Abstract
Objective:
The purpose of this study was to analyze the impact of easy access to alcohol and exposure to alcohol advertisements on women’s alcohol consumption, reproductive history, and health and social outcomes in an urban and rural site in South Africa.
Method:
Trained fieldworkers conducted face-to-face interviews with 1,018 women of childbearing age in the Moot, Mamelodi, and Eesterus areas of the City of Tshwane (Gauteng province) and in the rural Cederberg, Bergrivier, and Swartland municipalities (Western Cape province), recruited through random sampling and stratified cluster random sampling, respectively. Multivariate logistic regression analyses were conducted, stratified according to the urban and rural sites and controlled for four demographic factors.
Results:
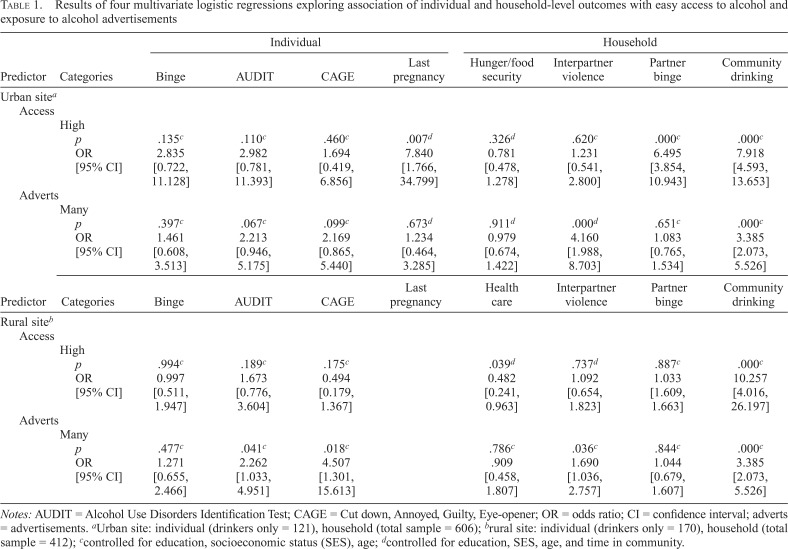
In Tshwane, complications in the last pregnancy (odds ratio [OR] = 7.84, 95% CI [1.77, 34.80]), interpartner binge drinking (OR = 6.50, 95% CI [3.85, 10.94]), and community drinking (OR = 7.92, 95% CI [4.59, 13.65]) were positively associated with alcohol accessibility. Interpartner violence (OR = 4.16, 95% CI [1.99, 8.70]) and community drinking (OR = 3.39, 95% CI [2.07, 5.53]) were positively associated with exposure to alcohol advertisements. In Western Cape, community drinking (OR = 10.26, 95% CI [4.02, 26.20]) was positively associated with alcohol accessibility, whereas ability to pay for health care (OR = 0.48, 95% CI [0.24, 0.96]) was inversely associated. Hazardous drinking on the Alcohol Use Disorders Identification Test (AUDIT; OR = 2.26, 95% CI [1.03, 4.95]) and CAGE (OR = 4.51, 95% CI [1.30, 15.61]), interpartner violence (OR = 1.69, 95% CI [1.04, 2.76]), and community drinking (OR = 3.39, 95% CI [2.07, 5.53]) were positively associated with exposure to alcohol advertisements.
Conclusion:
Easy access to alcohol and exposure to alcohol advertisements are positively associated with adverse health and social outcomes. Although further studies are needed, these findings lend support to emphasizing upstream policy interventions to limit access to alcohol and advertisements.
Alcohol consumption in africa is responsible for approximately 6.4% of deaths and 4.7% of disability-adjusted life years lost (Ferreira-Borges et al., 2015). It is a major risk factor for chronic disease, injury, HIV/AIDS, adverse women’s health outcomes, and interpersonal violence (Ghebremichael et al., 2009; Hingson et al., 2000; Kalichman et al., 2007; Miller et al., 2000; Qian et al., 2014). In the rural Western Cape of South Africa, alcohol use among women is often symptomatic of domestic and sexual violence, poverty, and a complex history of alcohol as a tool of colonization (London, 2000).
Prenatal alcohol use is associated with adverse consequences for the child, including childhood behavioral and developmental disorders (Katwan et al., 2011) and fetal alcohol spectrum disorders (FASD). Effects of FASD include irreversible birth defects that hinder children’s neurological, physical, and social development (Popova et al., 2017). Fetal alcohol syndrome (FAS) is the most severe form of FASD and is common in the Western Cape (Centers for Disease Control and Prevention [CDC], 2003; Te Water-Naude et al., 2000; Urban et al., 2015; Viljoen et al., 2005). In one Western Cape town in the rural West Coast District, a research site in this study, FAS prevalence rate was reported at 17% (Olivier et al., 2013)—the highest rate globally. South Africa’s elevated FAS rates are partly the result of historical practices under colonial agriculture of paying farm workers with alcohol (the Dop system), a practice that, despite its nominal illegality, persisted in some Western Cape farms well into the post-apartheid period (London, 2000). The historical legacy of the Dop system—along with poverty, easy access to alcohol and advertisements, and other intersecting social and health factors—has contributed to high levels of alcohol consumption and dependence in the Western Cape (London, 2000).
Throughout Africa, the alcohol industry has used marketing campaigns and lobbied intensely to halt public health measures aiming to limit alcohol availability (Babor et al., 2015; Jernigan & Babor, 2015). National legislation to ban alcohol advertising and sports sponsorship has been stalled, and equivalent Western Cape provincial legislation restricting access was substantially weakened following aggressive opposition by the liquor, sporting, and advertising industries (Ensor, 2017; Myers, 2015). In addition, self-regulation by alcohol companies has left adolescents vulnerable to the harmful effects of alcohol advertisements (Noel et al., 2017). The alcohol industry claims that it plays an indispensable role in South Africa’s formal and informal economies (Fieldgate et al., 2013). However, the consequences of alcohol consumption cost the economy approximately 10%–12% of South Africa’s 2009 gross domestic product (Matzopoulos et al., 2014; Rehm et al., 2009).
Research has shown that greater exposure to alcohol outlets and advertisements correlates with greater alcohol consumption at the community level (Bryden et al., 2012). Alcohol accessibility is an important risk factor in problem drinking (Donnelly et al., 2006; Grover, 1999; Pearson et al., 2014; Scribner et al., 2000), particularly among adolescents (Chen et al., 2009; Treno et al., 2008). Alcohol advertisements have been shown to influence young people’s attitudes toward drinking (Austin et al., 2006; Babor et al., 2017; Fleming et al., 2004; Hoffman et al., 2014; Pasch et al., 2007; Snyder et al., 2006) and risk of alcohol consumption (Anderson et al., 2009; Hurtz et al., 2007), as well as earlier initiation and heavier drinking globally (Anderson et al., 2009; Jernigan et al., 2017; Smith et al., 2009). In southern Africa, alcohol companies have targeted adolescents and women through heavy marketing and availability (Obot, 2013), potentially contributing to problem drinking among teenage students in Zambia and South Africa (Moyo, 2014; Swahn et al., 2011). Similarly, much alcohol advertising targets young African women (de Bruijn, 2011; European Centre for Monitoring Alcohol Marketing, 2008; Ferreira-Borges et al., 2015).
Given the adverse health, social, and economic consequences of alcohol use, the targeting of women by alcohol companies in Africa, and the significant associations of alcohol accessibility and advertising with early and problem drinking, this study aimed to test the hypotheses that (a) alcohol accessibility and (b) exposure to alcohol advertisements are associated with women’s problem drinking, reproductive complications, and a range of adverse health and social outcomes in urban and rural sites of South Africa. This study addresses a gap in the literature on the effects of alcohol accessibility and advertising among women of childbearing age, thereby helping to inform policy debates (Monteiro et al., 2017).
Method
Research design and sampling
This article analyzes data from a 2006 FAS prevention intervention study in South Africa that surveyed 1,018 women ages 18–44 years living in the Moot, Mamelodi, and Eesterus areas of the City of Tshwane in Gauteng province and in the rural Cederberg, Bergrivier, and Swartland municipalities in the Western Cape province (Morojele et al., 2010). In Tshwane, cluster random sampling was used to recruit 606 women, one from each of 10 households in 82 randomly selected census enumeration areas. In the rural Western Cape, stratified cluster random sampling was used to recruit 412 female participants from 150 randomly selected farms within the boundaries of the three municipalities. Trained fieldworkers administered 15- to 90-minute face-to-face interviews with consenting participants in their preferred language. The Faculty of Health Sciences Research Ethics Committees of the Universities of Pretoria (121/2005) and Cape Town (381/2005) approved the study protocol.
Exposure variables
Two exposure variables—alcohol accessibility and exposure to advertisements—were measured by women’s extent of agreement or disagreement with the prompts “it is easy to buy alcohol in your community if you want to” and “there are many advertisements in your community,” respectively. Both variables were measured on a 5-point Likert scale, which was recoded into a binary scale (score of 0 for those who neither agreed nor disagreed, moderately disagreed, or strongly disagreed and score of 1 for those who strongly or moderately agreed).
Outcome variables
The structured questionnaire included five individual-level and five household-level outcomes related to alcohol use, social impact, and reproductive health. The individual-level outcomes included any history of (a) general and (b) last-pregnancy-related adverse reproductive outcomes and problem drinking. General adverse reproductive impacts, using a history of miscarriage and having children with FAS, generated three categories: no miscarriages and no children with FAS; either at least one miscarriage or a child with FAS; or at least one miscarriage and at least one child with FAS. Adverse reproductive outcomes in the last pregnancy were categorized using a composite variable of complications during last birth, developmental issues of the last child, and adverse outcomes of the last pregnancy as follows: no complications in any category versus a complication in at least one of these categories. Problem drinking variables included (c) self-reported binge drinking (less than 6 drinks per occasion vs. 6 drinks or more per occasion); (d) the 10-item Alcohol Use Disorders Identification Test (AUDIT; Babor et al., 2001) categorized into a score of less than 8 versus a score of 8 or more; and (e) the CAGE questionnaire (Cut down, Annoyed, Guilty, Eyeopener; Mayfield et al., 1974) categorized into a score of less than 2 versus 2 or more.
Household-level alcohol-related outcome variables included (a) partner binge drinking (defined as 6 drinks or more per occasion) and (b) community drinking (participant neither agreed nor disagreed, moderately disagreed, or strongly disagreed that there is a lot of community drinking vs. strongly or moderately agreed). Social impact variables included (c) household hunger and food insecurity combined (household always has money for food and never goes hungry vs. household sometimes/never has enough money for food and/or seldom goes hungry), (d) money for health care (household always has money for health care vs. sometimes/never has enough money for health care), and (e) interpartner violence (participant neither agreed nor disagreed, moderately disagreed, or strongly disagreed that there was sometimes slapping/hitting in the relationship vs. strongly or moderately agreed).
Control variables
Demographic factors included age in three categories (18–24 years, 25–34 years, and 35–44 years old), education (educational status primary schooling or lower vs. above primary education), socioeconomic status (SES; reported possession of less than five out of eight household amenities vs. reporting five or more), and time lived in the community in three categories (0–14 years, 15–29 years, and 30–45 years).
Statistical analysis
Univariate logistic regression analyses were conducted to examine the relationships between the outcome variables and six demographic factors (Supplemental Table A) to determine outcome variables for inclusion in the multivariate regressions (p < .15). Forced entry multivariate logistic regression analyses were then run to explore the association of (a) easy access to alcohol and (b) exposure to alcohol advertising to each of the five individual-level adverse outcomes and the five household-level adverse outcomes, controlling for age, education, socioeconomic status, and time lived in the community (Table 1). Individual-level outcome variables were analyzed among women who had at least one drink in the past month, and household-level outcome variables were examined among both drinking and non-drinking women. Analyses were stratified by location because the urban and rural samples were notably different in terms of languages, historical practices, and sociocultural contexts. A third set of forced entry multiple regressions were conducted to assess whether there is a dose-response relationship between the exposure variables—easy access to alcohol and exposure to advertisements—and the significantly related outcome variables (Supplemental Table C). Analyses were conducted using IBM SPSS Statistics for Windows, Version 23.0 (IBM Corp., Armonk, NY). All statistical tests were two-tailed, using an α of .15 for univariate regression analyses and an α of .05 for multivariate regression analyses.
Table 1.
Results of four multivariate logistic regressions exploring association of individual and household-level outcomes with easy access to alcohol and exposure to alcohol advertisements
| Individual |
Household |
||||||||
| Predictor | Categories | Binge | AUDIT | CAGE | Last pregnancy | Hunger / food security | Interpartner violence | Partner binge | Community drinking |
| Urban sitea | |||||||||
| Access | |||||||||
| High | |||||||||
| p | .135c | .110c | .460c | .007d | .326d | .620c | .000c | .000c | |
| OR | 2.835 | 2.982 | 1.694 | 7.840 | 0.781 | 1.231 | 6.495 | 7.918 | |
| [95% CI] | [0.722, 11.128] | [0.781, 11.393] | [0.419, 6.856] | [1.766, 34.799] | [0.478, 1.278] | [0.541, 2.800] | [3.854, 10.943] | [4.593, 13.653] | |
| Adverts | |||||||||
| Many | |||||||||
| P | .397c | .067c | .099c | .673d | .911d | .000d | .651c | .000c | |
| OR | 1.461 | 2.213 | 2.169 | 1.234 | 0.979 | 4.160 | 1.083 | 3.385 | |
| [95% CI] | [0.608, 3.513] | [0.946, 5.175] | [0.865, 5.440] | [0.464, 3.285] | [0.674, 1.422] | [1.988, 8.703] | [0.765, 1.534] | [2.073, 5.526] | |
| Individual |
Household |
||||||||
| Predictor | Categories | Binge | AUDIT | CAGE | Last pregnancy | Health care | Interpartner violence | Partner binge | Community drinking |
| Rural siteb | |||||||||
| Access | |||||||||
| High | |||||||||
| P | .994c | .189c | .175c | .039d | .737d | .887c | .000c | ||
| OR | 0.997 | 1.673 | 0.494 | 0.482 | 1.092 | 1.033 | 10.257 | ||
| [95% CI] | [0.511, 1.947] | [0.776, 3.604] | [0.179, 1.367] | [0.241, 0.963] | [0.654, 1.823] | [1.609, 1.663] | [4.016, 26.197] | ||
| Adverts | |||||||||
| Many | |||||||||
| p | .477c | .041c | .018c | .786c | .036c | .844c | .000c | ||
| OR | 1.271 | 2.262 | 4.507 | .909 | 1.690 | 1.044 | 3.385 | ||
| [95% CI] | [0.655, 2.466] | [1.033, 4.951] | [1.301, 15.613] | [0.458, 1.807] | [1.036, 2.757] | [0.679, 1.607] | [2.073, 5.526] | ||
Notes: AUDIT = Alcohol Use Disorders Identification Test; CAGE = Cut down, Annoyed, Guilty, Eye-opener; OR = odds ratio; CI = confidence interval; adverts = advertisements.
Urban site: individual (drinkers only = 121), household (total sample = 606);
rural site: individual (drinkers only = 170), household (total sample = 412);
controlled for education, socioeconomic status (SES), age;
controlled for education, SES, age, and time in community.
Results
Participants in the urban (n = 606) and rural (n = 412) sites had similar age distributions (p = .15) but differed in education (28% urban-dwelling women had less than Grade 11 education vs. 92% of rural-dwelling women; p < .001); duration lived in the community (100% urban-dwelling vs. 71% rural-dwelling lived less than 15 years in that site; p < .001); and SES (67% of urban-dwelling women reported ownership of five or more amenities vs. 36% rural-dwelling women; p < .001). Urban-dwelling women identified predominantly as Black/African (81%) and spoke an African language (61%), whereas rural-dwelling women identified mostly as Coloured (91%) and spoke Afrikaans (93%); these were highly significant differences (p < .001).1 In the rural compared with urban sites, a greater percentage reported interpartner violence (39% vs. 10%, respectively, p < .001) and problem drinking at the individual level (87% CAGE score ≥ 2 vs. 8%, respectively, p < .001) (Supplemental Table A).
In the urban and rural sites, the individual-level outcome variable on general adverse reproductive outcomes (history of miscarriage and having children with FAS) and, in the urban site, the household-level outcome “money for health care” were not significantly associated with the exposure variables in the univariate analyses (Supplemental Table B) and were therefore excluded as outcomes for the respective multivariate regression analyses. In addition, univariate regression analyses were conducted confirming that the exposure variables were not themselves related. In the multivariate regression analyses controlling for demographic factors (Table 1), women in the urban site with easy access to alcohol were 7.8 times more likely to have experienced complications in the last pregnancy (95% CI [1.8, 34.8]), 6.5 times more likely to have a partner who binge drinks (95% CI [3.9, 10.9]), and 7.9 times more likely to report heavy community drinking (95% CI [4.6, 13.7]).
Women who reported high exposure to alcohol advertisements were 4.2 times more likely to experience interpartner violence (95% CI [2.0, 8.7]) and 3.4 times more likely to report heavy community drinking (95% CI [2.1, 5.5]). Rural-dwelling women with easy access to alcohol were 10.3 times more likely to report heavy community drinking (95% CI [4.0, 26.2]) and less likely to report household hunger/food insecurity (odds ratio [OR] = 0.5, 95% CI [0.2, 1.0]). Rural-dwelling women who reported high exposure to alcohol advertisements were 2.3 times more likely to report hazardous drinking according to AUDIT (95% CI [1.0, 5.0]), 4.5 times more likely to report problem drinking according to CAGE (95% CI [1.3, 15.6]), 1.7 times more likely to report interpartner violence (95% CI [1.0, 2.8]), and 3.4 times more likely to report heavy community drinking (95% CI [2.1, 5.5]).
Analyses of dose responses (Supplemental Table C) in the urban site suggested that there was a positive dose-response relationship for easy access to alcohol with reported community drinking. Compared with the category strongly disagree, ORs for high levels of community drinking increased from 0.9 for the category less than moderate agreement to 4.5 for the category moderate agreement to 6.3 for the category of strong agreement regarding easy access. There was also a positive dose-response relationship for exposure to alcohol advertisements with adverse outcomes. Compared with the category strongly disagree, ORs for problem drinking according to CAGE increased from 2.9 for the category less than moderate agreement and 2.6 for the category moderate agreement to 6.4 for the category of strong agreement regarding the presence of many advertisements in the community. Interpartner violence also showed a suggestive trend of association with advertising. Compared with the category strongly disagree, ORs for interpartner violence increased from 0.8 for the category less than moderate agreement to 2.7 for the category moderate agreement to 4.5 for the category of strong agreement regarding the presence of many advertisements in the community. Last, a similar pattern emerged with community drinking. Compared with the category strongly disagree, ORs for community drinking increased from 1.0 for the category less than moderate agreement to 3.1 for the category moderate agreement to 3.7 for the category of strong agreement regarding the presence of many advertisements in the community.
In the rural site, there was a negative dose-response relationship between easy access to alcohol and ability to pay for health care (those reporting moderate and strong agreement were 0.8 and 0.4 times more likely to report having money for health care, respectively, though this relationship was not statistically significant). There was a nonlinear increasing dose-response relationship between easy access and community drinking. Compared with the category strongly disagree, the categories reporting less than moderate agreement, moderate agreement, and strong agreement regarding easy access to alcohol were 1.4, 20.7 and 6.2 times more likely to report a lot of community drinking, respectively. Exposure to advertisements also demonstrated a positive dose-response relationship for three outcomes. Compared with the category strongly disagree, the categories reporting less than moderate agreement, moderate agreement, and strong agreement regarding advertising exposure were 0.9, 1.9, and 2.4 times more likely to report high AUDIT; were 1.1, 3.5, and 1.3 times more likely to report interpartner violence (slapping/hitting in the relationship) and 2.2, 6.2, and 2.1 times more likely to report a lot of community drinking, respectively.
Discussion
In both urban and rural sites, reported easy access to alcohol and exposure to alcohol advertisements were associated with adverse social and health outcomes. In urban Tshwane, easy access to alcohol was related to partner binge drinking, problem drinking in the community, and complications during pregnancy. Exposure to alcohol advertisements was related to hazardous drinking in the community and interpartner violence. In rural Western Cape, easy access to alcohol was related to community drinking and inversely related to the family’s ability to pay for health care. Exposure to alcohol advertisements was related to hazardous drinking among women, community drinking, and interpartner violence. These findings were generally supported by demonstration of dose-response effects for both advertising and access.
Differences in the findings between the urban and rural sites likely lie in the varied cultural, educational, and socioeconomic contexts of the different communities included in the study. Also, given the history of the Dop system in the Western Cape and its more recent manifestation as alcohol sold to workers but directly deducted from farm workers’ salaries (London, 2000), farm workers may have understated responses to “it is easy for you to buy alcohol in your community if you want to.” Limited disposable income in rural farm worker populations would also mean that the ease of accessing alcohol may not be best captured by a question linking easy access to an exchange of money (Atkinson, 2007; Kleinbooi, 2013).
Limitations
First, although research in comparable South African communities has found that women are unlikely to underreport alcohol use (May et al., 2005), there may still have been some social desirability and recall biases regarding alcohol use and other behaviors, despite assurances of confidentiality. Second, the exposure variables—alcohol accessibility and exposure to advertisements—are based on participants’ reports rather than objective measurements and should, ideally, be validated in future studies. Third, the sample did not include females below 18 or over 44 years and the data were collected in 2006, meaning that they may have become dated. Last, with a cross-sectional design, one cannot make firm conclusions on causality and further studies of more rigorous design would be needed to do so.
However, although the results from select urban and rural sites cannot represent the whole country, this is the first study in South Africa to identify potential associations involving easy access to alcohol and exposure to alcohol advertisements with adverse health and social outcomes. The study findings are generally consistent with literature on the relationships between alcohol accessibility, alcohol use, and a range of factors including sexual risks and food insecurity among women in southern Africa (Dewing et al., 2013; Eaton et al., 2014; Kalichman et al., 2007; Onah et al., 2016). Moreover, in both sites, education and socioeconomic status were negatively correlated with a range of adverse outcomes and positively correlated with ability to pay for health care—intuitive findings supporting the validity of the instruments used in this study and the findings regarding alcohol accessibility and advertisements.
Implications
The findings suggest that easy access to alcohol and exposure to alcohol advertisements are associated with a number of adverse health and social outcomes. In South Africa, despite the World Health Organization’s (WHO) policy recommendations for alcohol reduction strategies (WHO, 2010), the Department of Health and other government ministries face pressure from the alcohol industry to weaken or stall regulatory policies, often at the expense of the social, economic, and physical well-being of families in urban and rural South Africa. Nevertheless, upstream policy interventions that limit access to alcohol and advertisements by regulating the alcohol and marketing industries appear to be supported by these findings. Moreover, these results lend important insights for other low- and middle-income countries facing significant alcohol-related burdens of disease and injury, as well as economic costs (Benegal et al., 2005; Noto et al., 2015).
Footnotes
This work was supported by Grants Cooperative Agreement Number 1 U01 DD00044 from the Centers for Disease Control and Prevention, Kirstie Rendall-Mkosi, principal investigator, and Grant MD 001452 from the National Center on Minority Health and Health Disparities of the National Institutes of Health, Luz Claudio, principal investigator.
In the Western Cape of South Africa, “Coloured” has referred to heterogenous communities of mixed heritage—including Malay and Khoi-San—that typically speak Afrikaans and English. The usage of this term is specific to the historical and sociopolitical contexts in which this study was conducted and is not meant to condone racial categorization.
References
- Anderson P., de Bruijn A., Angus K., Gordon R., Hastings G. Impact of alcohol advertising and media exposure on adolescent alcohol use: A systematic review of longitudinal studies. Alcohol and Alcoholism. 2009;44:229–243. doi: 10.1093/alcalc/agn115. doi:10.1093/alcalc/agn115. [DOI] [PubMed] [Google Scholar]
- Atkinson D. Cape Town, South Africa: HSRC Press; 2007. Going for broke: The fate of farm workers in arid South Africa. [Google Scholar]
- Austin E. W., Chen M. J., Grube J. W. How does alcohol advertising influence underage drinking? The role of desirability, identification and skepticism. Journal of Adolescent Health. 2006;38:376–384. doi: 10.1016/j.jadohealth.2005.08.017. doi:10.1016/j.jadohealth.2005.08.017. [DOI] [PubMed] [Google Scholar]
- Babor T. F., Higgins-Biddle J. C., Saunders J. B., Monteiro M. G. Geneva, Switzerland: World Health Organization; 2001. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for use in primary care. [Google Scholar]
- Babor T. F., Robaina K., Jernigan D. The influence of industry actions on the availability of alcoholic beverages in the African region. Addiction. 2015;110:561–571. doi: 10.1111/add.12832. doi:10.1111/add.12832. [DOI] [PubMed] [Google Scholar]
- Babor T. F., Robaina K., Noel J. K., Ritson E. B. Vulnerability to alcohol-related problems: A policy brief with implications for the regulation of alcohol marketing. Addiction. 2017;112(Supplement 1):94–101. doi: 10.1111/add.13626. doi:10.1111/add.13626. [DOI] [PubMed] [Google Scholar]
- Benegal V., Nayak M., Murthy P., Chandra P., Gururaj G. Women and alcohol use in India. In: Obot I. S., Room R., editors. Alcohol, gender and drinking problems: Perspectives from low and middle income countries. Geneva, Switzerland: World Health Organization; 2005. pp. 89–124. [Google Scholar]
- Bryden A., Roberts B., McKee M., Petticrew M. A systematic review of the influence on alcohol use of community level availability and marketing of alcohol. Health & Place. 2012;18:349–357. doi: 10.1016/j.healthplace.2011.11.003. doi:10.1016/j.healthplace.2011.11.003. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Fetal alcohol syndrome—South Africa, 2001. Morbidity and Mortality Weekly Report. 2003;52:660–662. [PubMed] [Google Scholar]
- Chen M. J., Gruenewald P. J., Remer L. G. Does alcohol outlet density affect youth access to alcohol? Journal of Adolescent Health. 2009;44:582–589. doi: 10.1016/j.jadohealth.2008.10.136. doi:10.1016/j.jadohealth.2008.10.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruijn A. Utrecht: The Netherlands: Dutch Institute for Alcohol Policy (STAP); 2011. Alcohol marketing practices in Africa: Findings from the Gambia, Ghana, Nigeria and Uganda. [Google Scholar]
- Dewing S., Tomlinson M., le Roux I. M., Chopra M., Tsai A. C. Food insecurity and its association with co-occurring postnatal depression, hazardous drinking, and suicidality among women in peri-urban South Africa. Journal of Affective Disorders. 2013;150:460–465. doi: 10.1016/j.jad.2013.04.040. doi:10.1016/j.jad.2013.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly N., Poynton S., Weatherburn D., Bamford E., Nottage J. Liquor outlet concentrations and alcohol-related neighbourhood problems. BOCSAR NSW Alcohol Studies Bulletin. 2006;15 Retrieved from http://www.bocsar.nsw.gov.au/Documents/BB/ab08.pdf. [Google Scholar]
- Eaton L. A., Pitpitan E. V., Kalichman S. C., Sikkema K. J., Skinner D., Watt M. H., Cain D. N. Food insecurity and alcohol use among pregnant women at alcohol-serving establishments in South Africa. Prevention Science. 2014;15:309–317. doi: 10.1007/s11121-013-0386-6. doi:10.1007/s11121-013-0386-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ensor L. Nedlac stalls on tough liquor law changes without social-cost report. Business Day (South Africa) 2017 Retrieved from https://www.businesslive.co.za/bd/national/2017-05-30-nedlac-stalls-on-tough-liquor-law-changes-without-social-cost-report. [Google Scholar]
- European Centre for Monitoring Alcohol Marketing. Utrecht, The Netherlands: Author; 2008. Women—The new market: Trends in alcohol marketing. Retrieved from http://eucam.info/2008/05/06/women-the-new-market/ [Google Scholar]
- Ferreira-Borges C., Dias S., Babor T., Esser M. B., Parry C. D. Alcohol and public health in Africa: Can we prevent alcohol-related harm from increasing? Addiction. 2015;110:1373–1379. doi: 10.1111/add.12916. doi:10.1111/add.12916. [DOI] [PubMed] [Google Scholar]
- Fieldgate I., Jeffrey R., Madinane M., Ebrahim Y., Soobyah L., Jordaan J. Economic impact of an advertising ban on alcoholic beverages: For industry association for responsible alcohol use. 2013 Retrieved from http://5737034557ef5b8c02c0e46513b98f90.cdn.ilink247.com/ClientFiles/econometrix/Econometrix/Company/Documents/Economic_Impact_of_an_Ad_Ban_Econometrix.pdf.
- Fleming K., Thorson E., Atkin C. K. Alcohol advertising exposure and perceptions: Links with alcohol expectancies and intentions to drink or drinking in underaged youth and young adults. Journal of Health Communication. 2004;9:3–29. doi: 10.1080/10810730490271665. doi:10.1080/10810730490271665. [DOI] [PubMed] [Google Scholar]
- Ghebremichael M., Paintsil E., Larsen U. Alcohol abuse, sexual risk behaviors, and sexually transmitted infections in women in Moshi urban district, northern Tanzania. Sexually Transmitted Diseases. 2009;36:102–107. doi: 10.1097/OLQ.0b013e31818b20e6. doi:10.1097/OLQ.0b013e31818b20e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover P. L. U.S. Dept. of Health & Human Services; 1999. Preventing problems related to alcohol availability: Environmental approaches (Reference guide) [Google Scholar]
- Hingson R. W., Heeren T., Jamanka A., Howland J. Age of drinking onset and unintentional injury involvement after drinking. JAMA. 2000;284:1527–1533. doi: 10.1001/jama.284.12.1527. doi:10.1001/jama.284.12.1527. [DOI] [PubMed] [Google Scholar]
- Hoffman E. W., Pinkleton B. E., Weintraub Austin E., Reyes-Velázquez W. Exploring college students’ use of general and alcohol-related social media and their associations with alcohol-related behaviors. Journal of American College Health. 2014;62:328–335. doi: 10.1080/07448481.2014.902837. doi:10.1080/07448481.2014.902837. [DOI] [PubMed] [Google Scholar]
- Hurtz S. Q., Henriksen L., Wang Y., Feighery E. C., Fortmann S. P. The relationship between exposure to alcohol advertising in stores, owning alcohol promotional items, and adolescent alcohol use. Alcohol and Alcoholism. 2007;42:143–149. doi: 10.1093/alcalc/agl119. doi:10.1093/alcalc/agl119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jernigan D. H., Babor T. F. The concentration of the global alcohol industry and its penetration in the African region. Addiction. 2015;110:551–560. doi: 10.1111/add.12468. doi:10.1111/add.12468. [DOI] [PubMed] [Google Scholar]
- Jernigan D., Noel J., Landon J., Thornton N., Lobstein T. Alcohol marketing and youth alcohol consumption: A systematic review of longitudinal studies published since 2008. Addiction. 2017;112(Supplement S1):7–20. doi: 10.1111/add.13591. doi:10.1111/add.13591. [DOI] [PubMed] [Google Scholar]
- Kalichman S. C., Simbayi L. C., Kaufman M., Cain D., Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: Systematic review of empirical findings. Prevention Science. 2007;8:141–151. doi: 10.1007/s11121-006-0061-2. doi:10.1007/s11121-006-0061-2. [DOI] [PubMed] [Google Scholar]
- Katwan E., Adnams C., London L. Childhood behavioural and developmental disorders: association with maternal alcohol consumption in Cape Town, South Africa. South African Medical Journal. 2011;101:724–727. [PubMed] [Google Scholar]
- Kleinbooi K. Bellville, South Africa: Institute for Poverty, Land and Agrarian Studies (PLAAS), School of Government, University of the Western Cape; 2013. Farmworkers’ living and working conditions: Workshop report. Retrieved from http://www.plaas.org.za/sites/default/files/publications-pdf/farmworkers%20living%20working%20conditions.pdf. [Google Scholar]
- London L. Alcohol consumption amongst South African farm workers: A challenge for post-apartheid health sector transformation. Drug and Alcohol Dependence. 2000;59:199–206. doi: 10.1016/s0376-8716(99)00120-9. doi:10.1016/S0376-8716(99)00120-9. [DOI] [PubMed] [Google Scholar]
- Matzopoulos R. G., Truen S., Bowman B., Corrigall J. The cost of harmful alcohol use in South Africa. South African Medical Journal. 2014;104:127–132. doi: 10.7196/samj.7644. doi:10.7196/samj.7644. [DOI] [PubMed] [Google Scholar]
- May P. A., Gossage J. P., Brooke L. E., Snell C. L., Marais A. S., Hendricks L. S., Viljoen D. L. Maternal risk factors for fetal alcohol syndrome in the Western Cape Province of South Africa: A population-based study. American Journal of Public Health. 2005;95:1190–1199. doi: 10.2105/AJPH.2003.037093. doi:10.2105/AJPH.2003.037093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayfield D., McLeod G., Hall P. The CAGE questionnaire: Validation of a new alcoholism screening instrument. American Journal of Psychiatry. 1974;131:1121–1123. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- Miller B. A., Wilsnack S. C., Cunradi C. B. Family violence and victimization: Treatment issues for women with alcohol problems. Alcoholism: Clinical and Experimental Research. 2000;24:1287–1297. doi:10.1111/j.1530-0277.2000.tb02095.x. [PubMed] [Google Scholar]
- Monteiro M. G., Babor T. F., Jernigan D., Brookes C. Alcohol marketing regulation: From research to public policy. Addiction. 2017;112(Supplement 1):3–6. doi: 10.1111/add.13660. doi:10.1111/add.13660. [DOI] [PubMed] [Google Scholar]
- Morojele N. K., London L., Olorunju S. A., Matjila M. J., Davids A. S., Rendall-Mkosi K. M. Predictors of risk of alcohol-exposed pregnancies among women in an urban and a rural area of South Africa. Social Science & Medicine. 2010;70:534–542. doi: 10.1016/j.socscimed.2009.10.040. doi:10.1016/j.socscimed.2009.10.040. [DOI] [PubMed] [Google Scholar]
- Moyo L. Effects of alcohol advertisements and alcohol consumption amongst adolescents in selected high schools in the Eastern Cape, South Africa. Mediterranean Journal of Social Sciences. 2014;5:1649–1659. doi:10.5901/mjss.2014.v5n23p1649. [Google Scholar]
- Myers J. E. Department of the Premier, Western Cape Government; South Africa: 2015. Rapid review of the problem of alcohol harm reduction in the Western Cape Province. [Google Scholar]
- Noel J. K., Babor T. F., Robaina K. Industry self-regulation of alcohol marketing: A systematic review of content and exposure research. Addiction. 2017;112(Supplement 1):28–50. doi: 10.1111/add.13410. doi:10.1111/add.13410. [DOI] [PubMed] [Google Scholar]
- Noto A. R., Botéquio M. C., Lucas Dos Santos E., Bedendo A., Pinsky I. The hidden role of the alcohol industry in youth drinking in Brazil [Letter to the Editor] Journal of Studies on Alcohol and Drugs. 2015;76:981. doi: 10.15288/jsad.2015.76.981. doi:10.15288/jsad.2015.76.981. [DOI] [PubMed] [Google Scholar]
- Obot I. S. Commentary: Alcohol marketing in Africa: Not an ordinary business. African Journal of Drug and Alcohol Studies. 2013;12:63–73. Retrieved from https://www.ajol.info/index.php/ajdas/article/view/96893/86208. [Google Scholar]
- Olivier L., Urban M., Chersich M., Temmerman M., Viljoen D. Burden of fetal alcohol syndrome in a rural West Coast area of South Africa. South African Medical Journal. 2013;103:402–405. doi: 10.7196/samj.6249. doi:10.7196/SAMJ.6249. [DOI] [PubMed] [Google Scholar]
- Onah M. N., Field S., Heyningen T., Honikman S. Predictors of alcohol and other drug use among pregnant women in a peri-urban South African setting. International Journal of Mental Health Systems. 2016;10:38. doi: 10.1186/s13033-016-0070-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasch K. E., Komro K. A., Perry C. L., Hearst M. O., Farbakhsh K. Outdoor alcohol advertising near schools: What does it advertise and how is it related to intentions and use of alcohol among young adolescents? Journal of Studies on Alcohol and Drugs. 2007;68:587–596. doi: 10.15288/jsad.2007.68.587. doi:10.15288/jsad.2007.68.587. [DOI] [PubMed] [Google Scholar]
- Pearson A. L., Bowie C., Thornton L. E. Is access to alcohol associated with alcohol/substance abuse among people diagnosed with anxiety/mood disorder? Public Health. 2014;128:968–976. doi: 10.1016/j.puhe.2014.07.008. doi:10.1016/j.puhe.2014.07.008. [DOI] [PubMed] [Google Scholar]
- Popova S., Lange S., Probst C., Gmel G., Rehm J. Estimation of national, regional, and global prevalence of alcohol use during pregnancy and fetal alcohol syndrome: A systematic review and meta-analysis. The Lancet Global Health. 2017;5:e290–e299. doi: 10.1016/S2214-109X(17)30021-9. doi:10.1016/S2214-109X(17)30021-9. [DOI] [PubMed] [Google Scholar]
- Qian F., Ogundiran T., Hou N., Ndom P., Gakwaya A., Jombwe J., Huo D. Alcohol consumption and breast cancer risk among women in three sub-Saharan African countries. PLoS ONE. 2014;9(9):e106908. doi: 10.1371/journal.pone.0106908. doi:10.1371/journal.pone.0106908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Mathers C., Popova S., Thavorncharoensap M., Teerawattananon Y., Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. doi:10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Scribner R. A., Cohen D. A., Fisher W. Evidence of a structural effect for alcohol outlet density: A multilevel analysis. Alcoholism: Clinical and Experimental Research. 2000;24:188–195. doi:10.1111/j.1530-0277.2000.tb04590.x. [PubMed] [Google Scholar]
- Smith L. A., Foxcroft D. R. The effect of alcohol advertising, marketing and portrayal on drinking behaviour in young people: Systematic review of prospective cohort studies. BMC Public Health. 2009;9:51. doi: 10.1186/1471-2458-9-51. doi:10.1186/1471-2458-9-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder L. B., Milici F. F., Slater M., Sun H., Strizhakova Y. Effects of alcohol advertising exposure on drinking among youth. Archives of Pediatrics & Adolescent Medicine. 2006;160:18–24. doi: 10.1001/archpedi.160.1.18. doi:10.1001/archpedi.160.1.18. [DOI] [PubMed] [Google Scholar]
- Swahn M. H., Ali B., Palmier J. B., Sikazwe G., Mayeya J. Alcohol marketing, drunkenness, and problem drinking among Zambian youth: Findings from the 2004 Global School-Based Student Health Survey. Journal of Environmental and Public Health. 2011;2011 doi: 10.1155/2011/497827. Article ID 497827. doi:10.1155/2011/497827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Te Water-Naude J. M., Charlton K., Sayed R., Dausab M., Marco C., Rendall-Mkosi K., London L. Health on Farms – Stellenbosch 1998 Dopstop Association. HST Update. 2000;1(53):17–19. [Google Scholar]
- Treno A. J., Ponicki W. R., Remer L. G., Gruenewald P. J. Alcohol outlets, youth drinking, and self-reported ease of access to alcohol: A constraints and opportunities approach. Alcoholism: Clinical and Experimental Research. 2008;32:1372–1379. doi: 10.1111/j.1530-0277.2008.00708.x. doi:10.1111/j.1530-0277.2008.00708.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urban M. F., Olivier L., Viljoen D., Lombard C., Louw J. G., Drotsky L.-M., Chersich M. F. Prevalence of fetal alcohol syndrome in a South African city with a predominantly Black African population. Alcoholism: Clinical and Experimental Research. 2015;39:1016–1026. doi: 10.1111/acer.12726. doi:10.1111/acer.12726. [DOI] [PubMed] [Google Scholar]
- Viljoen D. L., Gossage J. P., Brooke L., Adnams C. M., Jones K. L., Robinson L. K., May P. A. Fetal alcohol syndrome epidemiology in a South African community: A second study of a very high prevalence area. Journal of Studies on Alcohol. 2005;66:593–604. doi: 10.15288/jsa.2005.66.593. doi:10.15288/jsa.2005.66.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Geneva, Switzerland: Author; 2010. Global strategy to reduce the harmful use of alcohol. Retrieved from http://www.who.int/substance_abuse/activities/gsrhua/en/ [Google Scholar]