Abstract
Medial patellofemoral ligament reconstruction is an essential component of surgical treatment for recurrent dislocation of the patella. Various techniques have been described, most of which potentially increase the risk of patellar fracture. We present a new technique for anatomic medial patellofemoral ligament reconstruction without using suture anchors or patellar tunnels, therefore, eliminating the risk of iatrogenic patellar fracture and making a revision procedure easier in case of failure.
Lateral dislocation of the patella is fairly common in the athletic population.1 The incidence of lateral patellar dislocation is 5.8 per 100,000, and it most commonly occurs in females between the age of 10 and 17.1 Osseous and soft tissue restraints maintain patellar stability and normal patellar tracking throughout the range of motion. During the first 30° of flexion, the patella does not fully engage within the trochlea, which decreases the contribution of osseous stability, and the medial patellofemoral ligament (MPFL) becomes the primary restraint to lateral patellar translation. A lateral patellar dislocation is essentially pathognomonic for disruption of the MPFL.2 Reconstruction of the torn ligament is indicated in recurrent instability, whereas surgical reconstruction in first time dislocators is controversial; some surgeons are inclined to surgically reconstruct the MPFL after a single patellar dislocation in athletes.3 Numerous surgical techniques have been described for MPFL reconstruction with no consensus, because a single technique has not yet shown superiority in the literature. Most of the techniques described include passing the graft through patellar tunnels, which potentially increases the risk of iatrogenic fracture of the patella. We describe a simple technique for MPFL reconstruction that is effective, without the need for patellar tunnels, therefore decreasing the risk of iatrogenic patellar fracture reported with other techniques.
Surgical Technique
Details of the surgical procedure are shown in Video 1.
Patient Positioning and Graft Preparation
The patient is placed in a supine position, and a tourniquet is applied to the upper thigh. A semitendinosus allograft with 6.5 mm diameter and approximately 250 mm length is prepared, and the free ends are controlled with a running locking stitch that uses a strong number 2 nonabsorbable suture material (Ethibond; Ethicon, Somerville, NJ). The graft is pretensioned at 20 pounds of pressure.
Examination Under Anesthesia and Knee Arthroscopy
The procedure begins with examination under anesthesia to confirm lateral patellar instability. A sterile skin marker under fluoroscopic guiding is used to draw out bony anatomic landmarks, specifically over the superior aspect of the patella and over the adductor tubercle on the medial side of the knee. Knee arthroscopy is routinely performed before MPFL reconstruction to assess articular cartilage and patellar tracking.
Lateral Retinacular Release and Preparation of the Patellar Attachment Site for the MPFL
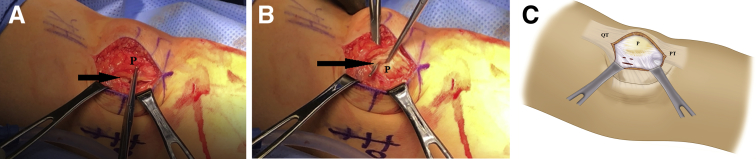
The open surgical procedure begins with a longitudinal midline incision that is approximately 3 cm in length overlying the patella, followed by subcutaneous dissection to expose retinacula on both sides. A longitudinal 5-cm incision is made 1 cm off the lateral border of the patella to release the lateral retinaculum. We routinely perform lateral release because we believe that it is necessary to allow a centered glide of the patella. The wound is then retracted medially to expose the medial retinaculum where a longitudinal 2-cm incision is made 1 cm off the medial border and superior to the equator of the patella. The junction between the upper third and lower two-thirds of the medial border of the patella is then identified, and 2 stab incisions are made superior and inferior to that point, just medial to the medial border of the patella, using a No. 11 blade (Fig 1).
Fig 1.
Incisions along the medial border of the patella (left knee). (A) A 2-cm longitudinal incision (arrow) 1 cm off the medial border of the patella (P) and superior to the equator. (B) A superior stab incision (arrow) along the medial border of the patella (P) above the junction between the upper and middle thirds. (C) An illustration showing the locations of the 3 incisions in the medial retinaculum. (PT, patellar tendon; QT, quadriceps tendon.)
Graft Attachment and Tubularization
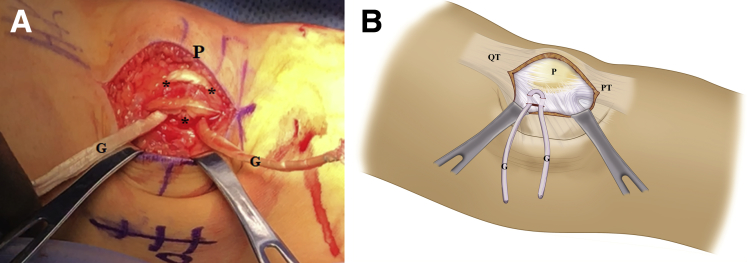
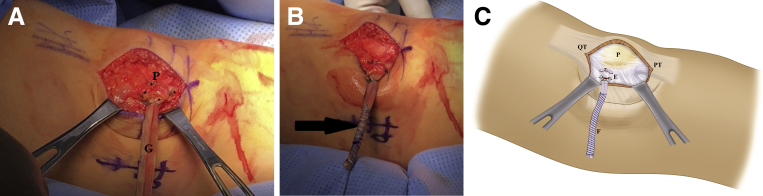
The previously prepared graft is then brought to the front table, placed through the initial 2-cm incision, then through the 2 stab portals, and pulled until the ends are brought even (Fig 2). Ethibond single stitches are used to attach the graft to the medial border of the patella, and 2-0 FiberWire (Arthrex, Naples, FL) is used to tubularize the whipstitched ends of the graft to prevent rupture of the graft inside the femoral tunnel. The 2 ends of the graft are pulled together toward the mark previously made on the skin over the adductor tubercle. The graft is cut off leaving at least 3 cm of the graft beyond the adductor tubercle so that enough length is available to go into the femoral tunnel (Fig 3).
Fig 2.
Passing the semitendinosus graft through the retinaculum (left knee). (A) The graft (G) is passed through the 3 incisions (*) along the medial border of the patella (P), and then pulled until both ends are even. (B) An illustration showing how the graft is passed through the medial retinacular incisions. (PT, patellar tendon; QT, quadriceps tendon.)
Fig 3.
Suturing the graft to the retinaculum and tubularizing the free ends (left knee). (A) Suturing the graft (G) to the medial border of the patella (P) using nonabsorbable Ethibond sutures (*). (B) Graft tubularized using 2-0 FiberWire (black arrow) to prevent its rupture inside the femoral tunnel. (C) An illustration showing suturing the graft to the medial border of the patella using Ethibond sutures (E) and tubularizing the graft using FiberWire (F). (PT, patellar tendon; QT, quadriceps tendon.)
Medial Approach and Locating the Femoral Attachment Site
The knee is then flexed to approximately 20° and an incision is made at the area that has been marked out over the adductor tubercle and dissected posterior to the vastus medialis and down to the adductor tubercle itself. Retractors are used to better visualize the adductor tubercle. A Beath pin is inserted at a point just distal to the adductor tubercle and used to create a femoral tunnel from medial to lateral. It has been shown that the anatomic femoral attachment site for the MPFL is 10 mm distal to the apex of the adductor tubercle.4 Fluoroscopy can be used to confirm the accurate placement of the Beath pin at the anatomic femoral attachment site of the MPFL, as described by Schöttle et al.,5 1.3 mm anterior to the posterior cortex extension, 2.5 mm distal to the posterior origin of the medial femoral condyle, and just proximal to the level of the posterior-most point of the Blumensaat line (Fig 4).
Fig 4.
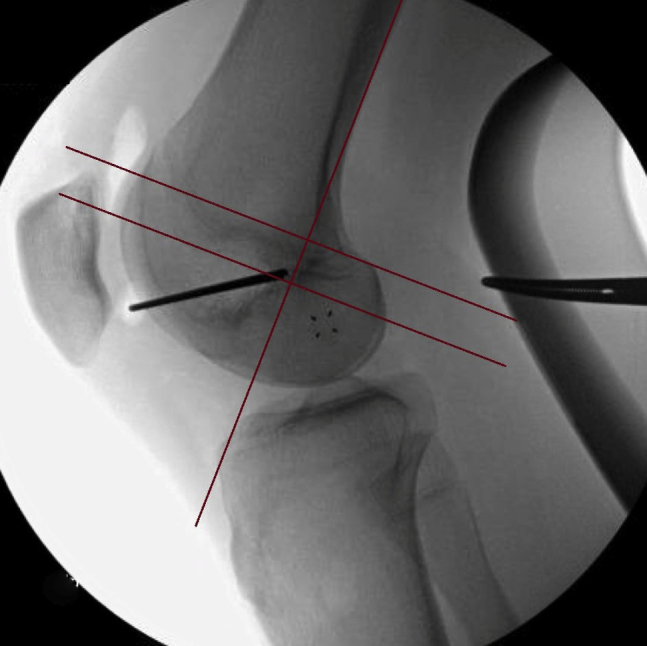
Locating the Schöttle point under fluoroscopy, 1.3 mm anterior to the posterior cortex extension, 2.5 mm distal to the posterior origin of the medial femoral condyle and just proximal to the level of the posterior-most point of the Blumensaat line.
Drilling the Femoral Tunnel and Passing the Graft
The femoral tunnel is reamed with a 7-mm-diameter reamer and a depth of approximately 50 mm. The graft is passed subcutaneously to the medial wound, and the ends of the suture are placed through the Beath pin. The Beath pin is pulled from the lateral aspect of the knee bringing the graft inside the tunnel and then tensioned. Accurate femoral tunnel placement and optimum graft tensioning are crucial for restoring the normal patellofemoral joint kinematics and contact stresses.6
Tension Adjustment and Fixation to the Anatomic Femoral Attachment Site
In acute traumatic dislocations, the tension is adjusted so that the patella can be displaced laterally between 1 and 2 quadrants of the patellar width. In patients with hyperlaxity, we tighten the patella a little more so that the patella can be displaced only 10% to 20% of its width. In general, care is taken not to excessively tighten the patella. An interference screw (Smith & Nephew, Andover, MA) is inserted to fix the graft in the femoral tunnel at 30° of flexion. Before routine wound closure, a knee examination is performed again to confirm optimum tension. Femoral fixation can be revised in case tension needs to be readjusted. Pearls and pitfalls are summarized in Table 1.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Longitudinal incision in the medial retinaculum at least 1 cm off the medial border to leave adequate soft tissue to attach the graft to | Small distance between any 2 of the 3 incisions in the medial retinaculum can lead to failure |
| Two stab incisions along the medial border of the patella above the equator to replicate the native anatomy | Overtightening of the graft can lead to pain, arthrosis, and decreased range of motion |
| The graft is tubularized using 2-0 FiberWire to prevent its rupture inside the femoral tunnel | Inaccurate placement of the femoral tunnel can lead to postoperative stiffness or graft rupture |
NOTE. Tension adjustment is performed in 30° of knee flexion. A total of 25% to 50% lateral patellar displacement is allowed in acute traumatic dislocations and 10% to 20% in patients with hyperlaxity.
Rehabilitation
Postoperatively, the knee is kept in a brace for 6 weeks while allowing passive and active assisted range of motion and weight-bearing as tolerated. The brace is initially locked in extension, and then flexion is gradually permitted. Strengthening exercises begin at 8 weeks. Patients return to contact sports at 6 months postoperatively.
Discussion
Multiple techniques have been described for MPFL reconstruction. Femoral fixation of the graft is usually performed using an interference screw, whereas fixation to the patella can be achieved by bony or soft tissue procedures. Bony procedures increase the risk of patellar fracture, and violation of the articular surface can occur. Soft tissue procedures generally achieve favorable results using suture anchors or nonabsorbable sutures. Drez et al.7 used nonabsorbable sutures, in addition to a suture anchor, to fix the graft to the patella. Schöttle et al.8 performed a bony groove into the patella and 2 suture anchors into that groove. Sillanpää et al.9 used the adductor magnus tendon with its distal insertion still attached to reconstruct the MPFL. They fixed the proximal cut end to the periosteum of the medial border of the patella with nonabsorbable sutures. Steensen et al.10 used a quadriceps tendon graft, leaving its patellar insertion intact, to reconstruct the MPFL.
The main advantage of our technique is that it is a simple, anatomic, and effective procedure with minimal cost and complications (Table 2). We attach the graft at the anatomic patellar attachment site without doing tunnels or inserting anchors in the patella. Passing the graft through 2 separate stab incisions in the soft tissue replicates the broad attachment of the native MPFL on the patella, whereas tendon transfer procedures described to the patella9 or to the femur10 are nonanatomic reconstruction procedures. The fact that we do not pass the graft through patellar tunnels nor insert suture anchors has several advantages; first, this provides more length of the graft available for MPFL reconstruction, which is important in the cases in which the graft is not long enough. Second, it eliminates the risk of patellar fracture and allows the use of allografts with larger diameters without worrying about drilling wide tunnels in the patella. Third, it makes a revision procedure much easier in case of failure. In patients who have had several surgeries, multiple patellar tunnels or the presence of suture anchors implanted in the patella adds to the risk of patellar fracture and makes a revision procedure more challenging.
Table 2.
Advantages and Disadvantage
| Advantages | Disadvantage |
|---|---|
| Simple technique | Biomechanically weaker than bony fixation |
| Anatomic | |
| No tunnels or anchors | |
| Graft length not wasted in tunnels | |
| No risk of patellar fracture | |
| Large-diameter grafts can be safely used | |
| Revision is easier in case of failure |
A potential limitation of this technique might be a decreased load to failure of the patellar attachment compared with bony fixation with tunnels or suture anchors. Suture fixation has been proven to be biomechanically weaker than bony fixation.11 However, the biomechanical difference does not imply a clinical difference. Sillanpää et al.9 reported excellent clinical results with suture fixation. A recent randomized controlled trial comparing soft tissue and bony fixation showed similar clinical outcomes in both.12
In conclusion, an alternative technique for MPFL reconstruction is fixing a semitendinosus allograft to the soft tissue along the medial border of the patella using nonabsorbable sutures, and to the anatomic attachment site on the femur using an interference screw. We believe that this technique is simple, relatively cheap, and effective. It also eliminates the risk of iatrogenic patellar fracture and makes a revision procedure easier in case of failure.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is placed in the supine position. This is the patient's left knee. The procedure begins with examination under anesthesia to confirm lateral patellar instability. A longitudinal midline incision is made over the patella followed by subcutaneous undermining both laterally and medially. We routinely perform lateral retinacular release as we believe that it is necessary to allow a centered glide of the patella. The wound is retracted medially, and a longitudinal 2-cm incision is made in the retinaculum 1 cm medial to the medial border and superior to the equator of the patella. Two stab incisions are made just medial to the patella above and below the junction between its upper and middle thirds. The semitendinosus allograft is passed through the incisions. We then use nonabsorbable sutures to attach the graft to the medial border of the patella. 2-0 FiberWire is used to tubularize the graft to prevent its rupture inside the femoral tunnel. The graft is cut off leaving at least 3 cm available to go into the femoral tunnel. A medial incision is made over the adductor tubercle followed by dissection below the vastus medialis oblique. A Beath pin is inserted at the anatomic femoral attachment site of the native medial patellofemoral ligament followed by a 7-mm-diameter reamer. The graft is passed to the medial incision and brought into the femoral tunnel using the Beath pin. An interference screw is inserted to fix the graft in the femoral tunnel at 30° of knee flexion. Care is taken not to excessively tighten the patella.
References
- 1.Fithian D.C., Paxton E.W., Stone M.L. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114–1121. doi: 10.1177/0363546503260788. [DOI] [PubMed] [Google Scholar]
- 2.Amis A.A., Firer P., Mountney J., Senavongse W., Thomas N.P. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10:215–220. doi: 10.1016/s0968-0160(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 3.Hinton R.Y., Sharma K.M. Acute and recurrent patellar instability in the young athlete. Orthop Clin North Am. 2003;34:385–396. doi: 10.1016/s0030-5898(03)00033-6. [DOI] [PubMed] [Google Scholar]
- 4.Fujino K., Tajima G., Yan J. Morphology of the femoral insertion site of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2015;23:998–1003. doi: 10.1007/s00167-013-2797-0. [DOI] [PubMed] [Google Scholar]
- 5.Schöttle P.B., Schmeling A., Rosenstiel N., Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 6.Stephen J.M., Kittl C., Williams A. Effect of medial patellofemoral ligament reconstruction method on patellofemoral contact pressures and kinematics. Am J Sports Med. 2016;44:1186–1194. doi: 10.1177/0363546516631736. [DOI] [PubMed] [Google Scholar]
- 7.Drez D., Edwards T.B., Williams C.S. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17:298–306. doi: 10.1053/jars.2001.21490. [DOI] [PubMed] [Google Scholar]
- 8.Schöttle P.B., Fucentese S.F., Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc. 2005;13:516–521. doi: 10.1007/s00167-005-0659-0. [DOI] [PubMed] [Google Scholar]
- 9.Sillanpää P., Mattila V.M., Visuri T., Mäenpää H., Pihlajamäki H. Ligament reconstruction versus distal realignment for patellar dislocation. Clin Orthop Relat Res. 2008;466:1475–1484. doi: 10.1007/s11999-008-0207-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steensen R.N., Dopirak R.M., Maurus P.B. A simple technique for reconstruction of the medial patellofemoral ligament using a quadriceps tendon graft. Arthroscopy. 2005;21:365–370. doi: 10.1016/j.arthro.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Mountney J., Senavongse W., Amis A.A., Thomas N.P. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005;87:36–40. [PubMed] [Google Scholar]
- 12.Lind M., Faunoe P., Sørensen O.G., Mygind-Klavsen B., Miller L., Nielsen T.G. Comparison of soft tissue and bone graft fixation for reconstruction of the medial patellofemoral ligament. A randomized controlled trial. Arthroscopy. 2017;33:e172. doi: 10.1016/j.arthro.2018.11.051. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed in the supine position. This is the patient's left knee. The procedure begins with examination under anesthesia to confirm lateral patellar instability. A longitudinal midline incision is made over the patella followed by subcutaneous undermining both laterally and medially. We routinely perform lateral retinacular release as we believe that it is necessary to allow a centered glide of the patella. The wound is retracted medially, and a longitudinal 2-cm incision is made in the retinaculum 1 cm medial to the medial border and superior to the equator of the patella. Two stab incisions are made just medial to the patella above and below the junction between its upper and middle thirds. The semitendinosus allograft is passed through the incisions. We then use nonabsorbable sutures to attach the graft to the medial border of the patella. 2-0 FiberWire is used to tubularize the graft to prevent its rupture inside the femoral tunnel. The graft is cut off leaving at least 3 cm available to go into the femoral tunnel. A medial incision is made over the adductor tubercle followed by dissection below the vastus medialis oblique. A Beath pin is inserted at the anatomic femoral attachment site of the native medial patellofemoral ligament followed by a 7-mm-diameter reamer. The graft is passed to the medial incision and brought into the femoral tunnel using the Beath pin. An interference screw is inserted to fix the graft in the femoral tunnel at 30° of knee flexion. Care is taken not to excessively tighten the patella.