Abstract
Background and Purpose
Intracerebral hemorrhage (ICH) is a considerable source of morbidity and mortality. This three-center study describes outcomes of pediatric ICH and identifies 2-year neurologic outcome predictors.
Methods
Children 29 days–18 years presenting with ICH from 3/2007–5/2015 were enrolled prospectively. Exclusion criteria: trauma, intracranial tumor, hemorrhagic transformation of arterial stroke or cerebral sinovenous thrombosis, isolated subdural, epidural, or subarachnoid hemorrhage, and abnormal baseline neurologic function. ICH and total brain volumes (TBV) were measured on neuroimaging. The Pediatric Stroke Outcome Measure (PSOM) assessed outcomes.
Results
Sixty-nine children were included (median age 9.7 years, IQR 2.2–14). Six children (9%) died during hospitalization. Outcomes in survivors were assessed at early follow-up in 98% (median 3.1 months, IQR 3.1–3.8) and at later follow-up in 94% (median 2.1 years, IQR 1.3–2.8). Over a third had a significant disability at 2 years (PSOM >2). Total PSOM score improved over time (p=0.0003), paralleling improvements in the sensorimotor subscore (p=0.0004). Altered mental status (OR 13, 95% CI 3.9–46, p<0.001), hemorrhage volume ≥4% of TBV (OR 17, 95% CI 1.9–156, p=0.01), and ICU length of stay (LOS) (OR 1.1, 95% CI 1.0–1.2, p=0.002) were significantly associated with poor 2-year outcome.
Conclusions
Over one-third of children experienced significant disability at 2 years. Improvements in outcomes were driven by recovery of sensorimotor function. AMS, hemorrhage volume ≥4% of TBV, and ICU LOS were independent predictors of significant disability at 2 years.
Keywords: intracerebral hemorrhage, pediatrics, outcome, predictors
Subject terms: Intracranial hemorrhage, Pediatrics, Prognosis, Mortality/Survival
Introduction
Although approximately half of pediatric strokes are hemorrhagic, studies of pediatric intracerebral hemorrhage (ICH) have rarely examined outcome predictors, and retrospective studies are limited by the inadequacy of ICD-9 code-based case identification1. Prospective studies have been small or have focused on short-term outcomes (<1 year)2,3. Study aims were to describe the spectrum of outcomes of pediatric spontaneous ICH prospectively at three pediatric centers and to identify predictors of poor 2-year neurologic outcome.
Methods
Case Identification and Clinical Data
All children presenting with ICH from 3/2007–5/2015 were included. The Institutional Review Board approved the study at each site; informed consent was obtained. Inclusion criteria: age 29 days–18 years, spontaneous ICH confirmed by CT or MRI. Exclusion criteria: trauma, intracranial tumor, hemorrhagic transformation of arterial stroke or cerebral sinovenous thrombosis, isolated epidural/subdural/subarachnoid hemorrhage, and abnormal baseline neurologic function. Data supporting the study findings are available from the corresponding author upon request.
Pediatric stroke neurologists collected data via parental interview, medical record abstraction, and at follow-up stroke clinic visits. Glasgow Coma Score (GCS) ≤9 was not obtained consistently. Thus, we defined altered mental status (AMS) as obtunded, comatose, or unresponsive on initial physician examination, or if GCS ≤9, when recorded.
Hemorrhage Analysis
Etiology was determined by medical history, imaging review, intraoperative observation, and surgical pathology. Parenchymal hemorrhage volume was measured as previously described and expressed as a percentage of total brain volume (TBV)4. Cut-offs of 2% of TBV and 4% of TBV defined large and very large hemorrhage. Children with isolated intraventricular hemorrhage (IVH) were excluded from volumetric analyses.
Outcomes
Outcomes were assessed at 3-month and 2-year clinic visits using the Pediatric Stroke Outcome Measure (PSOM), a standardized score of neurologic function commonly used in pediatric ischemic and hemorrhagic stroke2,4,5. Scores are assigned from 0–2 for 5 domains (right and left sensorimotor, expressive and receptive language, cognitive/behavioral) and are summed for a total PSOM score. A total score of >2 or death represented ‘poor’ outcome. A score >2 reflects a deficit in >1 domain and was chosen to distinguish between children with residual disability but a good degree of function and children at risk of long-term dependence. A short parent survey regarding the child’s level of functioning, which is included in the most recent International Pediatric Stroke Study PSOM Short Neuro Exam form, was also administered at these visits6.
Statistical Analyses
Wilcoxon signed-rank tests and Stuart-Maxwell tests compared equality of distributions and differences in proportions over time. Univariable logistic regressions evaluated associations between possible predictors and poor outcome at 2-year follow-up. The multivariable logistic regression model included the three most significant predictors on univariable analysis, adjusting for age. Analyses were conducted in STATA 15.0.
Results
Patient Characteristics
Sixty-nine children met inclusion criteria, median age 9.7 years (IQR 2.2–14, range 30 days–18 years). Supplemental Table I summarizes patient characteristics. Known medical risk factors were present in 20%, including cardiac, hematologic, immunologic, or genetic diagnoses. A precipitating factor for ICH was present in 19%, including hypertension (3%), infection (13%), surgery within one month (3%), coagulopathy (13%), and multiple factors (69%).
Hemorrhage was isolated parenchymal in 45%, isolated intraventricular in 9%, and involved >1 compartment in 46%. ICH volume could be calculated in 61 children (88%) and was <2% TBV in 54%, 2% to <4% TBV in 25%, and ≥4% TBV in 10%. Vascular malformations accounted for 63% of hemorrhages and coagulopathy for 17%. Etiology could not be determined in 19%, although vascular malformations were suspected in one-third. Children were carefully evaluated for ICH cause (Supplemental material). Median hospital length of stay (LOS) was 15 days (IQR 9–22); median ICU stay was 11 days (IQR 5–18). Six children died during hospitalization (9%). Most children were discharged to inpatient rehabilitation (52%) or home with outpatient rehabilitation (27%).
Outcomes
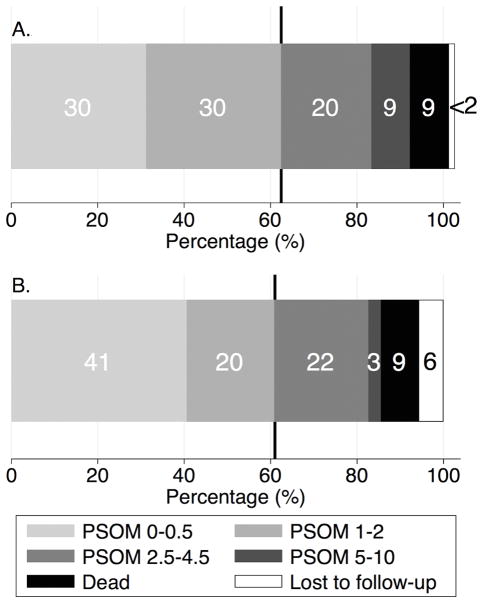
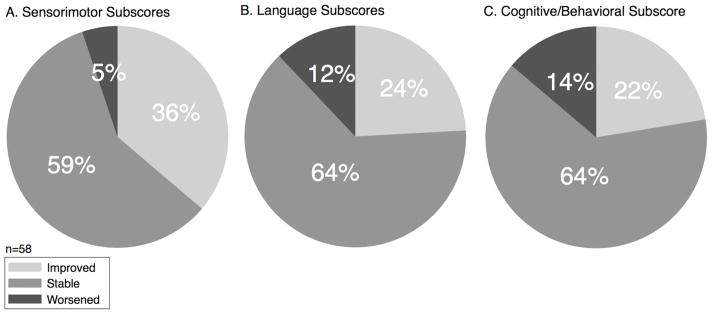
Outcomes were assessed at a median of 3.1 months (IQR 2.8–3.8) in 98% and again at 2.1 years (IQR 1.3–2.8 years) in 94%. Median total 3-month PSOM was 1.5 (IQR 0.5–3) and 2-year PSOM was 1 (IQR 0–2.5). Overall, 38% and 34% of children had poor outcomes, respectively (Figure 1). While total PSOM scores improved over time (median 1.5 to 1.0, p=0.0003), this was largely due to improvements in sensorimotor subscores (median 1.0 to 0.5, p=0.0004), while language and cognitive/behavioral subscores did not change significantly. Figure 2 shows direction of change for these subscores. From a functional standpoint, 76% of parents reported their children had not made a complete recovery, with 20% also noting the need for extra help with day-to-day activities compared to peers and 19% an impact on emotional state, behavior, and self-esteem.
Figure 1.
Total PSOM score distributions at: 3 months (A) and 2 years (B) (labeled with % in each category).
Figure 2.
Direction of change over time of PSOM sensorimotor (A), language (B), and cognitive/behavioral subscores (C).
Outcome Predictors
In univariable analyses, AMS and hemorrhage ≥4% of TBV were strongly associated with poor 2-year outcome (OR 13, 95% CI 3.9–46, p<0.001, and OR 17, 95% CI 1.9–156, p=0.01, Supplemental Table I). Longer hospital and ICU stay were significantly associated with poor outcomes (OR 1.1, 95% CI 1.0–1.1, p=0.005, and OR 1.1, 95% CI 1.0–1.2, p=0.002). Other associations with poor 2-year outcome included male sex, hemiparesis, hydrocephalus, and herniation. The three strongest outcome predictors (AMS, ICH volume ≥4% of TBV, ICU LOS) remained significantly associated with poor outcome in multivariable regression adjusted for age (Supplemental Table I). In univariable logistic regression, death was significantly associated with AMS, hemorrhage volume ≥4% of TBV, and coagulopathy (Supplemental Table II); hemorrhage volume ≥2% of TBV, edema, hydrocephalus, and herniation syndrome were not.
Discussion
In this multicenter prospective study, we describe outcomes of pediatric spontaneous ICH over time and identify 2-year outcome predictors. Over one-third of children had a poor 2-year outcome measured by dichotomized PSOM scores. Four prior studies have examined outcomes of pediatric ICH after one year3,7–9. Comparing studies is challenging due to use of different outcome assessments, study designs, and inclusion criteria. Studies show widely divergent outcomes, with 10%–75% of children experiencing clinically significant deficits, variably defined (Supplemental Table III). Mortality ranged from 4.5% to 39%2–4,7–9. Lower mortality (9%) in our study may reflect exclusion of children with intracranial tumors, management by dedicated stroke teams, and improvements in neurocritical care, including aggressive neurosurgical management.
AMS, hemorrhage volume, and ICU LOS were strongly associated with poor 2-year outcome on age-adjusted multivariable analysis. Prolonged ICU stay may reflect underlying medical complexity, hemorrhage severity, treatment complications, or a combination. The association of poor 2-year outcome with AMS at presentation and hemorrhage volume ≥4% of TBV is consistent with prior studies assessing short-term outcomes, and confirms its importance as a predictor in a larger prospective study2–4. AMS has not been a predictor in other pediatric studies, possibly because of differences in mental status assessment. Consistent with others’ findings, we did not observe an association between poor outcome and infratentorial location, intraventricular extension, or coagulopathy2. Coagulopathy was associated with mortality along with AMS and hemorrhage volume ≥4% of TBV. Consistently with other reports, volume ≥2% of TBV was not associated with death, which suggests a threshold effect3.
The improvements in sensorimotor subscores, without change in language and cognitive/behavioral subscores, are consistent with evidence in both pediatric hemorrhagic and ischemic stroke that cognitive and language deficits are increasingly observed over time, perhaps due to poor sensitivity of assessment measures at young ages or emerging deficits as cognitive demands children face increase.3,10
Study limitations include lack of a specific outcome measure validated for pediatric ICH. We chose the PSOM over other metrics because it was developed and validated for pediatric ischemic stroke, relies on a detailed physical examination, and correlates with results from standardized neuropsychological measures5,11,12. The PSOM, however, is limited in its ability to capture functional impairments. Sample size is a weakness of pediatric ICH studies due to low incidence. Our study is one of the largest prospective studies of pediatric ICH to have followed children beyond 1 year. Its prospective and multicenter nature are important strengths given difficulties with ascertainment and bias in single-center or retrospective studies, providing wider generalizability of results.
Conclusions
Over one-third of children had significant functional disability at 2 years, with a 9% mortality rate. Better outcomes over time were driven by improvements in the sensorimotor domain, compared to the language and cognitive/behavioral domains where deficits may emerge/become more evident with age. AMS, large hemorrhage volume, and ICU LOS were associated with significant functional disability at 2 years. Improved understanding of outcomes after pediatric ICH as well as factors that affect long-term outcomes will allow physicians to counsel families on prognosis.
Supplementary Material
Acknowledgments
Sources of Funding
NIH-K23-NS062110
Footnotes
Disclosures
None.
References
- 1.Golomb MR, Garg BP, Saha C, Williams LS. Accuracy and yield of ICD-9 codes for identifying children with ischemic stroke. Neurology. 2006;67:2053–2055. doi: 10.1212/01.wnl.0000247281.98094.e2. [DOI] [PubMed] [Google Scholar]
- 2.Beslow LA, Licht DJ, Smith SE, Storm PB, Heuer GG, Zimmerman RA, et al. Predictors of outcome in childhood intracerebral hemorrhage: A prospective consecutive cohort study. Stroke. 2010;41:313–318. doi: 10.1161/STROKEAHA.109.568071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lo WD, Hajek C, Pappa C, Wang W, Zumberge N. Outcomes in Children With Hemorrhagic Stroke. JAMA Neurol. 2013;70:66. doi: 10.1001/jamaneurol.2013.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jordan LC, Kleinman JT, Hillis AE. Intracerebral hemorrhage volume predicts poor neurologic outcome in children. Stroke. 2009;40:1666–71. doi: 10.1161/STROKEAHA.108.541383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kitchen L, Westmacott R, Friefeld S, MacGregor D, Curtis R, Allen A, et al. The Pediatric Stroke Outcome Measure: A Validation and Reliability Study. Stroke. 2012;43:1602–1608. doi: 10.1161/STROKEAHA.111.639583. [DOI] [PubMed] [Google Scholar]
- 6.Lo WD, Ichord RN, Dowling MM, Rafay M, Templeton J, Halperin A, et al. The pediatric stroke Recurrence and Recovery Questionnaire: Validation in a prospective cohort. Neurology. 2012;79:864–870. doi: 10.1212/WNL.0b013e318266fc9a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blom I, De Schryver ELLM, Kappelle LJ, Rinkel GJE, Jennekens-Schinkel A, Peters ACB. Prognosis of haemorrhagic stroke in childhood: A long-term follow-up study. Dev Med Child Neurol. 2003;45:233–239. doi: 10.1017/s001216220300046x. [DOI] [PubMed] [Google Scholar]
- 8.Meyer-Heim AD, Boltshauser E. Spontaneous intracranial haemorrhage in children: Aetiology, presentation and outcome. Brain Dev. 2003;25:416–421. doi: 10.1016/s0387-7604(03)00029-9. [DOI] [PubMed] [Google Scholar]
- 9.Lo WD, Lee JE, Rusin J, Perkins E, Roach ES. Intracranial hemorrhage in children: An evolving spectrum. Arch Neurol. 2008;65:1629–1633. doi: 10.1001/archneurol.2008.502. [DOI] [PubMed] [Google Scholar]
- 10.Westmacott R, Macgregor D, Askalan R, Deveber G. Late emergence of cognitive deficits after unilateral neonatal stroke. Stroke. 2009;40:2012–2019. doi: 10.1161/STROKEAHA.108.533976. [DOI] [PubMed] [Google Scholar]
- 11.Lo W, Gordon AL, Hajek C, Gomes A, Greenham M, Anderson V, et al. Pediatric stroke outcome measure: Predictor of multiple impairments in childhood stroke. J Child Neurol. 2014;29:1524–1530. doi: 10.1177/0883073813503186. [DOI] [PubMed] [Google Scholar]
- 12.Murphy LK, Compas BE, Gindville MC, Reeslund KL, Jordan LC. Cognitive functioning over 2 years after intracerebral hemorrhage in school-aged children. Dev Med Child Neurol. 2017;59:1146–1151. doi: 10.1111/dmcn.13547. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.