Abstract
The injuries of the posterolateral corner (PLC) of the knee often remain misdiagnosed. Because most structures in this anatomical region have low potential to heal, the posterolateral rotational instability results in a deterioration in patient quality of life, impaired biomechanics of the knee, and increased tension on other ligaments and the meniscus. Many open and a few arthroscopic techniques have been developed to repair or reconstruct the damaged structures of the PLC. Creating an additional midlateral arthroscopic portal on the lateral side of the knee was the key to developing the technique to recreate a static stabilizer against external rotational instability of the PLC by fixing the popliteus tendon as a native, vascularized material to the tibia.
Injuries of the posterolateral corner (PLC) of the knee are encountered in almost 16% of all knee injuries.1 Despite improvements in the understanding of PLC anatomy and biomechanics, proper diagnosis is difficult and remains a result based on subjective abilities like clinical skills and experience. It is the reason why many cases of PLC injuries still remain overlooked. The structures of the PLC have low potential to heal, and when they are left untreated, chronic posterolateral rotational instability develops.2 This instability affects the biomechanics of the knee, leading to increased load on medial compartment; as a consequence, earlier osteoarthritis may occur.1 Furthermore, unrecognized posterolateral instability may lead to failure of the anterior cruciate ligament/posterior cruciate ligament (PCL) reconstructions.3 Various open anatomic and isometric reconstruction techniques address these pathologies.1, 4, 5 In addition, arthroscopic reconstruction techniques have been developed.6, 7, 8 Following the idea of Frosch et al.,6, 7 the additional midlateral arthroscopic portal was created. Using this portal, a unique treatment option using popliteus tendon (PLT) as a static, natural, vascularized stabilizer for the PLC was developed. The arthroscopic PLC stabilization technique using popliteus tenodesis allows restoration of the static function of popliteus complex anatomically. The midlateral portal allows a direct visual anatomic approach to the sulcus popliteus with minimized invasiveness.
Diagnosis
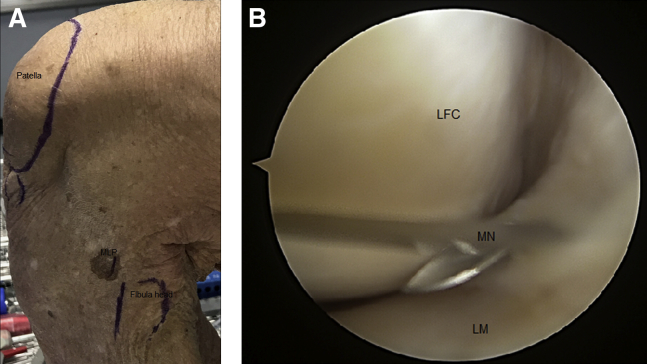
Posterolateral instability of the knee is diagnosed by physical examination (posterolateral drawer test, dial test in 30° and 90°) and arthroscopic visualization presenting an increased widening of lateral joint space (drive-through sign) with elevation of the lateral meniscus in the figure-of-4 position (Fig 1). All of the patients operated on with this technique signed a consent form. The study protocol was approved by the bioethics committee.
Fig 1.
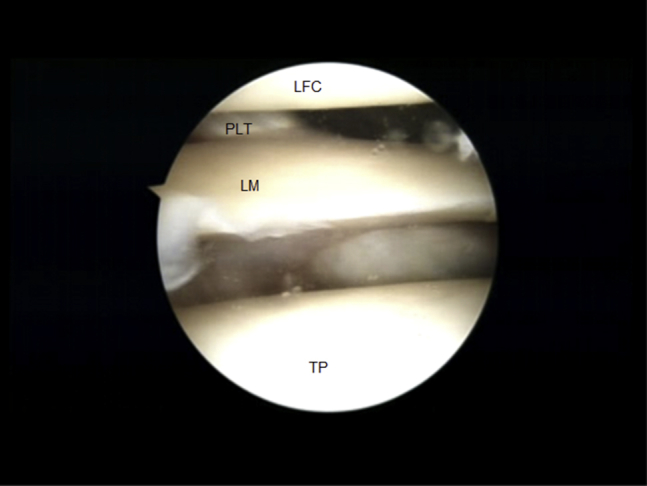
Arthroscopic view from the anterolateral viewing portal in the right knee. The drive-through sign with elevated lateral meniscus (LM) confirms the diagnosis of posterolateral corner injury. (LFC, lateral femoral condyle; PLT, popliteus tendon; TP, tibial plateau.)
Surgical Technique
Indications
The indication for surgery is posterolateral rotational instability of the knee. Grade A instability calls for an isolated procedure, and grades B and C are part of a combined procedure according to the Fanelli and Larson classification.9
Contraindications
The contraindications for surgery are damaged femoral PLT attachment, advanced degenerative joint disease, varus deformity of the knee, and systemic diseases such as rheumatoid arthritis.
Patient Positioning
The patient is placed in the supine position. A nonsterile thigh tourniquet is put on to limit intraoperative bleeding. The leg is placed in the leg holder and prepared in a standard sterile fashion.
Diagnostic Arthroscopy
Arthroscopy is performed through standard anterolateral and anteromedial portals with a 30° arthroscope. During the inspection, concomitant intra-articular lesions are ruled out. When the drive-through sign and elevation of lateral meniscus with the knee in figure-of-4 position are observed, the diagnosis of posterolateral instability is confirmed (Fig 1). The decision about performing PLC stabilization with popliteus tenodesis is made.
Arthroscopic PLC Stabilization With Popliteus Tenodesis
To visualize the PLC structures, the arthroscope is introduced through the anterolateral portal to the patellofemoral joint and then moved laterally to the lateral recess with the knee in full extension. Under visual control, the midlateral portal on the lateral side of the knee is created with a mark needle and scalpel. The portal is located 1.5 cm above the fibular head and 1 cm anterior to the lateral collateral ligament (LCL; Fig 2 Video 1). Then the arthroscopic hook probe is introduced through the above-mentioned portal to identify PLC structures (Fig 3, Video 1). In the next step, the approach is extended with Pean's forceps throughout tissues behind the PLT to facilitate introducing the instruments. Then the Scorpion suture passer (Arthrex, Munich, Germany) is introduced through the midlateral portal and used to pass the FiberTape (Arthrex) around the PLT at the level of the planned site for tenodesis (Fig 4, Video 1). It has been proven by Frosch et al. that the best place for PLT fixation is the crossing of a horizontal line at the tip of the fibular head with a vertical line at the medial edge of the fibular head.7 The proximal part of tibial popliteal marking hook (Arthrex) is positioned in the proper place, whereas the 3.5-mm drill sleeve for FlipCutter (Arthrex) is placed just below the pes anserinus and a small skin incision is made (Fig 5, Video 1). The FlipCutter is used to drill through the tibia until it reaches the target at the tibial popliteal marking hook (Video 1). The aiming guide is removed, and the tibial tunnel is drilled retrogradely at the depth of 2 cm with a 6-mm FlipCutter (Fig 6, Video 1). The FlipCutter is removed, and FiberStick (Arthrex) is passed through the tibial tunnel (Fig 7, Video 1). An arthroscopic grasper is used to pull the passing suture out of the joint. The passing suture is used to pull the FiberTape from back to front through the tibia in order to turn the popliteus down to the tibia (Fig 8, Video 1). The FiberTape is knotted to a TightRope ABS Button (Arthrex) on the anteromedial cortex. The tension of PLT tenodesis is regulated with Pean's forceps under scope control by twisting the SutureButton (Arthrex) until the drive-through sign and elevation of lateral meniscus are eliminated (Video 1).
Fig 2.
View of the left knee joint. Midlateral portal (MLP) positioning from the outside (A) and inside (B). (LFC, lateral femoral condyle; LM, lateral meniscus; MN, marking needle.)
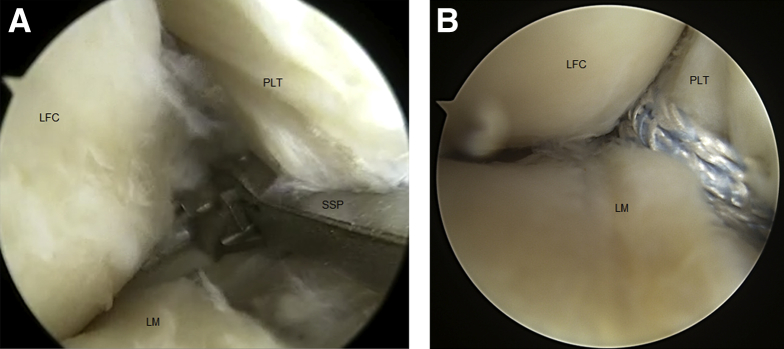
Fig 3.
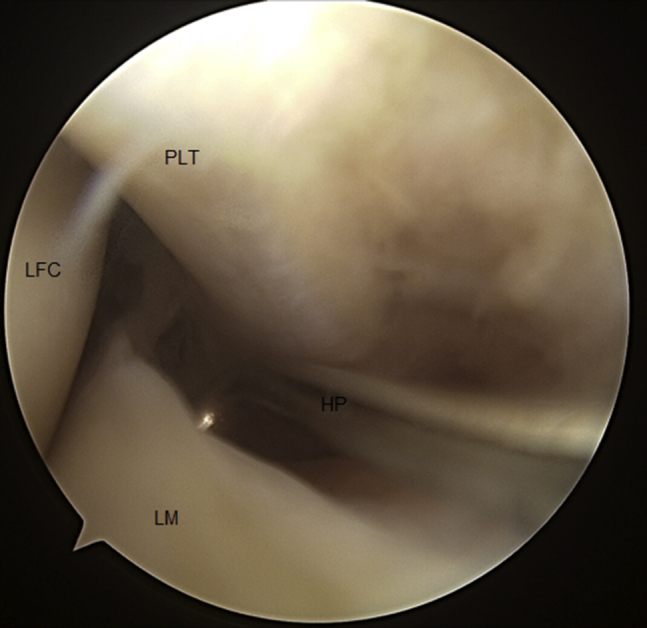
Arthroscopic view from the anterolateral viewing portal in the left knee joint. Identification of posterolateral corner structures with arthroscopic hook probe (HP). (LFC, lateral femoral condyle; LM, lateral meniscus; PLT, popliteus tendon.)
Fig 4.
Arthroscopic view from the anterolateral viewing portal in the left knee joint. The Scorpion suture passer (SSP) is introduced through the midlateral portal (A) and used to pass the FiberTape around the popliteus tendon (PLT) at the level of the planned site for tenodesis (B). (LFC, lateral femoral condyle; LM, lateral meniscus.)
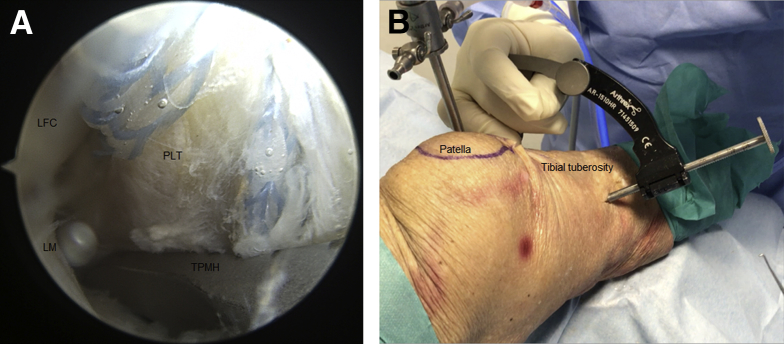
Fig 5.
(A) Arthroscopic view from the anterolateral viewing portal in the left knee joint. The tibial popliteal marking hook (TPMH) is positioned in the place for tenodesis below the lateral meniscus (LM). FiberTape rounds the popliteus tendon (PLT). LFC, lateral femoral condyle. (B) View on the left knee joint from the outside. The drill sleeve for FlipCutter is placed on the medial side of tibial tuberosity just below the pes anserinus.
Fig 6.

Arthroscopic view from the anterolateral viewing portal in the left knee joint. A 6-mm FlipCutter (FC) is used to retrogradely drill a tibial tunnel for popliteus tendon (PLT) tenodesis. (LFC, lateral femoral condyle.)
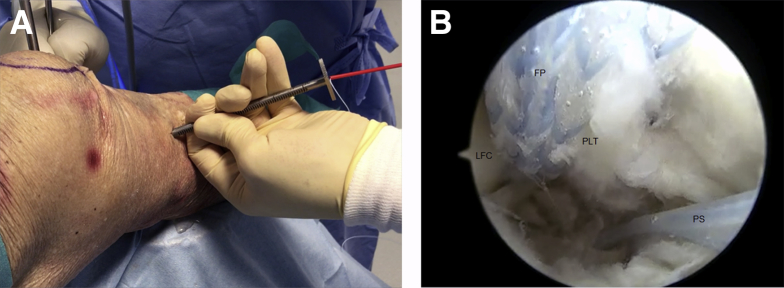
Fig 7.
(A) View on the left knee joint from the outside. FiberStick with passing suture introduced through the drill sleeve for FlipCutter. (B) Arthroscopic view from the anterolateral viewing portal in the left knee joint. Passing sutures (PS) used to introduce FiberTape (FP) with popliteus tendon (PLT) into the tibial tunnel. (LFC, lateral femoral condyle.)
Fig 8.
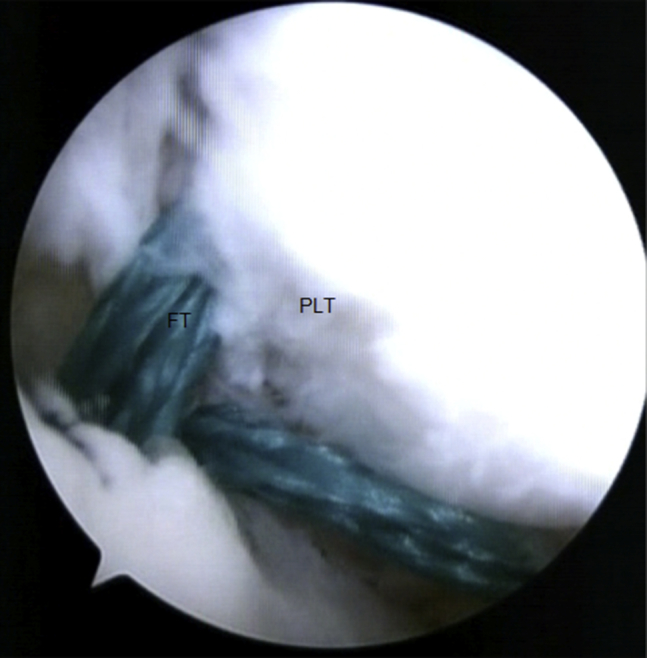
Arthroscopic view from the anterolateral viewing portal in the left knee joint. Popliteus tendon (PLT) tenodesis. (FT, FiberTape.)
Rehabilitation
The rehabilitation protocol is similar to that for PCL reconstruction. Passive knee motion is started from the second day after surgery. Walking on crutches for 6 weeks and orthesis with limited extension (30°) are recommended.
Discussion
Arthroscopic PLC stabilization with popliteus tenodesis is an efficient arthroscopic technique for posterolateral rotational instability of the knee. As an arthroscopic technique it avoids most of the disadvantages and risks of open surgeries. The perioperative tissue trauma is significantly lower than in the case of classic surgery, which makes the recovery time shorter and facilitates the introduction of more aggressive rehabilitation protocols. Arthroscopy provides visualization of important anatomical landmarks that cannot be viewed in open procedures. Furthermore, there is no need for common peroneal nerve preparation and neurolysis, what creates a potential risk of nerve injury in open procedures.4, 5 Reconstructions are still preferred rather than repairs for posterolateral instability.10 Despite the arthroscopic techniques that have been developed over the last 2 years, the tendency has not significantly changed.6, 7 However, the use of native material in arthroscopic posterolateral instability treatment has been reported by Ohnishi et al.8 Creating an arthroscopic portal on the lateral side of the knee (midlateral portal) was the key to achieving better access for PLC structures and to using PLT as a native material in posterolateral instability treatment. From the biological point of view, using a vascularized tendon presented in the knee joint accelerates the healing process and provides material with the most natural toughness. Moreover, PLT tenodesis in our technique is performed at tibia in the point described by Frosch et al.7 for his technique called popliteus bypass graft. This place of fixation with simultaneous preservation of the femoral attachment of PLT makes arthroscopic PLC stabilization with popliteus tenodesis the most anatomical treatment option for posterolateral knee instability which has ever been reported in the literature. In opposition to the proposition of Serra Cruz et al. and Frosch et al., the distal portion of the tibial tunnel is located medially in our technique, below the pes anserinus.4, 7 Another advantage is that there is no need for graft harvesting, which always creates a potential risk of graft place complaints. In addition, the material for future reconstructions has been preserved. The presented procedure is very efficient and reproducible and does not exhaust other treatment options for posterolateral instability of the knee. The recurrence of instability has not been reported yet.
The presented technique can be applied only in the knee with full range of motion. Due to the fact that the whole procedure is performed with the knee in full extension, each extension deficit can make the proper visualization of PLC structures impossible and limit precise instruments maneuvers. It is also worth noting that in general the procedure is very safe, but a possible risk of PLT or lateral meniscus injury exists when not enough attention is paid to the creation of the midlateral portal. Although arthroscopic PLC stabilization with popliteus tenodesis allows restoration of the static function of the popliteus complex, the dynamic function has been irreversibly lost. Furthermore, the popliteofibular ligament is not directly reconstructed in this technique. Its function is restored by proper positioning of PLT tenodesis. As with any other technique, the presented technique does not allow the possibility to recreate the connection between the lateral meniscus and popliteus complex. Pain in the place of tenodesis has been reported by a few patients shortly after surgery, but it has resolved over time. SutureButton use for tibial fixation may also cause minor discomfort. Despite its minimal invasiveness, complications such as wound infection or deep vein thrombosis can occur. This technique cannot be applied when the femoral attachment of PLT is damaged. Table 1 summarizes the advantages and disadvantages of arthroscopic PLC stabilization with popliteus tenodesis.
Table 1.
Advantages and Disadvantages of Arthroscopic Posterolateral Corner Stabilization with Popliteus Tendon Tenodesis
| Advantages | Disadvantages |
|---|---|
| Minimally invasive technique | Loss of popliteus dynamic function |
| No risk of common peroneal nerve injury | Pain in site of tenodesis (resolves over time) |
| Native, vascularized, strength material presented in the knee joint—biological benefit | Recreation of connections between popliteus complex and lateral meniscus is not possible. |
| Anatomical repair technique (natural femoral attachment preserved)—biomechanical benefit | In higher grade posterolateral corner injuries, lateral collateral ligament reconstruction is required. |
| Restoration of popliteus tendon static function | No reconstruction of popliteofibular ligament |
| No exhaustion of graft materials | Application of technique limited by knee extension deficit |
| Cost-effective method | Possibility of popliteus tendon or lateral meniscus injury during midlateral portal creation |
| Reproducible/easy revision No exhaustion of other treatment options |
Arthroscopic PLT tenodesis can be applied in isolated posterolateral instability as well as in cases with combined ligaments lesions. When LCL is significantly injured, there is a need for additional anatomical LCL reconstruction to achieve full stability.11, 12 It is also very important to treat cartilage or meniscus lesions and concomitant anterior cruciate ligament or PCL tears in a one-step procedure with arthroscopic popliteus tenodesis.13
Footnotes
All authors receive support from Arthrex in the form of human cadaver specimens. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic posterolateral corner stabilization with popliteus tenodesis in the left knee joint. During surgery, the patient is placed in the supine position. Three arthroscopic portals are used—anterolateral, anteromedial, and midlateral portal. The midlateral portal is located 1.5 cm above the fibular head and 1 cm anterior to the lateral collateral ligament and is created under visual control. Almost all of the procedure is performed with the knee in full extension. The arthroscopic hook probe is used to identify posterolateral corner structures. The approach for the suture passer is created with Pean's forceps. The Scorpion suture passer is used to pass the FiberTape around the PLT at the level of the planned site for tenodesis. The proximal part of the tibial popliteal marking hook is positioned in the proper place, whereas the 3.5-mm drill sleeve for FlipCutter is placed just below the pes anserinus and a small skin incision is created. The FlipCutter is used to drill through the tibia. When the posterior cortex is drilled, the instrument and aiming guide are removed. Then the tibial tunnel is drilled retrogradely at a depth of 2 cm. The FiberStick with passing sutures is used to retrieve the FiberTape through the tibial tunnel and introduce the popliteus tendon into the tibial tunnel. The tenodesis is assessed. The FiberTape is knotted to a TightRope ABS Button on the anteromedial cortex with the knee flexed to 90°, and the tension of tenodesis is regulated by twisting the SutureButton under arthroscopic control until the drive-through sign and elevation of lateral meniscus are eliminated.
References
- 1.Crespo B., James E.W., Metsavaht L., LaPrade R.F. Injuries to posterolateral corner of the knee: A comprehensive review from anatomy to surgical treatment. Rev Bras Ortop. 2014;50:363–370. doi: 10.1016/j.rboe.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Laprade R.F., Wentorf F.A., Olson E.J., Carlson C.S. An in vivo injury model of posterolateral knee instability. Am J Sports Med. 2006;34:1313–1321. doi: 10.1177/0363546506286785. [DOI] [PubMed] [Google Scholar]
- 3.Shon O.J., Park J.W., Kim B.J. Current concepts of posterolateral corner injuries of the knee. Knee Surg Relat Res. 2017;29:256–268. doi: 10.5792/ksrr.16.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Serra Cruz R., Mitchell J.J., Dean C.S., Chahla J., Moatshe G., LaPrade R.F. Anatomic posterolateral corner reconstruction. Arthrosc Tech. 2016;5:e563–572. doi: 10.1016/j.eats.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zantop T., Petersen W. Modified Larson technique for posterolateral corner reconstruction of the knee. Oper Orthop Traumatol. 2010;22:373–386. doi: 10.1007/s00064-010-9030-9. [DOI] [PubMed] [Google Scholar]
- 6.Frosch K.H., Akoto R., Heitmann M., Enderle E., Giannakos A., Preiss A. Arthroscopic reconstruction of the popliteus complex: Accuracy and reproducibility of a new surgical technique. Knee Surg Sports Traumatol Arthrosc. 2015;23:3114–3120. doi: 10.1007/s00167-014-3000-y. [DOI] [PubMed] [Google Scholar]
- 7.Frosch K.H., Akoto R., Drenck T., Heitmann M., Pahl C., Preiss A. Arthroscopic popliteus bypass graft for posterolateral instabilities of the knee: A new surgical technique. Oper Orthop Traumatol. 2016;28:193–203. doi: 10.1007/s00064-015-0432-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ohnishi Y., Pascual-Garrido C., Kumagae H., Sakai A., Uchida S. Arthroscopic technique for isolated posterolateral rotational instability of the knee. Arthrosc Tech. 2017;6:e291–e295. doi: 10.1016/j.eats.2016.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fanelli G.C., Larson R.V. Practical management of posterolateral instability of the knee. Arthroscopy. 2002;18(2 Suppl 1):1–8. doi: 10.1053/jars.2002.31779. Review. [DOI] [PubMed] [Google Scholar]
- 10.McCarthy M., Ridley T.J., Bollier M., Cook S., Wolf B., Amendola A. Posterolateral knee reconstruction versus repair. Iowa Orthop J. 2015;35:20–25. [PMC free article] [PubMed] [Google Scholar]
- 11.Murgier J., Boisrenoult P., Steltzlen C., Beaufils P., Pujol N. Anatomical knee postero-lateral corner reconstruction: The "Versailles" technique. Orthop Traumatol Surg Res. 2017;103:1031–1034. doi: 10.1016/j.otsr.2017.05.026. [DOI] [PubMed] [Google Scholar]
- 12.LaPrade R.F., Johansen S., Engebretsen L. Outcomes of an anatomic posterolateral knee reconstruction: Surgical technique. J Bone Joint Surg Am. 2011;93(Suppl 1):10–20. doi: 10.2106/JBJS.J.01243. [DOI] [PubMed] [Google Scholar]
- 13.Bonanzinga T., Zaffagnini S., Grassi A., Marcheggiani Muccioli G.M., Neri M.P., Marcacci M. Management of combined anterior cruciate ligament-posterolateral corner tears: A systematic review. Am J Sports Med. 2014;42:1496–1503. doi: 10.1177/0363546513507555. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic posterolateral corner stabilization with popliteus tenodesis in the left knee joint. During surgery, the patient is placed in the supine position. Three arthroscopic portals are used—anterolateral, anteromedial, and midlateral portal. The midlateral portal is located 1.5 cm above the fibular head and 1 cm anterior to the lateral collateral ligament and is created under visual control. Almost all of the procedure is performed with the knee in full extension. The arthroscopic hook probe is used to identify posterolateral corner structures. The approach for the suture passer is created with Pean's forceps. The Scorpion suture passer is used to pass the FiberTape around the PLT at the level of the planned site for tenodesis. The proximal part of the tibial popliteal marking hook is positioned in the proper place, whereas the 3.5-mm drill sleeve for FlipCutter is placed just below the pes anserinus and a small skin incision is created. The FlipCutter is used to drill through the tibia. When the posterior cortex is drilled, the instrument and aiming guide are removed. Then the tibial tunnel is drilled retrogradely at a depth of 2 cm. The FiberStick with passing sutures is used to retrieve the FiberTape through the tibial tunnel and introduce the popliteus tendon into the tibial tunnel. The tenodesis is assessed. The FiberTape is knotted to a TightRope ABS Button on the anteromedial cortex with the knee flexed to 90°, and the tension of tenodesis is regulated by twisting the SutureButton under arthroscopic control until the drive-through sign and elevation of lateral meniscus are eliminated.