Abstract
The treatment of articular cartilage lesions in young patients is certainly a complex matter and subject of continuous research, particularly for those located at the patellofemoral joint, given its peculiar biomechanical characteristics. Osteochondral grafts can be of relatively small size when the defect is focal and in an area that allows good stability and consequently the graft's integration. In case of large or multifocal lesions, it is possible to consider an osteochondral transplantation of the entire articular surface of the patella. We present a simple and reproducible technique to perform a patellar fresh osteochondral allograft resurfacing attempting to reduce the symptoms and delay a prosthetic implant in young patients with advanced patellar chondral injuries.
The treatment of articular cartilage lesions in young patients is certainly a complex matter and the focus of continuous research. This is the case for anterior knee pain due to chondral injuries at the patellofemoral joint, given its peculiar biomechanical characteristics.1, 2
In the event of the failure of conservative treatments to alleviate patient symptoms, surgical procedures are a valid alternative. The goal is to correct any abnormality in the patellofemoral kinematics, relieve patellofemoral pressures, and in some cases, to address chondral lesions in accordance with their location, extension, and depth.3
If on one hand we can say that there exists a menu a la carte to follow to approach the various biomechanical alterations and anatomical deformities, we can contrastingly say that the indications for chondral treatment may be more complex. The options at this point range from simple arthroscopic debridement to more invasive procedures such as osteochondral autograft transfer,4 autologous chondrocyte implantation,5 matrix-induced autologous chondrocyte implantation,6 and patellofemoral arthroplasty.7
Osteochondral grafts can be relatively small in size when the defect is focal and situated in a zone that makes for good stability and consequently the graft's integration. In case of large or multifocal lesions, it is possible to consider an osteochondral transplantation of the entire articular surface of the patella.8 Because of the vulnerability of the chondral tissue to standard storage techniques, the option of fresh allografting may become the only reliable alternative in such cases.9 Viable chondrocytes are needed to guarantee the viability of the graft after transplantation.10 This technique shows a logistic limitation as it allows storage for only up to 14 days before transplantation.11, 12
Despite the reticence of many surgeons to propose this type of rescue procedure, we believe that it is a valid option for those with large chondral defects who are still too young for prosthetic joint replacement.
The aim of this study was to present a simple and reproducible way to perform a fresh osteochondral patellar allograft resurfacing (FOPAR) procedure to reduce the symptoms and delay prosthetic solutions in young patients with advanced patellar chondral injuries.
Indication
A FOPAR procedure is indicated in young subjects with an extensive cartilage or osteochondral lesion that cannot be treated with other less aggressive techniques. Only patients with severe chronic pain that limits their daily activities and who see no improvement with conservative treatment are candidates for this option.
The most frequent indication is post-traumatic (patellar fracture) arthritis or osteonecrosis. In addition, cartilage lesions caused by instability can be treated concomitantly with the realignment procedure.
The only absolute local contraindication is advanced osteoarthritis of the knee. Generally speaking, other contraindications are the same as for any tissue transplantation such as infections, tumors, locally aggressive rheumatic disease, and diseases such as diabetes and vasculitis that could negatively affect the integration of the graft.
Relative contraindications are a body mass index higher than 30 as well as patients older than 50 even though a clear age cutoff has not yet been defined. Smoking must be stopped for at least 6 months after surgery.
Fresh Allograft Harvesting and Processing
Routinely, obtaining osteochondral tissue from donors over 45 years old is not recommended. Harvesting of the fresh grafts should not be delayed for more than 12 hours from the moment of death. However, the period can be extended by an extra 12 hours if the donor's body is cooled within the first 4-6 hours of death. The harvested osteochondral allograft is placed into a transport media (lactated Ringer's) and preserved refrigerated (4°C to 8°C) until its reception at the local authorized tissue bank. The preparation and cleaning of the graft, performed in a class A clean room, consist of the evaluation of a cartilage surface, removal of the soft tissue and periosteum, shaping of the graft, and high-pressure pulsatile lavage irrigation with sterile saline. The final graft is subjected to a decontamination process consisting of dry centrifugation and centrifugation with sterile phosphate-buffered saline. Microbiological tests are then performed on both the graft and the last wash solution. Finally, the graft is placed in a preservation solution consisting of lactated Ringer's and an antibiotic cocktail consisting of tobramycin (3 mg/mL), vancomycin (50 mg/mL), amphotericin (125 μg/mL), and cotrimoxazole (160 mg/mL). On the fifth postprocessing day, new microbiological tests are performed on both the graft and the preservation solution. From the day of processing to its implantation, the graft is kept refrigerated (4°C to 8°C). Nowadays, the estimation of the transmissions of the infectious disease is 1 case in 100,000 donations for the hepatitis B virus, 1 in 420,000 donations for the hepatitis C virus, and 1 case in 175,000 donations for human immunodeficiency virus.13
Allograft sizing is performed in accordance with a preoperative computed tomography scan (both in the patient and on the graft), anthropometric agreement between donor and recipient, and Wiberg's classification for the shape of the patella. If possible, it is desirable to have both the patella and the trochlea in the operating room for a more accurate assessment of the shape and congruency of the patella.
Surgical Technique
Positioning
Patients are placed in the supine position with a support for the foot and a lateral support for the thigh to maintain the knee at around 45° of flexion. A thigh tourniquet is used and the contralateral limb is placed in full extension.
Ideally, 2 surgical teams work in parallel to optimize operating times, one to prepare the receiving site and the other to prepare the graft.
Arthroscopic Assessment
An arthroscopic evaluation of all the compartments of the knee is previously performed to reconfirm that FOPAR is a proper indication for the patient. Special attention is paid to ensuring that there are no other trochlear chondral defects that have been overlooked during the preoperative planning. In the scenario of concomitant large trochlear cartilage injuries, a combined transplant of the patellar and trochlear surface can be an option.
Any anatomical deformity or biomechanical alteration of the patellofemoral joint must be corrected to avoid further cartilage degradation of the graft. These corrections may be addressed either in a previous surgery or, preferably, concomitantly with the FOPAR procedure.
Receiving Site Preparation
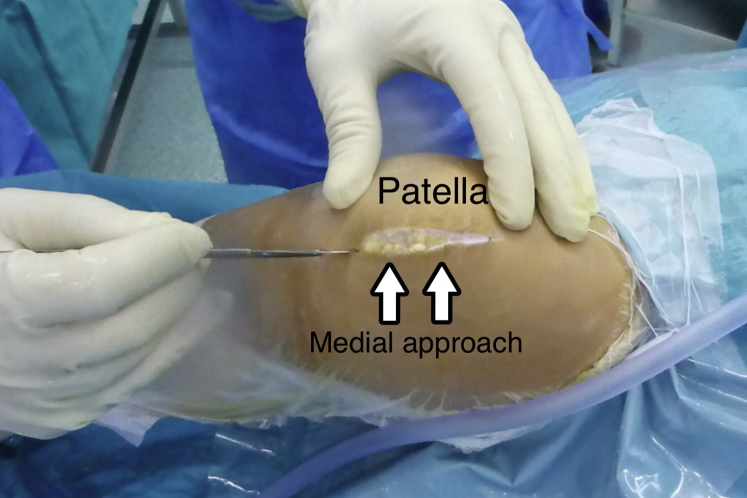
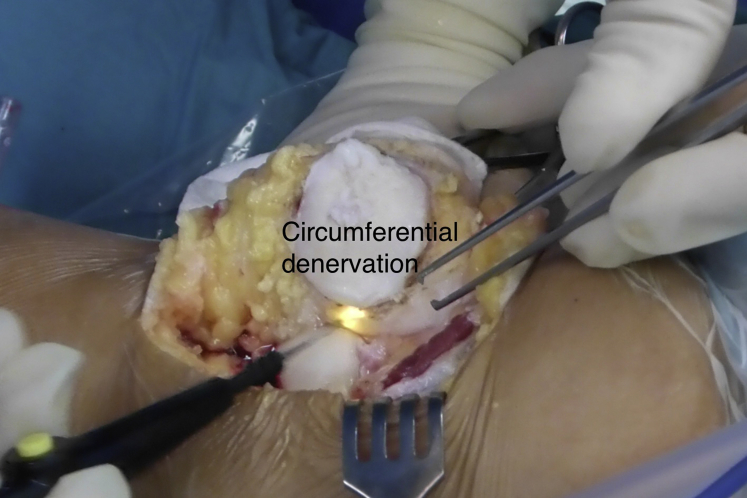
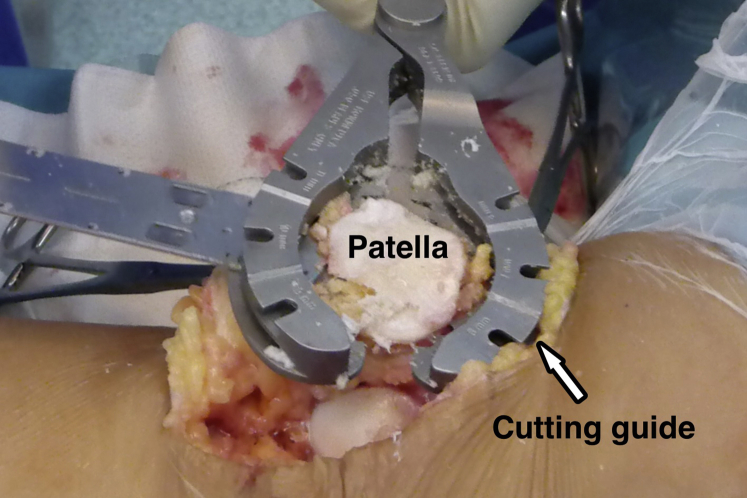
In case of no considerable varus deformity, a standard medial parapatellar approach (Fig 1) or a subvastus approach can be used. Dissection of soft tissues is performed sufficiently enough to allow for patellar eversion, but care is taken not to excessively remove tissue from Hoffa's fat pad because it is a source of vascularization for the knee extensor apparatus. The knee is extended and the patella is kept everted by twisting it with 2 atraumatic clamps at the level of the insertions of the quadriceps and patellar tendons. Careful measurement of the patellar thickness is calculated with a caliper so as to maintain the offset of the patellofemoral joint. Superior-inferior and medial-lateral measures are also assessed to make sure that it matches the donor's sizes and to avoid any instability or pain due to mismatching or overhang. Circumferential denervation of the patella is performed to decrease postoperative anterior knee pain (Fig 2). At this point, the articular side of the patella is resected using a standard patellar guide as those used in total knee arthroplasty (Fig 3). Care is also taken to position the cutting guide to eliminate only 6 to 8 mm of the subchondral bone tissue. This step is of utmost importance because the thicker the bone tissue, the higher the possibility of an immune reaction. In addition, osteochondral integration is accomplished because of a creeping substitution phenomenon only in the first 8 to 12 mm layer of bone tissue.14, 15
Fig 1.
Right knee. A standard short medial parapatellar approach is preferably used. The knee is maintained at around 45° of knee flexion.
Fig 2.
Right knee. Circumferential denervation of the patella is being performed to decrease postoperative anterior knee pain.
Fig 3.
Right knee. Six to eight millimeters of the subchondral bone is removed with the help of a standard patellar guide.
Donor Graft Preparation
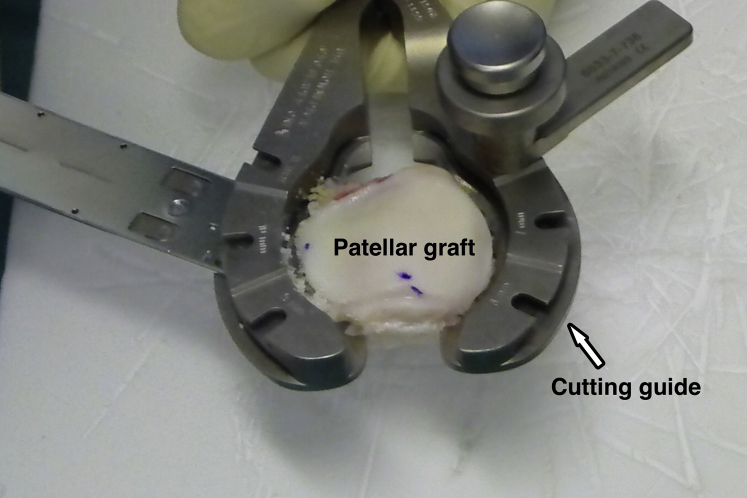
The graft is first warmed up at room temperature. It is then inspected to make sure that there is no macroscopic damage. With the same cutting guide and saws used to prepare the receiving site, the graft is cut (Fig 4) so as to obtain a final patellar thickness that matches the original patellar thickness (Fig 5). The goal is to maintain the patellofemoral offset. Significant attention should be given to removing all the remaining soft tissues to minimize any potential immunologic reaction. Finally, the graft is washed with a high-pressure pulsate irrigation system with saline solution (Fig 6). This also eliminates any trace of blood to reduce any possible immunogenic load and possible septic complications. Lavage is performed for at least 20 minutes. With a sterile skin marker, a mark is made at the proximal and lateral part of the graft to help in its proper placement. If the graft should fall on the floor, by any chance, we recommend a new washing process with high-pressure pulsatile lavage irrigation for no less than 20 minutes with subsequent immersion in a 1 g/100 mL vancomycin solution for 10 minutes.
Fig 4.
The patellar graft is being prepared with the help of a standard patellar guide. The thickness of the fresh allograft should be between 8 mm and 12 mm.
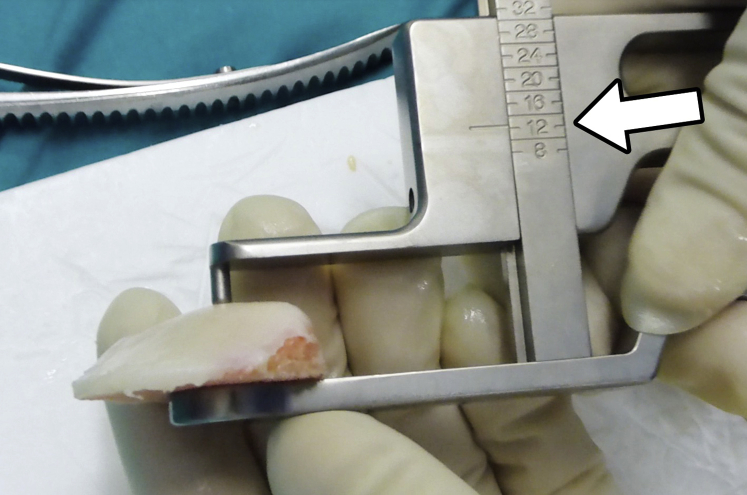
Fig 5.
Using a caliper, measure the thickness of the graft. The graft, together with the remaining host patella, must match the original patellar thickness.
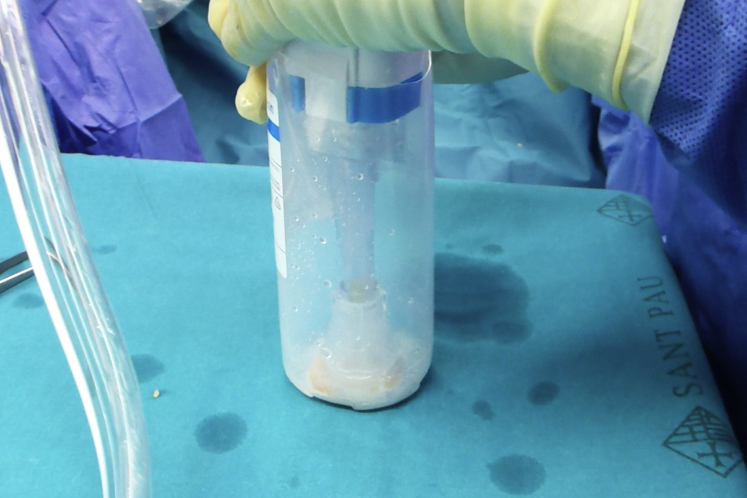
Fig 6.
The graft is generously washed with a high-pressure pulsate irrigation system with saline solution to decrease its immunogenicity. The graft is placed at the bottom of a long plastic recipient to help the washing procedure.
Graft Placement
Once the most appropriate position for the transplant is determined visually, it is advisable to temporally fix it with two to three 1.8-mm Kirschner wires positioned on the dorsal aspect of the patella (anterior to posterior) while taking care to avoid cartilage tissue piercing (Fig 7). At this point, the patellofemoral tracking is tested. If it is satisfactory, final fixation of the graft can be carried out. The authors suggest using 1.5-mm absorbable pins (SmartNail; Conmed, Largo, FL) positioned anterogradely through the cartilage surface (from posterior to anterior) as graft thickness is limited and it also allows for postoperative magnetic resonance imaging evaluation (Fig 8). Alternatively, fixation from the dorsal aspect of the patella with small metal screws can also be performed. Four absorbable pins at the level of each corner of the patella are recommended to give proper stability without damaging the cartilage surface implicated in gliding over the trochlear groove. Once the graft is fixed, the Kirschner wires are removed and the patellofemoral tracking and the implant stability are tested again. The approach is closed with special attention paid to respecting the synovial and the capsular layer. The vastus medialis muscle may be partially advanced over the patella to decrease lateral facet pressure. A step-by-step description of the surgical technique is summarized in Table 1. Table 2 provides pearls and pitfalls to performing this procedure. Video 1 shows the whole technique in detail.
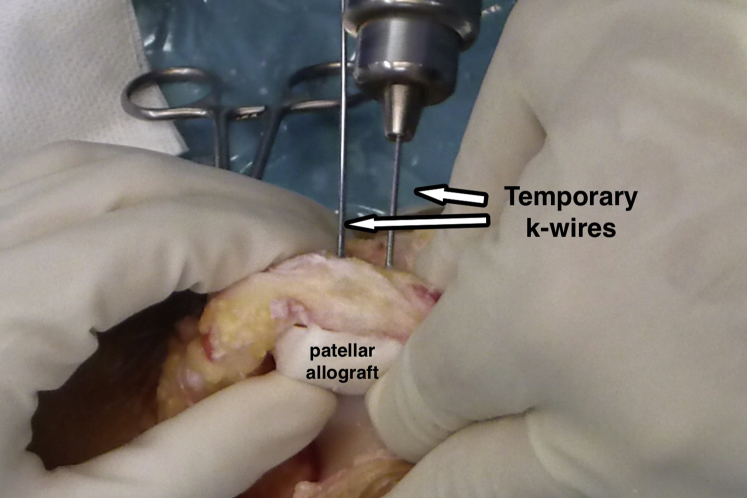
Fig 7.
Right knee. The graft is temporally fixed with two 1.8-mm Kirschner wires positioned on the dorsal aspect of the patella (anterior to posterior) while taking care to avoid cartilage tissue perforation.
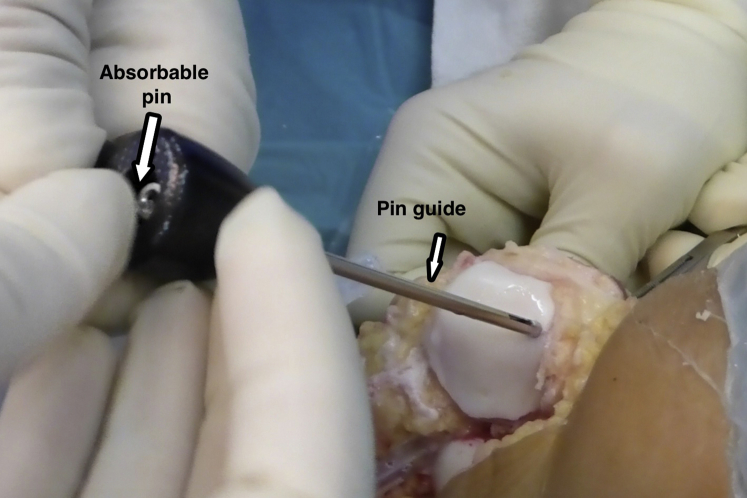
Fig 8.
Right knee. An absorbable pin is being placed from the articular side in the medial aspect of a right patella. Four pins are usually used to reliably fix the graft.
Table 1.
Step-by-Step Fresh Patellar Osteochondral Allograft
| Step | Description |
|---|---|
| 1 | The patient is positioned supine at the operative table, with 90° knee flexion, using a distal foot support and a lateral support for the thigh |
| 2 | A standard medial parapatellar approach or a subvastus approach can be used |
| 3 | The knee is extended and the patella is kept everted by twisting it with 2 atraumatic clamps at the level of the insertions of the quadriceps and patellar tendons |
| 4 | Careful measurement of the patellar thickness is calculated with a caliper so as to maintain the offset of the patellofemoral joint |
| 5 | An osteotomy is performed using a standard patellar guide. Care is also taken to position the cutting guide to eliminate only 6 to 8 mm of the subchondral bone, as the chondral layer is already gone |
| 6 | Circumferential denervation of the patella is performed to decrease postoperative anterior knee pain |
| 7 | The graft is cut to the same thickness as that removed from the patient's patella to maintain patellofemoral offset |
| 8 | Once the most appropriate position for the transplant is determined visually, fix it with two to three 1.8-mm Kirschner wires positioned on the dorsal aspect of the patella (anterior to posterior) while taking care to avoid cartilage tissue perforation |
| 9 | Four absorbable pins at the level of each corner of the patella are suggested to give absolute stability without damaging the cartilage surface implicated in gliding over the trochlear groove. Kirschner wires are then removed |
| 10 | The approach is closed in a usual manner. Vastus medialis muscle may be partially advanced over the patella to decrease lateral facet pressures |
Table 2.
Pearls, Pitfalls, and Risks
|
|
CT, computed tomography.
Rehabilitation Protocol
Controlled continuous passive motion is started within the first hours after the intervention. Full range of movement is allowed from the beginning. Isometric strengthening of the quadriceps and hamstring muscles is also recommended starting from the first days after the graft implantation. Full weight bearing is allowed but only with a brace locked in full extension. The brace is only needed for weight bearing and can be discontinued after 4 weeks. After the first month, rehabilitation focuses on restoring full range of motion and strengthening. Pivoting and strenuous activities are not recommended. Moreover, athletic activity should be limited to light sports. It is imperative that the patient be made aware of such limitations before FOPAR is considered.
Discussion
The treatment of large chondral defects of the patella in young patients works toward techniques that delay prosthetic implantation. Osteochondral patellar allografting is a good and reliable option if we can achieve a high number of vital chondrocytes within the extracellular matrix of the cartilage.16 The lack of chondral tissue vascularization and the hard consistency of its matrix prevents the migration of multipotent cells from the subchondral bone of the host. Thus, a graft with the best chondrocyte viability is the best option.14 It has been shown that cryopreservation damages up to 95% of the chondrocyte, given that the extracellular matrix acts as a barrier for the cryoprotectant. Similarly, a fresh frozen storage technique is not advisable. Thus, fresh allografting is preferred. The downside of fresh allografts is the fact that the osteochondral allograft has to be used within 2 weeks from harvesting and considerable logistics limitations entailed.11, 12 A list including the main advantages and disadvantages of the described technique is shown in Table 3.
Table 3.
Advantages and Limitations
|
|
MRI, magnetic resonance imaging.
Potentially, a FOPAR can lead to some degree of immunoreaction.14, 17 Some tricks and pearls that help to diminish such complications are: (1) careful removal of remnant soft tissue, (2) the use of a high-pressure pulsatile lavage irrigation to eliminate any trace of blood, and (3) transplanting a graft with the least amount of bone possible. A bone layer no thicker than 6 to 10 mm is thus recommended. This is also favorable for bone integration because only this thin layer of bone will be subjected to a necrosis process with subsequent revascularization during the integration progress.14, 15
Although allografting by its own should be sufficient to obtain a good outcome, circumferential denervation of the patella further helps in preventing residual anterior knee pain. Current evidence observed in patellar prosthetic replacement suggests that this denervation reduces pain in the first 12 months.18 This is the period when patients who have undergone a FOPAR procedure are subject to the most important rehabilitation overload. Therefore, the authors suggest associating denervation in this type of surgery with contribution to a pain-free rehabilitation program.
In conclusion, the current technique is a valid option and perhaps the most appropriate nonmetal alternative for invalidating anterior knee pain due to a large cartilage defect of the patella in young patients. Although the technique is not technically demanding, the use of fresh allografts carries considerable logistics limitations.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: P.E.G. is a consultant for CONMED, and receives payment for lectures including service on speakers bureaus from CONMED. J.C.M. has grants/grants pending from Spanish Ministerio de Economia, Industria y Competitividad (National Programme for Research Aimed at the Challenges of Society), and receives payment for lectures including service on speakers bureaus from Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Right knee. All the surgical steps of a fresh patellar osteochondral allograft transplantation are shown in detail. After an arthroscopic examination, a standard short medial parapatellar approach is performed. The allograft is then prepared. It must include the articular cartilage and few millimeters of its subchondral bone. Subsequently, the injured cartilage and around 6mm of subchondral bone is resected from the host patella. Finally, the graft is placed in the recipient area and fixed with 3 to 4 absorbable pins.
References
- 1.Draper C., Bezier T., Gold G., Fredericson M., Fiene A., Beaupre A. Is cartilage thickness different in young subjects with and without patellofemoral pain? Osteoarthritis Cartilage. 2006;14:931–937. doi: 10.1016/j.joca.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 2.Mason J.J., Leszko F., Johnson T., Komistek R.D. Patellofemoral joint forces. J Biomech. 2008;41:2337–2348. doi: 10.1016/j.jbiomech.2008.04.039. [DOI] [PubMed] [Google Scholar]
- 3.Timothy L., Sébastien L., Elvire S., Philippe N. Chondral injury in patellofemoral instability. Cartilage. 2014;5:136–144. doi: 10.1177/1947603514530142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hangody L., Vásárhelyi G., Hangody L.R. Autologous osteochondral grafting—Technique and long-term results. Injury. 2008;39(suppl 1):S32–S39. doi: 10.1016/j.injury.2008.01.041. [DOI] [PubMed] [Google Scholar]
- 5.Niemeyer P., Albrecht D., Andereya S. Autologous chondrocyte implantation (ACI) for cartilage defects of the knee: A guideline by the working group “Clinical Tissue Regeneration” of the German Society of Orthopaedics and Trauma (DGOU) Knee. 2016;23:426–435. doi: 10.1016/j.knee.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Filardo G., Kon E., Andriolo L., Di Martino A., Zaffagnini S., Marcacci M. Treatment of “patellofemoral” cartilage lesions with matrix-assisted autologous chondrocyte transplantation: A comparison of patellar and trochlear lesions. Am J Sports Med. 2014;42:626–634. doi: 10.1177/0363546513510884. [DOI] [PubMed] [Google Scholar]
- 7.Lustig S. Patellofemoral arthroplasty. Orthop Traumatol Surg Res. 2014;100:35–43. doi: 10.1016/j.otsr.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 8.Gracitelli G.C., Meric G., Pulido P.A., Görtz S., De Young A.J., Bugbee W.D. Fresh osteochondral allograft transplantation for isolated patellar cartilage injury. Am J Sports Med. 2015;43:879–884. doi: 10.1177/0363546514564144. [DOI] [PubMed] [Google Scholar]
- 9.Spak R.T., Teitge R.A. Fresh osteochondral allografts for patellofemoral arthritis. Clin Orthop Relat Res. 2006;443:193–200. doi: 10.1097/01.blo.0000201152.98830.ed. [DOI] [PubMed] [Google Scholar]
- 10.Bugbee W.D., Pallante-Kichura A.L., Gortz S., Amiel D., Sah R. Osteochondral allograft transplantation in cartilage repair: Graft storage paradigm, translational models, and clinical applications. J Orthop Res. 2016;34:31–38. doi: 10.1002/jor.22998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schmidt S., Schulte A., Schwarz S. Fresh osteochondral allografts-procurement and tissue donation in Europe. Injury. 2017;48:1296–1301. doi: 10.1016/j.injury.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Williams S.K., Amiel D., Ball S.T. Prolonged storage effects on the articular cartilage of fresh human osteochondral allograft. J Bone Joint Surg Am. 2003;85:2111–2120. doi: 10.2106/00004623-200311000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Zou S., Dodd R.Y., Stramer S.L., Strong D.M., Tissue Safety Study Group Probability of viremia with HBV, HCV, HIV, and HTLV among tissue donors in the United States. N Engl J Med. 2004;351:751–759. doi: 10.1056/NEJMoa032510. [DOI] [PubMed] [Google Scholar]
- 14.De Caro F., Bisicchia S., Amendola A., Ding L. Large fresh osteochondral allografts of the knee: A systematic clinical and basic science review of the literature. Arthroscopy. 2015;31:757–767. doi: 10.1016/j.arthro.2014.11.025. [DOI] [PubMed] [Google Scholar]
- 15.Chui K., Jeys L., Snow M. Knee salvage procedures: The indications, techniques and outcomes of large osteochondral allografts. World J Orthop. 2015;6:340–350. doi: 10.5312/wjo.v6.i3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lattermann C., Kremser V., Altintas B. Use of fresh osteochondral allografts in the patellofemoral joint. J Knee Surg. 2018;31:227–230. doi: 10.1055/s-0037-1607324. [DOI] [PubMed] [Google Scholar]
- 17.Langer F., Czitrom A., Pritzker K.P., Gross A.E. The immunogenicity of fresh and frozen allogeneic bone. J Bone Joint Surg. 1975;57:216–220. [PubMed] [Google Scholar]
- 18.Xie X., Pei F., Huang Z., Tan Z., Yang Z., Kang P. Does patellar denervation reduce post-operative anterior knee pain after total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc. 2015;23:1808–1815. doi: 10.1007/s00167-015-3566-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Right knee. All the surgical steps of a fresh patellar osteochondral allograft transplantation are shown in detail. After an arthroscopic examination, a standard short medial parapatellar approach is performed. The allograft is then prepared. It must include the articular cartilage and few millimeters of its subchondral bone. Subsequently, the injured cartilage and around 6mm of subchondral bone is resected from the host patella. Finally, the graft is placed in the recipient area and fixed with 3 to 4 absorbable pins.