Abstract
Hip arthroscopy is useful in the treatment of several intra-articular pathologies, however, its use in high-energy hip and pelvis injuries raises concerns about fluid extravasion and stability of the pelvic ring. We present our arthroscopic surgical technique (initial access to the peripheral compartment) to remove intra-articular loose bodies and treat associated lesions, as well as our concerns with the technique, in case of a traumatic hip dislocation associated with a contralateral pelvic ring injury.
One of the earliest indications for hip arthroscopy was the removal of loose bodies. Currently it is the gold standard for diagnosis and treatment of intra-articular hip pathology, namely, labral tears, chondral lesions, femoroacetabular impingement, and synovial pathology, among others.1, 2
Intra-articular loose bodies after a traumatic hip dislocation may lead to additional chondral damage, although the severity of the lesion may be directly related to the dislocation. These two related conditions may lead to early development of arthritis.3
The use of hip arthroscopy in high-energy injuries like hip dislocation or pelvic ring fractures raises some concerns. The use of intra-articular fluid under pressure after hip dislocation with capsular disruption may lead to soft-tissue extravasation and eventually secondary abdominal or thigh compartment syndrome.4 As for the pelvic ring fracture, the use of traction on the lower limbs to access the central compartment may displace fractures and exasperate the pelvic instability.5
The purpose of this article is to report our approach in case of a nonconcentric reduction after traumatic hip dislocation and a pelvic ring fracture.
Surgical Technique
Clinical Case and Preoperative Planning
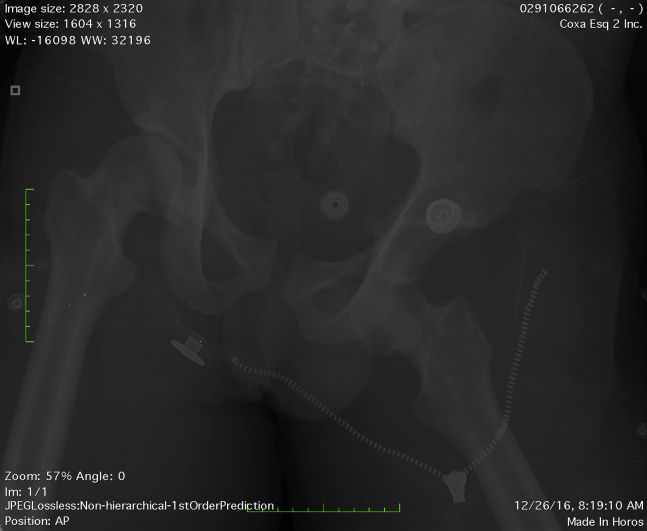
We present our technique used in a left hip anteroinferior dislocation with a pelvic ring injury (fracture of the contralateral iliac wing associated with symphyseal diastasis of less than 25 mm; Fig 1). This represents a variant of the anteroposterior compression (APC I)6 injury with a fracture of the ilium instead of the disruption of the anterior sacroiliac ligaments.
Fig 1.
Pelvis radiograph showing the anteroinferior left hip dislocation and the contralateral wing of ilium fracture.
In this type of lesion, the patient should be submitted to an emergent close reduction of the hip dislocation under general anesthesia. Likewise, other life-threatening lesions should be promptly addressed.
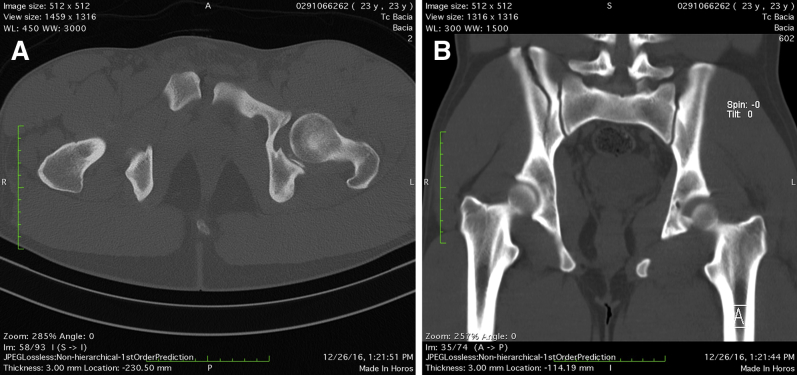
Imaging after reduction should be obtained to evaluate joint congruency, associated fractures, and intra-articular loose bodies. If it reveals a nonconcentric reduction of the hip (Fig 2), a postreduction computed tomography scan might show intra-articular bone fragments in the central compartment (Fig 3).
Fig 2.

Anteroposterior pelvis radiograph in dorsal decubitus after reduction of the dislocation showing a nonconcentric reduction of the left hip, right iliac fracture, widening, and slight translation of the pubic symphysis. The arrow shows increased medial joint space.
Fig 3.
Pelvic computed tomography after reduction. (A) Axial reconstruction showing widening and anterior translation of the right pubic bone. (B) Coronal reconstruction showing a fracture of the right iliac wing without involvement of the sacroiliac joint (this fracture is complete). Both images show a nonconcentric reduction and the presence of intra-articular posteroinferior bone fragments interposed between the femoral head and acetabulum.
Indication for the Procedure
The nonconcentric reduction of the hip and the presence of intra-articular loose bodies are clinically problematic and would probably lead to post-traumatic early osteoarthritis. Surgical intervention to remove loose bodies and treat other intra-articular lesions should be expeditious.
Our first choice for the surgical management is hip arthroscopy as it is a less invasive technique in a high-energy pelvic trauma, although the surgeon should also be prepared for an open hip surgery if necessary.
Patient Position and Preparation
The feet and the perineal post are protected with foam pads to diminish the risk of traction-related complications (supine perineal post pad and supine boot insert pad, Smith and Nephew, Andover, MA).
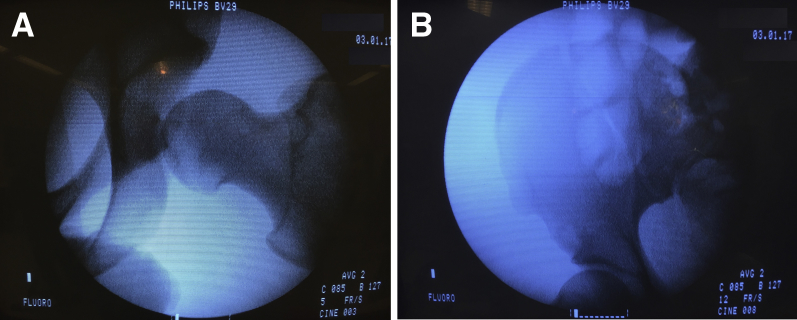
Our first concern is the stability of the pelvic ring fracture as no fixation is planned for that type of fracture. For that reason and before starting the arthroscopy, with the patient in the supine position on the traction table, the hip is tested under traction with fluoroscopy and general anesthesia. The hip distraction is usually easily achieved (due to capsular and ligament injury), and no deviation of the iliac fracture or the pubic symphysis should be found on fluoroscopy (Fig 4).
Fig 4.
Preoperative fluoroscopy during traction test of the left hip (A). No fracture deviation was shown (B).
Arthroscopic Procedure
As the pelvic injury is stable under traction, we can proceed with hip arthroscopy and follow our routine technique starting with the peripheral compartment approach without traction as described by Dienst.7 Due to the risk of fluid extravasation, we use low pressure in the fluid pump (Double Pump; Medical Vision AB, Nacka, Sweden; parameters pressure 50 mmHg, flow 100 mL/m) and constantly check for thigh or abdominal swelling as we use transparent surgical fields (Barrier Vertical Isolation Drape 330 × 240 cm, incise area 25 × 86 cm; Mölnlycke Health Care AB, Gothenburg, Sweden).
Peripheral Compartment
For the peripheral compartment access, a proximal anterolateral portal is established without traction (Disposable Hip Pac, Smith and Nephew) as the viewing portal (using an arthroscope with a 70° lens) and anterior and anterolateral portals as working portals.7
Findings and Procedures
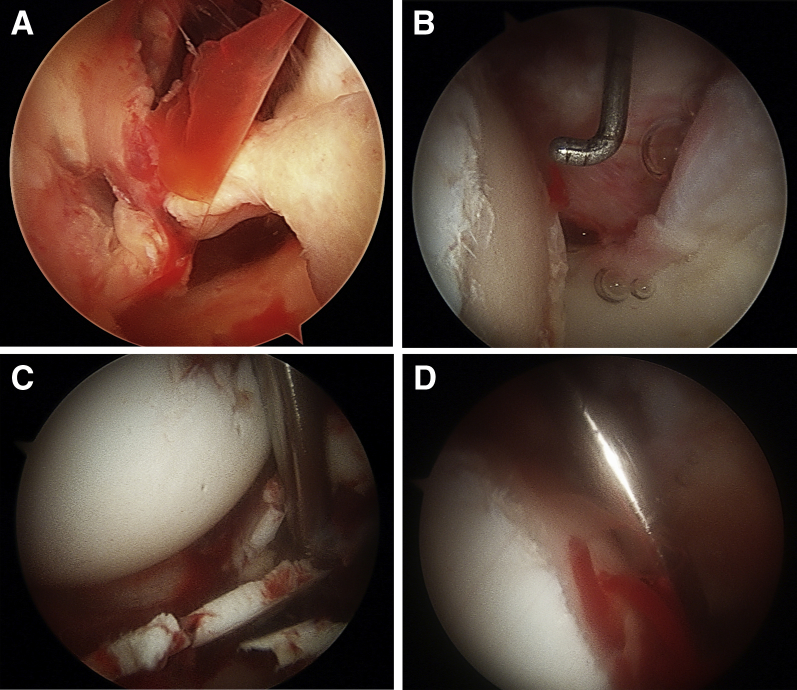
In the peripheral compartment we found a hematoma, rupture of the anteroinferior capsule, a gap between the femoral head and acetabulum, and extensive chondral damage of the femoral head with subchondral bone exposure (Beck grade 4; Fig 5).8 To increase maneuverability of the instruments and improve visualization, we perform a synovectomy and a capsular thinning, particularly at the zona orbicularis, using a shaver and radiofrequency wand (shaver 4.5-mm-long Incisor Plus Elite Blade 180 mm and radiofrequency wand AMBIENT HipVac 50 IFS 4.7 mm 50° Suction; Smith and Nephew; Video 1).
Fig 5.
Left hip arthroscopy. (A) Intra-articular hematoma and rupture of the anteroinferior capsule; (B) chondral lesion of the femoral head with subchondral bone exposure at the central compartment, (C) intra-articular chondral fragments, and (D) microfractures on the femoral head, which continued to bleed.
Establishing Access to Central Compartment
The least amount of traction possible is used as we establish access to the central compartment from the peripheral compartment (anterolateral portal) under direct arthroscopic control (proximal anterolateral portal) with the use of a switching stick (anterior portal) to push the lateral capsule.7, 9
Central Compartment
Findings and Procedures
In this compartment we can see the full extension of the chondral lesion in the femoral head with subchondral bone exposure (Beck grade 4)8 at zones 2 and 3 as described by Ilizaliturri et al.,10 ligamentum teres rupture, chondral fragments, and an irreparable complete tear with a flap of the labrum in zone 5 (Fig 5 and Video 1).
During the procedure, the viewing and working portals are alternated for enhanced exposure and access within the central compartment.
We performed a debridement of the ligamentum teres, and loose chondral fragments and a posterior labrum flap were removed through the anterolateral and posterolateral portals, respectively (basket punch 90° rotary; Smith and Nephew).
We also performed microfractures (XL Microfracture 90° Pick, Smith and Nephew) on the exposed subchondral bone of the femoral head, and bleeding was noticed upon closing the inflow tube (Fig 5).
Final Step
Finally, at the end of the surgery we check whether there was any fracture displacement of the ilium and pubic symphysis or fluid extravasation. The indication/contraindications for the procedure, pearls/pitfalls, and advantages/disadvantages of this technique are listed in Table 1, Table 2, Table 3, respectively.
Table 1.
Indications and Contraindications for the Arthroscopic Treatment of Hip Dislocation Associated With a Pelvic Ring Fracture
| Indications | Contraindications |
|---|---|
| Stable patterns of pelvic ring fracture or patterns amenable to fixation. | Unstable pelvic ring fractures. |
| Dislocation with associated soft-tissue injuries: labral tears, osteocondral fragments, capsular rupture. | Ipsilateral fracture that precludes application of traction. |
Table 2.
Step-by-Step Analysis of Pearls and Pitfalls
| Pearls | Pitfalls | |
|---|---|---|
| Preoperative evaluation | Use computed tomography (CT) to assess the quality of the reduction as well as the extent and patterns of associated fractures. | CT underestimates the extent of the associated soft-tissue injuries. |
| Stability assessment | Traction should be applied slowly and constantly checked in the image intensifier for gross instability. Disruption of the capsule and labrum leads to an easily distractible joint. |
Fluoroscopy may underestimate fracture displacement. Excessive traction may increase capsular and ligament injury and can lead to neurovascular injury. |
| Arthroscopic procedure | Transparent surgical fields and low pump pressures diminish fluid extravasation risks. Peripheral compartment access first is established without traction while also precluding iatrogenic articular damage on entering the central compartment. Arthroscopic visualization of articular distraction allows better control of the amount of traction needed. Unconventional portal placement could be important according to the identified lesions. |
Hematoma can impair visualization; mechanical shaver should be used instead of high pump pressures. Several solutions should be readily available for labrum tears, osteocondral lesions, capsular management. |
Table 3.
Advantages and Disadvantages of Arthroscopic Treatment of Hip Dislocation Associated With a Pelvic Ring Fracture
| Advantages | Disadvantages |
|---|---|
| Arthroscopy allows the diagnosis and concomitant treatment of undiagnosed lesions in the preoperative image assessment. | Hip arthroscopy has a steep learning curve and is technically very demanding. |
| Less invasive and decreases the risk of further capsular damage and blood supply compromise. | The use of a fluid pump in a hip with capsular damage increases the risk of fluid extravasation and compartmental syndrome. |
| Traction can displace an otherwise stable pelvic ring fracture. |
Rehabilitation
The rehabilitation protocol should include continuous passive motion device with hip flexion limited to 70° started on day one. Sitting in bed and walking with partial weight bearing on the nonfracture side can be started as tolerated. At 6 weeks, progressive weight bearing on both sides can be started as tolerated with the use of crutches, until full weight bearing.
Discussion
Many investigators agree that hip arthroscopy is useful in treating the intra-articular lesions (namely, loose bodies, labral tears, chondral lesions) documented in radiological exams after traumatic hip dislocation in order to prevent further complications.11, 12, 13, 14 Some (Mullis and Dahners) go further to say that a routine hip arthroscopy should be done after traumatic hip dislocation, as intraoperative loose bodies can be found in patients in which standard radiographic studies found no loose bodies and a concentric reduction was obtained.15, 16
However, there are few case reports addressing early hip arthroscopy after hip dislocation and even less associated with pelvic ring fractures. The APC type I pelvic fractures are complete disruptions of the anterior pelvic ring combined with incomplete disruptions of the posterior arch that allow rotation of the hemipelvis. This fracture pattern therefore presents with rotational instability in the absence of vertical instability.17 Therefore the use of a traction device in the contralateral hip should present no significant risk for further displacement. Despite that, careful preoperative and intraoperative fluoroscopic assessment of the pelvic ring, as traction is applied, is fundamental. The presence of capsular and ligament lesions of the dislocated hip further helped to obtain gentle distraction of the joint without fracture displacement. To the best of our knowledge, there is only one case report of hip arthroscopy performed early after an accident involving hip dislocation and pelvic ring fracture, even though in that case the pelvic ring injury was treated with osteosynthesis prior to arthroscopy.5 With the technique that we describe, no complication in the pelvic fracture was noticed after hip arthroscopy provided that the pelvis is stable under traction testing.
We believe that the initial access to the peripheral compartment is beneficial for several reasons. First, with this technique we can perform a sequential examination and treatment in this compartment without traction, therefore limiting the adverse effects of a prolonged traction time. Second, we establish access to the central compartment under arthroscopic visualization, which decreases the risk of further articular damage.7 Hip distraction under direct arthroscopic control has advantages over the fluoroscopic imaging because it is possible to determine the exact space needed to access the central compartment with the arthroscopic cannula and minimize the amount of traction. Lastly, with this approach we can minimize the capsular incisions, which further compromise hip stability.
In anterior dislocation, osteochondral impaction usually occurs at the posterolateral aspect of the femoral head. The chondral lesion results from impaction of the femoral head on the anteroinferior rim of the acetabulum after the femoral head exits the acetabulum.16 These defects may be positioned anteriorly or posteriorly, depending on the degree of external rotation of the femur at the time of the dislocation.
One of the risks after traumatic hip dislocation is avascular necrosis of the femoral head, which can occur in 5% to 40% of injuries but can become clinically apparent several years after injury.3 In addition, hip arthroscopy can be associated with avascular necrosis of the femoral head due to traction on vessels supplying the femoral head, direct injury to such vessels during portal entrance, femoral osteochondroplasty, raised intra-articular pressure, or prolonged operating time, estimating this risk at 0.4%.18, 19 We believe that femoral head can maintain its viability because we do intermittent traction and after femoral head microfractures bleeding can be seen.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: P.D. receives support from Smith and Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The case of a left hip anteroinferior dislocation with a pelvic ring injury (fracture of the contralateral iliac wing associated with symphyseal diastasis of less than 25 mm) is shown. The patient is submitted to an emergent close reduction of the hip dislocation under general anesthesia. Imaging evaluation after reduction shows nonconcentric reduction of the hip with intra-articular bone fragments of the central compartment. The concerns in doing an arthroscopy of the injured hip include (1) fracture displacement and (2) fluid extravasation. The following aspects of planning the hip arthroscopy are shown: (1) preoperative hip traction test in supine with fluoroscopy under general anesthesia; (2) fluid pump with low pressure; (3) transparent surgical fields; (4) arthroscopy technique—peripheral compartment first and access to central compartment with arthroscopic control. The following aspects of performing the arthroscopy are shown: (1) peripheral compartment access—a proximal anterolateral portal is established without traction as the viewing portal (arthroscope 70° lens) and anterior and anterolateral portals as working portals. To increase maneuverability of the instruments and improve visualization, perform a synovectomy and a capsular thinning, particularly of the zona orbicularis, using a shaver and radiofrequency wand. (2) Findings in the peripheral compartment: hematoma, rupture of the anteroinferior capsule, gap between the femoral head and the acetabulum, and chondral lesion of the femoral head with subchondral bone exposure. (3) Establishing access to central compartment: minimum traction is established and access to the central compartment from the anterolateral portal under arthroscopic control. (4) During the procedure, the viewing and working portals are alternated for enhanced exposure and access. (5) Findings in the central compartment: chondral lesion of the femoral head with subchondral bone exposure at zones 2 and 3, ligamentum teres rupture, chondral fragments, and an irreparable complete tear of the labrum in zone 5. Debridement of the ligamentum teres, removal of loose chondral fragments and labrum performed through the anterolateral and posterolateral portals, respectively. Microfractures of the defect in the femoral head and bone bleeding.
References
- 1.Phillips B.B., Mihalko M.J. Arthroscopy of the lower extremity. In: Azar F.M., Beaty J.H., Canale S.T., editors. Campbell's operative orthopaedics. Elsevier; Philadelphia: 2017. pp. 2486–2566. [Google Scholar]
- 2.Marin-Peña O., Tey-Pons M., Perez-Carro L. The current situation in hip arthroscopy. EFORT Open Rev. 2017;2:58–65. doi: 10.1302/2058-5241.2.150041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Egol K.A., Koval K.J., Zuckerman J.D. Wolters Kluwer Health; Philadelphia: 2015. Handbook of fractures. [Google Scholar]
- 4.Kocher M.S., Frank J.S., Nasreddine A.Y. Intra-abdominal fluid extravasation during hip arthroscopy: a survey of the MAHORN group. Arthroscopy. 2012;28:1654–1660. doi: 10.1016/j.arthro.2012.04.151. [DOI] [PubMed] [Google Scholar]
- 5.Kindler M., Halfmann B., Schoepp C., Rixen D. Hüftgelenkarthroskopie nach Luxatio obturatoria. Der Unfallchirurg. 2016;119:62–68. doi: 10.1007/s00113-015-0011-1. [DOI] [PubMed] [Google Scholar]
- 6.Burgess A.R., Eastridge B.J., Young J.W. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 1990;30:848–856. [PubMed] [Google Scholar]
- 7.Dienst M. Peripheral compartment approach to hip arthroscopy. In: Sekiya J.K., Safran M.R., Ranawat A.S., Leunig M., editors. Techniques in hip arthroscopy and joint preservation surgery. Elsevier; Philadelphia: 2011. pp. 105–112. [Google Scholar]
- 8.Beck M., Leunig M., Parvizi J., Boutier V., Wyss D., Ganz R. Anterior femoroacetabular impingement. Part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73. [PubMed] [Google Scholar]
- 9.Aguiar T., Dantas P. Arthroscopic resection of intra-articular osteochondromas of the hip. Arthrosc Techn. 2014;3:e347–e350. doi: 10.1016/j.eats.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ilizaliturri V.M., Jr., Byrd J.W., Sampson T.G. A geographic zone method to describe intra-articular pathology in hip arthroscopy: cadaveric study and preliminary report. Arthroscopy. 2008;24:534–539. doi: 10.1016/j.arthro.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 11.Kekatpure A., Ahn T., Lee S.J., Jeog M.Y., Chang J.S., Yoon P.W. Arthroscopic reduction and internal fixation for Pipkin type I femoral head fracture: technical note. Arthrosc Techn. 2016;5:e997–e1000. doi: 10.1016/j.eats.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park M.S., Yoon S.J., Choi S.M. Hip arthroscopic management for femoral head fractures and posterior acetabular wall fractures (Pipkin type IV) Arthrosc Tech. 2013;2:e221–e225. doi: 10.1016/j.eats.2013.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stabile K.J., Neumann J.A., Mannava S., Howse E.A., Stubbs A.J. Arthroscopic treatment of bucket-handle labral tear and acetabular fracture. Arthrosc Tech. 2014;3:e283–e287. doi: 10.1016/j.eats.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hwang J.T., Lee W.Y., Kang C., Hwang D.S., Kim D.Y., Zheng L. Usefulness of arthroscopic treatment of painful hip after acetabular fracture or hip dislocation. Clin Orthop Surg. 2015;7:443–448. doi: 10.4055/cios.2015.7.4.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mullis B.H., Dahners L.E. Hip arthroscopy to remove loose bodies after traumatic dislocation. J Orthop Trauma. 2006;20:22–26. doi: 10.1097/01.bot.0000188038.66582.ed. [DOI] [PubMed] [Google Scholar]
- 16.Mandell J.C., Marshall R.A., Banffy M.B., Khurana B., Weaver M.J. Arthroscopy after traumatic hip dislocation: a systematic review of intra-articular findings, correlation with magnetic resonance imaging and computed tomography, treatments, and outcomes. Arthroscopy. 2018;34:917–927. doi: 10.1016/j.arthro.2017.08.295. [DOI] [PubMed] [Google Scholar]
- 17.Bellabarba C., Winkelmann M., Decker S., Bransford R.J., Krettek C. Pelvic ring injuries. In: Browner B.D., Jupiter J.B., Krettek C., Anderson P.A., editors. Skeletal trauma: basic science, management, and reconstruction. Elsevier; Philadelphia: 2015. pp. 1021–1105. [Google Scholar]
- 18.Santos S., Seijas R., Alvarez P. Femoral head osteonecrosis following a hip arthroscopy: a case report. Ann Sports Med Res. 2015;2:1033. [Google Scholar]
- 19.Gupta A., Redmond J.M., Hammarstedt J.E., Schwindel L., Domb B.G. Safety measures in hip arthroscopy and their efficacy in minimizing complications: a systematic review of the evidence. Arthroscopy. 2015;30:1342–1348. doi: 10.1016/j.arthro.2014.04.103. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The case of a left hip anteroinferior dislocation with a pelvic ring injury (fracture of the contralateral iliac wing associated with symphyseal diastasis of less than 25 mm) is shown. The patient is submitted to an emergent close reduction of the hip dislocation under general anesthesia. Imaging evaluation after reduction shows nonconcentric reduction of the hip with intra-articular bone fragments of the central compartment. The concerns in doing an arthroscopy of the injured hip include (1) fracture displacement and (2) fluid extravasation. The following aspects of planning the hip arthroscopy are shown: (1) preoperative hip traction test in supine with fluoroscopy under general anesthesia; (2) fluid pump with low pressure; (3) transparent surgical fields; (4) arthroscopy technique—peripheral compartment first and access to central compartment with arthroscopic control. The following aspects of performing the arthroscopy are shown: (1) peripheral compartment access—a proximal anterolateral portal is established without traction as the viewing portal (arthroscope 70° lens) and anterior and anterolateral portals as working portals. To increase maneuverability of the instruments and improve visualization, perform a synovectomy and a capsular thinning, particularly of the zona orbicularis, using a shaver and radiofrequency wand. (2) Findings in the peripheral compartment: hematoma, rupture of the anteroinferior capsule, gap between the femoral head and the acetabulum, and chondral lesion of the femoral head with subchondral bone exposure. (3) Establishing access to central compartment: minimum traction is established and access to the central compartment from the anterolateral portal under arthroscopic control. (4) During the procedure, the viewing and working portals are alternated for enhanced exposure and access. (5) Findings in the central compartment: chondral lesion of the femoral head with subchondral bone exposure at zones 2 and 3, ligamentum teres rupture, chondral fragments, and an irreparable complete tear of the labrum in zone 5. Debridement of the ligamentum teres, removal of loose chondral fragments and labrum performed through the anterolateral and posterolateral portals, respectively. Microfractures of the defect in the femoral head and bone bleeding.