Abstract
Knee extension deficit is frequently observed after anterior cruciate ligament reconstruction or rupture and other acute knee injuries. Loss of terminal extension often occurs because of hamstring contracture and quadriceps inactivation rather than mechanical intra-articular pathology. Failure to regain full extension in the first few weeks after anterior cruciate ligament reconstruction is a recognized risk factor for adverse long-term outcomes, and therefore, it is important to try to address it. In this Technical Note, a simple, rapid, and effective technique to help regain full knee extension and abolish quadriceps activation failure is described.
A patient who presents with an extension deficit after an acute knee injury or surgery can be challenging to manage. The medical provider who first evaluates the patient must differentiate between 2 separate situations: In the “locked knee,” a displaced intra-articular structure mechanically prevents full extension, whereas the “pseudo-locked knee” occurs without the presence of any true mechanical block to motion.1 Although frequently observed in clinical practice, the pathophysiology of the latter scenario had remained unclear for decades. In 1986 Allum and Jones1 observed that spasms of the hamstrings were related to an extension deficit after knee injury, but no explanation was given. More recently, there has been increased interest in the subject, and multiple authors have postulated that the extension deficit, also observed after knee surgery, may be due to a process called “arthrogenic muscle inhibition” (AMI).2, 3 AMI is believed to be responsible for the failure of quadriceps activation that is associated with hamstring contracture.
In this Technical Note, we describe a set of exercises that reliably counter the physiological pathways of AMI and quickly regain full active and passive knee extension (Table 1). No special equipment is necessary. Video 1 shows the efficacy of the technique in a patient with AMI after an anterior cruciate ligament (ACL) injury.
Table 1.
Steps, Pearls, and Pitfalls of Conservative Method to Regain Full Extension of Knee and Recover Activation of Quadriceps
| Step | Pearls | Pitfalls |
|---|---|---|
| 1 and 3 | The patient should be examined in a semi-recumbent position. | If the patient is lying completely flat, it is more difficult to evaluate quadriceps function because the rectus femoris is already under tension. |
| 1 | It is important to differentiate between rectus femoris and vastus medialis contractions. | Rectus femoris function is typically preserved in AMI and can mislead the practitioner into thinking that quadriceps activation failure is not present. |
| 2 | The foot should be supported in the relaxation phase of hamstring fatigue exercises. | Without support, the patient will be in pain, and therefore, it will be more difficult for him or her to relax. |
| Eccentric exercises should not be performed; rather, the foot should be held to cause an isometric contraction. | Forcing the hamstring into eccentric contraction will cause pain. | |
| 3 | When the patient is performing quadriceps activation exercises, a pillow under the knee should be used initially to facilitate hamstring relaxation. | Recurrent hamstring contracture can occur. Using a pillow under the knee helps to relax the hamstrings. |
| If quadriceps activation failure persists, it is important to reassess the hamstrings for recurrent contracture. | If hamstring contracture is present, it is counterproductive to continue with quadriceps activation exercises. Instead, a return to step 2 is necessary. | |
| The practitioner should teach the patient hamstring relaxation and quadriceps activation exercises and instruct the patient to perform the exercises frequently. This repetition targets cortical neuroplasticity. | If patient compliance is low, then AMI may not improve rapidly. |
AMI, arthrogenic muscle inhibition.
Technique to Abolish Knee Extension Deficit and Quadriceps Activation Failure
Step 1: Identification of Quadriceps Activation Failure and Hamstring Contracture
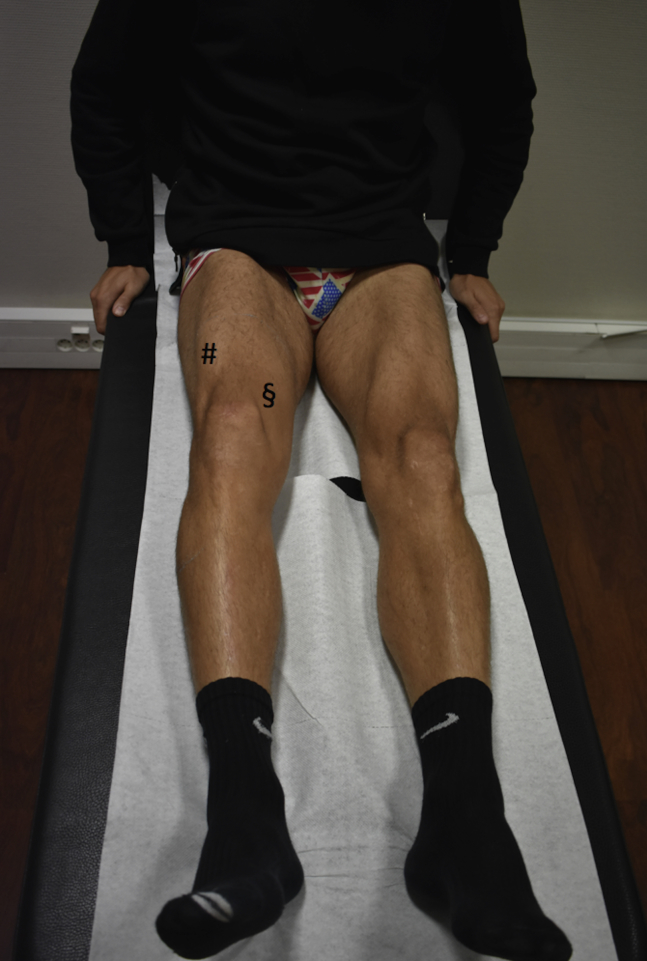
After a standard acute knee examination is performed and the presence of an extension deficit is established, the patient is positioned on the examination couch in a semi-recumbent position (Fig 1). Quadriceps activation failure is identified by asking the patient to contract the quadriceps muscles. The practitioner should observe specifically for contraction of the vastus medialis. Patients with AMI typically maintain the ability to contract the rectus femoris (hip flexor) but have a more profound inability to contract the vastus medialis (knee extensor) (Fig 2).
Fig 1.
Knee extension deficit evaluation of right knee (asterisk) with patient in supine position.
Fig 2.
Right quadriceps inactivation with lack of vastus medialis contraction (section sign) and active knee extension deficit. The rectus femoris contraction (pound sign) is maintained with active hip flexion.
After identification of quadriceps activation failure, the patient is placed prone on the examination couch. In this position, side-to-side palpation of the hamstrings allows determination of the presence of muscle contracture. If a hamstring contracture is not present, this should raise the suspicion that the extension deficit does not result from AMI and the differential diagnosis of a locked knee should be considered further.
Step 2: Hamstring Fatiguing
In the prone position, the patient is asked to repetitively contract and relax the hamstrings. The practitioner places his or her hand against the patient's leg to provide resistance against the contraction (Fig 3A). This limits the range of motion required to perform the exercise, thus making it more comfortable, but also helps to fatigue the hamstrings more rapidly. The contraction should be held for 2 to 3 seconds. Between each contraction, the patient is asked to relax the hamstrings completely to the best of his or her ability. To help fully relax the hamstrings, without causing pain, the practitioner should also gently support the foot on its way down to the examination table (Fig 3B). Once the hamstrings are fully fatigued, the muscle contracture resolves, leading to full extension of the knee (Fig 4). Usually, this can be achieved within 10 minutes, but on some occasions, it can take longer. It is important to note that the practitioner should never push against the leg to gain passive extension of the knee because it is painful.
Fig 3.
Hamstring fatigue. The patient is asked to repetitively contract against resistance (A) and relax the hamstrings (B). To help fully relax the hamstrings, the practitioner should gently support the foot on its way down to the examination table. A right knee is shown with the patient in the prone position.
Fig 4.
Full knee extension (asterisk) recovery after hamstring fatigue. A right knee is shown with the patient in the prone position.
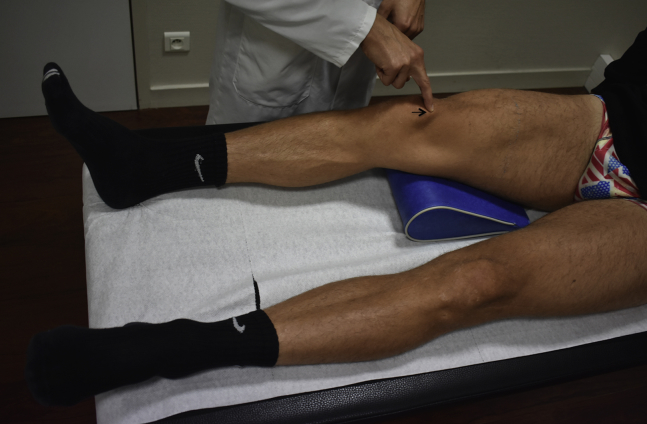
Step 3: Reactivation of Quadriceps Muscle Contraction
Once full passive extension of the knee is recovered, it is important to regain active extension. If the patient remains unable to perform effective contraction of the quadriceps, a recurrent extension deficit is likely to occur when the hamstrings recover from the fatiguing exercises. Therefore, it is important that the patient regain the ability to strongly contract the quadriceps, primarily the vastus medialis.
In the semi-recumbent position, a small pillow is placed under the knee to obtain approximately 30° of flexion. This helps to allow relaxation of the hamstrings; it also allows the patient visual feedback of quadriceps contraction. Next, the patient is asked to perform heel lifts and straighten the knee. The practitioner can facilitate the movement by holding the great toe (passive muscle contraction) (Fig 5). This phase focuses on isometric quadriceps contractions. The patient is asked to contract the muscle without lifting the heel. An easy way to check the correct contraction of the muscle is to palpate the patella (Fig 6). During each contraction, the patella has to migrate proximally. If the patient only contracts the rectus femoris, the practitioner will observe a muscular contraction of the thigh without any movement of the patella. Once the patient is able to reliably contract the vastus medialis, the thickness of the pillow placed under the knee is progressively reduced until it can be removed completely and the patient can still show good contraction.
Fig 5.
Passive muscle contraction of quadriceps. The patient is requested to do a heel lift (arrow) and straighten the knee. The practitioner can facilitate the movement by holding the great toe. A right knee is shown with the patient in the supine position.
Fig 6.
Active isometric muscle contraction of quadriceps. The patient is asked to contract the muscle without lifting the heel. To check the correct contraction of the muscle, the practitioner should palpate the patella to feel its proximal migration (arrow). A right knee is shown with the patient in the supine position.
During these exercises, it is important to check that the patient does not have co-contraction of the quadriceps and hamstrings. If this is the case, then the thickness of the pillow should be increased and quadriceps contractions repeated. It is also important to make sure the hamstrings remain relaxed and are not again in contracture. If a recurrent contracture is observed, then hamstring fatigue exercises (step 2) should be repeated.
Discussion
This Technical Note and accompanying video describe a simple set of exercises that typically result in full restoration of extension and good quadriceps activation within a few minutes. These exercises are therefore a quick and easy solution to what has traditionally been considered a difficult problem in some patients.
Regaining full symmetrical extension is a primary goal of early-phase rehabilitation after ACL reconstruction. Failure to regain full extension by 3 weeks after ACL reconstruction is an important predictive factor for subsequent cyclops syndrome.2 We believe that this technique has transformed our practice. We have previously reported a post–ACL reconstruction cyclops rate of 2.1%, which was noted to reduce to 0.1% after we introduced this technique.2
After knee injury, it is important not to confuse AMI with a locked knee. It should be noted that a magnetic resonance imaging–proven displaced bucket-handle tear does not definitively show that the extension deficit is due to a mechanical block to extension. Shakespeare and Rigby4 observed that 10% of patients with a displaced bucket-handle tear of the meniscus did not present with any locking of the knee. In addition, Allum and Jones1 reported that among patients presenting with a knee extension deficit after injury, 92% had intra-articular pathology but only 16% of the knees remained locked after induction of anesthesia. They concluded that the knee extension deficit present in most patients was due to hamstring muscle spasms.
Since the 1990s, studies have shown that hamstring contracture was associated with quadriceps inactivation and that this occurred because of a process known as AMI.3 Orthopaedic surgeons deal with these types of clinical presentations on a daily basis. However, AMI is not a well-established orthopaedic concept because most articles on this subject have been published in non-orthopaedic journals.
The underlying mechanism of AMI is not fully understood but is believed to be initiated by acute swelling, inflammation, pain, and joint laxity.3 These pathologies lead to changes in the discharges of intra-articular receptors, which subsequently result in an increase in certain central nervous system pathways such as the flexion reflex.3 This reflex results in overstimulation of the hamstring muscle and inhibition of the quadriceps. The described exercises specifically target AMI by reducing the influence of spinal hyperreflexia by fatiguing the hamstrings and tackling cortical neuroplasticity through repetition of quadriceps activation exercises.
AMI is an important problem in the preoperative knee surgery patient. Preoperative full knee extension has been shown to be important in regaining postoperative knee extension and limiting arthrofibrosis after ACL surgery.5 Similarly, quadriceps weakness has been shown to result in muscle atrophy, poor function, persistent knee pain, and cyclops syndrome.2, 6, 7 To avoid these complications, Cosgarea et al.8 suggested delaying surgery until the patient has achieved “nearly normal knee motion,” which could sometimes take weeks or months. Other therapeutic interventions have been described to combat AMI, but these all require additional equipment, are time-consuming, and have varied results.3 The exercises described in this technical article are a simple and effective method for restoration of full knee extension and quadriceps activation within minutes (Table 2). It is our opinion that everyone dealing with acute knee injuries should be familiar with these exercises because they are easy to perform and highly effective.
Table 2.
Advantages and Disadvantages of Proposed Method to Combat AMI
| Advantages |
| Easy to perform |
| Rapid restoration of full extension and quadriceps activation |
| Reduced rate of cyclops lesions |
| No special equipment necessary |
| Pain alleviation |
| Easier postoperative recovery if patient is aware of how to contract quadriceps immediately |
| Speeds up time taken for patient to achieve full extension and, if necessary, can proceed with surgery sooner without increased risk of arthrofibrosis |
| No recognized reliable alternative |
| Disadvantages |
| Takes extra time in office |
| Can be painful to patient if performed incorrectly (Table 1) |
AMI, arthrogenic muscle inhibition.
Footnotes
The authors report the following potential conflict of interest or source of funding: A.S. receives support from Arthrex. Consultant. M.T. receives support from Arthrex. Consultant. B.S-C. receives support from Arthrex. Consultant, royalties. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Step-by-step demonstration of an easy and rapid method that any practitioner can apply in his or her medical office to abolish knee extension deficit after injury or surgery.
References
- 1.Allum R.L., Jones J.R. The locked knee. Injury. 1986;17:256–258. doi: 10.1016/0020-1383(86)90231-7. [DOI] [PubMed] [Google Scholar]
- 2.Pinto F.G., Thaunat M., Daggett M. Hamstring contracture after ACL reconstruction is associated with an increased risk of cyclops syndrome. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967116684121. 2325967116684121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rice D.A., McNair P.J. Quadriceps arthrogenic muscle inhibition: Neural mechanisms and treatment perspectives. Semin Arthritis Rheum. 2010;40:250–266. doi: 10.1016/j.semarthrit.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Shakespeare D.T., Rigby H.S. The bucket-handle tear of the meniscus. A clinical and arthrographic study. J Bone Joint Surg Br. 1983;65:383–387. doi: 10.1302/0301-620X.65B4.6874707. [DOI] [PubMed] [Google Scholar]
- 5.McHugh M.P., Tyler T.F., Gleim G.W., Nicholas S.J. Preoperative indicators of motion loss and weakness following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1998;27:407–411. doi: 10.2519/jospt.1998.27.6.407. [DOI] [PubMed] [Google Scholar]
- 6.Amin S., Baker K., Niu J. Quadriceps strength and the risk of cartilage loss and symptom progression in knee osteoarthritis. Arthritis Rheum. 2009;60:189–198. doi: 10.1002/art.24182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lindstrom M., Strandberg S., Wredmark T., Fellander-Tsai L., Henriksson M. Functional and muscle morphometric effects of ACL reconstruction. A prospective CT study with 1 year follow-up. Scand J Med Sci Sports. 2013;23:431–442. doi: 10.1111/j.1600-0838.2011.01417.x. [DOI] [PubMed] [Google Scholar]
- 8.Cosgarea A.J., Sebastianelli W.J., DeHaven K.E. Prevention of arthrofibrosis after anterior cruciate ligament reconstruction using the central third patellar tendon autograft. Am J Sports Med. 1995;23:87–92. doi: 10.1177/036354659502300115. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Step-by-step demonstration of an easy and rapid method that any practitioner can apply in his or her medical office to abolish knee extension deficit after injury or surgery.