Abstract
PURPOSE: To evaluate the management and outcomes of naïve bilateral retinoblastoma treated at a single-center over a 5-year period during the era of ophthalmic artery chemosurgery (OAC) and intravitreous chemotherapy. METHODS: Retrospective cohort study of 46 patients (92 eyes) with naïve bilateral retinoblastoma treated at Memorial Sloan Kettering Cancer Center between January 2012 and February 2017. Indirect ophthalmoscopy, fundus photography, ultrasonography, and ultrasonic biomicroscopy were used to evaluate clinical response. Patient, ocular, ocular progression-free, ocular recurrent event–free, and second ocular survivals were assessed by Kaplan-Meier estimates. Retinal toxicity was evaluated by electroretinography. Snellen visual acuity and complete blood count metrics were recorded. RESULTS: Sixty-four eyes (70%) in 41 patients (89%) received ophthalmic artery chemosurgery as part of their treatment. Twenty-six patients (56%) received tandem OAC (bilateral simultaneous infusions). Seven eyes were primarily enucleated. No eye receiving initial OAC was enucleated. There was a single secondary enucleation in an eye initially treated with focal therapy with anterior chamber recurrence. The 3-year Kaplan-Meier estimates for overall ocular, secondary ocular (survival after treatment for recurrence), progression-free, and recurrent event–free survival were 91.3% [95% confidence interval (CI) 83.4-95.5], 98.7% (95% CI 91.3-99.8), 91.5% (95% CI 83.0-95.8), and 78.9% (95% CI 68.2-86.3), respectively. Overall and secondary ocular survivals were 100% for International Classification of Retinoblastoma (ICRB) groups A-C. Overall ocular survival was 91.5% (95% CI 70-97.8) for ICRB group D and 71.4% (95% CI 47.1-79.4) for group E. Secondary ocular survival was 95.4% (95% CI 71.8-99.3) for ICRB group D and 100% for group E. There were no treatment-related deaths, three patients developed trilateral retinoblastoma (one died), and one patient (who did not receive OAC) developed metastatic disease and is in remission at 32-month follow-up. CONCLUSION: The majority (89%) of bilateral retinoblastoma patients in the current era and at this center were treated with OAC. This has resulted in saving a historic number of eyes. A quarter of eyes developed recurrent disease (defined as recurrent disease requiring any treatment including focal), the majority of which occurred in the first year after treatment, and all but one was saved. There has been no compromise in patient survival.
Abbreviations: SPMs, second primary malignancies; EBR, external beam radiation; OAC, ophthalmic artery chemosurgery; ERG, electroretinogram; PFS, progression-free survival (an event included any treatment with enucleation, external beam radiation and OAC following completion of initial treatment and was calculated from the initial treatment date); ReFS, recurrent event–free survival (an event was defined as recurrence if receiving any treatment, including focal. and calculated from the end date of the initial treatment to date of recurrence diagnosis)
Introduction
Retinoblastoma involving both eyes occurs in a third of patients, is accompanied by a germline RB1 mutation, and is uniquely devastating. Patients are at risk for potentially losing both eyes and losing vision in both eyes, and unlike the majority of unilateral patients, they are at increased risk for second primary malignancies (SPMs) and having children with the disease. These factors have influenced how the management of bilateral retinoblastoma has evolved over decades and continues to change at present (Table 1) [[1], [2], [3], [4], [5], [6], [7], [8], [9], [10]].
Table 1.
Published, Historical Data for Naïve Bilateral Retinoblastoma
| Author | Year | Subjects | No. Pts. | No. Eyes | Treatment | Patient Survival | Overall OS | Primary Enuc | Secondary OS |
|---|---|---|---|---|---|---|---|---|---|
| Reese | 1949 | bl | 53 | 106 | enuc advanced, EBR less advanced | 41/53 (77%) | 43/106 (41%) | 53/106 (50%) | 40/53 (75%) |
| Abramson | 1979 | bl | 24 | 48 | bl enuc | 19/24 (80%) | 0% | 48/48 (100%) | 0% |
| Gagnon | 1980 | bl | 25 | 50 | enuc advanced, EBR if less advanced | 67.6% at 5 yrs | 22/50 (44%) | 22/50 (50%) | 22/28 (79%) |
| Abramson | 1981 | RE IV or V | 32 | 64 | bilateral EBR | 28/32 (88%) | 19/64 (30%) | NR | 19/64 (30%) |
| Abramson | 1981 | RE I to III | 37 | 74 | bilateral EBR | 30/32 (94%) | 63/74 (85%) | NR | 63/74 (85%) |
| Haye | 1987 | bl rb eye RE V) | 33 | 66 | systemic chemo, EBR | 15/23 (63%) | NR | 18/66 (27%) | 7/21 (33%) |
| Kingston | 1996 | RE V | 14 | 28 | systemic chemo, EBR | 12/14 (86%) | 17/28 (61%) | 4/28 (14%) | 17/24 (71%) |
| Gallie | 1996 | bl | 31 | 62 | chemoreduction | 30/31 (97%) | 38/62 (61%) | 22/62 (35%) | 38/40 (95%) |
| Lee | 2003 | bl, one eye enuc | 107 | 107 | systemic chemo, radiation, focal | 100/108 (93%) | 72/214 (34%) | 107/214 (50%) | 72/107 (67%) |
| Sohajda | 2006 | bl, one eye enuc | 13 | 26 | systemic chemo, brachy | 12/13 (93%) | 12/26 (46%) | 13/26 (50%) | 12/13 (93%) |
| Berry | 2013 | bl, only IC D | 49 | 62 | systemic chemo, IMRT, brachy, focal | NR | NA | NA | 45/55 (82%) |
| Francis | 2018 | bl | 46 | 92 | majority OAC | 41/42 (98%) | 84/92 (91%) | 7/92 (7.6%) | 83/84 (99%) |
No., number; Pts., patients; Enuc, enucleation; bl, bilateral; brachy, brachytherapy; IMRT, intense modulated radiation therapy; yrs, years; mos, months; NR, not recorded; NA, insufficient data on fellow eyes.
As treatment modalities for retinoblastoma advance over the decades, centers have reported specifically on how patients with bilateral retinoblastoma fair with contemporary managements. The evolution of these treatments and the outcomes for retinoblastoma patients are summarized in Table 1. Historically, bilateral retinoblastoma was treated with bilateral enucleation, rendering the patient blind and severely impacting quality of life. In 1936, in an effort to improve vision and quality of life, Reese et al. introduced the approach of enucleation of the more advanced eye and treatment of the fellow eye with external beam radiation (EBR) [1]. As radiation techniques evolved, some eyes were then treated with simultaneous bilateral radiation [[4], [5], [6], [7], [8], [9], [10], [11]]. Despite no difference in metastatic deaths between double enucleation and bilateral radiation [4], it was later recognized that radiation increased the risk of SPMs (and therefore mortality) in this genetically primed group of patients [12].
Some groups combined systemic chemotherapy with radiation as globe-conserving treatment for the only remaining but advanced eye with the hope of being able to deliver less radiation [5]. Subsequently, systemic chemotherapy alone was used to treat the remaining eye or both eyes in appropriate cases [[6], [7]]. However, chemoreduction was observed to be less efficacious than primary EBR [8]. Besides focal treatments, failed cases often received secondary EBR: an approach that potentially increases the SPM risk from combination chemotherapy and radiation. Furthermore, the toxic effects of systemic chemotherapy (myelosuppression, ototoxicity, and secondary malignancies) made it a less attractive treatment option. Ototoxicity would be particularly devastating in a child afflicted with bilateral disease and impaired vision.
Since May 2006, our center has been treating retinoblastoma patients with ophthalmic artery chemosurgery (OAC), which involves selective catheterization of the ophthalmic artery and focal delivery of chemotherapy. We initially treated single eyes with advanced disease but quickly advanced to simultaneous bilateral OAC (tandem therapy) [13]. Due to the impressive ocular salvage, improved toxicity profile over systemic chemotherapy, and no increased risk for metastatic deaths [14], we have abandoned EBR and multiagent systemic chemotherapy in the treatment of intraocular retinoblastoma (for unilateral or bilateral disease). OAC has become our standard of care for both unilateral and bilateral patients. This study evaluates how the OAC era, along with the introduction of intravitreous chemotherapy in 2012, has influenced the care and outcome of naïve bilateral retinoblastoma patients treated at the Memorial Sloan Kettering Cancer Center (MSKCC).
Methods
This MSKCC Institutional Review Board–approved retrospective study included all bilateral retinoblastoma patients who presented consecutively to MSKCC between January 2012 and July 2016 and had not received any prior treatment. Patients not treated with OAC were included. Included patients required at least 3 months of follow-up by end of study period. Data collection ended February 28 2017. No child was lost to follow up. Informed consent for treatment was obtained for each patient from his/her guardian, caregiver, or parent. The study was Health Insurance Portability and Accountability Act compliant. Research adhered to the tenets of the Declaration of Helsinki.
Ophthalmic artery chemosurgery was given to 64 eyes in a manner previously described [15]. The drug dosages were selected based on the following age-dependent guidelines {Francis:2015wn}: age 3-6 months: melphalan 2.5-3 mg, topotecan 0.3 mg, carboplatin 30 mg; 6-12 months: melphalan 3 mg, topotecan 0.5 mg, carboplatin 30 mg; 1-3 years: melphalan 4 mg, topotecan 1 mg, carboplatin 40 mg; >3 years: melphalan 5 mg, topotecan 1 mg, carboplatin 40 mg; and number of drugs was titrated to the extent of tumor/advancement of disease. The final drug dose and number of drugs depended on additional factors including route of drug administration (via ophthalmic artery versus balloon technique versus middle meningeal), perfusion and distribution of blood vessel, prior response to treatment, and the aim of maintaining cumulative melphalan dose less than 0.4 mg/kg between both eyes (to prevent myelosuppression). Monthly examinations assessed tumor response and the need for additional OAC infusions based on tumor regression.
Radiation exposure potentially increases the risk of SPMs, particularly in genetically primed bilateral retinoblastoma patients. As such, our group takes extra precautions to significantly reduce radiation exposure during the OAC procedure (by using short fluoroscopy times and minimal use of subtraction angiography). As such, our group’s average radiation exposure is 35 to 194 times lower than published doses from other groups [16].
Bridge patients were those less than 3 months of age who received systemic chemotherapy (single-agent carboplatin 18.7 mg/kg in the majority of cases, although vincristine and etoposide were also used; details below) with the intention of receiving subsequent OAC once 3 months of age and body weight of 6 kg were reached. Ten eyes did not require subsequent OAC and were termed partial bridge. The intravitreous (melphalan 30 μg and topotecan 20 μg) and periocular (topotecan 1 mg) injections were performed as previously described [17] and were given to 15 eyes. Periocular topotecan was given to eyes with diffuse seeding that had demonstrated inadequate response to prior intravitreous melphalan alone. Injections were given at a weekly to monthly interval, predominantly based on the patients’ availability (with a trend towards monthly injections if feasible). Eyes with particularly advanced disease or lack of response with melphalan injections alone were given concomitant intravitreous injections of topotecan.
The clinical status was evaluated under anesthesia with indirect ophthalmoscopy, RetCam fundus photography (Clarity, Pleasanton, CA), B-scan ultrasonography (Ellex, Adelaide, Australia), and ultrasonic biomicroscopy (Ellex, Adelaide, Australia). At each subsequent exam, the burden of residual disease was reevaluated, and additional treatments were given if indicated.
Patient data included sex, laterality at diagnosis, age at diagnosis, family history, eye status (salvaged or enucleated), vital status (alive or dead), development of second cancers or metastatic disease, and follow-up time from diagnosis of disease. Tumor data included Reese-Ellsworth (RE) grouping, Children’s Oncology group version of International Classification (IC), and type of tumor recurrence (retinal, subretinal, or vitreous). Treatment data included initial treatment and treatment for recurrent/persistent disease; number of OAC infusions; maximum and cumulative dose of OAC melphalan, topotecan, and carboplatin; route of OAC (>50% via the ophthalmic artery versus other route which includes middle meningeal or balloon); number of intravenous chemotherapy cycles and drugs; number of injections (intravitreous melphalan, intravitreous/periocular topotecan); and focal treatment (laser or cryotherapy). The initial treatment course was defined as a period that included initial treatment without a treatment-free period lasting 3 months or more. Treatments occurring after 3 months from the completion of initial treatment were defined as recurrence or persistence. Recurrence was defined as new tumor activity visible on ophthalmoscopic exam, including regrowth from regressed tumor and/or new subretinal or vitreous seeds. Persistence was defined as stable, noncalcified tumor that demonstrated no new growth but was treated at the clinician’s discretion. A complete blood count was requested after each cycle of OAC or systemic chemotherapy, and considered evaluable if performed within 7 to 14 days, or if grade 3 or 4 toxicity was noted at any time point. There were 94 evaluable cycles. The standard Common Terminology Criteria for Adverse Events version 4.0 was used to grade hematologic toxicity.
Primary outcomes were patient, ocular (overall and secondary), ocular progression-free, and ocular recurrent event–free survival. Secondary outcomes included visual acuity, ocular toxicity (by ERG), systemic toxicity, metastasis, SPMs, and death.
Ocular Toxicity
ERG recordings were obtained during regularly scheduled examination under anesthesia according to an International Society for Clinical Electrophysiology of Vision standard protocol which had been modified to limit anesthesia time, as previously described [18]. Reported here are the response amplitudes to 30-Hz photopic flicker stimulation, which are representative of the full protocol [19]. Electroretinogram responses were analyzed at baseline and at the last follow-up visit. All responses greater that 100 μV were recorded as 100 μV. ERG studies were deemed nonevaluable if the baseline recording amplitudes were not large enough to allow demonstration of ERG reduction over the injection course or if there was no ERG testing performed (due to the absence of an electrophysiologist). ERG was evaluable on 62 eyes.
Statistical Analysis
Categorical variables were summarized using frequency and percent; continuous variables were summarized using median and range. Ocular survival (OS) and disease-free survival were assessed with Kaplan-Meier (KM) estimates. Curves comparisons were evaluated by log-rank (Mantel-Cox) test. For overall OS, an event was defined as primary or secondary enucleation (no eyes received EBR as salvage treatment). For secondary OS, an event was enucleation following failure of or recurrence after initial treatment. For progression-free survival (PFS), an event included any treatment with enucleation, EBR, and OAC following completion of initial treatment and was calculated from the initial treatment date. For recurrent event–free survival (ReFS), an event was defined as recurrence (see above) receiving any treatment, including focal, and calculated from the end date of the initial treatment to date of recurrence diagnosis. Patients were censored at last contact up to February 28, 2017. Analysis was performed with Prism 7 (www.graphpad.com), and a P value < .05 was considered statistically significant.
Results
Ninety-two eyes in 46 patients (63% female, 37% male) were included in the study. Twenty-six percent of patients had a family history of retinoblastoma. The age at diagnosis was 5.48 months (median) and 8.49 months (mean), range 0.33-27.9 months. The follow-up was 38.7 months (median) and 36.5 months (mean), range 6.9-60.9 months. All patients had bilateral disease, but three patients had unilateral disease at presentation. For these three patients, the median age at unilateral diagnosis was 2.6 months (0.6, 2.6, and 6.5 months), and the median age at bilateral diagnosis was 6.9 months (3.6, 6.9, and 12.9 months). RE classifications were group I (10 eyes), group II (8 eyes), group III (19 eyes), group IV (9 eyes), and group V (46 eyes). International Classification of Retinoblastoma (ICRB) classes were A (5 eyes), B (30 eyes), C (12 eyes), D (24 eyes), and E (21 eyes).
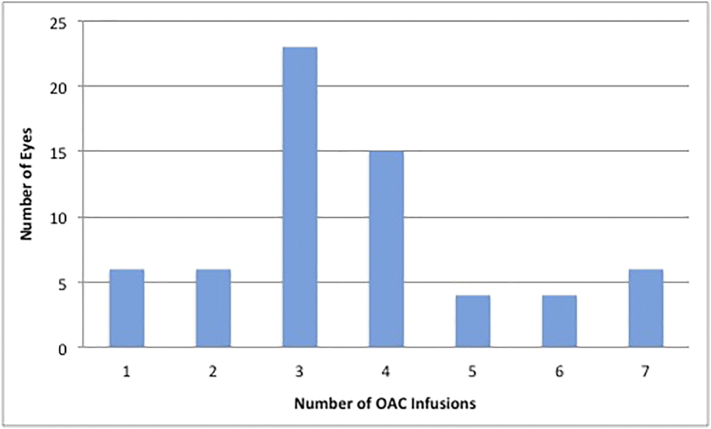
Initial treatment characteristics per eye and per patient are outlined in Table 2. OAC was used as initial treatment in 64 (70%) eyes and 41 (89%) patients. During initial treatment, the number of OAC infusions per eye was 3 (median) and 3.6 (mean), and the number of infusions is depicted in Figure 1. Fifty-two eyes of 26 patients (57%) had tandem therapy (simultaneous bilateral OAC). The ranges of maximum drug doses per infusion were melphalan: 1-7 mg, topotecan: 0.5-2 mg, carboplatin: 30-80 mg. The median cumulative drug doses per weight per eye were melphalan: 0.86 mg/kg, topotecan: 0.27 mg/kg, and carboplatin: 12.7 mg/kg. The median number of days between OAC infusions was 29.9 days (19-62 days). Of the bridge patients, 16 patients received a median of 2 cycles of 18.7 mg/kg carboplatin (range 1-5 cycles). One patient received vincristine with carboplatin for three cycles due to advanced intraocular disease, and one patient received two cycles of carboplatin followed by a third with the addition of vincrinstine due to poor initial tumor response. One patient received carboplatin, vincrinstine, and etoposide because of advanced disease and failed OAC due to a carotid artery anomaly. One patient received systemic chemotherapy due to treatment of concomitant trilateral retinoblastoma.
Table 2.
Initial Treatment Characteristics Per Eye and Per Patient
| Per Eye (n = 92) | Per Patient (n = 46) | ||
|---|---|---|---|
| Bridge | 16 | Bridge | 9 |
| Bridge and intravitreal chemo | 5* | Bridge and intraocular chemo | 5 |
| Partial bridge | 9 | Bridge and plaque | 0 |
| Partial bridge and intraocular chemo | 1 | Partial Bridge | 2 |
| Enucleation | 7 | Enucleation and OAC | 2 |
| OAC | 38 | Enucleation and bridge | 1 |
| OAC and intraocular chemo | 5† | Enucleation and OAC and Ivit | 1 |
| OAC and plaque | 0 | Enucleation and focal | 3 |
| Intraocular chemo | 1 | OAC | 12 |
| Focal | 10 | OAC and intraocular chemo | 4 |
| OAC and plaque | 0 | ||
| OAC and focal | 7 | ||
| Total eyes receiving OAC | 64 | Total patients receiving OAC | 41 |
Two eyes had concomitant periocular chemo.
One eye had concomitant periocular chemo; 1 eye had plaque.
Figure 1.
Chart demonstrating the number of ophthalmic artery chemosurgery infusions per eye given as initial treatment
Progression and Recurrence
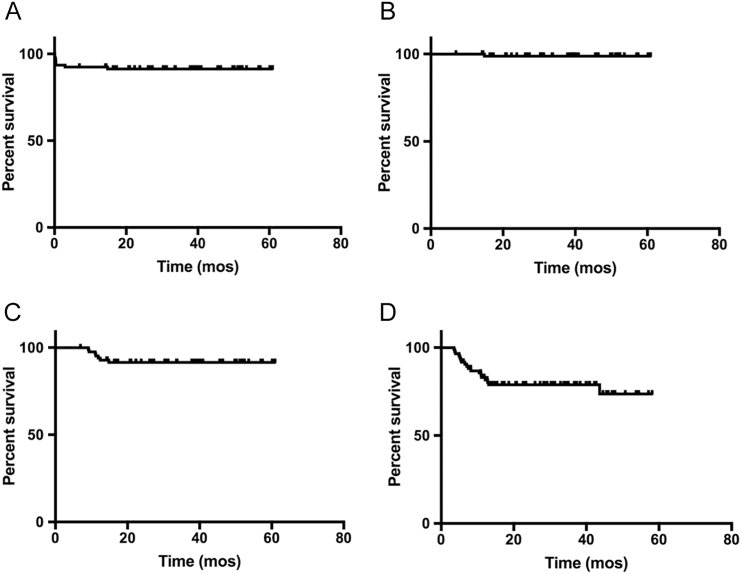
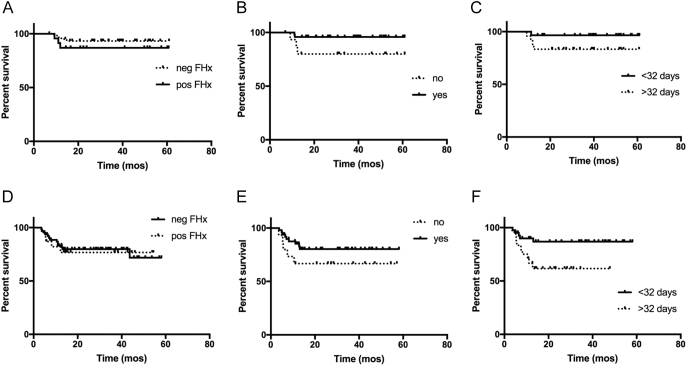
Seventeen eyes had recurrent disease, and 11 eyes had persistence. Fourteen and 8 of these eyes were initially treated with OAC, respectively. Four of four eyes treated with second-course OAC were salvaged. The 36-month KM estimate for PFS was 91.5% [95% confidence interval (CI) 83.0-95.8], and ReFS was 78.9% (95% CI 68.2-86.3); they are shown in Figure 2 and Table 3 by tumor classification. The PFS and ReFS were not statistically different between eyes in patients with positive versus negative family history. PFS was significantly superior (detials) and ReFS was not significant in eyes receiving more than 50% of their infusions via the ophthalmic artery versus other routes (80.4% vs. 66.7%, P value = .2). There was no significant PFS and ReFS in eyes with an interval between OAC infusions of less than 32 days versus greater than 32 days (PFS 96.5% vs. 83.3%, P value = .1 and ReFS 86.8% vs. 61.7%, P value = .02, respectively) (see Figure 3). The types of recurrent disease and number of eyes were retinal: 10, subretinal: 5, retinal and subretinal: 1, vitreous: 0, and other: 1. The treatment types for recurrent disease and number of eyes were focal only: 8, OAC: 5, plaque brachytherapy: 1, periocular chemotherapy :1, plaque/OAC/intravitreous/laser: 1, and enucleation: 1.
Figure 2.
KM estimate survival curves. (A) Overall OS, (B) secondary OS (survival after treatment for recurrent tumor), (C) PFS, and (D) ReFS.
Table 3.
Overall OS, Secondary OS, and Recurrence-Free Survival According to RE Classification and ICRB
| IC | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall OS |
Secondary OS |
PFS |
ReFS |
|||||||||
| n | KM 36 mos | % | n | KM 36 mos | % | n | KM 36 mos | % | n | KM 36 mos | % | |
| A | 5 | 100% | 100% | 5 | 100% | 100% | 5 | 80.0 (95% CI 20.4-96.9) | 80% | 5 | 80.0 (95% CI 20.4-96.9) | 80% |
| B | 30 | 100% | 100% | 30 | 100% | 100% | 30 | 96.6 (95% CI 78-93.6) | 97% | 30 | 80.8 (95% CI 59.5-91.6) | 83% |
| C | 12 | 100% | 100% | 12 | 100% | 100% | 12 | 91.7 (95% CI 53.9-98.8) | 92% | 12 | 75.0 (95% CI 40.8-91.2) | 75% |
| D | 24 | 91.5 (95% CI 70-97.8) | 92% | 23 | 95.4 (95% CI 71.8-99.3) | 96% | 23 | 95.5 (95% CI 71.9-99.4) | 97% | 23 | 81.5 (95% CI 57.7-92.7) | 74% |
| E | 21 | 71.4 (95% CI 47.1 -79.4) | 71% | 15 | 100% | 100% | 15 | 80 (95% CI 50.0-93.1) | 80% | 15 | 73.3 (95% CI 43.6-89.0) | 73% |
| RE Classification | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall OS |
Secondary OS |
PFS |
ReFS |
|||||||||
| n | KM 36 mos | % | n | KM 36 mos | % | n | KM 36 mos | % | n | KM 36 mos | % | |
| I | 10 | 100% | 100% | 10 | 100% | 100% | 10 | 100% | 100% | 10 | 100% | 100% |
| II | 8 | 100% | 100% | 8 | 100% | 100% | 8 | 100% | 100% | 8 | 100% | 100% |
| III | 19 | 100% | 100% | 19 | 100% | 100% | 19 | 82.4 (95% CI 54.8-94) | 84% | 19 | 65.7 (95% CI 48.3-92.7) | 68% |
| IV | 9 | 100% | 100% | 9 | 100% | 100% | 9 | 100% | 100% | 9 | 63.5 (95% CI 23.8-86.6) | 66% |
| V | 46 | 82.6 (95% CI 68.2-90.8) | 83% | 39 | 97.4 (95% CI 83.1-99.6) | 97% | 39 | 89.7 (95% CI 74.9-96) | 87% | 39 | 79.3 (95% CI 62.8-89.1) | 77% |
Figure 3.
KM estimate survival curves. (A) PFS comparing family history status, (B) PFS comparing >50% OAC delivered via ophthalmic artery (yes) compared to other route (no), (C) PFS comparing interval of OAC > or <32 days, (D) ReFS comparing family history status, (E) ReFS comparing >50% OAC delivered via ophthalmic artery (yes) compared to other route (no), and (F) ReFS comparing interval of OAC > or <32 days.
Ocular Survival
Seven eyes were primarily enucleated (7/92=7.6%). Only a single eye had a secondary enucleation (1/92=1%): this eye was initially treated with cryotherapy and developed anterior chamber recurrence. All eyes treated by initial OAC were salvaged.
The 24-month KM estimate of overall OS was 91.3% (95% CI 83.4-95.5) and is shown in Figure 2 and Table 3.
The 24-month KM estimate of secondary OS was 98.7% (95% CI 91.3-99.8) and is shown in Figure 2 and Table 3.
Secondary Outcomes
There was one death from pineoblastoma. Two additional patients developed trilateral retinoblastoma (one pineal, one suprasellar) and were alive at last follow-up. One patient (initially treated by enucleation and focal treatment to the fellow eye) developed metastatic disease and is alive at 32 months following treatment. There were no metastatic deaths.
Fifty eyes had evaluable vision, including 8 cases of enucleation, which were recorded as “no light perception.” Of the remaining 42 eyes, 37 (88%) had macula tumors. Of the 52 eyes, 26 (50%) had vision better than 20/200, and 19 (37%) eyes had vision better than 20/60. Of the 25 patients with evaluable vision, 22 (88%) and 18 (72%) patients had vision better than 20/200 and better than 20/60 in at least one eye, respectively. Comparing between eyes with and without macula tumors, there were no significant difference in vision better than 20/200 (56% vs. 71% of eyes, P = .45) and a trend towards eyes without macula tumors more likely to have vision better than 20/60 compared to those with (80% vs. 36%, P = .06). ICRB-stratified visual acuity per eye is shown in Table 4.
Table 4.
Snellen Visual Acuity of 42 Evaluable, Salvaged Eyes Stratified by ICRB
| Snellen VA | Group A (4 of 5) |
Group B (16 of 30) |
Group C (7 of 12) |
Group D (9 of 24) |
Group E (8 of 21) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Macula | No Macula | Macula | No Macula | Macula | No Macula | Macula | No Macula | Macula | No Macula | |
| <20/200 | 1 | 0 | 5 | 0 | 2 | 0 | 3 | 0 | 5 | 2 |
| 20/60-20/200 | 1 | 0 | 1 | 0 | 3 | 0 | 2 | 0 | 0 | 0 |
| >20/60 | 1 | 1 | 8 | 2 | 2 | 0 | 2 | 2 | 1 | 0 |
Grouping refers to ICRB. VA, visual acuity; Macula, macula tumor present in eye; No Macula, no macula tumor present in eye.
Sixty-two eyes had evaluable ERGs comparing response before and after OAC treatment: 12 (19.4%) had a decrease in response, 34 eyes (54.8%) had stable responses, and 16 eyes (25.8%) had an increase in response.
A total of 28.7% (27 of 94) and 21.3% (20 of 94) of evaluable OAC infusions had grade 3 or 4 hematologic toxic events, respectively; 25.9% (7 of 27) and 20% (4 of 20) occurred in patients receiving bridge OAC. During treatment of their intraocular retinoblastoma (excluding treatment of trilateral or metastatic disease), no patient required blood transfusion of any product, and no patient was treated for chemotherapy-induced fever/neutropenia.
Discussion
There has been a complete change in the management of bilateral retinoblastoma in our center. In Algernon Reese’s (early 1900s) time, patients were managed with bilateral enucleation and then enucleation of one eye and EBR to the fellow eye. Under Robert Ellsworth (mid 1900s), bilateral enucleation became rare, and patients were treated with more focused (higher energy) EBR to one eye and enucleation of the fellow eye and then cautiously bilateral external beam. The introduction of xenon arc photocoagulation, cryotherapy, and plaque brachytherapy enabled some eyes to avoid both enucleation and external beam irradiation. Currently, at our center, initial treatment of naïve bilateral retinoblastoma involves OAC in 89% of patients, which results in historically high ocular salvage rates. In fact, over half the patients (63%) were treated with simultaneous sequential OAC (tandem therapy). The 24-month KM estimate of overall OS (including the 7 eyes primarily enucleated) was 91.3%. Only a single eye was enucleated following recurrence, giving a secondary OS of 98.7%. All eyes initially treated with initial OAC were salvaged even after recurrence. Unlike some systemic chemotherapy protocols [10], EBR was not used in the treatment of or to salvage any eye. These notable results are found in this typical retinoblastoma cohort in which greater than half the eyes were either RE V or IC D or E. In contrast, historical ocular salvage rates range from 0% (bilateral enucleation) to approximately 50% (or 85% in RE I-III only) (Table 1).
Our findings are consistent with prior published data on OAC treatment: that simultaneous tandem OAC results in excellent ocular salvage despite limited melphalan dose to each of the two eyes [13], second-course OAC can successfully treat eyes that have recurred following initial OAC [20], and the addition of intravitreous chemotherapy may account for the high ocular salvage rate and absence of vitreous seed recurrences [21].
We defined recurrence as any new tumor activity requiring additional treatment, including focal therapy. The recurrence rate was similar to our overall OAC cohort [22]: approximately one quarter of eyes had recurrent disease (36-month KM estimate of ReFS 78.9%), with 88% of the events occurring in the first year. Prior literature estimates do not include eyes with regrowth treated by focal therapy alone (nor do they always recognize that most of the Group D/E eyes were primarily enucleated), and therefore, our recurrent event rates cannot be easily compared to the literature.
However, our estimates of PFS are comparable to published definitions in which an event is defined as enucleation or EBR. As a present-day proxy for these, we have also included second-course OAC as an event. In this present study, our 36-month PFS was 91.5%, which is much higher than any published numbers for naïve bilateral retinoblastoma. For example, in a study published within the past 5 years, following treatment with systemic chemotherapy, over half the eyes will develop regrowth of tumor necessitating EBR or enucleation [10]. In the present study, it is to be recalled that all but a single eye were salvaged despite recurrence. We found significantly fewer recurrences in eyes receiving OAC infusions fewer than 32 days apart and statistically fewer progression events in eyes receiving more than 50% of their infusions via the ophthalmic artery versus other routes.
Published reports of naïve bilateral retinoblastoma cohorts have observed metastatic deaths and, as would be expected in germline mutant retinoblastoma, SPMs. Our cohort had no metastatic deaths (one patient who did not receive OAC developed metastatic disease and is alive at 32-month follow-up) and three cases of trilateral retinoblastoma (two alive and one dead). The incidence of pineoblastoma cannot be compared to the literature because published numbers include unilateral germline patients. Like a large collaborative study demonstrated [14], using a management strategy heavily favoring OAC to save children’s eyes does not compromise patient survival.
In describing treatment with systemic chemotherapy, Kingston et al. note that, in their series, bone marrow suppression was toxic, necessitating hospitalization with transfusions or antibiotics “in all children” [6]. On the topic of systemic chemotherapy, Gallie et al. note, “as expected for these chemotherapeutic drugs, neutropenia was common…anemia and thrombocytopenia were common” [7]. However, no specific details are provided. In the 94 evaluable cycles of this study, approximately a quarter had grade 3 neutropenia and a fifth had grade 4 neutropenia, and no child required transfusion of any blood product or treatment for fever/neutropenia. It is difficult to compare these numbers to previous experience without details provided in prior published literature. However, unlike treatment with multiagent systemic chemotherapy, no child receiving OAC required transfusion. In our experience, the risk of vascular damage (either to the eye or to the central nervous system) is exceedingly low, but with any neurointerventional radiology technique, this small risk does exist and should be kept in mind.
When discussing treatment of bilateral retinoblastoma, Reese described four types of failure. Besides death and enucleation due to uncontrolled disease or secondary to treatment toxicity, failure also constituted “patient survival without recurrence but with no useful vision”[1] (although useful vision was not defined). Of 55 patients treated with enucleation and radiation, 25 (47.2%) survived without recurrence and retained useful vision [1]. Despite visual data being limited to children old enough to measure Snellen acuities in the present study, 22 (88%) and 18 (72%) patients had vision >20/200 and >20/60 in at least one eye, respectively. This is remarkable given that the vast majority of eyes (85%) had tumors located in the macula. Clearly, the present treatment of bilateral retinoblastoma saves more eyes and importantly eyes with useful vision.
This study is limited by its retrospective nature and the heterogeneity in the treatment plans, which are tailored to each individual eye. This makes reproducibility of the data difficult. Furthermore, due to the young ages of the patients, final reliable visual acuities are not available for all patients, resulting in a small visual acuity data set which may not fully represent the cohort.
Historically, both eyes were sacrificed in bilateral retinoblastoma. Then methods were used to save at least one eye but at the expense of increased mortality from SPMs (radiation) or increased systemic toxicity (intravenous chemotherapy). Compared to patients with unilateral disease, the era of intraarterial and intravitreous chemotherapy has helped to level the field for bilateral retinoblastoma patients, who are typically at a disadvantage due to the bilateral burden of their disease: patients retain more eyes—importantly, many with useful vision—with no compromise for patient survival. Not only are fewer eyes enucleated at initial presentation but even more eyes are saved by eye-conserving treatment. The results presented here are comparable for patient survival to recently reported cohorts and surpass any historical data for OS. With success in these two measures, the next goal will be to refine treatment with the goal of even superior visual outcomes. Now that the benefits of OAC can be used to advance the management of bilateral retinoblastoma, we invite other centers to present their data and confirm or surpass our findings.
Acknowledgements
This study was supported by The Fund for Ophthalmic Knowledge and Cancer Center Support Grant (P30 CA008748). The sponsor or funding organization had no role in the design or conduct of this research.
References
- 1.Reese AB, Merriam GR, Martin HE. Treatment of bilateral retinoblastoma by irradiation and surgery; report on 15-year results. Am J Ophthalmol. 1949;32:175–190. doi: 10.1016/0002-9394(49)90132-4. [DOI] [PubMed] [Google Scholar]
- 2.Gagnon JD, Ware CM, Moss WT, Stevens KR. Radiation management of bilateral retinoblastoma: the need to preserve vision. Int J Radiat Oncol Biol Phys. 1980;6:669–673. doi: 10.1016/0360-3016(80)90221-7. [DOI] [PubMed] [Google Scholar]
- 3.Abramson DH, Ronner HJ, Ellsworth RM. Second Tumors in Nonirradiated Bilateral Retinoblastoma. Am J Ophthalmol. 1979;87:624–627. doi: 10.1016/0002-9394(79)90293-9. [DOI] [PubMed] [Google Scholar]
- 4.Abramson DH, Ellsworth RM, Tretter P, Adams K, Kitchin FD. Simultaneous Bilateral Radiation for Advanced Bilateral Retinoblastoma. Arch Ophthalmol. 1981;99:1763–1766. doi: 10.1001/archopht.1981.03930020637003. [DOI] [PubMed] [Google Scholar]
- 5.Haye C, Desjardins L, Schlienger P, Zucker JM, Laurent M. Treatment of bilateral retinoblastoma stage V at the Curie Foundation. 33 cases. Ophthalmic Paediatr Genet. 1987;8:73–76. doi: 10.3109/13816818709028520. [DOI] [PubMed] [Google Scholar]
- 6.Kingston JE, Hungerford JL, Madreperla SA, Plowman PN. Results of combined chemotherapy and radiotherapy for advanced intraocular retinoblastoma. Arch Ophthalmol. 1996;114:1339–1343. doi: 10.1001/archopht.1996.01100140539004. [DOI] [PubMed] [Google Scholar]
- 7.Gallie BL, Budning A, DeBoer G, Thiessen JJ, Koren G, Verjee Z, Ling V, Chan HSL. Chemotherapy with focal therapy can cure intraocular retinoblastoma without radiotherapy. Arch Ophthalmol. 1996;114:1321–1328. doi: 10.1001/archopht.1996.01100140521001. [DOI] [PubMed] [Google Scholar]
- 8.Lee V, Hungerford JL, Bunce C, Ahmed F, Kingston JE, Plowman PN. Globe conserving treatment of the only eye in bilateral retinoblastoma. Br J Ophthalmol. 2003;87:1374–1380. doi: 10.1136/bjo.87.11.1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sohajda Z, Damjanovich J, Bárdi E, Szegedi I, Berta A, Kiss C. Combined local treatment and chemotherapy in the management of bilateral retinoblastomas in Hungary. J Pediatr Hematol Oncol. 2006;28:399–401. doi: 10.1097/00043426-200606000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Berry JL, Jubran R, Kim JW, Wong K, Bababeygy SR, Almarzouki H, Lee TC, Murphree AL. Long-term outcomes of Group D eyes in bilateral retinoblastoma patients treated with chemoreduction and low-dose IMRT salvage. Pediatr Blood Cancer. 2013;60:688–693. doi: 10.1002/pbc.24303. [DOI] [PubMed] [Google Scholar]
- 11.Abramson DH, Ellsworth RM, Tretter P, Javitt J, Kitchin FD. Treatment of Bilateral Groups I Through III Retinoblastoma With Bilateral Radiation. Arch Ophthalmol. 1981;99:1761–1762. doi: 10.1001/archopht.1981.03930020635002. [DOI] [PubMed] [Google Scholar]
- 12.Abramson DH, Ellsworth RM, Zimmerman LE. Nonocular cancer in retinoblastoma survivors. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1976;81:454–457. [PubMed] [Google Scholar]
- 13.Abramson DH, Marr BP, Francis JH, Dunkel IJ, Fabius AWM, Brodie SE, Mondesire-Crump I, Gobin YP. Simultaneous Bilateral Ophthalmic Artery Chemosurgery for Bilateral Retinoblastoma (Tandem Therapy) PLoS ONE. 2016;11:e0156806. doi: 10.1371/journal.pone.0156806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abramson DH, Shields CL, Jabbour P, Teixeira LF, Fonseca JRF, Marques MCP, Munier FL, Puccinelli F, Hadjistilianou D, Bracco S. Metastatic deaths in retinoblastoma patients treated with intraarterial chemotherapy (ophthalmic artery chemosurgery) worldwide. Int J Retina Vitreous. 2017;3 doi: 10.1186/s40942-017-0093-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gobin YP, Dunkel IJ, Marr BP, Brodie SE, Abramson DH. Intra-arterial chemotherapy for the management of retinoblastoma: four-year experience. Arch Ophthalmol. 2011;129:732–737. doi: 10.1001/archophthalmol.2011.5. [DOI] [PubMed] [Google Scholar]
- 16.Gobin YP, Rosenstein LM, Marr BP, Brodie SE, Abramson DH. Radiation exposure during intra-arterial chemotherapy for retinoblastoma. Arch Ophthalmol. 2012;130:403–404. doi: 10.1001/archopthalmol.2011.2717. [–authorreply404–5] [DOI] [PubMed] [Google Scholar]
- 17.Francis JH, Brodie SE, Marr B, Zabor EC, Mondesire-Crump I, Abramson DH. Efficacy and Toxicity of Intravitreous Chemotherapy for Retinoblastoma: Four-Year Experience. Ophthalmology. 2017;124:488–495. doi: 10.1016/j.ophtha.2016.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Francis JH, Schaiquevich P, buitrago E, Del Sole MJ, Zapata G, Croxatto JO, Marr BP, Brodie SE, Berra Alejandro, Chantada GL. Local and systemic toxicity of intravitreal melphalan for vitreous seeding in retinoblastoma: a preclinical and clinical study. Ophthalmology. 2014;121:1810–1817. doi: 10.1016/j.ophtha.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 19.Liu CY, Jonna G, Francis JH, Marr BP, Abramson DH, Brodie SE. Non-selectivity of ERG reductions in eyes treated for retinoblastoma. Doc Ophthalmol. 2014;128:13–23. doi: 10.1007/s10633-013-9416-8. [DOI] [PubMed] [Google Scholar]
- 20.Francis JH, Abramson DH, Gobin YP, Marr BP, Tendler I, Brodie SE, Dunkel IJ. Efficacy and toxicity of second-course ophthalmic artery chemosurgery for retinoblastoma. Ophthalmology. 2015;122:1016–1022. doi: 10.1016/j.ophtha.2014.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Francis JH, Iyer S, Gobin YP, Brodie SE, Abramson DH. Retinoblastoma Vitreous Seed Clouds (Class 3): A Comparison of Treatment with Ophthalmic Artery Chemosurgery with or without Intravitreous and Periocular Chemotherapy. Ophthalmology. 2017;124:1548–1555. doi: 10.1016/j.ophtha.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 22.Francis JH, Levin AM, Zabor EC, Gobin YP, Abramson DH. Ten-year experience with ophthalmic artery chemosurgery: Ocular and recurrence-free survival. PLoS ONE. 2018;13 doi: 10.1371/journal.pone.0197081. [DOI] [PMC free article] [PubMed] [Google Scholar]