Abstract
Background
Current and lifetime psychopathology is common in adult patients seeking bariatric surgery, with major depressive disorder and binge eating disorder affecting a higher proportion of this group than the general population. While depressive symptoms have been previously associated with eating pathology, potential mediators of this relationship are not well understood.
Methods
This study used a naturalistic, retrospective design to investigate cognitive and behavioral aspects of eating behavior (cognitive restraint, disinhibition, and hunger) as potential mediators of the relationship between depressive symptoms and binge eating within a sample of 119 adult patients (82.4% female; 96.6% white; mean age = 47 years) seeking bariatric surgery (Rouxen-Y and sleeve gastrectomy) at a large university medical center. Patients completed a standardized presurgical psychological evaluation to determine appropriateness for bariatric surgery as part of routine clinical practice. Binge eating was assessed via clinician rating (number of binge eating episodes per week) based on DSM-IV diagnostic criteria and self-report measures (Binge Eating Scale) in order to account for potential methodological differences. Depressive symptoms were assessed using the Beck Depression Inventory.
Results
Depressive symptoms were a significant predictor of binge eating, disinhibition, and hunger. However, only disinhibition emerged as a significant mediator of the relationship between depressive symptoms and binge eating.
Conclusions
Behavioral disinhibition, or a tendency toward overconsumption of food and challenges restraining impulses associated with a loss of control eating, may represent an important variable in determining the relation between depressive symptoms and binge eating, in bariatric surgery patients.
Keywords: Bariatric surgery, Psychological evaluation, Binge eating disorder, Three-Factor Eating Questionnaire
While bariatric surgery represents an effective treatment for long-term weight loss [1], not all patients seeking weight loss surgery are considered ideal candidates. An estimated 9% of patients who undergo gastric bypass fail to lose more than 5% of their initial weight over a 10-year period [2]. Previous research has attempted to identify psychosocial factors that contribute to poor outcomes following bariatric surgery such as psychopathology, psychosocial functioning, and disordered eating [3]. More specifically, the impact of binge eating behavior and binge eating disorder (BED) on the outcome of bariatric surgery has been previously investigated [4, 5] and recognized as possible contributor to suboptimal weight loss. However, previous literature notes wide variability in prevalence rates of binge eating symptoms and it is therefore challenging to gain a clear picture of the impact of symptoms on postsurgical outcomes.
For example, a previous review by Mitchell and Steffen (2009) [6] identified over 30 studies that investigated binge eating rates in bariatric samples as well as the relationship between binge eating pre- and postoperatively with weight loss outcomes. The rates of binge eating preoperatively vary widely, ranging from 6 to 64%. Similarly, postoperative binge eating rates have ranged from 0 to 71% and 0 to 32% for full syndromal BED [6]. Wide ranging estimates likely reflect the variable methodologies used for assessing binge eating [6]. Methodological differences in the assessment of binge eating may also explain mixed findings on the relationship between binge eating and weight loss. For instance, Mitchell and Steffen (2009) identified only two out of nine studies that demonstrated a link between binge eating and lack of weight loss or weight regain. However, studies that identify “loss of control” eating and weight loss outcomes consistently demonstrate an association with suboptimal weight loss. Meany et al. have more recently reviewed 15 studies that specifically consider loss of control eating; all but one study indicated that the presence of binge eating/binge eating disorder/loss of control eating postoperatively is associated with suboptimal weight loss [7]. As such, a more thorough and standardized assessment of binge eating, including “loss of control” eating may help to identify and treat patients at risk for poorer outcomes [6, 7].
Additionally, depressive symptoms are also consistently associated with both obesity [8] as well as binge eating [9, 10]. Previous research has indicated that depressive symptoms, obesity, and binge eating are interrelated; individuals with obesity who experience binge eating are more likely to exhibit depressive symptoms [11] and greater psychological impairment [12]. In bariatric samples, approximately one third of patients may be diagnosed with major depressive disorder in their lifetime [13]. Yet, not all patients with depressive symptoms will experience binge eating. Therefore, identifying possible mediators of this relationship may provide additional insight as to why some patients may be especially at risk. While depressive symptoms represent an important predictor of binge eating, few studies have examined the relationship between depressive symptoms and binge eating in a bariatric sample, despite evidence indicating high comorbidity and the potential for poorer surgical and weight loss outcomes at long-term follow-up. No studies to date have examined possible mediators of the relationship between depressive symptoms and binge eating.
The primary aims of the current study are to (1) investigate the relationship between depressive symptoms and binge eating in bariatric surgery candidates using two strategies for assessment and to (2) determine if specific eating related behaviors/cognitions further explain the relationship between depressive symptoms and binge eating. More specifically, the current study seeks to address the discrepancies in the literature related to methodological differences in the assessment of binge eating by including both a standardized measure of binge eating (Binge Eating Scale [14]) as well as clinician-rated binge eating episodes per week (as defined in the DSM-IV-TR [15], in which “loss of control” eating is present). It is hypothesized that depressive symptoms will be predictive of binge eating, as measured by both the Binge Eating Scale and DSM-IV-TR [15] criteria clinician-rated binge eating episodes per week (hypothesis 1).
Additionally, this study examines behavioral and cognitive components of eating (as assessed with the Three-Factor Eating Questionnaire [16]) as a mediator of the relationship between depressive symptoms and binge eating. The three variables assessed by the Three-Factor Eating Questionnaire include cognitive restraint, disinhibition, and hunger. The cognitive restraint scale is a measure of dietary restraint, e.g., the extent to which an individual attempts to exert control over food intake in an attempt to influence body shape and weight. The disinhibition scale measures a tendency toward overconsumption of food and challenges restraining impulses associated with a loss of control eating. The hunger scale measures subjective feelings of hunger and food cravings.
Previous research has examined changes in these variables pre- and postbariatric surgery [17] as well as the relationship between these variables and eating pathology [18]. Both disinhibition and hunger have been found to be related to binge eating in bariatric populations [18]. However, despite the fact that that the relationship between depressive symptoms and binge eating is well established [9, 10], the relationship with these variables in the context of depression is unclear. Some previous evidence suggests that these variables may mediate the relationship between constructs potentially linked to depression (i.e., body image dissatisfaction) and binge eating [19], yet no studies have specifically examined the relationship to depressive symptoms. Thus, the current study seeks to examine these constructs in order to better determine how these variables may impact binge eating in the context of depressive symptoms.
Cognitive restraint, disinhibition, and hunger are hypothesized to affect the relationship between depressive symptoms and binge eating, with disinhibition being the strongest mediator (hypothesis 2). More specifically, cognitive restraint is likely inversely related to problematic episodes of overeating or loss of control eating. As cognitive restraint has not been a significant mediator of the relationship between constructs potentially linked to depression and binge eating [19], it is hypothesized that cognitive restraint will not represent a significant mediator in this model (hypothesis 2a). Disinhibition reflects a behavioral tendency or trait that contributes to problematic eating behavior. As depressive symptoms may increase susceptibility to overeating in response to negative emotional states, hypothesized disinhibition will mediate the relationship between depressive symptoms and binge eating (hypothesis 2b). Hunger may be related to episodes of overeating by contributing to increased appetite and challenges with feelings of satiety. As depression may contribute to increased appetite, hunger is hypothesized to mediate the relationship between depressive symptoms and binge eating (hypothesis 2c).
Methods
Participants
Participants were 119 bariatric surgery candidates evaluated in 2012–2013 at a large university medical center. The population includes a predominately rural Appalachian population. Participants were 83% female and 17% male, with an age range of 17–77 years old (M= 46.68, SD = 12.01). The sample was primarily Caucasian (97% Caucasian, 3% African American), with a mean of 13.61 years of education (SD = 2.9). The majority of patients were employed full time (52%) with the remaining sample on disability (23%), self-identified as a “homemaker” (10%), unemployed (7%), retired (5%), or a student (4%). The majority of the sample was married (54%), with 18% divorced, 18% single, 2% separated, and 2% widowed. The sample had a mean body mass index (BMI) of 50.77 (SD = 10.01). Most patients were interested in pursuing Roux-en-Y gastric bypass (91.6%); 4.2% were interested in lap band and 4.2% were interested in sleeve gastrectomy.
Procedure
All patients completed a standard psychological evaluation as part of preoperative requirements for surgery between September 2012 and August 2013. Participants completed a clinical interview with a licensed psychologist, who was a member of the bariatric surgery program. Patients completed self-report, psychosocial measures on the same day as part of their psychological evaluation. This study was approved by the university’s Institutional Review Board.
Measures
Demographics
Participants’ age, sex, height, weight/BMI (kg/m2), race, level of education, marital status, work status, insurance type, and number of medical comorbidities were collected.
Binge Eating
Binge eating was assessed with the Binge Eating Scale (BES) and clinician-rated binge eating episodes per week.
Binge Eating Scale (BES; Gormally al. 1982 [14])
The Binge Eating Scale is a 16-item self-report questionnaire used to assess the prevalence of binge eating behavior indicative of an eating disorder. Each item includes four statements corresponding with increasing prevalence of binge eating. In a bariatric surgery sample, the BES has demonstrated good internal consistency (Cronbach’s alpha of 0.90) and construct validity with regard to its ability to distinguish between minimal, moderate, and severe binge eating [20].
Clinician-rated binge eating episodes per week based on DSM-IV-TR [15] criteria
Binge eating episodes per week were evaluated by a licensed psychologist conducting the presurgical psychological assessments. Diagnosed binge eating episodes per week were based on DSM-IV-TR [15] research criteria for binge eating disorder. An episode of binge eating was characterized by both of the following: (1) eating, in a discrete period of time (e.g., within any 2-h period), an amount of food that is definitely larger than most people would eat in a similar period of time under similar circumstances; (2) a sense of lack of control over eating during the episode (e.g., a feeling that one cannot stop eating or control what or how much one is eating). Binge eating episodes must also have been associated with three or more of the following: eating much more rapidly than normal, eating until feeling uncomfortably full, eating large amounts of food when not feeling physically hungry, eating alone because of embarrassment by how much one is eating, feeling disgusted with oneself, depressed, or very guilty after overeating.
Depressive Symptoms
Beck Depression Inventory-II (BDI-II; Beck et al. [21]). The BDI-II is a 21-item self-report measure of severity of depressive symptoms. Each item includes a 4-item response indicating severity of a particular symptom over the past 2 weeks. The total score is derived by summing all item responses (range 0 to 63), with higher scores indicating more severe depression concerns. The BDI-II has been found to be a good measure for screening for clinical depression in bariatric surgery candidates [22, 23]. It has also demonstrated excellent internal consistency (Cronbach’s alpha of 0.90), convergent validity, and criterion-related validity in a bariatric surgery population [24].
Eating Related Cognitions
Three-Factor Eating Questionnaire (TFEQ; Stunkard and Messick [16]). The TFEQ is a self-report questionnaire used to measure cognitive and behavioral components of eating. This 51-itemmeasure includes 36 items with a yes/no response, 14 items rated on a 1–4 Likert scale, and one item with a vertical rating ranging from 1 to 6 from no restraint in eating to total restraint. The TFEQ includes three subscales: cognitive restraint (21 items), disinhibition (16 items), and hunger (14 items). The three factors of the TFEQ have demonstrated adequate internal consistency (Cronbach’s alpha of 0.87 for cognitive restraint of eating, 0.80 for disinhibition, and 0.73 for hunger) and validity in an obese population [25]. Further, the TFEQ has demonstrated construct validity with regard to its ability to distinguish between binge and non-binge eaters in a bariatric surgery sample [26].
Statistical Analysis
SPSS version 22.0 was used for the analyses (SPSS Inc., Chicago, IL, USA). Descriptive statistics and Pearson correlations were run to examine all demographic variables and self-report and clinician-rated measures. Linear regression was used to investigate hypothesis 1, and mediation analyses were conducted to answer hypothesis 2. Mediation analyses were conducted using Barron and Kenny’s [27] steps for mediation.
Results
Descriptive statistics and correlations for binge eating (as assessed with BES and clinician-rated), BDI-II and components of the TFEQ are presented in Table 1. Binge eating as assessed by the Binge Eating Scale and clinician-rated binges per week was significantly correlated with all variables, p < .05. Frequency data for the BES and clinician-rated binges per week is presented in Table 2. Eleven out of 119 patients had two or more episodes of binge eating per week. As this study utilized DSM-IV-TR [15] diagnostic criteria, this equates to 9.2% of the sample with a binge eating diagnosis (i.e., eating disorder not otherwise specified).
Table 1.
Descriptive statistics
| Correlations | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| N | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
| 1 Binge Eating Scale (BES) | 117 | 12.55 | 8.11 | 1 | |||||
| 2 Clinician-Rated Binge Eating | 119 | 0.66 | 2.44 | .37** | 1 | ||||
| 3 Beck Depressive symptoms Inventory (BDI) | 117 | 11.97 | 10.06 | .51** | .28** | 1 | |||
| 4 Cognitive restraint | 115 | 11.41 | 4.50 | − .37** | −.216* | −.10 | 1 | ||
| 5 Disinhibition | 115 | 7.30 | 3.83 | .75** | .38** | .47** | −.41** | 1 | |
| 6 Hunger | 114 | 5.93 | 4.11 | .53** | .25** | .29** | −.37** | .64** | 1 |
p < .05;
p < .01
Table 2.
Frequencies for Binge Eating Scale and clinician-rated binge eating episodes per week
| N | Frequency | Percentage | Cumulative percentage |
|
|---|---|---|---|---|
| Binge Eating Scale (BES) | 117 | |||
| Non-binge eating; < 17 | 88 | 75.2% | 75.2% | |
| Moderate binge eating; | 23 | 19.7% | 94.9% | |
| 18–26 | ||||
| Severe binge eating; | 6 | 5.1% | 100% | |
| >27 | ||||
| Clinician-rated binge eating episodes | 119 | |||
| None | 101 | 84.9% | 84.9% | |
| 1 episode per week | 7 | 5.9% | 90.8% | |
| 2 episodes per week | 3 | 2.5% | 93.3% | |
| 5 episodes per week | 2 | 1.7% | 95.0% | |
| 7 episodes per week | 5 | 4.2% | 99.2% | |
| > 8 episodes per week | 1 | 0.8% | 100.0% |
Linear regression analysis was used to investigate hypothesis 1. Results indicated that depressive symptoms were a significant predictor of binge eating as measured by the BES, b = 0.41, SE= 0.07, p < .00, and depressive symptoms was also a significant predictor of clinician-rated binge eating, b = 0.67, SE= 0.02, p < .00.
Regression analysis was also used to investigate hypothesis 2. Results for each of the three factors are discussed below.
Cognitive Restraint as a Mediator of the Relationship Between Depressive Symptoms and Binge Eating
Results indicated that depressive symptoms were not associated with cognitive restraint, b = − 0.04, SE = 0.04, p = .31. As such, cognitive restraint may not be considered a mediator of the relationship between depressive symptoms and binge eating.
Disinhibition as a Mediator of the Relationship Between Depressive Symptoms and Binge Eating
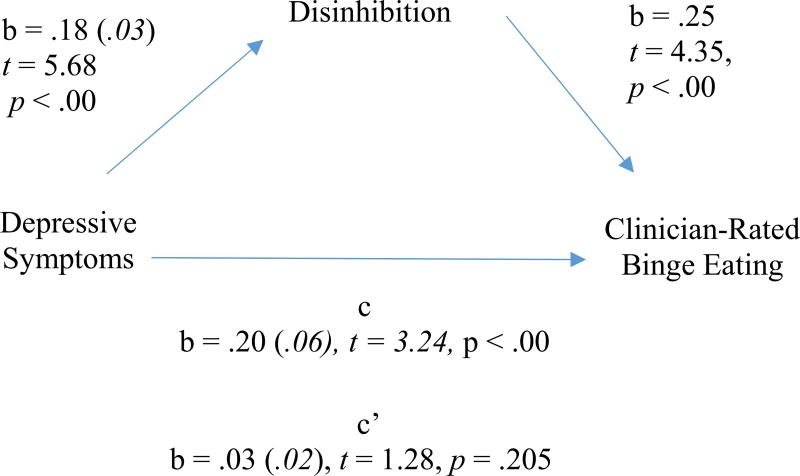
Results indicated that depressive symptoms were a significant predictor of disinhibition, b = 0.18, SE= 0.03, p < .00, and that disinhibition was a significant predictor of clinician-rated binge eating, b = 0.25, SE = 0.06, p < .00. Depressive symptoms were no longer a significant predictor of clinician-rated binge eating after controlling for the mediator, disinhibition, b = 0.03, SE = 0.02, p = ns, consistent with full mediation. Approximately 16% of the variance in clinician-rated binge eating was accounted for by the predictors (R = .396). The mediational analysis is presented in Fig. 1. Disinhibition was not a significant predictor of binge eating as rated by the BES.
Fig. 1.
Unstandardized regression coefficients and standard errors for the relationship between depressive symptoms and clinician-rated binge eating as mediated by disinhibition
Hunger as a Mediator of the Relationship Between Depressive Symptoms and Binge Eating
Results indicated that depressive symptoms were a significant predictor of hunger, b = 0.12, SE = 0.04, p < .00, and that hunger was a significant predictor of both clinician-rated binge eating, b = 0.15, SE = 0.05, p < .05, and binge eating as measured by the BES, b = 1.05, SE = 0.16, p < .00. However, depressive symptoms remained a significant predictor of both clinician-rated binge eating, b = 0.05, SE = 0.02, p < .05, and binge eating as measured by the BES, b = 0.31, SE= 0.06, p < .00, indicating lack of mediation for both models.
Discussion
Results indicated that depressive symptoms were a significant predictor of binge eating, both as measured by the BES and by clinician ratings in this sample. This finding is not surprising, given the relationship between depressive symptoms and binge eating demonstrated in previous literature [9, 10]. Given the frequency of mixed results and variety of methodologies used to assess binge eating, it is important to note that this result was consistent for both measures of binge eating. It is possible that depressive symptoms contribute to an overall increased risk of maladaptive eating habits as well as specific binge eating with loss of control eating. For this reason, measures that are not sensitive with regard to loss of control eating still may have utility in terms of correlations with depressive symptoms.
The present study also sought to investigate the factors that contribute to binge eating among patients who experience depressive symptoms, i.e., factors that mediate the relationship between depressive symptoms and binge eating. Only disinhibition emerged as a significant mediator of the relationship between depressive symptoms and binge eating when assessed using clinician-rated binge eating. Cognitive restraint and hunger did not mediate this relationship. Although it was hypothesized that individuals with depressive symptoms may score lower on cognitive restraint, no relationship between depressive symptoms and cognitive restraint was found. As such, it was not considered as a possible mediator of the relationship between depressive symptoms and binge eating. It may be that depressive symptoms do not exert influence on attempts at specifically restricting one’s intake. While depressive symptoms were predictive of hunger and levels of hunger did influence binge eating, hunger did not represent a mediational variable. In contrast to results examining the relationship between depressive symptoms and binge eating, in which depressive symptoms were predictive of both methodologies for binge eating, the mediation was only significant when examining clinician-rated binge eating. This finding is of particular interest as binge eating episodes were identified on the basis of loss of control eating, along with other diagnostic criteria. The BES does not specifically include this assessment of loss of control eating. For this reason, loss of control eating may represent a more sensitive measure when attempting to examine eating pathology. This finding is supported in previous studies in which loss of control eating confers additional risk for maladaptive eating behavior and eating disorders [28].
Taken together, these results also indicate that disinhibition plays an important role in considering the relationship between depressed mood and binge eating. Depressive symptoms may contribute to greater difficulty in regulating one’s behavior and controlling impulses to eat, thereby increasing problematic eating behavior. Previous research suggests that there may be a particular subgroup of patients with binge eating characterized by greater levels of disinhibition [28, 29]. These individuals may be at elevated risk for maladaptive eating behaviors and poor outcome following surgery, especially in the presence of depressive symptoms. Disinhibition may represent a set of endurable characteristics that serve as a predisposition for opportunistic eating, including eating in response to negative effect.
Limitations of the present study include a smaller sample size as well as the limited number of individuals with binge eating disorder or clinician-rated binge eating episodes. However, a larger proportion of the sample endorsed moderate binge eating on objective measures possibly reflecting subsyndromal overeating episodes. This consideration highlights the challenges of assessment of binge eating, which can differ depending on methodology. An additional limitation is the limited variability in ethnicity. Our sample is predominately Caucasian and may have unique characteristics based on our location, which may limit the generalizability of the outcome. This study makes a unique contribution by investigating this relationship in a predominately rural, Appalachian population. Although previous studies have found that patients who reside in more rural areas have similar outcomes postsurgically [30], future studies may also consider how rural status may influence problematic eating.
Additionally, the current study is based on a presurgical, semistructured psychological evaluation rather than on a structured clinical interview. The latter may have more accurately captured DSM disorders. Future studies may consider investigating these variables with a more diverse patient population and consider inclusion of outcome data postsurgery. Interpretation of the results must also be considered with the methodology of the study in mind. The current study utilized a cross-sectional design, rather than a continuous time longitudinal model or a temporal method of assessment in which the predictive variables are assessed prior to mediation and outcome variables. Mediational analyses conducted with cross-sectional samples may represent a “statistical mediation, ” rather than a method of determining causal inferences. Longitudinal mediational models may be helpful for future studies to better specify the timing of relationships among variables, temporal causality, or bidirectional relationships. In particular, although this study specifically examined the impact of depressive symptoms on eating behavior, it is important to note that the relationship between depressive symptoms and binge eating may be bidirectional. Previous prospective studies have found that individuals who report depressive symptoms at baseline are two times more likely to initiate binge eating, and individuals who engage in binge eating are two times more likely to develop depressive symptoms [31]. Future studies may wish to utilize causal modeling approaches that include consideration of this potential bidirectional relationship.
In conclusion, this study highlights the importance of screening for problematic eating and has potential to inform treatment interventions. Only disinhibition emerged as a significant mediator of the relationship between depressive symptoms and binge eating when assessed using clinician-rated binge eating. These results may have implications for presurgical psychological evaluations. Individuals with higher levels of disinhibition may constitute an at risk subgroup. Future studies may consider strategies to identify this group of individuals in order to target treatment interventions.
Footnotes
Compliance with Ethical Standards
Informed Consent Formal consent is not required for data collection as part of routine clinical practice.
The study was conducted in accordance with Good Clinical Practice and consistent with the Declaration of Helsinki.
Conflicts of Interest The authors declare that they have no conflicts of interest
References
- 1.Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37. doi: 10.1001/jama.292.14.1724. https://doi.org/10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 2.Sjöström L, Lindroos A-K, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93. doi: 10.1056/NEJMoa035622. https://doi.org/10.1056/nejmoa035622. [DOI] [PubMed] [Google Scholar]
- 3.Hsu LK, Benotti PN, Dwyer J, et al. Nonsurgical factors that influence the outcome of bariatric surgery: a review. Psychosom Med. 1998;60(3):338–46. doi: 10.1097/00006842-199805000-00021. https://doi.org/10.1097/00006842-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 4.Chao AM, Wadden TA, Faulconbridge LF, et al. Binge-eating disorder and the outcome of bariatric surgery in a prospective, observational study: two-year results. Obesity. 2016;24(11):2327–33. doi: 10.1002/oby.21648. https://doi.org/10.1002/oby.21648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wadden TA, Faulconbridge LF, Jones-Corneille LR, et al. Binge eating disorder and the outcome of bariatric surgery at one year: a prospective, observational study. Obesity. 2011;19(6):1220–8. doi: 10.1038/oby.2010.336. https://doi.org/10.1038/oby.2010.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mitchell JE, Steffen K. The interface between eating disorders and bariatric surgery. Eat Disord Rev. 2009;20(1):1. [Google Scholar]
- 7.Meany G, Conceição E, Mitchell JE. Binge eating, binge eating disorder and loss of control eating: effects on weight outcomes after bariatric surgery. Eur Eat Disord Rev. 2014;22(2):87–91. doi: 10.1002/erv.2273. https://doi.org/10.1002/erv.2273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herva A, Laitinen J, Miettunen J, et al. Obesity and depression: results from the longitudinal Northern Finland 1966 Birth Cohort Study. Int J Obes. 2005;30(3):520–7. doi: 10.1038/sj.ijo.0803174. https://doi.org/10.1038/sj.ijo.0803174. [DOI] [PubMed] [Google Scholar]
- 9.Telch CF, Agras WS, Rossiter EM. Binge eating increases with increasing adiposity. Int J Eat Disord. 1988;7(1):115–9. https://doi.org/10.1002/1098-108X(198801)7:1<115::AID-EAT2260070112>3.0.CO;2-W. [Google Scholar]
- 10.Linde JA, Jeffery RW, Levy RL, et al. Binge eating disorder, weight control self-efficacy, and depressive symptoms in overweight men and women. Int J Obes. 2004;28(3):418–25. doi: 10.1038/sj.ijo.0802570. https://doi.org/10.1038/sj.ijo.0802570. [DOI] [PubMed] [Google Scholar]
- 11.Marcus MD, Wing RR, Ewing L, et al. Psychaitric disorders among obese binge eaters. Int J Eat Disord. 1990;9(1):69–77. https://doi.org/10.1002/1098-108X(199001)9:1<69::AID-EAT2260090108>3.0.CO;2-K. [Google Scholar]
- 12.Grissett NI, Fitzgibbon ML. The clinical significance of binge eating in an obese population; support for BED and questions regarding its criteria. Addict Behav. 1996;21(1):57–66. doi: 10.1016/0306-4603(95)00039-9. https://doi.org/10.1016/0306-4603(95)00039-9. [DOI] [PubMed] [Google Scholar]
- 13.Mitchell JE, Selzer F, Karlarchian MA, et al. Psychopathology before surgery in the Longitudinal Assessment of Bariatric Surgery-3 (LABS-3) psychosocial study. Surg Obes Relat Dis. 2012;8(5):533–41. doi: 10.1016/j.soard.2012.07.001. https://doi.org/10.1016/j.soard.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gormally J, Black S, Daston S, et al. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7(1):47–55. doi: 10.1016/0306-4603(82)90024-7. https://doi.org/10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- 15.Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 16.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29(1):71–83. doi: 10.1016/0022-3999(85)90010-8. https://doi.org/10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 17.Sarwer DB, Wadden TA, Moore RH, et al. Preoperative eating behavior, postoperative dietary adherence, and weight loss after gastric bypass surgery. Surg Obes Relat Dis. 2008;4(5):640–6. doi: 10.1016/j.soard.2008.04.013. https://doi.org/10.1016/j.soard.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kalarchian MA, Marcus MD, Wilson GT, et al. Binge eating among gastric bypass patients at long-term follow-up. Obes Surg. 2002;12(2):270–5. doi: 10.1381/096089202762552494. https://doi.org/10.1381/096089202762552494. [DOI] [PubMed] [Google Scholar]
- 19.Ricciardelli LA, Tate D, Williams RJ. Body dissatisfaction as a mediator of the relationship between dietary restraint and bulimic eating patterns. Appetite. 1997;29(1):43–54. doi: 10.1006/appe.1997.0093. https://doi.org/10.1006/appe.1997.0093. [DOI] [PubMed] [Google Scholar]
- 20.Ashton K, Drerup M, Windover A, et al. Brief, four-session group CBT reduces binge eating behaviors among bariatric surgery candidates. Surg Obes Relat Dis. 2009;5(2):257–62. doi: 10.1016/j.soard.2009.01.005. https://doi.org/10.1016/j.soard.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 21.Beck AT, Steer RA, Brown GK. Manual for the Beck Depressive symptoms Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 22.Hayden MJ, Brown WA, Brennan L, et al. Validity of the Beck Depression Inventory as a screening tool for a clinical mood disorder in bariatric surgery candidates. Obes Surg. 2012;22(11):1666–75. doi: 10.1007/s11695-012-0682-4. https://doi.org/10.1007/s11695-012-0682-4. [DOI] [PubMed] [Google Scholar]
- 23.Marek RJ, Heinberg LJ, Lavery M, et al. A review of psychological assessment instruments for use in bariatric surgery evaluations. Psychol Assess. 2016;28(9):1142–57. doi: 10.1037/pas0000286. https://doi.org/10.1037/pas0000286. [DOI] [PubMed] [Google Scholar]
- 24.Hall BJ, Hood MM, Nackers LM, et al. Confirmatory factor analysis of the Beck Depression Inventory-II in bariatric surgery candidates. Psychol Assess. 2013;25(1):294–9. doi: 10.1037/a0030305. https://doi.org/10.1037/a0030305. [DOI] [PubMed] [Google Scholar]
- 25.Allison DB, Kalinsky LB, Gorman BS. A comparison of the psychometric properties of three measures of dietary restraint. Psychol Assess. 1992;4(3):391–8. https://doi.org/10.1037/1040-3590.4.3.391. [Google Scholar]
- 26.Kalarchian MA, Wilson GT, Brolin RE, et al. Binge eating in bariatric surgery patients. Int J Eat Disord. 1998;23(1):89–92. doi: 10.1002/(sici)1098-108x(199801)23:1<89::aid-eat11>3.0.co;2-i. https://doi.org/10.1002/(SICI)1098-108X(199801)23:1<89::AID-EAT11>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 27.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research—conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82. doi: 10.1037//0022-3514.51.6.1173. https://doi.org/10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 28.Colles SL, Dixon JB, O’Brien PE. Loss of control is central to psychological disturbance associated with binge eating disorder. Obesity. 2008;16(3):608–14. doi: 10.1038/oby.2007.99. https://doi.org/10.1038/oby.2007.99. [DOI] [PubMed] [Google Scholar]
- 29.Hsu LKG, Mulliken B, McDonagh B, et al. Binge eating disorder in extreme obesity. Int J Obes Relat Metab Disorders. 2002;26(10):1398. doi: 10.1038/sj.ijo.0802081. [DOI] [PubMed] [Google Scholar]
- 30.Bergman K, Cox S, Tabone LT. The influence of a rural environment on patient access and outcomes for bariatric surgery. Surg Obes Relat Dis. 2017;11(6) doi: 10.1016/j.soard.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 31.Skinner HH, Haines J, Austin SB, et al. A prospective study of overeating, binge eating, and depressive symptoms among adolescent and young adult women. J Adolesc Health. 2012;50(5):478–83. doi: 10.1016/j.jadohealth.2011.10.002. https://doi.org/10.1016/j.jadohealth.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]