Abstract
Objective:
Few studies have found support for coping as a mechanism of behavior change (MOBC) following coping skills training interventions for alcohol use disorder (AUD). One potential reason for null findings is heterogeneity in the patterns of coping skills acquired during treatment. This study sought to identify latent classes of coping and to test the latent class variable as a mediator of the effect of a combined behavioral intervention for AUD.
Method:
Secondary analyses of data from the Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence (COMBINE) Study (N = 1,124; mean age = 44.4 years; 69.1% male; 23.2% non-White), a multisite study of medication and behavioral treatments for individuals with AUD. Latent class mediation models were estimated to test whether patterns of alcohol-specific coping mediated the effect of combined behavioral intervention with medication management, as compared with medication management only, on drinking outcomes 12 months following treatment.
Results:
Three classes were identified, which differed in repertoire broadness, or the degree in which a wide range of different skills were used. Coping repertoire class was a significant mediator of the effect of the combined behavioral intervention on drinking outcomes. Receiving the combined behavioral intervention, in addition to medication management, predicted a greater likelihood of expected classification in the broad coping repertoire class, which in turn was associated with significant improvements in drinking outcomes.
Conclusions:
Using the novel methodological approach of latent class mediation, this study identified coping repertoire as a significant mediator of behavioral intervention efficacy for AUD. Future work examining heterogeneity in mediators and outcomes may help refine AUD treatment to be maximally effective.
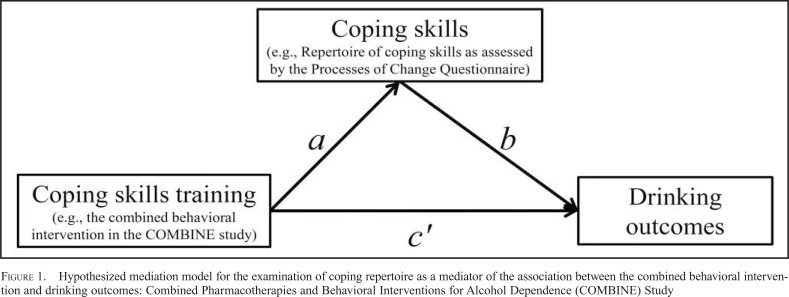
Mechanisms of behavior change (MOBCs) can be defined as processes by which behavior change occurs, and, in the context of treatment, it is often defined as processes through which a treatment is effective (Kazdin, 2007). Alcohol use disorder (AUD) treatment researchers have considered many different mediators, defined as intervening variables that explain an association between the treatment (independent variable) and the outcome (dependent variables), to support specific MOBCs (Longabaugh et al., 2005). For example, one variable that has received a great deal of attention as a potential MOBC of behavioral treatments for AUD is coping (Morgenstern & Longabaugh, 2000). Coping skills training is a core feature of numerous behavioral skills training approaches for AUD (Kadden et al., 1989; Litt et al., 2003; Marlatt & Donovan, 2005). As shown in Figure 1, it has been hypothesized that coping skills training, as compared with alternative treatments, should produce significant improvements in coping skills (the a path), and improvements in coping skills should be associated with significantly better drinking outcomes (the b path). Thus, the effect of coping skills training on better drinking outcomes (the c path) would be explained by the significant mediating (i.e., indirect, a × b path) effect of coping skills. Yet, few studies have provided support for coping as a mediator of the effects of coping skills training (Morgenstern & Longabaugh, 2000).
Figure 1.
Hypothesized mediation model for the examination of coping repertoire as a mediator of the association between the combined behavioral intervention and drinking outcomes: Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence (COMBINE) Study
Heterogeneity in alcohol use disorder clinical course and mechanisms of behavior change
One potential explanation for why evidence for hypothesized MOBCs is not found or not replicated is individual heterogeneity in processes of change. There are several ways in which heterogeneity in patient characteristics, treatment targets, and processes of change may produce null findings for any particular mediator. First, failures of a mediation model to detect effects of treatment on outcomes via hypothesized MOBCs could be because of heterogeneity in outcomes (Gueorguieva et al., 2010; Witkiewitz, 2008; Witkiewitz et al., 2010). Second, failures of a mediation model to detect critical treatment effects on the mediator can potentially be the result of significant heterogeneity in the mediator (Roos & Witkiewitz, 2016).
Recently, Roos and Witkiewitz (2016) identified significant heterogeneity in coping responses following AUD treatment, such that individuals could be characterized into one of three latent classes (i.e., subgroups) characterized by discrete patterns of coping responses. Those who had the broadest repertoire of coping responses had the best drinking outcomes following treatment. Furthermore, those who received a behavioral intervention versus those who received medication management were significantly more likely to be in the broadest repertoire subgroup. Roos and Witkiewitz (2016) did not test whether coping responses mediated the effects of the behavioral intervention on drinking outcomes.
Unfortunately, there is little guidance for testing the significance of the mediated effect when the mediator and/or outcome variables are latent class variables (Muthén & Asparouhov, 2015; VanderWeele, 2016), and no prior studies have examined heterogeneity in mediators and outcomes in the context of AUD treatment research. The primary goal of the present study was to identify latent classes of coping and to test the latent class variable as a statistical mediator of the effect of a combined behavioral intervention for AUD among individuals in the Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence (COMBINE) Study.
Method
Participants and procedures
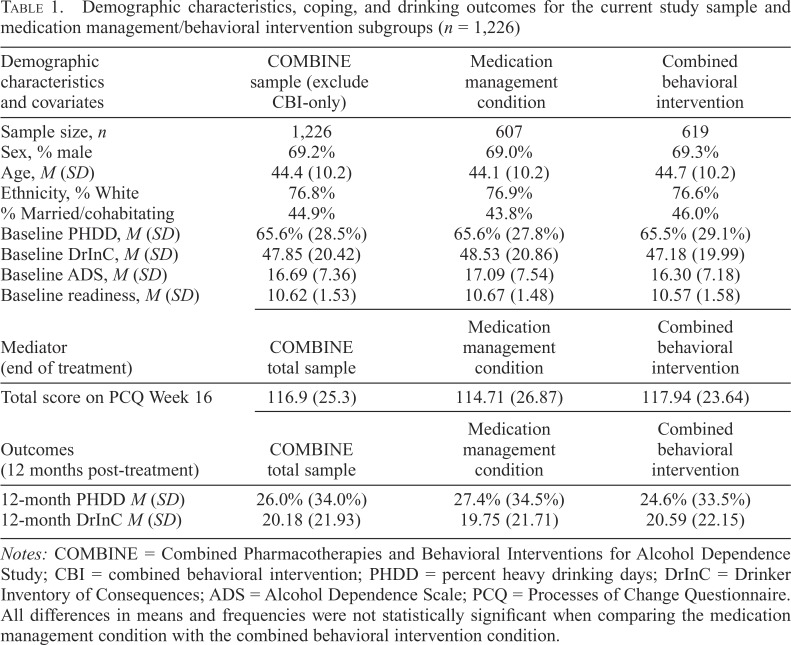
The current study is a secondary data analysis of the COMBINE Study data (Anton et al., 2006; COMBINE Study Research Group, 2003). Participants (N = 1,383) in COMBINE were recruited from 11 research units across the United States. All participants met criteria for alcohol dependence based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 1994), and all participants were seeking outpatient alcohol treatment. Descriptive information about participants in the total sample and separated by the behavioral intervention treatment conditions is provided in Table 1.
Table 1.
Demographic characteristics, coping, and drinking outcomes for the current study sample and medication management/behavioral intervention subgroups (n = 1,226)
| Demographic characteristics and covariates | COMBINE sample (exclude CBI-only) | Medication management condition | Combined behavioral intervention |
| Sample size, n | 1,226 | 607 | 619 |
| Sex, % male | 69.2% | 69.0% | 69.3% |
| Age, M (SD) | 44.4 (10.2) | 44.1 (10.2) | 44.7 (10.2) |
| Ethnicity, % White | 76.8% | 76.9% | 76.6% |
| % Married/cohabitating | 44.9% | 43.8% | 46.0% |
| Baseline PHDD, M (SD) | 65.6% (28.5%) | 65.6% (27.8%) | 65.5% (29.1%) |
| Baseline DrInC, M (SD) | 47.85 (20.42) | 48.53 (20.86) | 47.18 (19.99) |
| Baseline ADS, M (SD) | 16.69 (7.36) | 17.09 (7.54) | 16.30 (7.18) |
| Baseline readiness, M (SD) | 10.62 (1.53) | 10.67 (1.48) | 10.57 (1.58) |
| Mediator (end of treatment) | COMBINE total sample | Medication management condition | Combined behavioral intervention |
| Total score on PCQ Week 16 | 116.9 (25.3) | 114.71 (26.87) | 117.94 (23.64) |
| Outcomes (12 months post-treatment) | COMBINE total sample | Medication management condition | Combined behavioral intervention |
| 12-month PHDD M (SD) | 26.0% (34.0%) | 27.4% (34.5%) | 24.6% (33.5%) |
| 12-month DrInC M (SD) | 20.18 (21.93) | 19.75 (21.71) | 20.59 (22.15) |
Notes: COMBINE = Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence Study; CBI = combined behavioral intervention; PHDD = percent heavy drinking days; DrInC = Drinker Inventory of Consequences; ADS = Alcohol Dependence Scale; PCQ = Processes of Change Questionnaire. All differences in means and frequencies were not statistically significant when comparing the medication management condition with the combined behavioral intervention condition.
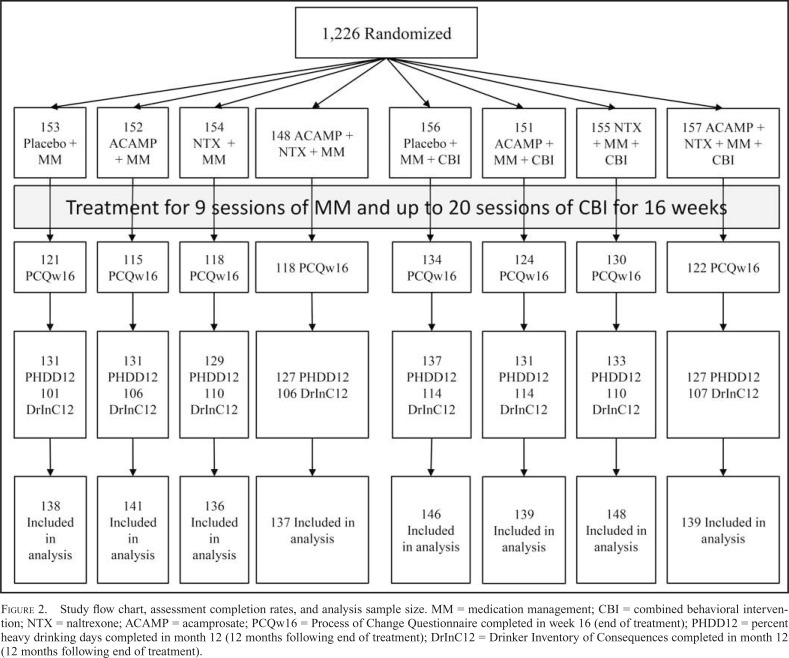
Participants were randomized within each site to one of nine treatment conditions, with eight of the treatment conditions including combinations of medication (naltrexone, acamprosate, or placebo equivalents) and behavioral interventions (combined behavioral intervention [CBI] and/or medication management [MM]) and the ninth treatment condition consisting of the CBI-only without any pills or MM. We excluded individuals in the CBI-only condition (n = 157; see flow chart in Figure 2) given that they did not receive MM or medications. The CBI protocol (Miller, 2004) was designed as an individual behavioral treatment that included up to 20 sessions over 16 weeks. The majority of treatment sessions were focused on cognitive-behavioral coping skills training (Kadden et al., 2003). Individuals who received CBI + MM were coded as CBI = 1, and individuals who received MM-only were coded as CBI = 0.
Figure 2.
Study flow chart, assessment completion rates, and analysis sample size. MM = medication management; CBI = combined behavioral intervention; NTX = naltrexone; ACAMP = acamprosate; PCQw16 = Process of Change Questionnaire completed in week 16 (end of treatment); PHDD12 = percent heavy drinking days completed in month 12 (12 months following end of treatment); DrInC12 = Drinker Inventory of Consequences completed in month 12 (12 months following end of treatment).
COMBINE included an extensive assessment battery, and the assessments used in the current study are described below. For more information about the COMBINE Study, including participation rates, we refer interested readers to the primary publications from the study (Anton et al., 2006; LoCastro et al., 2009; Miller et al., 2005).
Measures
Coping skills.
The Processes of Change Questionnaire (PCQ; Prochaska et al., 1988), adapted for AUD populations (DiClemente et al., 1994), was used to assess alcohol-specific coping skills, assessed at the end of treatment (Week 16 assessment). The PCQ is a 40-item, self-report measure that assesses the frequency of using several different coping skills to prevent drinking (e.g., engaging in alterative activities, seeking social support, avoiding cues). Participants (n = 1,101, 89.9% with complete data) respond to each item on a five-point Likert-type scale (ranging from 1 = never to 5 = repeatedly). Reliability analyses indicated that the reliability of the total scale was acceptable (α = .941).
Alcohol use outcomes.
The Form 90 (Miller, 1996) was used to assess alcohol use outcomes during 90-day windows. We examined the percentage of heavy drinking days (PHDD) during the baseline window and at the 1-year follow-up assessment (Week 68 post-baseline, Week 52 post-treatment; n = 1,171, 95.5% with complete data) as the primary alcohol use outcome. A heavy drinking day was defined as four or more standard drinks for females and five or more standard drinks for males.
Alcohol-related consequences.
Alcohol-related consequences were assessed with the Drinker Inventory of Consequences (DrInC; Miller et al., 1995), a 50-item measure of problems related to alcohol use assessed using a Likert-type response scale (1 = never, 4 = daily or almost daily). In this study, we used the DrInC to assess alcohol-related consequences at baseline and at the 1-year follow-up assessment (n = 969, 79.0% with complete data).
Covariates.
A demographic questionnaire was used to assess self-reported sex, race/ethnicity, marital status, and age. The University of Rhode Island Change Assessment (URICA) was used to measure overall readiness to change at baseline (McConnaughy et al., 1983). The Alcohol Dependence Scale (ADS), a 25-item self-report measure of dependence severity, was used to assess baseline severity of alcohol dependence (Skinner & Horn, 1984). These covariates were selected based on prior research establishing the associations between the covariates and drinking outcomes and/or coping repertoire in the COMBINE Study (Anton et al., 2006; Roos & Witkiewitz, 2016).
Statistical analyses
Mplus Version 7.4 (Muthén & Muthén, 2012) was used for all analyses, and all variables were checked for distributional assumptions and outliers before the analyses. The drinking outcomes were non-normal with an inflation of zeroes for both the PHDD and DrInC outcomes, which led to our use of latent class models for the drinking outcomes (described below). Considering the complex sampling design in the COMBINE Study (participants recruited from 11 academic sites), all parameters were estimated using a robust maximum likelihood estimator in which all the standard errors were computed using a sandwich estimator (Yuan & Bentler, 2010) correcting for potential within-site intracorrelation. The robust maximum likelihood estimator also accommodates missing data for endogenous variables (e.g., PCQ items, drinking outcomes), given at least some available data on either PCQ or drinking outcomes and assuming the data are missing at random (Schafer & Graham, 2002; Witkiewitz et al., 2014). Individuals with missing data on covariates (n = 11) and those with no PCQ data and no drinking outcome data (n = 91) were excluded; thus, the analysis sample size was 1,124 (91.6% of 1,226 who received MM or MM + CBI). Attrition analyses revealed no significant differences on any study variables between those with missing data and those with complete data. Two primary analysis approaches were used in the current study: latent class analysis (LCA) and latent class mediation modeling.
Latent class analysis.
The basic latent class model is a measurement model in which classes are defined by the pattern of responses to each observed indicator (item), and individuals with similar patterns of responses are considered part of the same latent class (Collins & Lanza, 2009). Latent class proportions indicate how many individuals in the sample are expected to be in each class; the measurement parameters help define/interpret the patterns of responses in latent classes. When the indicators are categorical, the measurement parameters of the latent class model (i.e., response probabilities) are the probabilities of responding to an item, given that one is expected to be in each latent class (membership probabilities closer to 1.0 indicate a strong correspondence between latent class membership and endorsement of the item). When the observed indicators are continuous, the measurement parameters of the latent class model (i.e., latent profile model) are the average level of the continuous indicator within class and the within-class variability in the indicator.
The number of classes was determined by multiple indices: Bayesian Information Criterion (BIC; Schwarz, 1978), the Lo–Mendell–Rubin Likelihood Ratio Test (LRT) p value (Lo et al., 2001), classification precision (defined by entropy, a summary measure of the estimated posterior class probabilities), and interpretability of latent classes. Nylund and colleagues (2007) showed superior performance of the BIC in accurately identifying the correct number of classes most of the time, with a lower BIC indicating a better fitting model. The LRT provides a test of the improvement in fit for each additional estimated class (k), thus testing whether a k class model fits significantly better than a k − 1 class model.
Two separate latent class models were estimated in the current study. First, we replicated Roos and Witkiewitz (2016) in testing a three-class model of the 40 items of the PCQ. Second, we estimated a latent class of drinking outcomes, wherein the indicators were PHDD and DrInC total scores at the 12-month follow-up. Consistent with our prior work (Witkiewitz, 2008; Witkiewitz et al., 2010), we anticipated that a three-class solution for the drinking outcomes would provide the best fit to the data.
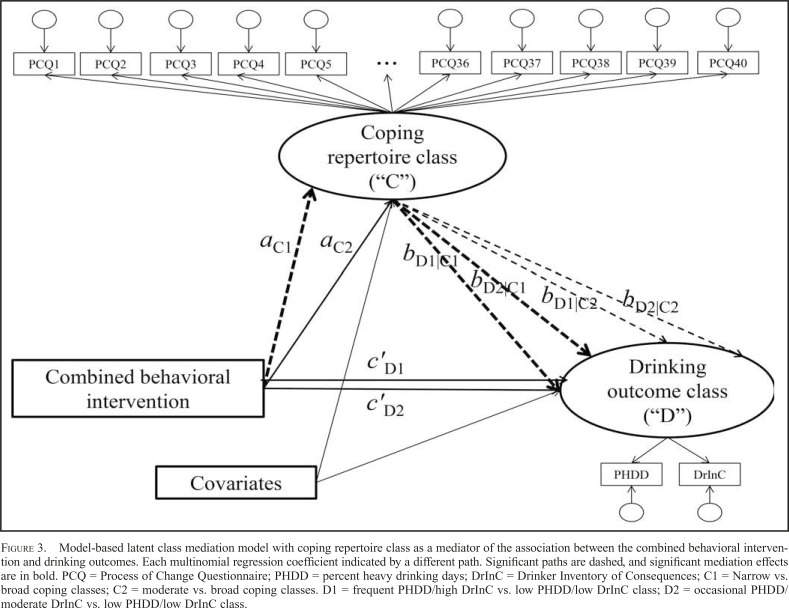
Latent class mediation.
For the purposes of the current study, we specified a latent class mediation model in which both the mediator and outcome variables were latent class variables (Figure 3). Specifically, we used a model-based approach (as shown in Figure 3) that allowed for the estimation of a latent class mediator predicting the latent class drinking outcomes, with both the latent class mediator and latent class outcome regressed on the behavioral intervention, as well as the covariates (see supplementary materials for the Mplus code to estimate this model). Thus, in this context, latent class mediation can be conceptualized as the extent to which receiving a specific treatment predicts membership in one of the mediator latent classes (a path) and the extent to which membership in one of the mediator latent classes predicts membership in one of the outcome latent classes (b path).
Figure 3.
Model-based latent class mediation model with coping repertoire class as a mediator of the association between the combined behavioral intervention and drinking outcomes. Each multinomial regression coefficient indicated by a different path. Significant paths are dashed, and significant mediation effects are in bold. PCQ = Process of Change Questionnaire; PHDD = percent heavy drinking days; DrInC = Drinker Inventory of Consequences; C1 = Narrow vs. broad coping classes; C2 = moderate vs. broad coping classes. D1 = frequent PHDD/high DrInC vs. low PHDD/low DrInC class; D2 = occasional PHDD/moderate DrInC vs. low PHDD/low DrInC class.
The significance of the mediated effect for the latent class mediator was computed using RMediation (Tofighi & MacKinnon, 2011). The RMediation program provides asymmetric 95% confidence intervals (CI) for the mediated effect based on the product of the coefficients approach (MacKinnon, 2008; Tofighi & MacKinnon, 2011). Specifically, the product of the coefficients approach defines the mediated effect as the a path multiplied by the b path of the mediation model. In the current study (as shown in Figure 3), we first estimate multinomial logistic regression because both the mediator and outcome variables are nominal variables with three categories each. A multinomial logistic regression simultaneously fits a number of logistic regression equations (the number of classes minus one), which represent the odds of being in each class versus a reference class. As can be seen in Figure 3, we fit two multinomial logistic regression models for the mediator and outcome variables to estimate a paths and b paths, respectively. To estimate the effect of intervention on coping skills, a multinomial logistic regression uses two logistic regression equations, each modeling the odds of being in a nonreference class relative to a reference class.
To calculate indirect effects, we computed the product of the coefficients obtained from the multinomial logistic regression for the mediator and outcome variable. Specifically, we estimated four products of coefficients: (1) aC1 × bD1|C1, which represented the a path for Class 1 of the mediator (aC1) multiplied by the b path for Class 1 of the outcome regressed on Class 1 of the mediator (bD1|C1); (2) aC1 × bD2|C1, which represented the a path for Class 1 of the mediator (aC1) multiplied by the b path for Class 2 of the outcome regressed on Class 1 of the mediator (bD2|C1); (3) aC2 × bD1|C2, which represented the a path for Class 2 of the mediator (aC2) multiplied by the b path for Class 1 of the outcome regressed on Class 2 of the mediator (bD1|C2); and (4) aC2 × bD2|C2, which represented the a path for Class 2 of the mediator (aC2) was multiplied by the b path for Class 2 of the outcome regressed on Class 2 of the mediator (bD2|C2). Thus, only the b path associations (e.g., bD1|C1 and bD2|C1) that corresponded to the same class of the mediator (e.g., aC1) were included in the product of coefficients testing (i.e., we did not test aC1 × bD1|C2 or aC1 × bD2|C2 or aC2 × bD1|C1 or aC2 × bD2|C1).
Results
Latent class analysis
Coping repertoire.
We identified three latent classes of coping repertoire, as measured by the 40 PCQ items. The LRT was significant for a three-class model (adjusted LRT = 4277.7, p < .01, suggesting rejection of the two-class model in favor of the three-class model) and was not significant for a four-class model (adjusted LRT = 2327.6, p = .812, suggesting that the four-class model did not fit significantly better than a three-class model). The entropy of the three-class model (entropy = .950) was excellent (Nylund et al., 2007). The decrease in BIC was also greatest for the three-class model.
The latent classes could be defined as a narrow repertoire coping class (approximately 22% of the sample), a moderate repertoire coping class (approximately 42% of the sample), and a broad repertoire coping class (approximately 36% of the sample). The response probabilities on the 40 PCQ items for the narrow repertoire coping class indicated the highest probability of endorsing the “never” category for most of the PCQ items. Among those most likely classified in the moderate repertoire coping class, there was a moderate probability of endorsing the “repeatedly” category for most of the PCQ items. The broad repertoire coping class had the highest probability of endorsing the “repeatedly” category for most of the PCQ items. In sum, the broad repertoire coping class was characterized by consistently using a broad range of different skills consistently, whereas the moderate repertoire coping class was characterized by using a moderate range of different skills consistently, and the narrow repertoire coping class was characterized by using a narrow range of different skills infrequently. Receiving the CBI with MM, as compared with MM-only, was associated with significantly reduced odds of expected classification in the narrow repertoire coping class relative to the broad repertoire coping class (odds ratio [OR] = 0.68, p < .01), providing initial support for the a path in the hypothesized mediation model shown in Figure 1. The CBI did not significantly predict membership in the moderate repertoire coping class relative to the broad repertoire coping class (OR = 0.86, p > .05).
Drinking outcomes.
PHDD and scores on the DrInC at the 12-month follow-up were included as continuous indicators of a categorical latent class variable. Means of the drinking outcomes were allowed to vary across classes, and residual variances of each outcome were constrained to equality across classes. We tested two- through five-class models of the two continuous drinking outcomes and found that the LRT was significant for a three-class model (adjusted LRT = 527.27, p = .0046, suggesting rejection of the two-class model in favor of the three-class model) and was not significant for a fourclass model (adjusted LRT = 146.037, p = .323). The five-class model also did not fit significantly better than a four-class model (adjusted LRT = 132.67, p = .497). The entropy of the three-class model (entropy = 0.949) was excellent (Nylund et al., 2007). The decrease in BIC was also greatest for the three-class model. The largest latent class (approximately 63% of the sample, “low PHDD/low DrInC”) was characterized by low PHDD (M = 3.6%) and low DrInC scores (M = 10.97). The second largest latent class (approximately 21%, “occasional PHDD/moderate DrInC”) of the sample was characterized by occasional PHDD (M = 42.7%) and moderately high DrInC scores (M = 33.53). The smallest latent class (approximately 16% of the sample, “frequent PHDD/high DrInC”) was characterized by very frequent PHDD (M = 91.2%) and high DrInC scores (M = 40.51).
Latent class mediation
To test latent class mediation, we used a model-based approach that included the estimation of the latent repertoire coping classes mediating the effect of the behavioral intervention on the drinking latent classes. Sensitivity analyses, provided in supplementary materials, indicated that the class solutions did not substantively change across six alternative models that examined the measurement models for each of the latent classes with and without inclusion of covariates, the CBI variable, and the mediator or outcome latent classes.
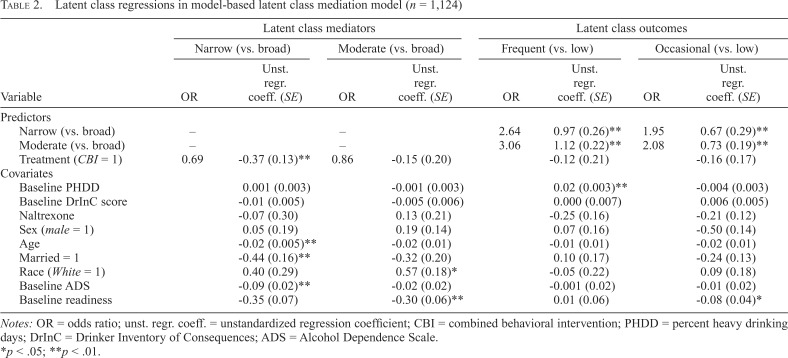
For all models, the broad repertoire coping class was the reference class for the mediator, and the low PHDD/low DrInC latent class was the reference class for the drinking outcomes. Receiving the CBI predicted a significantly lower probability of expected membership in the narrow repertoire coping class, as compared with the broad class (OR = 0.69; B [SE] = -0.372 [0.126], p = .003), providing support for the aC1 path of the mediation model (Table 2). Receiving the CBI was not significantly associated with expected membership in the moderate repertoire coping class (OR = 0.86; B [SE] = -0.15 [0.20], p = .45), as compared with the broad repertoire coping class. Receiving CBI did not predict membership in the moderate repertoire coping class, as compared with the narrow repertoire coping class.
Table 2.
Latent class regressions in model-based latent class mediation model (n = 1,124)
| Latent class mediators |
Latent class outcomes |
|||||||
| Narrow (vs. broad) |
Moderate (vs. broad) |
Frequent (vs. broad) |
Occasional (vs. broad) |
|||||
| Variable | OR | Unst. regr. coeff. (SE) | OR | Unst. regr. coeff. (SE) | OR | Unst. regr. coeff. (SE) | OR | Unst. regr. coeff. (SE) |
| Predictors | ||||||||
| Narrow (vs. broad) | – | – | 2.64 | 0.97 (0.26)** | 1.95 | 0.67 (0.29)** | ||
| Moderate (vs. broad) | – | – | 3.06 | 1.12 (0.22)** | 2.08 | 0.73 (0.19)** | ||
| Treatment (CBI = 1) | 0.69 | -0.37 (0.13)** | 0.86 | -0.15 (0.20) | -0.12 (0.21) | -0.16 (0.17) | ||
| Covariates | ||||||||
| Baseline PHDD | 0.001 (0.003) | -0.001 (0.003) | 0.02 (0.003)** | -0.004 (0.003) | ||||
| Baseline DrInC score | -0.01 (0.005) | -0.005 (0.006) | 0.000 (0.007) | 0.006 (0.005) | ||||
| Naltrexone | -0.07 (0.30) | 0.13 (0.21) | -0.25 (0.16) | -0.21 (0.12) | ||||
| Sex (male = 1) | 0.05 (0.19) | 0.19 (0.14) | 0.07 (0.16) | -0.50 (0.14) | ||||
| Age | -0.02 (0.005)** | -0.02 (0.01) | -0.01 (0.01) | -0.02 (0.01) | ||||
| Married = 1 | -0.44 (0.16)** | -0.32 (0.20) | 0.10 (0.17) | -0.24 (0.13) | ||||
| Race (White = 1) | 0.40 (0.29) | 0.57 (0.18)* | -0.05 (0.22) | 0.09 (0.18) | ||||
| Baseline ADS | -0.09 (0.02)** | -0.02 (0.02) | -0.001 (0.02) | -0.01 (0.02) | ||||
| Baseline readiness | -0.35 (0.07) | -0.30 (0.06)** | 0.01 (0.06) | -0.08 (0.04)* | ||||
Notes: OR = odds ratio; unst. regr. coeff. = unstandardized regression coefficient; CBI = combined behavioral intervention; PHDD = percent heavy drinking days; DrInC = Drinker Inventory of Consequences; ADS = Alcohol Dependence Scale.
p < .05;
p < .01.
Expected membership in the narrow repertoire coping latent class, as compared with the broad repertoire coping class, significantly predicted a greater likelihood of being in both the frequent PHDD/high DrInC class (OR = 2.64; B [SE] = 0.97 [0.26], p < .001) and the occasional PHDD/moderate DrInC class (OR = 1.95; B [SE] = 0.67 [0.29], p = .02), as compared with the low PHDD/low DrInC, providing support for the bD1|C1 path and the bD2|C1 path of the mediation model, respectively. Similarly, expected membership in the moderate repertoire coping latent class, as compared to the broad repertoire coping class, significantly predicted a greater likelihood of being in either the frequent PHDD/high DrInC class (OR = 3.06; B [SE] = 1.12 [0.22], p < .001) or the occasional PHDD/moderate DrInC class (OR = 2.08; B [SE] = 0.73 [0.19], p < .001), as compared to the low PHDD/low DrInC, providing support for the bD1|C2 path and the bD2|C2 path of the mediation model, respectively.
Using the product of coefficients approach within RMediation (Tofighi & MacKinnon, 2011) to calculate the significance of the indirect effect, we found that the effect of CBI on being in the frequent PHDD/high DrInC class in comparison to the low PHDD/low DrInC class was mediated by being in the narrow repertoire coping class versus the broad repertoire coping class (aC1 × bD1|C1 indirect effect = -0.361, 95% CI [-0.714, -0.095]). The effect of CBI on being in the occasional PHDD/moderate DrInC class as opposed to the low PHDD/low DrInC class was mediated by being in the narrow repertoire coping class, as compared to the broad repertoire coping class (aC1 × bD2|C1 indirect effect = -0.249, 95% CI [-0.572, -0.024]). The mediating effect of the moderate repertoire coping class was not significant for either drinking outcome latent classes (aC2 × bD1|C2 p > .05 and aC2 × bD2|C2 p > .05).
Discussion
The current study examined coping repertoire as a mediator of the association between receiving the CBI and drinking outcomes 12 months following treatment in the COMBINE Study. Consistent with Roos and Witkiewitz (2016), we found that receiving CBI was associated with a broader repertoire of coping skills following treatment, which in turn was associated with significant improvements in drinking outcomes. The current study extends these findings by using latent class mediation to demonstrate that broad coping repertoire statistically mediated the association between CBI and drinking outcomes. Hence, the current study is one of very few studies (Kiluk et al., 2010; Roos et al., 2017) to find support for coping as a significant mediator in predicting alcohol and substance use outcomes following a behavioral intervention that included coping skills training. We hypothesized that coping has not traditionally been supported as mediator in AUD treatment research (Morgenstern & Longabaugh, 2000) because of significant heterogeneity in coping skills acquisition during the course of treatment.
The current study findings demonstrate that developing a broad repertoire of coping skills may be a key MOBC in behavioral interventions for AUD that include coping skills training. As noted by Roos and Witkiewitz (2016), there were no qualitative differences between classes based on using particular types of skills. Rather, the broadness of the repertoire (i.e., the number of different skills that were used consistently) appeared to be the key factor that distinguished the classes. Future research on repertoires of coping would help clarify the relative importance of facilitating clients in developing a broad repertoire of coping skills versus teaching particular types of skills that are uniformly highly effective across clients.
To our knowledge, the current study is also the first application of latent class mediation analyses to examine MOBCs in AUD treatment. One of the major challenges is that because latent classes are model based, the latent classes for the mediator are themselves determined in part by the outcomes, which is inconsistent with the assumptions of the mediation model. Sensitivity analyses (shown in supplementary materials) indicated that latent classes of the mediator and latent classes of the outcome did not change considerably when tested together in the full model, providing some support for the assumption of the mediator being defined independently from the outcome in the final latent class mediation model. Additional analyses (not shown) were also conducted using an inclusive classify–analyze two-step approach (Bray et al., 2015), and the substantive conclusions did not change.
Limitations
Numerous limitations of the current study need to be acknowledged. First, the primary limitation of the current study was that the mediator was only assessed at the end of treatment, and thus we cannot estimate the degree to which coping repertoire changed during treatment. We were limited to the available data in the COMBINE Study, and the COMBINE Study did not administer the PCQ at the baseline assessment. To fully assess coping as an MOBC, we would need to establish that the differences observed were caused by random assignment to the behavioral intervention condition and not by pre-existing differences in coping repertoire.
Second, a limitation of the analytic approach is that latent class models are probabilistic and therefore always have some degree of misclassification. The model-based approach we used in the current study incorporated the misclassification into the model estimates, and model entropy was quite high across the coping repertoire latent classes and the drinking outcomes latent classes, which does provide some confidence in the final class solutions.
Future directions and conclusions
To expand the study of MOBCs in AUD treatment and inform the development of more effective treatments for AUD, more work needs to be done to examine the possibility that treatment effects may differ for individuals or subsets of individuals (Kranzler & McKay, 2012; McKay, 2013). Recent work in causal mediation could also be useful for identifying how individuals respond to intervention and change over time (MacKinnon, 2008; MacKinnon & Pirlott, 2015; Wang et al., 2014).
The field has benefitted from nearly 20 years examining mediators of AUD treatment effectiveness (Magill & Longabaugh, 2013), yet the effect sizes for behavioral interventions have not notably improved across time (e.g., Magill & Ray, 2009). We contend that further empirical work on the heterogeneity in MOBCs is needed to clarify which treatments are most effective for which individuals. Through the examination of heterogeneity in mediators and outcomes, we might gain a better sense of the specific components of treatment that are most effective for which individuals and further refine treatment to be maximally effective.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism Grants R01 AA022328 and R01AA025539. The content is solely the responsibility of the authors and does not necessarily reflect the views of the National Institutes of Health.
References
- American Psychiatric Association. 4th ed. Washington, DC: Author; 1994. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- Anton R. F., O’Malley S. S., Ciraulo D. A., Cisler R. A., Couper D., Donovan D. M., Zweben A. the COMBINE Study Research Group. Combined pharmacotherapies and behavioral interventions for alcohol dependence: The COMBINE Study: A randomized controlled trial. JAMA. 2006;295:2003–2017. doi: 10.1001/jama.295.17.2003. doi:10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- Bray B. C., Lanza S. T., Tan X. Eliminating bias in classify analyze approaches for latent class analysis. Structural Equation Modeling. 2015;22:1–11. doi: 10.1080/10705511.2014.935265. doi:10.1080/10705511.2014.935265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins L. M., Lanza S. T. New York, NY: Wiley; 2009. Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. [Google Scholar]
- COMBINE Study Research Group. Testing combined pharmacotherapies and behavioral interventions in alcohol dependence: Rationale and methods. Alcoholism. Clinical and Experimental Research. 2003;27:1107–1122. doi: 10.1097/00000374-200307000-00011. doi:10.1111/j.1530-0277.2003.tb02873.x. [DOI] [PubMed] [Google Scholar]
- DiClemente C. C., Carroll K. M., Connors G. J., Kadden R. M. Process assessment in treatment matching research. Journal of Studies on Alcohol, Supplement. 1994;12:156–162. doi: 10.15288/jsas.1994.s12.156. doi:10.15288/jsas.1994.s12.156. [DOI] [PubMed] [Google Scholar]
- Gueorguieva R., Wu R., Donovan D., Rounsaville B. J., Couper D., Krystal J. H., O’Malley S. S. Naltrexone and combined behavioral intervention effects on trajectories of drinking in the COMBINE Study. Drug and Alcohol Dependence. 2010;107:221–229. doi: 10.1016/j.drugalcdep.2009.10.017. doi:10.1016/j.drugalcdep.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadden R. M., Carroll K. M., Donovan D. M., Cooney N. L., Monti P. M., Abrams D., Hester R. K. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. Project MATCH Monograph Series, Volume 3. Cognitive-Behavioral Coping Skills Therapy Manual. [Google Scholar]
- Kadden R. M., Cooney N. L., Getter H., Litt M. D. Matching alcoholics to coping skills or interactional therapies: Posttreatment results. Journal of Consulting and Clinical Psychology. 1989;57:698–704. doi: 10.1037//0022-006x.57.6.698. doi:10.1037/0022-006X.57.6.698. [DOI] [PubMed] [Google Scholar]
- Kazdin A. E. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. doi:10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kiluk B. D., Nich C., Babuscio T., Carroll K. M. Quality versus quantity: Acquisition of coping skills following computerized cognitive-behavioral therapy for substance use disorders. Addiction. 2010;105:2120–2127. doi: 10.1111/j.1360-0443.2010.03076.x. doi:10.1111/j.1360-0443.2010.03076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kranzler H. R., McKay J. R. Personalized treatment of alcohol dependence. Current Psychiatry Reports. 2012;14:486–493. doi: 10.1007/s11920-012-0296-5. doi:10.1007/s11920-012-0296-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt M. D., Kadden R. M., Cooney N. L., Kabela E. Coping skills and treatment outcomes in cognitive-behavioral and interactional group therapy for alcoholism. Journal of Consulting and Clinical Psychology. 2003;71:118–128. doi: 10.1037//0022-006x.71.1.118. doi:10.1037/0022-006X.71.1.118. [DOI] [PubMed] [Google Scholar]
- Lo Y., Mendell N. R., Rubin D. B. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. doi:10.1093/biomet/88.3.767. [Google Scholar]
- LoCastro J. S., Youngblood M., Cisler R. A., Mattson M. E., Zweben A., Anton R. F., Donovan D. M. Alcohol treatment effects on secondary nondrinking outcomes and quality of life: The COMBINE Study. Journal of Studies on Alcohol and Drugs. 2009;70:186–196. doi: 10.15288/jsad.2009.70.186. doi:10.15288/jsad.2009.70.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R., Donovan D. M., Karno M. P., McCrady B. S., Morgenstern J., Tonigan J. S. Active ingredients: How and why evidence-based alcohol behavioral treatment interventions work. Alcoholism: Clinical and Experimental Research. 2005;29:235–247. doi: 10.1097/01.alc.0000153541.78005.1f. doi:10.1097/01.ALC.0000153541.78005.1F. [DOI] [PubMed] [Google Scholar]
- MacKinnon D. P. New York, NY: Taylor & Francis Group; 2008. Introduction to statistical mediation analysis. [Google Scholar]
- MacKinnon D. P., Pirlott A. G. Statistical approaches for enhancing causal interpretation of the M to Y relation in mediation analysis. Personality and Social Psychology Review. 2015;19:30–43. doi: 10.1177/1088868314542878. doi:10.1177/1088868314542878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M., Longabaugh R. Efficacy combined with specified ingredients: A new direction for empirically supported addiction treatment. Addiction. 2013;108:874–881. doi: 10.1111/add.12013. doi:10.1111/add.12013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M., Ray L. A. Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials. Journal of Studies on Alcohol and Drugs. 2009;70:516–527. doi: 10.15288/jsad.2009.70.516. doi:10.15288/jsad.2009.70.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt G. A., Donovan D. M. 2nd ed. New York, NY: Guilford Press; 2005. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. [Google Scholar]
- McConnaughy E. A., Prochaska J. O., Velicer W. F. Stages of change in psychotherapy: Measurement and sample profiles. Psychotherapy. 1983;20:368–375. doi:10.1037/h0090198. [Google Scholar]
- McKay J. R. Commentary on Magill & Longabaugh (2013): Specifying the active ingredients in evidence-based treatments—Setting the bar too high? Addiction. 2013;108:882–883. doi: 10.1111/add.12136. discussion 883–884. doi:10.1111/add.12136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W. R. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1996. Form 90: A structured assessment interview for drinking and related behaviors. [Google Scholar]
- Miller W. R. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2004. Combined behavioral intervention manual: A clinical research guide for therapists treating people with alcohol abuse and dependence. [Google Scholar]
- Miller W. R., Moyers T. B., Arciniega L., Ernst D., Forcehimes A. Training, supervision and quality monitoring of the COMBINE Study behavioral interventions. Journal of Studies on Alcohol, Supplement. 2005;15:188–195. doi: 10.15288/jsas.2005.s15.188. doi:10.15288/jsas.2005.s15.188. [DOI] [PubMed] [Google Scholar]
- Miller W. R., Tonigan J. S., Longabaugh R. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. The Drinker Inventory of Consequences (DrInC) [Google Scholar]
- Morgenstern J., Longabaugh R. Cognitive-behavioral treatment for alcohol dependence: A review of evidence for its hypothesized mechanisms of action. Addiction. 2000;95:1475–1490. doi: 10.1046/j.1360-0443.2000.951014753.x. doi:10.1046/j.1360-0443.2000.951014753.x. [DOI] [PubMed] [Google Scholar]
- Muthén B. O., Asparouhov T. Causal effects in mediation modeling: An introduction with applications to latent variables. Structural Equation Modeling: A Multidisciplinary Journal. 2015;22:12–23. doi:10.10 80/10705511.2014.935843. [Google Scholar]
- Muthén L. K., Muthén B. O. Los Angeles, CA: Authors; 2012. Mplus user’s guide (Version 7) [Google Scholar]
- Nylund K. L., Asparouhov T., Muthén B. O. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14:535–569. doi:10.1080/10705510701575396. [Google Scholar]
- Prochaska J. O., Velicer W. F., DiClemente C. C., Fava J. Measuring processes of change: Applications to the cessation of smoking. Journal of Consulting and Clinical Psychology. 1988;56:520–528. doi: 10.1037//0022-006x.56.4.520. doi:10.1037/0022-006X.56.4.520. [DOI] [PubMed] [Google Scholar]
- Roos C. R., Maisto S. A., Witkiewitz K. Coping mediates the effects of cognitive-behavioral therapy for alcohol use disorder among out-patient clients in Project MATCH when dependence severity is high. Addiction. 2017;112:1547–1557. doi: 10.1111/add.13841. doi:10.1111/add.13841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos C. R., Witkiewitz K. Adding tools to the toolbox: The role of coping repertoire in alcohol treatment. Journal of Consulting and Clinical Psychology. 2016;84:599–611. doi: 10.1037/ccp0000102. doi:10.1037/ccp0000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer J. L., Graham J. W. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. doi:10.1037/1082-989X. 7.2.147. [PubMed] [Google Scholar]
- Schwarz G. E. Estimating the dimension of a model. Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Skinner H. A., Horn J. L. Toronto, Ontario: Addiction Research Foundation; 1984. Alcohol Dependence Scale (ADS) user’s guide. [Google Scholar]
- Tofighi D., MacKinnon D. P. RMediation: An R package for mediation analysis confidence intervals. Behavior Research Methods. 2011;43:692–700. doi: 10.3758/s13428-011-0076-x. doi:10.3758/s13428-011-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele T. J. Mediation analysis: A practitioner’s guide. Annual Review of Public Health. 2016;37:17–32. doi: 10.1146/annurev-publhealth-032315-021402. doi:10.1146/annurevpublhealth-032315-021402. [DOI] [PubMed] [Google Scholar]
- Wang C.-P., Jo B., Brown C. H. Causal inference in longitudinal comparative effectiveness studies with repeated measures of a continuous intermediate variable. Statistics in Medicine. 2014;33:3509–3527. doi: 10.1002/sim.6120. doi:10.1002/sim.6120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K. Lapses following alcohol treatment: Modeling the falls from the wagon. Journal of Studies on Alcohol and Drugs. 2008;69:594–604. doi: 10.15288/jsad.2008.69.594. doi:10.15288/jsad.2008.69.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K., Falk D. E., Kranzler H. R., Litten R. Z., Hallgren K. A., O’Malley S. S., Anton R. F the Alcohol Clinical Trials Initiative (ACTIVE) Workgroup. Methods to analyze treatment effects in the presence of missing data for a continuous heavy drinking outcome measure when participants drop out from treatment in alcohol clinical trials. Alcoholism: Clinical and Experimental Research. 2014;38:2826–2834. doi: 10.1111/acer.12543. doi:10.1111/acer.12543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K., Maisto S. A., Donovan D. M. A comparison of methods for estimating change in drinking following alcohol treatment. Alcoholism: Clinical and Experimental Research. 2010;34:2116–2125. doi: 10.1111/j.1530-0277.2010.01308.x. doi:10.1111/j.1530-0277.2010.01308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan K.-H., Bentler P. M. Finite normal mixture SEM analysis by fitting multiple conventional SEM models. Sociological Methodology. 2010;40:191–245. doi: 10.1111/j.1467-9531.2010.01224.x. doi:10.1111/j.1467-9531.2010.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]