk factor for COPD, may contribute to PIAT [2, 3, 5]. However, some reports have found no such association [4, 7, 8]. For example, in one study individuals with a history of TB were twice as likely to be current smokers than those in the non-TB group; yet, greater lung dysfunction over time in the TB group was independent of smoking in a multivariate analysis [4]. A similar lack of association between smoking and impaired lung function was observed among patients completing TB treatment in Indonesia [7, 8]. HIV co-infection may be an additional risk factor for lung function decline. Several studies have now shown that HIV-infected patients are at increased risk for impaired gas exchange as well as airway obstruction [25–27]. However, data are conflicting and sparse with respect to lung function in HIV/TB co-infected patients [2, 8]. Other risk factors for poor lung function after TB may include comorbidities such as diabetes, as well as environmental factors like indoor smoke from biomass fuels. Although these risks have been linked to COPD [26, 28], they remain to be investigated in the context of post-TB lung disability.
Variability in lung function deficits
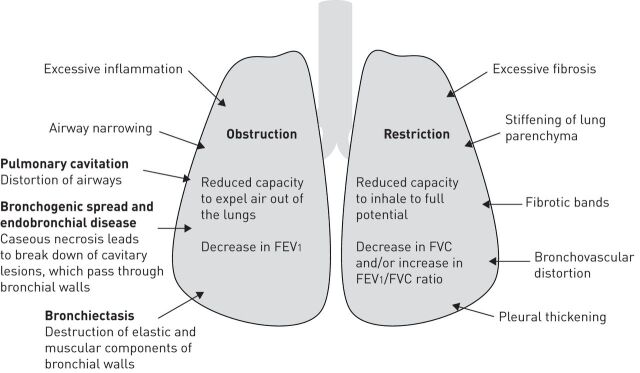
PIAT can involve airflow obstruction and/or restrictive ventilatory defects, as well as impairment in gas exchange (figure 1) [3, 11, 13, 15, 20]. Airflow defects can be detected by spirometry, which quantitates the flow and volume of air inhaled and exhaled [29]. Impaired gas exchange is determined by measuring the diffusing capacity of the lung for carbon monoxide (DLCO) [30]. The American Thoracic Society and the European Respiratory Society provide standardised guidelines on conducting and interpreting these tests [30–32]. Airflow obstruction is associated with decreased capacity to completely expel air out of the lungs and is probably due to inflammation-induced narrowing of airways. In contrast, restriction is probably linked to the reduced ability to inhale fully resulting from extensive fibrosis and stiffening of the lung parenchyma. Lung manifestations of pneumonia are mediated, in part, by immune mechanisms [14, 33], and so heterogeneity in pulmonary deficits in TB may be linked to variability in the host's response to MTB.
FIGURE 1.
Mechanisms and radiographic features associated with airflow obstruction and restrictive ventilatory defects in patients with a history of tuberculosis. FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity.
Airflow obstruction
Symptoms associated with airflow obstruction include dyspnoea, reduced exercise capacity and chronic bronchitis [34]. The magnitude of airway obstruction is commonly quantified by measuring the forced expiratory volume in 1 s (FEV1) [32]. FEV1 is reported as both an absolute volume and as a percentage of predicted normal [32], with a 100 mL decrease in FEV1 being considered clinically significant [35]. Several studies have observed a decline in FEV1 during and after TB treatment [3, 7, 8, 11, 13, 20]. A Korean study found a mean FEV1 decline of 38.2±8 mL·year−1 [20] in cured TB patients that was consistent with the rate of reduction in FEV1 over time (33±2 mL·year−1) in COPD patients without TB [20]. Comparable rates of FEV1 decline were observed in a study comparing patients with a history of TB to age-matched controls [4]. Additionally, a study in Indonesia (n=200) found moderate-to-severe (FEV1 <60% pred) airflow obstruction in approximately half the patients at baseline and determined only a small improvement of 14.8% in % FEV1 with treatment [8].
Decline in FEV1 may be linked to multiple underlying pathological mechanisms (figure 1). Pulmonary cavitation may obliterate or distort airways, leading to airflow obstruction. In a study of serial changes in lung structure and pulmonary function, patients with cavities had significantly lower FEV1 at baseline and at 1 month post-TB treatment initiation compared to patients without cavities [15]. Additionally, bronchogenic spread is a hallmark of pulmonary TB, where caseous material released during cavitary disintegration passes through the bronchial walls [14, 36–38]. Furthermore, destruction of elastic and muscular components of the bronchial walls resulting in bronchiectasis, which is associated with airflow obstruction [39], was detected more frequently in patients with cavities (64%) than those without (11%) [15]. Bronchiectasis is a permanent distortion of airways that predisposes to lifelong morbidity with recurrent episodes of purulent sputum production, haemoptysis and sometimes progression to pneumonia [40]. Bronchiectasis as a sequela of pulmonary TB has been long recognised [41] and can persist or worsen despite TB treatment completion [42]. Post mortem autopsy studies of TB patients found bronchiectasis in 19–65% of those examined [43, 44]. It is alarming to note that in one study, conducted more recently, 86% patients had cylindrical bronchiectasis 6 months post-TB treatment on chest computed tomography (CT) [45]. Consistently, a systematic review reported the prevalence of bronchiectasis post-TB to be 35–86% in the five CT studies they assessed [46]. Furthermore, a population-based study of >10 000 adults in China revealed that having a history of TB increased the odds of having a diagnosis of bronchiectasis three-fold compared to those without previous TB (OR 3.07, 95% CI 1.89–4.98) [47]. However, our understanding of the mechanisms that drive such structural changes and associated airflow obstruction following TB are poor.
Restrictive ventilatory defects
Patients also suffer from restricted airflow [3, 13, 18, 19], where symptoms commonly include chest pain, cough and shortness of breath. Restriction is defined either as a decrease in forced vital capacity and/or an increase in the FEV1/forced vital capacity ratio [32]. In one study, restriction was detected at baseline and at the end of TB treatment in 57% and 24% of patients, respectively; however, further longitudinal analyses were not performed in this study [3]. Although airflow obstruction in TB has received the greatest attention, mixed patterns of airflow obstruction/restrictive ventilatory defects was the most common form of lung dysfunction in a review of population-based and observational studies conducted in South Africa [48]. Structural changes in the lung resulting from aberrant lung tissue repair (e.g. bronchovascular distortion, fibrotic bands and pleural thickening) [15, 20, 49] may explain airflow restriction in TB patients.
Impaired diffusing capacity and ventilation/perfusion mismatch
There is also evidence for impaired gas exchange early in TB disease [50, 51]. Decrease in DLCO is probably due to reduction in surface area for gas exchange following alveolitis or “lipoid pneumonia”, which occurs during cavitation (described in the Granulomas to cavitation during TB section). Although DLCO improves with treatment, some individuals may have permanently impaired diffusion and ventilation/perfusion mismatch, resulting in chronic hypoxaemia [15, 52]. Long-term oxygen therapy is known to improve outcomes in COPD patients with severe chronic hypoxaemic respiratory failure [53, 54]. Currently there is little information on the prevalence of severe hypoxaemia in TB survivors.
Mediators of lung damage and dysfunction in TB
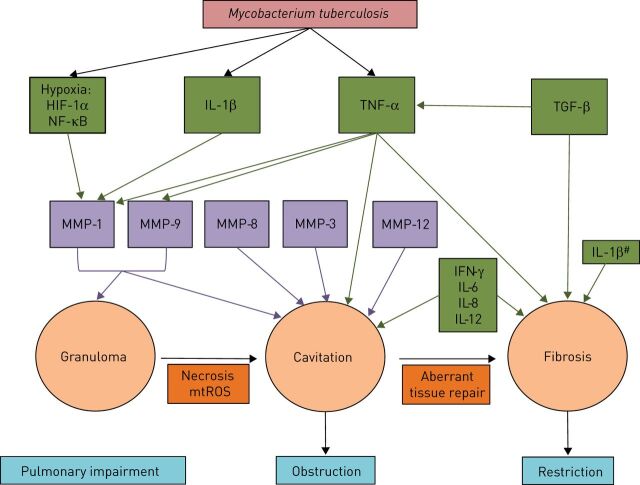
Targeted treatment of TB-associated lung impairment requires knowledge of the precise mechanisms of immune pathology. A major barrier to studying TB immunopathogenesis longitudinally in humans is that serial lung biopsies through disease progression and treatment, which could be used to determine local immune pathways involved in tissue injury, are nearly impossible to obtain. Thus, our current understanding of the immunological basis for lung tissue injury in TB derives largely from animal models. Although TB in non-human primates and certain aspects of disease in other animal models are similar to human disease [55, 56], no single model recapitulates the entire spectrum of human lung pathology [14]. Nevertheless, human studies and data from animal models provide compelling evidence for the crucial role of the host's immune response to MTB in lung remodelling (summarised in figure 2). Such host–pathogen interactions may persist even after treatment completion. For example, a recent longitudinal study using positron emission tomography and CT to evaluate local lung inflammation in pulmonary TB patients demonstrated that many patients have enhancement and/or development of new inflammatory lesions despite 6 months of anti-TB therapy and following 1 year of treatment completion [57]. Moreover, patients deemed culture negative at the end of treatment were found to have MTB mRNA in respiratory fluids, suggesting persistent bacterial transcription may fuel inflammatory reactions in the lung [57]. Although this study did not conduct formal lung function tests, patients had signs and symptoms consistent with lung impairment [57].
FIGURE 2.
Immune mediators of tissue remodelling and lung function impairment in tuberculosis. Transcription factors, cytokines and chemokines that drive expression of tissue-degrading enzymes or directly mediate cavitation and/or fibrosis are shown in green. Matrix metalloproteinases (MMP) that promote granuloma and cavitation are depicted in purple. HIF: hypoxia inducible factor; NF: nuclear factor; IL: interleukin; TNF: tumour necrosis factor; TGF: transforming growth factor; IFN: interferon; mtROS: mitochondrial reactive oxygen species. #: IL-1β regulates fibrogenesis in idiopathic pulmonary fibrosis and may play a role in tuberculosis. Pathological processes contributing to the progression of lesions may influence the development of airflow obstruction and restrictive ventilatory patterns of pulmonary impairment.
We also hypothesise that while certain immunological mechanisms may specifically drive TB-associated airflow obstruction or restrictive ventilatory impairment, many patients could have considerable overlap. Immune mediators and pathways that perhaps drive necrosis and cavitation during TB may also set up for subsequent fibrosis. These immunological factors could potentially be targeted to prevent airflow obstruction and/or restrictive ventilatory defects after TB.
Granulomas to cavitation during TB
The host's immune system responds to the invading mycobacterium and triggers granuloma formation during primary infection [14, 58]. A granuloma is a highly organised structure consisting of many immune cell types (e.g. macrophages, neutrophils, natural killer cells and T- and B-cells) that surround a caseous necrotic core of MTB-infected alveolar macrophages [33, 58]. The granuloma is traditionally thought to be host-protective by sequestering and preventing dissemination of MTB, but studies using the zebrafish model for TB have demonstrated that granulomas can be conducive to MTB proliferation and spread [59, 60]. Moreover, there appears to be substantial heterogeneity in the bacterial load, size and inflammatory profile between granulomatous lesions within a single host based on recent non-human primate studies [61–63]. It has been shown that a single or few granulomas that fail to control mycobacterial proliferation can dramatically influence disease progression and clinical outcome [64].
A widely held view, based on data from animal models, is that these granulomas coalesce and breakdown via liquefactive necrosis, leaving behind a cavity during active disease [56, 65]. However, human studies suggest that cavities originate from lipid pneumonia during post-primary TB [14, 66]. These lipid pneumonia lesions may develop into areas of caseous pneumonia as a result of caseous necrosis [14, 66]. During caseous necrosis, alveolar cells are destroyed, along with nearby structures such as vessels and bronchi [14]. However, elastic fibres of the alveolar walls and vessels appear to remain intact [14, 67]. This necrotic tissue begins to soften and fissure and is eventually coughed out [14, 67]. Gas-filled spaces surrounded by a collagen capsule in turn replace normal lung tissue following cavitation.
Although the precise immune mechanisms underlying liquefactive or caseous necrosis are not fully understood, robust immune responses probably play a significant role [68, 69]. Initial evidence for this comes from Robert Koch's observations over a century ago. He noted that when guinea pigs previously infected with MTB are rechallenged, they develop necrotic lesions that expand in circumference at the site of cutaneous injection [70]. The Koch Phenomenon has been described by others [71], including Moreira et al. [72], where MTB-infected mice were treated with a recombinant bacillus Calmette–Guerin (BCG) vaccine that released cytokines (e.g. tumour necrosis factor (TNF)-α) shown to reduce bacterial burden in a pre-infection vaccine model. Paradoxically, post-infection treatment with BCG–TNF-α exacerbated lung pathology without decreasing MTB load in these mice [72]. Furthermore, Shwartzman [73] found that rabbits previously injected with Gram-negative bacteria in the skin developed haemorrhagic necrosis at the initial site of injection following an intravenous injection of the same bacteria 24 h later. This reaction may be explained, in part, by T-cell mediated MTB-specific immune responses, given that depleting CD4+ T-cells in pre-immunised mice inhibited this reaction [74]. This study also highlighted an important role for TNF-α in perpetuating necrosis [74]. Other studies have corroborated these findings [75]. In addition to an excessive and tissue-damaging immune response directed towards viable and nonviable mycobacteria [65, 76], dysregulation of host lipid metabolism has recently been hypothesised to influence caseous necrosis [77]. We expand our discussion on possible immune mechanisms underlying lung pathology and dysfunction in the sections below.
Regardless of the way granulomas and cavities form, they can have variable trajectories of resolution through the course of disease or treatment, and may undergo abnormal repair resulting in focal or extensive tissue fibrosis [14, 78]. Thus, it is plausible that host immune responses that drive inflammation, cavitation and fibrosis contribute to the variable patterns of lung healing, manifesting as persistent airflow obstruction and/or restrictive ventilatory defects. Additionally, differences in the quality and quantity of immune effector responses underlying these processes may also contribute to variability in PIAT.
Matrix metalloproteinases
Matrix metalloproteinases (MMPs) are a family of 25 potent proteases that can degrade extracellular matrix components [79] and are probably central to TB-associated lung injury. MMPs can promote different stages of lung remodelling during TB [80]. Transcriptomic analyses of lesion biopsies from TB patients showed dramatic upregulation of tissue damaging networks that included MMP-1 and MMP-9 gene expression [81]. Furthermore, TB patients with chest radiographs showing extensive lung involvement had 8.5-fold higher levels of MMP-1 in their bronchoalveolar lavage (BAL) versus patients with less lung involvement [82]. Consistent with this, transgenic mice expressing human MMP-1 had greater alveolar wall damage and matrix destruction following MTB infection versus wild-type mice [82]. A recent imaging study revealed that TB lesions in humans are severely hypoxic [83]. Reproducing hypoxia in in vitro culture conditions resulted in upregulation of MMP-1 in MTB-infected cells via hypoxia-inducible factor and nuclear factor (NF)-κB activation [83]. Collectively, these studies suggest an important role for MMP-1 in lesion progression during TB that plausibly occurs upstream of lung impairment.
MMPs are tightly regulated at the level of transcription and proteolytic maturation, as well as by tissue inhibitors of metalloproteinases (TIMPs) [84]. In a rabbit model for cavitary TB disease, MTB was shown to drive an imbalance in MMP-1 and its specific inhibitor, TIMP-3, which associated with the progression of consolidated regions in the lungs to cavities [85]. Also, dysregulation in MMPs/TIMPs was demonstrated in the plasma [84] and respiratory fluids [82] of patients with active TB. Thus, uninhibited MMP expression and activity may lead to tissue destruction that ultimately contributes to PIAT.
Multiple other MMPs have been implicated in perpetuating TB-associated lung injury. For example, neutrophil-derived MMP-8 and -9 were associated with cavitary disease in TB patients [86]. In a pilot study of advanced HIV/TB co-infected patients, rapid increase in MMP-8 levels following antiretroviral therapy (ART) initiation was associated with impaired lung function nearly 2 years after TB treatment completion [87]. These preliminary findings are in line with the tissue destructive role of MMP-8 [87]. MMP-3 [82] and -12 [88] may also induce lung injury during TB. Although TB treatment appears to decrease sputum MMP-1, -3 and -8, they do return to normal levels [89]. Several other proteases such as neutrophil-associated elastase, proteinase-3 and cathepsin G have also been linked to matrix degradation in COPD and may participate in destroying lung tissue during TB [90]. Taken together, it is conceivable that a complex network of MMPs and other proteases mediate TB-associated lung injury with long-term impact on lung function.
Inflammatory cytokines
Few studies have directly investigated the relationship between inflammation and lung function in TB. A study by Plit et al. [3] demonstrated that elevated C-reactive protein, which is a non-specific inflammatory marker, correlated with decreased FEV1 in TB patients after treatment completion. In clinical trials of adjunctive corticosteroid versus standard therapy alone for TB [91–93], lung disability was generally the same between groups; however, steroid administration increased vital capacity in one report [93]. It should be noted that adjunctive steroid treatment in TB patients has been associated overall with a trend towards improved clinical outcome [94–96], but its prolonged use at higher doses should be approached with caution given the long-term cardiovascular and metabolic risks. Furthermore, corticosteroids broadly suppress inflammation by inhibiting NF-κB signalling [97, 98], which regulates the expression of several cytokines including interleukin (IL)-1, IL-2, IL-6, IL-8, TNF-α and interferon (IFN)-γ. Thus, preventing or treating TB-associated lung impairment may require a more targeted approach.
TNF-α is a key regulator of host immune responses to TB with pleiotropic effects [99]. Intracellular pathogen clearance via macrophage activation is a crucial host-protective role of TNF-α [99, 100]. This cytokine can also promote apoptosis [101]. Apoptosis is a non-inflammatory mode of cell death that eliminates infected cells; however, TNF-α-induced apoptosis appears suboptimal for MTB control [100]. Moreover, MTB can stimulate expression of an inhibitor of TNF-α, soluble TNF-receptor II (sTNF-RII), and evade apoptosis [102]. Low levels of TNF-α may be problematic, as this has been shown to lead to inefficient macrophage activation and reduced microbicidal activity [103]. With uninhibited MTB replication, excessive inflammation and necrosis can ensue [103]. Conversely, elevated TNF-α levels may drive necrosis through the induction of mitochondrial reactive oxygen species, despite reduced MTB growth [103, 104]. The hyper-inflammatory nature of necrotic cell death can ultimately cause cavitation and lung tissue damage. Of note, a higher ratio of TNF-α to sTNF-RI and -RII correlated with larger cavity size [105]. Moreover, TNF-α is necessary for MMP-1 and -9 expression by monocyte–bronchial epithelial cell networks [106, 107]. Taken together, TNF-α perhaps potentiates tissue destruction in multiple ways during TB.
In addition to TNF-α, elevated IL-6, IL-8 and IL-12 levels in the BAL have been correlated with cavities, bronchial wall thickening and fibrotic bands in active TB patients [108]. In another pulmonary TB study, several cytokines were compared between patients classified as early or late responders based on improvement in chest radiographs after 2 or 6 months of TB treatment, respectively [109]. Late responders had higher levels of IL-1β, TNF-α and IFN-γ versus early responders [109], implicating these cytokines in lung tissue injury. Notably, TNF-α levels can rapidly increase following TB treatment [110]. Given that inflammatory cytokines levels are highly dynamic soon after TB treatment initiation [89, 111], lung remodelling is perhaps ongoing during and after TB treatment completion.
Fibrogenic cytokines
Permanent changes in lung architecture after TB may be, in part, due to aberrant wound-healing processes. Excessive collagen deposition and fibrotic scarring can occur through the course of TB disease and treatment [14, 112]. TNF-α may play a role in tissue fibrosis after TB. Treatment of MTB-infected rabbits with etanercept, a TNF-α antagonist, reduced expression of several genes involved in fibrosis and collagen metabolism [113]. Transforming growth factor (TGF)-β is considered the principal mediator of fibrogenesis [114]. Activation of the TGF-β signalling pathway correlated with elevated collagen levels in lung lesions before and during TB treatment [112]. In pleural TB patients, higher TGF-β levels in the pleural fluid associated with greater pleural thickening before and after anti-TB therapy [49]. Additionally, IL-1β has been linked to fibrosis in patients with idiopathic pulmonary fibrosis (IPF), which is a progressive and fatal lung disease characterised by restrictive ventilatory defects [115]. Specifically, an imbalance in IL-1β and its receptor antagonist (IL-1RA) was implicated in propagating a pro-fibrotic milieu in IPF [116]. TB patients were reported to have a similar imbalance in IL-1β and IL-1RA that correlated with enhanced cavity size [105]. Although this study did not evaluate the relationship between IL-1β/IL-1RA imbalance and fibrosis [105], it is plausible that such dysregulation may contribute to aberrant tissue repair in TB patients. Collectively, TNF-α, TGF-β and IL-1β mediated fibrogenesis may contribute to restrictive ventilatory defects in patients with a history of TB and requires further investigation.
Neutrophils and CD4 T-cells
Multiple cell types have been implicated in orchestrating the development and progression of lesions and ultimately lung damage in TB. During primary infection, the first cell type infected with MTB is thought to be the lung-resident alveolar macrophage [14, 117]. These cells release inflammatory cytokines and chemokines upon activation, in turn recruiting both innate (natural killer cells, neutrophils, γ/δ T-cells and dendritic cells) and adaptive immune cells to the site of infection [65, 118]. While these early events are essential for containing the pathogen, dysregulation of immune responses probably drive caseation and cavitation [58, 119]. Evaluating the contribution of each of these cell types in TB-associated lung damage is beyond the scope of this review; however, we will discuss the role of neutrophils and CD4+ T-cells in mediating tissue injury during TB disease.
Studies using murine models of TB have attributed a protective role for neutrophils very early in infection; however, these cells appear to play an adverse role during chronic, poorly controlled TB disease [120–122]. For example, MTB-infected neutrophils were found to facilitate host-protective adaptive immune response by delivering TB antigens to dendritic cells shortly after infection in mice [121]. Depletion of neutrophils led to decreased migration of dendritic cells to lymph nodes, as well as delayed activation and reduced proliferation of naïve TB-specific CD4 T-cells in these mice [121]. In contrast, massive infiltration and accumulation of neutrophils in the lungs is associated with increased pathology later in disease [123–125]. Consistently, depletion of neutrophils reduced lung injury in a hyper-susceptible mouse model of TB [126].
In humans, neutrophils are perhaps the predominant cell type in the lungs that are infected with replicating MTB during active pulmonary TB [127]. Moreover, it has been reported that cavitary lesions in humans are primarily lined by neutrophils [86, 127]. Several different tissue-damaging pathways may be triggered by neutrophils. In one study that examined lung biopsies, the cavity walls stained positive for neutrophils expressing extracellular matrix destroying MMP-8 and -9 [86]. Another study demonstrated that lung pathology resulting from neutrophilic inflammation during TB was dependent on calprotectin (S100A8/A9) secretion by these cells [122]. S100A8/A9 may not only be a surrogate for lung inflammation, but may also stimulate influx of destructive neutrophils to the lungs [122], along with other chemokines such as CXCL5 [128].
There is a growing body of evidence for the induction of neutrophil extracellular traps in TB [129, 130], which could fuel tissue damage and pulmonary dysfunction as observed in other lung diseases [131–133]. Neutrophil extracellular traps are released upon neutrophil activation and function to capture and kill bacteria [134]. They are composed of chromatin fibres, histones and proteases such as myeloperoxidase (MPO), capthesin G and neutrophil-associated elastase [134, 135]. Although these proteases have antimicrobial properties, they can potentially drive severe lung pathology [136–138]. Of note, MMP-8 and calprotectin have recently been found within neutrophil extracellular traps [86, 139]. Collectively, these studies underscore the contribution of inflammatory neutrophils in driving lung injury.
CD4 T-cells mount protective TB-specific responses; however, these cells may perpetuate tissue damage if their responses go unchecked [87, 140]. The association between CD4 T-cells and lung damage is evident from studies of advanced HIV/TB co-infected patients. In one study, HIV/TB patients with CD4 counts <150 cells·μL-1 were five times more likely to have a normal chest radiograph than HIV-negative TB patients [141]. Moreover, ART-mediated reversal of CD4 lymphopenia in advanced HIV/TB patients is associated with incident lung involvement, particularly in those who experience TB-immune reconstitution inflammatory syndrome (IRIS) [142]. In a small study, TB-IRIS and robust CD4 T-cell recovery after ART initiation were associated with lower FEV1 post-TB treatment completion [87]. Mechanistically, TB-specific CD4 T-cells that secrete TNF-α and IFN-γ perhaps trigger multiple downstream pathways and the activation of effectors like MMPs. These responses may converge on excessive inflammation and tissue injury and subsequent lung disability.
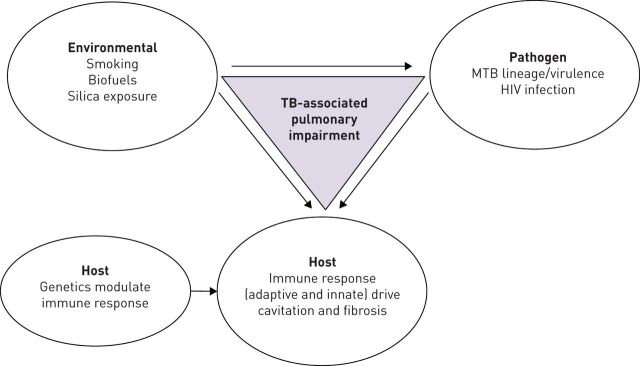
Genetic predisposition for lung injury in TB
Epidemiological and immunological studies point to remarkable heterogeneity in inflammation, lung pathology and pulmonary function among TB patients. Although environmental factors like smoking or exposure to silica among mineworkers [2–4, 7], differences in MTB virulence [143] or HIV co-infection [2, 8, 144] may contribute to this heterogeneity, variation in the host genes that regulate immune response to MTB could also be involved (figure 3). However, the literature is sparse in terms of the genetic correlates of lung damage in TB (table 3). Wang et al. [145] investigated a polymorphic site in the MMP-1 promoter, which can consist of a single guanine nucleotide (1G) or have an insertion of a G (2G). Patients with the MMP-1 1G variant were more likely to have advanced lung fibrosis a year after TB treatment completion [145]. Other groups have demonstrated an association between MMP-1 1G and cavitary disease [146] and TB that is primarily endobronchial [147]. TB patients carrying the MMP-1 1G allele also had an increased risk for tracheobronchial stenosis following treatment [147]. The mechanism underlying lung damage in the MMP-1 1G carriers remains unclear, as it is the MMP-1 2G allele that introduces an Ets transcription binding site and increases MMP-1 expression [167]. In line with the MMP-1 2G variant's functional role, a study found that patients with the MMP-1 2G/2G genotype had a 6.5-fold increased risk of permanent lesions following TB treatment versus patients with other genotypes at this locus [148]. However, this association was only in the presence of an additional variant in the monocyte chemoattractant protein (MCP)-1 promoter (MCP-1 G/G). Patients harbouring both the MCP-1 G/G and MMP-1 2G/2G genotypes had extensive fibrosis and increased prevalence of bronchiectasis at the end of TB treatment [148]. These studies, however, did not assess lung function to relate to genotype and lung pathology.
FIGURE 3.
Conceptual model of factors that potentially contribute to lung impairment after tuberculosis (TB). MTB: Mycobacterium tuberculosis.
TABLE 3.
Immunogenetic studies of lung dysfunction potentially relevant to pulmonary impairment after tuberculosis (TB)
| Biomarker/gene | Polymorphism | Implication on lung pathology/function | Reference |
| TB | |||
| MMP-1 | MMP-1 -1607G (1G) (rs1799750) | Extensive fibrosis after 1 year of TB treatment Cavitary disease Endobronchial TB and tracheobronchial stenosis |
[145–147] |
| MCP-1+MMP-1 | MCP-1 -2518G (G/G) (rs1024611) MMP-1 -1607GG (2G/2G) Guanine insertion at this locus |
Permanent lesions after TB treatment Fibrosis Bronchiectasis |
[148] |
| TOLLIP | TOLLIP rs5743899 rs3750920 |
Decreased TOLLIP mRNA expression Increased inflammatory cytokine expression Increased risk for TB |
[149] |
| COPD | |||
| MMP-1+MMP-12 | MMP-1 2G+MMP-12 nsSNP (rs652438) |
Increased rate of lung function decline | [150] |
| MMP-9 | MMP-9 -1562C/T | Increased risk of COPD in a Korean population | [151] |
| MMP-12 | MMP-12 rs652438 and rs2276109 |
Severe (GOLD stage III) and very severe COPD (GOLD IV), lower FEV1 % | [152] |
| TIMP-2 | TIMP-2 +853G/A -418G/C |
Increased risk for COPD Decreased transcription and stability of mRNA |
[153] |
| TNF-α | TNF-α -308G/A (rs1800629) |
Increased risk of COPD Increased yearly reduction in FEV1 Chronic bronchitis Elevated TNF-α, IL-8, and myeloperoxidase in sputum |
[154,155] |
| IL-8 | IL-8 rs4073 rs2227306 rs2227307 |
Significant decrease in FEV1 and FVC during follow-up of COPD patients | [156] |
| IPF | |||
| TGF-β+TNF-α | TGFβ (rs1800469) +TNF-α (rs361525) |
Additive effect on lung impairment measured as FEV1 | [157] |
| IL-6 | IL-6 -174G/C | Decrease in FEV1 | [158] |
| IL-1RA | IL-1RN +2018C/T (rs419598) Variable number tandem repeat (VNTR)*2 rs2637988 |
Risk for fibrosing alveolitis and IPF Increased susceptibility for IPF Decreased IL-1RA mRNA levels that may predispose to IPF |
[159, 160] |
| TNF-α | TNF-α -308G/A (rs1800629) |
Fibrosing alveolitis risk | [159] |
| IL-6 | IL-6 intron 4A/G | Lower carbon monoxide diffusion | [161] |
| TGF-β | TGF-β Codon 10T/C(rs1982073) Codon 25G/C(rs1800471) |
Decreased gas exchange in IPF patients | [162, 163] |
| MUC5B | MUC5B rs35705950 rs868903 |
Associated with pulmonary fibrosis in genome-wide association studies Increased MUC5B expression |
[164–166] |
| TOLLIP | TOLLIP rs5743890 rs111521887 rs5743894 |
Associated with reduced TOLLIP expression in lung tissue from IPF patients rs5743890 linked to mortality in IPF patients |
MMP: matrix metalloproteinase; MCP: monocyte chemoattractant protein; COPD: chronic obstructive pulmonary disease; TIMP: tissue inhibitor of metalloproteinase; TNF: tumour necrosis factor; IL: interleukin; IPF: idiopathic pulmonary fibrosis; TGF: transforming growth factor; GOLD: Global Initiative for Chronic Obstructive Lung Disease; FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity.
In contrast, studies have intensely interrogated genetic susceptibility for COPD [168]. Given the link between history of TB and COPD, we hypothesise that immunogenetic risk factors associated with COPD may be potential candidates for airflow obstruction after TB. For example, the MMP-1 2G variant discussed above in combination with a single nucleotide polymorphism (SNP) in MMP-12 was associated with accelerated lung function decline in COPD patients [150]. Polymorphisms in MMP-9 and -12, as well as TIMP genes have been linked to COPD and rapid FEV1 decline [151–153, 169]. These variants may be relevant in the context of TB-associated lung impairment and should be examined further.
Variants in inflammatory cytokine genes have also been implicated in COPD. A meta-analysis of 36 studies demonstrated that the TNF-α -308A polymorphism increased risk of COPD in Asians [154]. In addition to being associated with greater yearly decline in FEV1 and chronic bronchitis compared to those without the variant allele, the TNF-α -308A polymorphism was linked to elevated sputum levels of TNF-α, IL-8 and MPO in COPD patients [155]. Gene variants of pro-inflammatory markers such as IL-8 [156], TGF-β [157] and IL-6 [158] have been associated with airflow limitation in COPD. It is yet to be determined if all or any of these common genetic variants play a role in contributing to lung dysfunction in TB.
Immune mechanisms underlying fibrotic interstitial lung diseases, such as IPF, may overlap with those driving fibrogenesis in TB. Thus, it is plausible that common genetic variants implicated in IPF have a role in abnormal tissue repair, impaired gas exchange and restrictive ventilatory defects in TB patients. Notably, variants in the IL-1 receptor antagonist and TNF-α genes have been associated with increased risk of IPF [159, 160]. A SNP in IL-6 has been associated with decline in DLCO in the lungs of IPF patients [161]. Furthermore, SNPs in the TGF-β gene were linked to decreased gas exchange in IPF [162, 163]. Moreover, multiple genome-wide association studies have implicated SNPs in mucin 5B (MUC5B) and TOLLIP, which modulate innate immune responses, in IPF [164–166]. Genetic variation in TOLLIP is particularly interesting, given its role in negatively regulating the TGF-β [170] and Toll-like receptor signalling cascade [149]. TOLLIP deficiency leads to an increase in IL-6 and TNF-α secretion in mice and humans [149, 171]. Furthermore, individuals who harboured the TOLLIP rs5743899 or rs3750920 SNP had diminished TOLLIP mRNA expression, elevated levels of inflammatory cytokines and at an increased risk for TB [149]. However, these SNPs have not been examined in the context of lung pathology in TB or PIAT.
Future directions
It is evident from epidemiological studies that pulmonary impairment is relatively common among patients with a history of TB. Clinical trials investigating new drug regimens for TB should consider including lung function tests to evaluate the impact of these therapies on long-term pulmonary morbidity. Given the variety of lung function abnormalities, management of TB can potentially be pulmonary impairment specific and could target specific underlying immunopathological mechanisms. Furthermore, investigating the role of common variants in TB-associated lung injury may provide insight into the immunopathogenesis of PIAT. Genome-wide association studies combined with global transcriptomic analyses may also reveal novel biomarkers and networks of pathways associated with lung damage in TB.
Therapies that harness the host's immune response to supplement existing anti-TB treatment regimens have garnered interest [172]. Host-directed therapies that block inflammatory effectors and pathways involved in lung damage are a particularly attractive way to reverse lung injury and improve pulmonary function. However, the variability in inflammatory profiles and pulmonary outcomes between patients should be considered when evaluating host-directed therapies, as patients may not all benefit equally from a single treatment option. In fact, Tobin et al. [103] demonstrated that TB-meningitis patients carrying a leukotriene A4 hydrolase (LTA4H) gene variant associated with elevated TNF-α expression benefited the most from dexamethasone adjunctive therapy compared to those without this polymorphism. Personalised adjunctive host-directed therapies could improve TB treatment, where therapies against lung damage are tailored to target specific immune pathways based on the patient's inflammatory and immunogenetic profile. In addition, the potential relative benefit of host-directed therapies targeting elements of the inflammatory response early in the course of TB treatment versus anti-fibrotic therapies during TB resolution is currently unknown. These and other research priorities are detailed in table 4.
TABLE 4.
Summary of key research priorities to address pulmonary impairment after tuberculosis (TB)
| Epidemiological studies |
| Population-based studies that determine the prevalence of: 1) lung function defects by type (airflow obstruction, restrictive ventilatory defects, gas exchange abnormalities, V′/Q mismatch and mixed defects); and 2) lung damage by type (cavitation, fibrosis and bronchiectasis) Investigate risk factors (host, environmental, pathogen) associated with PIAT Measure impact of PIAT on quality of life Determine the prevalence of PIAT and characterise lung deficits in specific patient populations, such as those co-infected with HIV, who have diabetes mellitus or are infected with multidrug-resistant TB |
| Basic/translational science |
| Delineate the immunopathogenesis of pulmonary cavitation, fibrosis and bronchiectasis in pulmonary TB Determine the immunogenetic correlates of hyper-inflammation and tissue damage in pulmonary TB utilising genome-wide association studies similar to those in IPF and COPD Identify key biomarkers or immune pathways as targets for immunomodulation to reduce lung pathology in pulmonary TB |
| Clinical/translational science |
| Diagnosis and diagnostic tests: investigate the utility of chest radiographs, CT, PET-CT, pulse oximetry, 6-min walk test and PFTs prior and post-TB treatment in diagnosing those at increased risk for PIAT Prevention and treatment: Develop effective vaccines to prevent TB and lung tissue damage post infection Develop novel drugs and biologics for TB that not only shorten treatment duration, but also reduce lung tissue injury Investigate the use of adjunctive host-directed therapy to treat TB and associated lung pathology Evaluate the efficacy of the use of common COPD and anti-fibrotic medications in preventing and/or treatment of post-TB lung injury These initiatives would be informed by studies that address the basic/translational science priorities described above |
V′/Q: ventilation/perfusion; PIAT: pulmonary impairment after TB; IPF: idiopathic pulmonary fibrosis; COPD: chronic obstructive pulmonary disease; CT: computed tomography; PET: positron emission tomography; PFT: pulmonary function test.
In conclusion, there is a critical need for translational studies to illuminate the immunopathogenesis of PIAT and inform prevention and therapeutic strategies. Genetic predisposition to pulmonary morbidity after TB should also be evaluated for a comprehensive understanding of this important outcome.
Disclosures
G.P. Bisson ERR-0077-2017_Bisson (1.2MB, pdf)
S. Ravimohan ERR-0077-2017_Ravimohan (1.2MB, pdf)
Footnotes
Support statement: This study was supported by the National Center for Advancing Translational Sciences (KL2TR001879) and the National Institute of Allergy and Infectious Diseases (R01AI120821) of the National Institutes of Health. Funding information for this article has been deposited with the Crossref Funder Registry.
Conflict of interest: Disclosures can be found alongside this article at err.ersjournals.com
Provenance: Submitted article, peer reviewed.
References
- 1.World Health Organization. Global Tuberculosis Report 2015. 20th edition. Geneva, WHO, 2015. [Google Scholar]
- 2.Hnizdo E, Singh T, Churchyard G. Chronic pulmonary function impairment caused by initial and recurrent pulmonary tuberculosis following treatment. Thorax 2000; 55: 32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Plit ML, Anderson R, Van Rensburg CE, et al. Influence of antimicrobial chemotherapy on spirometric parameters and pro-inflammatory indices in severe pulmonary tuberculosis. Eur Respir J 1998; 12: 351–356. [DOI] [PubMed] [Google Scholar]
- 4.Ross J, Ehrlich RI, Hnizdo E, et al. Excess lung function decline in gold miners following pulmonary tuberculosis. Thorax 2010; 65: 1010–1015. [DOI] [PubMed] [Google Scholar]
- 5.Pasipanodya JG, Miller TL, Vecino M, et al. Pulmonary impairment after tuberculosis. Chest 2007; 131: 1817–1824. [DOI] [PubMed] [Google Scholar]
- 6.Pasipanodya JG, McNabb SJ, Hilsenrath P, et al. Pulmonary impairment after tuberculosis and its contribution to TB burden. BMC Public Health 2010; 10: 259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maguire GP, Anstey NM, Ardian M, et al. Pulmonary tuberculosis, impaired lung function, disability and quality of life in a high-burden setting. Int J Tuberc Lung Dis 2009; 13: 1500–1506. [PubMed] [Google Scholar]
- 8.Ralph AP, Kenangalem E, Waramori G, et al. High morbidity during treatment and residual pulmonary disability in pulmonary tuberculosis: under-recognised phenomena. PLoS One 2013; 8: e80302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schunemann HJ, Dorn J, Grant BJ, et al. Pulmonary function is a long-term predictor of mortality in the general population: 29-year follow-up of the Buffalo Health Study. Chest 2000; 118: 656–664. [DOI] [PubMed] [Google Scholar]
- 10.Amaral AF, Coton S, Kato B, et al. Tuberculosis associates with both airflow obstruction and low lung function: BOLD results. Eur Respir J 2015; 46: 1104–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Byrne AL, Marais BJ, Mitnick CD, et al. Tuberculosis and chronic respiratory disease: a systematic review. Int J Infect Dis 2015; 32: 138–146. [DOI] [PubMed] [Google Scholar]
- 12.Menezes AM, Hallal PC, Perez-Padilla R, et al. Tuberculosis and airflow obstruction: evidence from the PLATINO study in Latin America. Eur Respir J 2007; 30: 1180–1185. [DOI] [PubMed] [Google Scholar]
- 13.Willcox PA, Ferguson AD. Chronic obstructive airways disease following treated pulmonary tuberculosis. Respir Med 1989; 83: 195–198. [DOI] [PubMed] [Google Scholar]
- 14.Hunter RL. Pathology of post primary tuberculosis of the lung: an illustrated critical review. Tuberculosis (Edinb) 2011; 91: 497–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Long R, Maycher B, Dhar A, et al. Pulmonary tuberculosis treated with directly observed therapy: serial changes in lung structure and function. Chest 1998; 113: 933–943. [DOI] [PubMed] [Google Scholar]
- 16.Gaensler EA, Lindgren I. Chronic bronchitis as an etiologic factor in obstructive emphysema; preliminary report. Am Rev Respir Dis 1959; 80: 185–193. [DOI] [PubMed] [Google Scholar]
- 17.Birath G, Caro J, Malmberg R, et al. Airways obstruction in pulmonary tuberculosis. Scand J Respir Dis 1966; 47: 27–36. [PubMed] [Google Scholar]
- 18.Akkara SA, Shah AD, Adalja M, et al. Pulmonary tuberculosis: the day after. Int J Tuberc Lung Dis 2013; 17: 810–813. [DOI] [PubMed] [Google Scholar]
- 19.Manji M, Shayo G, Mamuya S, et al. Lung functions among patients with pulmonary tuberculosis in Dar es Salaam – a cross-sectional study. BMC Pulm Med 2016; 16: 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rhee CK, Yoo KH, Lee JH, et al. Clinical characteristics of patients with tuberculosis-destroyed lung. Int J Tuberc Lung Dis 2013; 17: 67–75. [DOI] [PubMed] [Google Scholar]
- 21.Lee CH, Lee MC, Lin HH, et al. Pulmonary tuberculosis and delay in anti-tuberculous treatment are important risk factors for chronic obstructive pulmonary disease. PLoS One 2012; 7: e37978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de la Mora IL, Martinez-Oceguera D, Laniado-Laborin R. Chronic airway obstruction after successful treatment of tuberculosis and its impact on quality of life. Int J Tuberc Lung Dis 2015; 19: 808–810. [DOI] [PubMed] [Google Scholar]
- 23.Pefura-Yone EW, Kengne AP, Tagne-Kamdem PE, et al. Clinical significance of low forced expiratory flow between 25% and 75% of vital capacity following treated pulmonary tuberculosis: a cross-sectional study. BMJ Open 2014; 4: e005361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choi CJ, Choi WS, Lee SY, et al. The definition of past tuberculosis affects the magnitude of association between pulmonary tuberculosis and respiratory dysfunction: Korea National Health and Nutrition Examination Survey, 2008–2012. J Korean Med Sci 2017; 32: 789–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gingo MR, George MP, Kessinger CJ, et al. Pulmonary function abnormalities in HIV-infected patients during the current antiretroviral therapy era. Am J Respir Crit Care Med 2010; 182: 790–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Zyl Smit RN, Pai M, Yew WW, et al. Global lung health: the colliding epidemics of tuberculosis, tobacco smoking, HIV and COPD. Eur Respir J 2010; 35: 27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gingo MR, He J, Wittman C, et al. Contributors to diffusion impairment in HIV-infected persons. Eur Respir J 2014; 43: 195–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Glaser S, Kruger S, Merkel M, et al. Chronic obstructive pulmonary disease and diabetes mellitus: a systematic review of the literature. Respiration 2015; 89: 253–264. [DOI] [PubMed] [Google Scholar]
- 29.Crapo RO. Pulmonary-function testing. N Engl J Med 1994; 331: 25–30. [DOI] [PubMed] [Google Scholar]
- 30.Macintyre N, Crapo RO, Viegi G, et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J 2005; 26: 720–735. [DOI] [PubMed] [Google Scholar]
- 31.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005; 26: 319–338. [DOI] [PubMed] [Google Scholar]
- 32.Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J 2005; 26: 948–968. [DOI] [PubMed] [Google Scholar]
- 33.Dorhoi A, Kaufmann SH. Pathology and immune reactivity: understanding multidimensionality in pulmonary tuberculosis. Semin Immunopathol 2016; 38: 153–166. [DOI] [PubMed] [Google Scholar]
- 34.Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007; 176: 532–555. [DOI] [PubMed] [Google Scholar]
- 35.Cazzola M, MacNee W, Martinez FJ, et al. Outcomes for COPD pharmacological trials: from lung function to biomarkers. Eur Respir J 2008; 31: 416–469. [DOI] [PubMed] [Google Scholar]
- 36.Hatipoglu ON, Osma E, Manisali M, et al. High resolution computed tomographic findings in pulmonary tuberculosis. Thorax 1996; 51: 397–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murata K, Itoh H, Todo G, et al. Centrilobular lesions of the lung: demonstration by high-resolution CT and pathologic correlation. Radiology 1986; 161: 641–645. [DOI] [PubMed] [Google Scholar]
- 38.Im JG, Itoh H, Shim YS, et al. Pulmonary tuberculosis: CT findings – early active disease and sequential change with antituberculous therapy. Radiology 1993; 186: 653–660. [DOI] [PubMed] [Google Scholar]
- 39.Roberts HR, Wells AU, Milne DG, et al. Airflow obstruction in bronchiectasis: correlation between computed tomography features and pulmonary function tests. Thorax 2000; 55: 198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Milliron B, Henry TS, Veeraraghavan S, et al. Bronchiectasis: mechanisms and imaging clues of associated common and uncommon diseases. Radiographics 2015; 35: 1011–1030. [DOI] [PubMed] [Google Scholar]
- 41.Grancher J. La dilatation des bronches chez les tuberculeux. Gazz Med de Paris 1878; 146. [Google Scholar]
- 42.Ko JM, Kim KJ, Park SH, et al. Bronchiectasis in active tuberculosis. Acta Radiol 2013; 54: 412–417. [DOI] [PubMed] [Google Scholar]
- 43.Jones EM, Peck WM. Relationships between tuberculosis and bronchiectasis; a study of clinical and of post-mortem material. Am Rev Tuberc 1950; 61: 387–398. [DOI] [PubMed] [Google Scholar]
- 44.Salkin D. Tuberculosis as a cause of upper lobe bronchiectasis. Calif Med 1950; 73: 577–580. [PMC free article] [PubMed] [Google Scholar]
- 45.Capone RB, Capone D, Mafort T, et al. Tomographic aspects of advanced active pulmonary tuberculosis and evaluation of sequelae following treatment. Pulm Med 2017; 2017: 9876768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Meghji J, Simpson H, Squire SB, et al. A systematic review of the prevalence and pattern of imaging defined post-TB lung disease. PLoS One 2016; 11: e0161176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhou YM, Wang C, Yao WZ, et al. [The prevalence and risk factors of bronchiectasis in residents aged 40 years old and above in seven cities in China]. Zhonghua Nei Ke Za Zhi 2013; 52: 379–382. [PubMed] [Google Scholar]
- 48.Ehrlich RI, Adams S, Baatjies R, et al. Chronic airflow obstruction and respiratory symptoms following tuberculosis: a review of South African studies. Int J Tuberc Lung Dis 2011; 15: 886–891. [DOI] [PubMed] [Google Scholar]
- 49.Seiscento M, Vargas FS, Antonangelo L, et al. Transforming growth factor β-1 as a predictor of fibrosis in tuberculous pleurisy. Respirology 2007; 12: 660–663. [DOI] [PubMed] [Google Scholar]
- 50.Malmberg R. Gas exchange in pulmonary tuberculosis. II. Review of literature clinical significance and conclusions. Scand J Respir Dis 1966; 47: 277–305. [PubMed] [Google Scholar]
- 51.Pipavath SN, Sharma SK, Sinha S, et al. High resolution CT (HRCT) in miliary tuberculosis (MTB) of the lung: correlation with pulmonary function tests and gas exchange parameters in north Indian patients. Indian J Med Res 2007; 126: 193–198. [PubMed] [Google Scholar]
- 52.Kim MA, Kim SH, Zo JH, et al. Right heart dysfunction in post-tuberculosis emphysema. Int J Tuberc Lung Dis 2004; 8: 1120–1126. [PubMed] [Google Scholar]
- 53.Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. Nocturnal Oxygen Therapy Trial Group. Ann Intern Med 1980; 93: 391–398. [DOI] [PubMed] [Google Scholar]
- 54.Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Report of the Medical Research Council Working Party. Lancet 1981; 1: 681–686. [PubMed] [Google Scholar]
- 55.Flynn JL, Gideon HP, Mattila JT, et al. Immunology studies in non-human primate models of tuberculosis. Immunol Rev 2015; 264: 60–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Helke KL, Mankowski JL, Manabe YC. Animal models of cavitation in pulmonary tuberculosis. Tuberculosis (Edinb) 2006; 86: 337–348. [DOI] [PubMed] [Google Scholar]
- 57.Malherbe ST, Shenai S, Ronacher K, et al. Persisting positron emission tomography lesion activity and Mycobacterium tuberculosis mRNA after tuberculosis cure. Nat Med 2016; 22: 1094–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ramakrishnan L. Revisiting the role of the granuloma in tuberculosis. Nat Rev Immunol 2012; 12: 352–366. [DOI] [PubMed] [Google Scholar]
- 59.Volkman HE, Pozos TC, Zheng J, et al. Tuberculous granuloma induction via interaction of a bacterial secreted protein with host epithelium. Science 2010; 327: 466–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Davis JM, Ramakrishnan L. The role of the granuloma in expansion and dissemination of early tuberculous infection. Cell 2009; 136: 37–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lin PL, Ford CB, Coleman MT, et al. Sterilization of granulomas is common in active and latent tuberculosis despite within-host variability in bacterial killing. Nat Med 2014; 20: 75–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gideon HP, Phuah J, Myers AJ, et al. Variability in tuberculosis granuloma T cell responses exists, but a balance of pro- and anti-inflammatory cytokines is associated with sterilization. PLoS Pathog 2015; 11: e1004603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Martin CJ, Cadena AM, Leung VW, et al. Digitally barcoding Mycobacterium tuberculosis reveals in vivo infection dynamics in the macaque model of tuberculosis. MBio 2017; 8: e00312-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Coleman MT, Maiello P, Tomko J, et al. Early changes by 18fluorodeoxyglucose positron emission tomography coregistered with computed tomography predict outcome after Mycobacterium tuberculosis infection in Cynomolgus macaques. Infect Immun 2014; 82: 2400–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dannenberg AM Jr, Sugimoto M. Liquefaction of caseous foci in tuberculosis. Am Rev Respir Dis 1976; 113: 257–259. [DOI] [PubMed] [Google Scholar]
- 66.Hunter RL, Jagannath C, Actor JK. Pathology of postprimary tuberculosis in humans and mice: contradiction of long-held beliefs. Tuberculosis (Edinb) 2007; 87: 267–278. [DOI] [PubMed] [Google Scholar]
- 67.Grosset J. Mycobacterium tuberculosis in the extracellular compartment: an underestimated adversary. Antimicrob Agents Chemother 2003; 47: 833–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rook GA, al Attiyah R. Cytokines and the Koch phenomenon. Tubercle 1991; 72: 13–20. [DOI] [PubMed] [Google Scholar]
- 69.Dheda K, Booth H, Huggett JF, et al. Lung remodeling in pulmonary tuberculosis. J Infect Dis 2005; 192: 1201–1209. [DOI] [PubMed] [Google Scholar]
- 70.Koch R. Fortsetzung uber ein Heilmittel gegen Tuberculose. Dtsch Med Wochenschr 1891; 17: 101–102. [Google Scholar]
- 71.Taylor JL, Turner OC, Basaraba RJ, et al. Pulmonary necrosis resulting from DNA vaccination against tuberculosis. Infect Immun 2003; 71: 2192–2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Moreira AL, Tsenova L, Aman MH, et al. Mycobacterial antigens exacerbate disease manifestations in Mycobacterium tuberculosis-infected mice. Infect Immun 2002; 70: 2100–2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shwartzman G. Phenomenon of local skin reactivity to Bacillus tuberculosis: I. Skin-preparatory and reacting potencies of tuberculin, O.T., and Bacillus tuberculosis culture filtrates. J Exp Med 1935; 61: 369–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.al Attiyah R, Moreno C, Rook GA. TNFα-mediated tissue damage in mouse footpads primed with mycobacterial preparations. Res Immunol 1992; 143: 601–610. [DOI] [PubMed] [Google Scholar]
- 75.Cardona PJ, Llatjos R, Gordillo S, et al. Towards a “human-like” model of tuberculosis: intranasal inoculation of LPS induces intragranulomatous lung necrosis in mice infected aerogenically with Mycobacterium tuberculosis. Scand J Immunol 2001; 53: 65–71. [DOI] [PubMed] [Google Scholar]
- 76.Yamamura Y, Ogawa Y, Maeda H, et al. Prevention of tuberculous cavity formation by desensitization with tuberculin-active peptide. Am Rev Respir Dis 1974; 109: 594–601. [DOI] [PubMed] [Google Scholar]
- 77.Kim MJ, Wainwright HC, Locketz M, et al. Caseation of human tuberculosis granulomas correlates with elevated host lipid metabolism. EMBO Mol Med 2010; 2: 258–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Barry CE 3rd, Boshoff HI, Dartois V, et al. The spectrum of latent tuberculosis: rethinking the biology and intervention strategies. Nat Rev Microbiol 2009; 7: 845–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Greenlee KJ, Werb Z, Kheradmand F. Matrix metalloproteinases in lung: multiple, multifarious, and multifaceted. Physiol Rev 2007; 87: 69–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Salgame P. MMPs in tuberculosis: granuloma creators and tissue destroyers. J Clin Invest 2011; 121: 1686–1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Subbian S, Tsenova L, Kim MJ, et al. Lesion-specific immune response in granulomas of patients with pulmonary tuberculosis: a pilot study. PLoS One 2015; 10: e0132249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Elkington P, Shiomi T, Breen R, et al. MMP-1 drives immunopathology in human tuberculosis and transgenic mice. J Clin Invest 2011; 121: 1827–1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Belton M, Brilha S, Manavaki R, et al. Hypoxia and tissue destruction in pulmonary TB. Thorax 2016; 71: 1145–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Arpino V, Brock M, Gill SE. The role of TIMPs in regulation of extracellular matrix proteolysis. Matrix Biol 2015; 44–46: 247–254. [DOI] [PubMed] [Google Scholar]
- 85.Kubler A, Luna B, Larsson C, et al. Mycobacterium tuberculosis dysregulates MMP/TIMP balance to drive rapid cavitation and unrestrained bacterial proliferation. J Pathol 2015; 235: 431–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ong CW, Elkington PT, Brilha S, et al. Neutrophil-derived MMP-8 drives AMPK-dependent matrix destruction in human pulmonary tuberculosis. PLoS Pathog 2015; 11: e1004917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ravimohan S, Tamuhla N, Kung SJ, et al. Matrix metalloproteinases in tuberculosis-immune reconstitution inflammatory syndrome and impaired lung function among advanced HIV/TB co-infected patients initiating antiretroviral therapy. EBioMedicine 2016; 3: 100–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Subbian S, Tsenova L, O'Brien P, et al. Phosphodiesterase-4 inhibition combined with isoniazid treatment of rabbits with pulmonary tuberculosis reduces macrophage activation and lung pathology. Am J Pathol 2011; 179: 289–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ugarte-Gil CA, Elkington P, Gilman RH, et al. Induced sputum MMP-1, -3 & -8 concentrations during treatment of tuberculosis. PLoS One 2013; 8: e61333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Owen CA. Roles for proteinases in the pathogenesis of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2008; 3: 253–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Angel JH, Chu LS, Lyons HA. Corticotropin in the treatment of tuberculosis. A controlled study. Arch Intern Med 1961; 108: 353–369. [DOI] [PubMed] [Google Scholar]
- 92.Marcus H, Yoo OH, Akyol T, et al. A randomized study of the effects of corticosteroid therapy on healing of pulmonary tuberculosis as judged by clinical, roentgenographic, and physiologic measurements. Am Rev Respir Dis 1963; 88: 55–64. [DOI] [PubMed] [Google Scholar]
- 93.Malik SK, Martin CJ. Tuberculosis, corticosteroid therapy, and pulmonary function. Am Rev Respir Dis 1969; 100: 13–18. [DOI] [PubMed] [Google Scholar]
- 94.Dooley DP, Carpenter JL, Rademacher S. Adjunctive corticosteroid therapy for tuberculosis: a critical reappraisal of the literature. Clin Infect Dis 1997; 25: 872–887. [DOI] [PubMed] [Google Scholar]
- 95.Critchley JA, Young F, Orton L, et al. Corticosteroids for prevention of mortality in people with tuberculosis: a systematic review and meta-analysis. Lancet Infect Dis 2013; 13: 223–237. [DOI] [PubMed] [Google Scholar]
- 96.Wallis RS. Corticosteroid effects on sputum culture in pulmonary tuberculosis: a meta-regression analysis. Open Forum Infect Dis 2014; 1: ofu020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Auphan N, DiDonato JA, Rosette C, et al. Immunosuppression by glucocorticoids: inhibition of NF-kappa B activity through induction of I kappa B synthesis. Science 1995; 270: 286–290. [DOI] [PubMed] [Google Scholar]
- 98.Scheinman RI, Cogswell PC, Lofquist AK, et al. Role of transcriptional activation of I kappa B alpha in mediation of immunosuppression by glucocorticoids. Science 1995; 270: 283–286. [DOI] [PubMed] [Google Scholar]
- 99.Dorhoi A, Kaufmann SH. Tumor necrosis factor alpha in mycobacterial infection. Semin Immunol 2014; 26: 203–209. [DOI] [PubMed] [Google Scholar]
- 100.Ray JC, Flynn JL, Kirschner DE. Synergy between individual TNF-dependent functions determines granuloma performance for controlling Mycobacterium tuberculosis infection. J Immunol 2009; 182: 3706–3717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Laster SM, Wood JG, Gooding LR. Tumor necrosis factor can induce both apoptic and necrotic forms of cell lysis. J Immunol 1988; 141: 2629–2634. [PubMed] [Google Scholar]
- 102.Fratazzi C, Arbeit RD, Carini C, et al. Macrophage apoptosis in mycobacterial infections. J Leukoc Biol 1999; 66: 763–764. [DOI] [PubMed] [Google Scholar]
- 103.Tobin DM, Roca FJ, Oh SF, et al. Host genotype-specific therapies can optimize the inflammatory response to mycobacterial infections. Cell 2012; 148: 434–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Roca FJ, Ramakrishnan L. TNF dually mediates resistance and susceptibility to mycobacteria via mitochondrial reactive oxygen species. Cell 2013; 153: 521–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tsao TC, Hong J, Li LF, et al. Imbalances between tumor necrosis factor-alpha and its soluble receptor forms, and interleukin-1beta and interleukin-1 receptor antagonist in BAL fluid of cavitary pulmonary tuberculosis. Chest 2000; 117: 103–109. [DOI] [PubMed] [Google Scholar]
- 106.Elkington PT, Green JA, Emerson JE, et al. Synergistic up-regulation of epithelial cell matrix metalloproteinase-9 secretion in tuberculosis. Am J Respir Cell Mol Biol 2007; 37: 431–437. [DOI] [PubMed] [Google Scholar]
- 107.Elkington PT, Emerson JE, Lopez-Pascua LD, et al. Mycobacterium tuberculosis up-regulates matrix metalloproteinase-1 secretion from human airway epithelial cells via a p38 MAPK switch. J Immunol 2005; 175: 5333–5340. [DOI] [PubMed] [Google Scholar]
- 108.Casarini M, Ameglio F, Alemanno L, et al. Cytokine levels correlate with a radiologic score in active pulmonary tuberculosis. Am J Respir Crit Care Med 1999; 159: 143–148. [DOI] [PubMed] [Google Scholar]
- 109.Su WL, Perng WC, Huang CH, et al. Association of reduced tumor necrosis factor α, γ interferon, and interleukin-1β (IL-1β) but increased IL-10 expression with improved chest radiography in patients with pulmonary tuberculosis. Clin Vaccine Immunol 2010; 17: 223–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Bekker LG, Maartens G, Steyn L, et al. Selective increase in plasma tumor necrosis factor-alpha and concomitant clinical deterioration after initiating therapy in patients with severe tuberculosis. J Infect Dis 1998; 178: 580–584. [DOI] [PubMed] [Google Scholar]
- 111.Riou C, Perez Peixoto B, Roberts L, et al. Effect of standard tuberculosis treatment on plasma cytokine levels in patients with active pulmonary tuberculosis. PLoS One 2012; 7: e36886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.DiFazio RM, Mattila JT, Klein EC, et al. Active transforming growth factor-β is associated with phenotypic changes in granulomas after drug treatment in pulmonary tuberculosis. Fibrogenesis Tissue Repair 2016; 9: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Tsenova L, O'Brien P, Holloway J, et al. Etanercept exacerbates inflammation and pathology in a rabbit model of active pulmonary tuberculosis. J Interferon Cytokine Res 2014; 34: 716–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wynn TA. Integrating mechanisms of pulmonary fibrosis. J Exp Med 2011; 208: 1339–1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wilson MS, Madala SK, Ramalingam TR, et al. Bleomycin and IL-1β-mediated pulmonary fibrosis is IL-17A dependent. J Exp Med 2010; 207: 535–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Barlo NP, van Moorsel CH, Korthagen NM, et al. Genetic variability in the IL1RN gene and the balance between interleukin (IL)-1 receptor agonist and IL-1β in idiopathic pulmonary fibrosis. Clin Exp Immunol 2011; 166: 346–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Russell DG, Cardona PJ, Kim MJ, et al. Foamy macrophages and the progression of the human tuberculosis granuloma. Nat Immunol 2009; 10: 943–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Guirado E, Schlesinger LS, Kaplan G. Macrophages in tuberculosis: friend or foe. Semin Immunopathol 2013; 35: 563–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Martin CJ, Carey AF, Fortune SM. A bug's life in the granuloma. Semin Immunopathol 2016; 38: 213–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pedrosa J, Saunders BM, Appelberg R, et al. Neutrophils play a protective nonphagocytic role in systemic Mycobacterium tuberculosis infection of mice. Infect Immun 2000; 68: 577–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Blomgran R, Ernst JD. Lung neutrophils facilitate activation of naive antigen-specific CD4+ T cells during Mycobacterium tuberculosis infection. J Immunol 2011; 186: 7110–7119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Gopal R, Monin L, Torres D, et al. S100A8/A9 proteins mediate neutrophilic inflammation and lung pathology during tuberculosis. Am J Respir Crit Care Med 2013; 188: 1137–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Eruslanov EB, Lyadova IV, Kondratieva TK, et al. Neutrophil responses to Mycobacterium tuberculosis infection in genetically susceptible and resistant mice. Infect Immun 2005; 73: 1744–1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Pichugin AV, Yan BS, Sloutsky A, et al. Dominant role of the sst1 locus in pathogenesis of necrotizing lung granulomas during chronic tuberculosis infection and reactivation in genetically resistant hosts. Am J Pathol 2009; 174: 2190–2201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Repasy T, Martinez N, Lee J, et al. Bacillary replication and macrophage necrosis are determinants of neutrophil recruitment in tuberculosis. Microbes Infect 2015; 17: 564–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Yeremeev V, Linge I, Kondratieva T, et al. Neutrophils exacerbate tuberculosis infection in genetically susceptible mice. Tuberculosis (Edinb) 2015; 95: 447–451. [DOI] [PubMed] [Google Scholar]
- 127.Eum SY, Kong JH, Hong MS, et al. Neutrophils are the predominant infected phagocytic cells in the airways of patients with active pulmonary TB. Chest 2010; 137: 122–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Nouailles G, Dorhoi A, Koch M, et al. CXCL5-secreting pulmonary epithelial cells drive destructive neutrophilic inflammation in tuberculosis. J Clin Invest 2014; 124: 1268–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Repasy T, Lee J, Marino S, et al. Intracellular bacillary burden reflects a burst size for Mycobacterium tuberculosis in vivo. PLoS Pathog 2013; 9: e1003190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ramos-Kichik V, Mondragon-Flores R, Mondragon-Castelan M, et al. Neutrophil extracellular traps are induced by Mycobacterium tuberculosis. Tuberculosis (Edinb) 2009; 89: 29–37. [DOI] [PubMed] [Google Scholar]
- 131.Narasaraju T, Yang E, Samy RP, et al. Excessive neutrophils and neutrophil extracellular traps contribute to acute lung injury of influenza pneumonitis. Am J Pathol 2011; 179: 199–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Grabcanovic-Musija F, Obermayer A, Stoiber W, et al. Neutrophil extracellular trap (NET) formation characterises stable and exacerbated COPD and correlates with airflow limitation. Respir Res 2015; 16: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Dicker AJ, Crichton ML, Pumphrey EG, et al. Neutrophil extracellular traps are associated with disease severity and microbiota diversity in chronic obstructive pulmonary disease. J Allergy Clin Immunol 2018; 141: 117–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Brinkmann V, Reichard U, Goosmann C, et al. Neutrophil extracellular traps kill bacteria. Science 2004; 303: 1532–1535. [DOI] [PubMed] [Google Scholar]
- 135.Kaplan MJ, Radic M. Neutrophil extracellular traps: double-edged swords of innate immunity. J Immunol 2012; 189: 2689–2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Guyot N, Wartelle J, Malleret L, et al. Unopposed cathepsin G, neutrophil elastase, and proteinase 3 cause severe lung damage and emphysema. Am J Pathol 2014; 184: 2197–2210. [DOI] [PubMed] [Google Scholar]
- 137.Cheng OZ, Palaniyar N. NET balancing: a problem in inflammatory lung diseases. Front Immunol 2013; 4: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hoenderdos K, Condliffe A. The neutrophil in chronic obstructive pulmonary disease. Am J Respir Cell Mol Biol 2013; 48: 531–539. [DOI] [PubMed] [Google Scholar]
- 139.Urban CF, Ermert D, Schmid M, et al. Neutrophil extracellular traps contain calprotectin, a cytosolic protein complex involved in host defense against Candida albicans. PLoS Pathog 2009; 5: e1000639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kwan CK, Ernst JD. HIV and tuberculosis: a deadly human syndemic. Clin Microbiol Rev 2011; 24: 351–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Chamie G, Luetkemeyer A, Walusimbi-Nanteza M, et al. Significant variation in presentation of pulmonary tuberculosis across a high resolution of CD4 strata. Int J Tuberc Lung Dis 2010; 14: 1295–1302. [PMC free article] [PubMed] [Google Scholar]
- 142.Meintjes G, Lawn SD, Scano F, et al. Tuberculosis-associated immune reconstitution inflammatory syndrome: case definitions for use in resource-limited settings. Lancet Infect Dis 2008; 8: 516–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Via LE, Weiner DM, Schimel D, et al. Differential virulence and disease progression following Mycobacterium tuberculosis complex infection of the common marmoset (Callithrix jacchus). Infect Immun 2013; 81: 2909–2919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Walker NF, Clark SO, Oni T, et al. Doxycycline and HIV infection suppress tuberculosis-induced matrix metalloproteinases. Am J Respir Crit Care Med 2012; 185: 989–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Wang CH, Lin HC, Lin SM, et al. MMP-1(-1607G) polymorphism as a risk factor for fibrosis after pulmonary tuberculosis in Taiwan. Int J Tuberc Lung Dis 2010; 14: 627–634. [PubMed] [Google Scholar]
- 146.Ninomiya S, Niimi T, Shimizu S, et al. Matrix metalloproteinase-1 polymorphism of promoter region in sarcoidosis and tuberculosis patients. Sarcoidosis Vasc Diffuse Lung Dis 2004; 21: 19–24. [DOI] [PubMed] [Google Scholar]
- 147.Kuo HP, Wang YM, Wang CH, et al. Matrix metalloproteinase-1 polymorphism in Taiwanese patients with endobronchial tuberculosis. Tuberculosis (Edinb) 2008; 88: 262–267. [DOI] [PubMed] [Google Scholar]
- 148.Ganachari M, Guio H, Zhao N, et al. Host gene-encoded severe lung TB: from genes to the potential pathways. Genes Immun 2012; 13: 605–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Shah JA, Vary JC, Chau TT, et al. Human TOLLIP regulates TLR2 and TLR4 signaling and its polymorphisms are associated with susceptibility to tuberculosis. J Immunol 2012; 189: 1737–1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Joos L, He JQ, Shepherdson MB, et al. The role of matrix metalloproteinase polymorphisms in the rate of decline in lung function. Hum Mol Genet 2002; 11: 569–576. [DOI] [PubMed] [Google Scholar]
- 151.Lee SY, Kim MJ, Kang HG, et al. Polymorphisms in matrix metalloproteinase-1, -9 and -12 genes and the risk of chronic obstructive pulmonary disease in a Korean population. Respiration 2010; 80: 133–138. [DOI] [PubMed] [Google Scholar]
- 152.Haq I, Chappell S, Johnson SR, et al. Association of MMP-2 polymorphisms with severe and very severe COPD: a case control study of MMPs-1, 9 and 12 in a European population. BMC Med Genet 2010; 11: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Hirano K, Sakamoto T, Uchida Y, et al. Tissue inhibitor of metalloproteinases-2 gene polymorphisms in chronic obstructive pulmonary disease. Eur Respir J 2001; 18: 748–752. [DOI] [PubMed] [Google Scholar]
- 154.Zhang L, Gu H, Gu Y, et al. Association between TNF-α -308 G/A polymorphism and COPD susceptibility: a meta-analysis update. Int J Chron Obstruct Pulmon Dis 2016; 11: 1367–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Sapey E, Wood AM, Ahmad A, et al. Tumor necrosis factor-α rs361525 polymorphism is associated with increased local production and downstream inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2010; 182: 192–199. [DOI] [PubMed] [Google Scholar]
- 156.Cordoba-Lanus E, Baz-Davila R, Espinoza-Jimenez A, et al. IL-8 gene variants are associated with lung function decline and multidimensional BODE index in COPD patients but not with disease susceptibility: a validation study. COPD 2015; 12: 55–61. [DOI] [PubMed] [Google Scholar]
- 157.Chiang CH, Chuang CH, Liu SL. Transforming growth factor-β1 and tumor necrosis factor-α are associated with clinical severity and airflow limitation of COPD in an additive manner. Lung 2014; 192: 95–102. [DOI] [PubMed] [Google Scholar]
- 158.He JQ, Foreman MG, Shumansky K, et al. Associations of IL6 polymorphisms with lung function decline and COPD. Thorax 2009; 64: 698–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Whyte M, Hubbard R, Meliconi R, et al. Increased risk of fibrosing alveolitis associated with interleukin-1 receptor antagonist and tumor necrosis factor-α gene polymorphisms. Am J Respir Crit Care Med 2000; 162: 755–758. [DOI] [PubMed] [Google Scholar]
- 160.Korthagen NM, van Moorsel CH, Kazemier KM, et al. IL1RN genetic variations and risk of IPF: a meta-analysis and mRNA expression study. Immunogenetics 2012; 64: 371–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Pantelidis P, Fanning GC, Wells AU, et al. Analysis of tumor necrosis factor-α, lymphotoxin-α, tumor necrosis factor receptor II, and interleukin-6 polymorphisms in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2001; 163: 1432–1436. [DOI] [PubMed] [Google Scholar]
- 162.Xaubet A, Marin-Arguedas A, Lario S, et al. Transforming growth factor-β1 gene polymorphisms are associated with disease progression in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2003; 168: 431–435. [DOI] [PubMed] [Google Scholar]
- 163.Son JY, Kim SY, Cho SH, et al. TGF-β1 T869C polymorphism may affect susceptibility to idiopathic pulmonary fibrosis and disease severity. Lung 2013; 191: 199–205. [DOI] [PubMed] [Google Scholar]
- 164.Seibold MA, Wise AL, Speer MC, et al. A common MUC5B promoter polymorphism and pulmonary fibrosis. N Engl J Med 2011; 364: 1503–1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Fingerlin TE, Murphy E, Zhang W, et al. Genome-wide association study identifies multiple susceptibility loci for pulmonary fibrosis. Nat Genet 2013; 45: 613–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Noth I, Zhang Y, Ma SF, et al. Genetic variants associated with idiopathic pulmonary fibrosis susceptibility and mortality: a genome-wide association study. Lancet Respir Med 2013; 1: 309–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Rutter JL, Mitchell TI, Buttice G, et al. A single nucleotide polymorphism in the matrix metalloproteinase-1 promoter creates an Ets binding site and augments transcription. Cancer Res 1998; 58: 5321–5325. [PubMed] [Google Scholar]
- 168.Marciniak SJ, Lomas DA. Genetic susceptibility. Clin Chest Med 2014; 35: 29–38. [DOI] [PubMed] [Google Scholar]
- 169.Hegab AE, Sakamoto T, Uchida Y, et al. Association analysis of tissue inhibitor of metalloproteinase2 gene polymorphisms with COPD in Egyptians. Respir Med 2005; 99: 107–110. [DOI] [PubMed] [Google Scholar]
- 170.Zhu L, Wang L, Luo X, et al. Tollip, an intracellular trafficking protein, is a novel modulator of the transforming growth factor-β signaling pathway. J Biol Chem 2012; 287: 39653–39663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Didierlaurent A, Brissoni B, Velin D, et al. Tollip regulates proinflammatory responses to interleukin-1 and lipopolysaccharide. Mol Cell Biol 2006; 26: 735–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Zumla A, Rao M, Wallis RS, et al. Host-directed therapies for infectious diseases: current status, recent progress, and future prospects. Lancet Infect Dis 2016; 16: e47–e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
G.P. Bisson ERR-0077-2017_Bisson (1.2MB, pdf)
S. Ravimohan ERR-0077-2017_Ravimohan (1.2MB, pdf)