Abstract
Mindfulness has drawn increased attention in prevention programs targeting parents. Commonly, mindfulness-based programs are provided to reduce parental stress and improve child outcomes. Less often, researchers incorporate a mindfulness-informed approach, integrating a low dose of mindfulness exercises into an existing evidence-based parent training model. Little is known about participant engagement with mindfulness exercises in such programs. This non-experimental study focuses on families who are at risk for impaired parenting due to the unique stressor of a parent’s deployment to war. The goal is to examine military parents’ online engagement in mindfulness exercises and associations between engagement and dispositional mindfulness within a web-enhanced parent training program. Online tracking records and self-reported data were obtained from 370 military parents (207 families) who were assigned to the program; at 6-month follow-up, 68.6% of these parents were retained (at least one parent reported from 75.4% of families). Results showed that nearly half (44.6%) of the parents engaged with the exercises. Participants who attended face-to-face group sessions (i.e., attendees) engaged throughout the intervention period whereas participants who never attended group sessions (i.e., non-attendees) mostly engaged during the first month in the program. Attendees and mothers engaged more than non-attendees and fathers. While engaged parents self-reported increased dispositional mindfulness at 6-month follow-up compared to baseline, only mothers’ engagement accounted for a significant proportion of the variance (3%) in dispositional mindfulness at 6-month follow-up, after controlling for covariates. Implications for incorporating online mindfulness exercises into parent training are discussed in the context of programming for military families.
Keywords: mindfulness, parenting, prevention, online, military families
Introduction
Some parents are more in need of parent training as they undergo life stressors. Wartime deployment of a military parent is a unique family stressor that increasingly has garnered attention in the literature. About 2 million children in the United States have been affected by the deployment of a parent to the conflicts in Iraq and Afghanistan since 2001 (Chartrand et al. 2008). Reintegrating military parents are at risk for mental health problems such as posttraumatic stress disorder (PTSD) symptoms (Milliken et al. 2007). Their civilian spouses also show higher rates of mental health problems than civilians who are not partnered with previously deployed military service members (Eaton et al. 2008), and their children are at risk for both emotional and behavioral problems (Chandra et al. 2010; Lester et al. 2010). Given strong evidence that parenting is impaired when families face severe stressors (Forgatch et al. 2013), and that parenting is crucial for children’s adjustment (Collins et al. 2000), there is an urgent need to develop, evaluate, and implement preventive parent training programs for postdeployed military families (Gewirtz et al., 2011; Gewirtz et al. 2017). Studies on mindfulness interventions for military service members exist in the literature (Jha et al. 2010; Kearney et al. 2012); however, none have focused on military parents.
Mindfulness interventions have emerged and proliferated in the parenting sphere (Whittingham 2014). Rooted in Eastern Buddhism, mindfulness is being scientifically investigated in the secular world as a construct related to health and wellbeing. In theory, mindfulness practice may benefit a family system and influence parenting through multiple pathways such as: a) reducing parental stress; (b) reducing parental preoccupation and/negative bias; (c) improving parental executive functioning/reducing reactivity; (d) breaking the cycle of intergenerational continuity of dysfunctional parenting; (e) increasing self-nourishing attention and self-compassion; and (f) reducing marital conflict (Bögels et al. 2010). A growing body of research has provided support for some of these hypotheses. For instance, Bögels et al. (2014) presented evidence that an 8-week mindfulness-based parenting program showed positive effects on parenting style and co-parenting practice in parents who experienced difficulties with their children. In addition, in a randomized controlled trial, Benn et al. (2012) examined a short mindfulness training program (5 weeks) in a sample of parents and educators of children with special needs, showing significant intervention effects on reducing participants’ stress and anxiety, and increasing mindfulness and self-compassion.
The term mindfulness-based is used when mindfulness meditation is a central principle in the program (Crane 2017). For example, in programs such as mindfulness-based stress reduction (MBSR; Kabat-Zinn 1990) or mindfulness-based cognitive therapy (MBCT; Segal et al. 2013), sustained formal and informal in-group and at-home practices of mindfulness play a key role. In the area of parenting, researchers have adopted mindfulness-based programs for parents of children with Attention Deficit Hyperactivity Disorder (Haydicky et al. 2013; Van de Weijer-Bergsma et al. 2012), Autism Spectrum Disorder or other disabilities (Bazzano et al. 2013; Dyken et al. 2014; Singh et al. 2014), developmental delays (Neece 2014; Roberts and Neece 2015), and parents who experience parenting-related difficulties with their typically-developing children (Bögels et al. 2014). Benefits have been shown in reducing parenting stress, psychological stress, and improving mindful parenting and life satisfaction. In contrast, mindfulness-informed programs share some similarities with mindfulness-based programs but are inherently distinctive. Utilizing mindfulness as a skill, mindfulness-informed programs have been developed as part of the “third wave” of psychotherapies, with an emphasis on acceptance and how individuals relate to their experiences. In this sense, they are unlike behavioral therapy (“first wave”) or cognitive therapy (“second wave”) (Crane et al. 2017). Examples of mindfulness-informed programs include Acceptance and Commitment Therapy (ACT; Hayes et al. 2003), Dialectical Behavioral Therapy (Linehan 1987), and Compassion Focused Therapy (Gilbert, 2009).
To summarize, mindfulness-based and mindfulness-informed programs share underpinnings in that they both teach participants to become aware of moment-by-moment experiences while cultivating an accepting, open and compassionate attitude towards the experiences. Both emphasize engaging participants in a range of mindfulness exercises. However, mindfulness-based programs involve meditation practice as a fundamental approach, whereas mindfulness-informed programs typically provide relatively low dose, brief mindfulness exercises for program participants.
Some research has focused on the incorporation of low dose, brief mindfulness exercises into existing evidence-based parent training programs, which are theory-driven and widely-validated. Evidence-based parent training programs have obtained strong empirical support through a series of rigorous testing using randomized controlled trials, and thus are regarded as effective “best-practice” strategies. For some parents, especially those who are stressed or distressed, participating in an evidence-based parent training program with a focus on behavior management may be insufficient to alleviate their stress or distress. Mindfulness may bring transformative changes to parents, children, and their families that are beyond what behavioral parenting strategies produce (Singh et al. 2014). In light of the above, the Mindfulness-Enhanced Strengthening Families Program was developed for adolescent substance use and problem behaviors (Coatsworth et al. 2010; Coatsworth et al. 2015). While the key elements of the Strengthening Families Program (an evidence-based program) were retained, mindful parenting strategies were incorporated to help improve the quality of parent-child interactions. As another example, building upon the Stepping Stones Triple P model (also an evidence-based program), researchers incorporated the core components of ACT into a new program for parents of children with acquired brain injury and cerebral palsy (Brown et al. 2015; Whittingham et al. 2010). Both programs were tested in randomized controlled trials, and the results supported the additive benefits of mindfulness components compared to the original models without mindfulness (Coatsworth et al. 2015; Whittingham et al. 2016). These programs can be considered mindfulness-informed, given the low doses of mindfulness practice included in the program curricula.
In a similar vein, After Deployment Adaptive Parenting Tools (ADAPT; Gewirtz et al. 2017) was developed for postdeployed military parents. The ADAPT program integrates low dose mindfulness exercises (one exercise each week, taught during the group session, lasting 2–20 minutes) into a parent training program. ADAPT was based on the well-validated Parent Management Training-Oregon Model (PMTO) (Forgatch et al. 2013) whose theoretical foundation is Social Interaction Learning (Patterson 2005). Results from randomized controlled trials using intent-to-treat analyses and multi-method, multi-reporter assessment have demonstrated the positive effects of PMTO on preventing child and adolescent behavioral and emotional problems (Forgatch & Gewirtz 2017). The ADAPT curriculum incorporates PMTO’s focus on contingency management in parenting, adding attention to emotional and cognitive processes to improve parental emotion regulation and parents’ emotion coaching of children. Integrating mindfulness into PMTO is ideally suited to the needs of postdeployed military families.
The goals of integrating mindfulness in the ADAPT program are primarily twofold. First, given the literature on mindful emotion regulation (Chiesa and Serretti 2010), mindfulness may help to reduce experiential avoidance (a key concept of ACT; Hayes et al. 2006). Experiential avoidance has been found to predict PTSD symptoms in military service members (Snyder et al. 2016). It also has been correlated with less positive parenting and more observed withdrawal avoidance in deployed fathers (Brockman et al. 2016). For individuals who are at risk for PTSD symptoms, mindfulness may assist them in connecting their feelings and thoughts, promoting acceptance of experiences (the opposite of experiential avoidance). Parents with high levels of dispositional mindfulness can respond to their emotions more effectively, reducing stress, particularly when a child is noncompliant. Consequently, parents may experience more ease in applying behavioral contingencies in parenting (Singh et al. 2014; Snyder et al. 2013). Second, mindfulness exercises may enhance parents’ attunement with their children which further facilitates emotion coaching. Emotion coaching is an important element of the ADAPT program. Parents can coach their children in the world of emotions only if they are aware of both their own and their children’s feelings (Gottman et al. 1996, 1997). Ultimately, parents’ mindfulness provides opportunities for modeling and emotion coaching that helps shape children’s emotional experiences and regulation skills (Snyder et al. 2016).
In the ADAPT program, mindfulness exercises are taught in group sessions but also are accessible through the program’s website. Because the ADAPT program is voluntary and provides a range of parenting tools, parents are likely to vary in their practice. Moreover, group attendance in parent training programs varies widely and is often low (Baker et al. 2011). Thus, digital delivery may serve as a supplementary strategy for boosting behavior change in parents (Breitenstein et al. 2014). It appears that today’s parents with young children are comfortable with and skilled at using the Internet to obtain parenting information they need (Duggan et al. 2015).
Understanding how parents use the Internet to support their parenting is helpful for enhancing the effect of parent training materials delivered online. Related to parents’ use of the Internet and the potential benefits of mindfulness exercises, questions of interest might include: how frequently do parents use online supplemental mindfulness exercises (OSMEs) during their participation in a face-to-face parent training intervention? What is the relationship between group attendance and engagement with OSMEs? Finally, is parents’ engagement in OSMEs associated with dispositional mindfulness? Dispositional mindfulness refers to one’s general capacity to attend to the present moment nonjudgmentally and purposefully, and it has been positively associated with health outcomes and wellbeing (Brown and Ryan 2003). A prior study investigated parents’ engagement patterns in the ADAPT program (Doty et al. 2016), but the study focused on face-to-face group attendance and online engagement in general, with little information gathered about the OSMEs specifically.
The Current Study
We tested three hypotheses. First, we hypothesized that attendees of the face-to-face groups of the ADAPT program would show significantly greater engagement in the OSMEs than non-attendees. Attendees refer to those who attended at least one face-to-face group sessions, and non-attendees refer to those who never attended and would only practice mindfulness in a relatively self-help manner, if at all. We were interested in the assumedly different patterns of engagement across attendees and non-attendees. Second, we tested whether baseline dispositional mindfulness would predict engagement in the OSMEs. We hypothesized that parents would engage more if they had higher levels of baseline dispositional mindfulness. Finally, we focused on the engaged parents and examined the impacts of engagement on levels of dispositional mindfulness at 6-month follow-up. Daily practicing of brief mindfulness exercises was encouraged as part of the home assignment throughout the ADAPT program (Table 1), and we hypothesized that more engagement would be significantly associated with higher levels of dispositional mindfulness at 6-month post-intervention. In the current study, engagement was operationalized as the frequency of “clicks” on the OSMEs, tracked by online data log in real time, which is interpretable as participants’ attempt to practice mindfulness at home.
Table 1.
Face-to-face group topic, in-group mindfulness practice, and OSME home assignment for each session
| ADAPT session | In-group practice | OSME | |
|---|---|---|---|
| 1 | Building Blocks of Resilience | None | None |
| 2 | Encouraging Cooperation | Mindful Eating | Mindful eating Ten deep breaths |
| 3 | Teaching New Behavior | Sitting and Observing | Sitting and observing |
| 4 | Recognizing Emotions | Body Scan | Body scan Notice five things |
| 5 | Responding to Emotions | Leaves on a Stream | Drop Anchor Leaves on a stream Bell Ringing |
| 6 | Setting Limits | Sitting and Observing | Sitting and observing |
| 7 | Follow Through | Hexaflexercise* | Hexaflexercise |
| 8 | Communicating with Children | Wisdom | Hexaflexercise |
| 9 | Problem Solving | Hexaflexercise | Wisdom |
| 10 | Managing Conflict | Loving Kindness | Loving kindness |
| 11 | Monitoring Children | Stretching 1 | Stretching 1 |
| 12 | Promoting School Success | Stretching 2 | Stretching 2 |
| 13 | Linking Home and School | Loving kindness | Loving kindness |
| 14 | Balancing Work and Play | None | None |
Note: ADAPT = After Deployment Adaptive Parenting Tools parenting program; OSME = Online supplemental mindfulness exercises.
Used with permission from Russ Harris.
Method
Participants
This study analyzed data provided by families who had consented to participate in a larger randomized controlled trial evaluating the ADAPT program designed to improve parenting practices and child adjustment among postdeployed National Guard/Reserve families. Only families randomized to the parenting program (i.e. the intervention group) were included in analyses. The sample in the current study consisted of 370 parents from 207 families (M age = 36.79 years, SD = 6.04, range = 24–52). The families had at least one parent who had been deployed overseas to the conflicts in Iraq and Afghanistan since 2001, and at least one child aged 4–12 years at the time they entered the study. The sample was primarily White (91.4%), and approximately half of participants were female (female n = 190). Upon entering the study, most participants (88.3%) were married. The median annual household income of this sample was between $70,000–$79,000. Over half (67.9%) of the sample held an associate’s degree, a bachelor’s degree, or a professional degree, and over one-fifth (23.2%) of the sample had attended some college. Almost all fathers (96.1%) and a minority of mothers (17.4%) had been deployed.
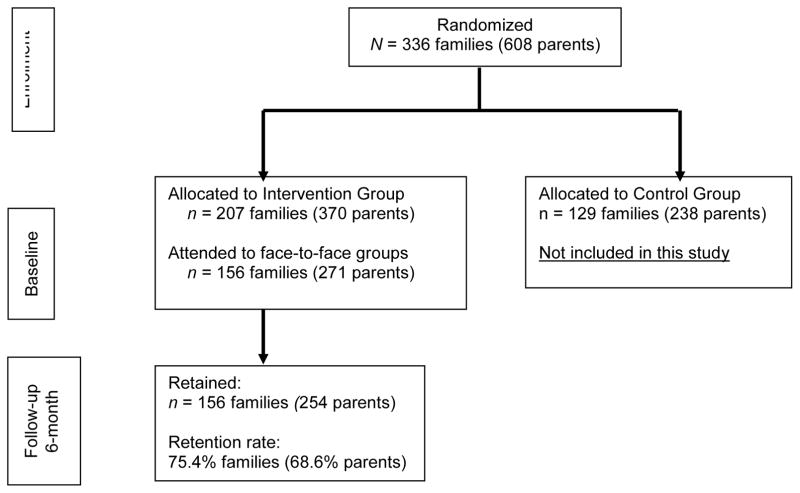
Procedure
A CONSORT diagram is presented in Figure 1. All participants in the intervention group were invited to participate in a 14-session face-to-face group program and were given access to a website that provided supplemental parenting resources including OSMEs, ordered in 14-modules matching the topics of the face-to-face group sessions. The group program lasted 14 weeks on average (range: 12–18 weeks); sessions were postponed for severe weather or holidays. Altogether, 29 face-to-face 14-session groups took place. Each group included 6–15 parents and was led by 2–3 facilitators. The ADAPT parenting group facilitators were human service professionals or trainees, including military personnel and civilians who participated in 10 days of training on the intervention curriculum. They also received ongoing coaching from the principal investigator (the fourth author) and two additional ADAPT/PMTO-certified professionals. They were encouraged to complete an MBSR program and practice mindfulness personally. None of the facilitators were mindfulness teachers. However, two thirds of the ADAPT groups were led by one facilitator who completed an MBSR course, and 90% of the groups were led by at least one facilitator who reported personally practicing mindfulness while facilitating the groups. Lastly, online records indicated that many facilitators were clicking on the OSMEs as well.
Figure 1.
A CONSORT diagram of the ADAPT trial
Each face-to-face group session lasted 2 hours. The teaching of mindfulness and guided meditation was manualized (as was the full program); these exercises typically took up 2–20 minutes of the group time. Each meditation exercise was practiced and debriefed in the group to reinforce the utility and values of being mindful. Participants also received mindfulness-related home practice assignments, which were debriefed at the beginning of next session. A few tips for mindfulness practice were available in the handouts (distributed at face-to-face groups but also available online), including brief instructions such as “practice being mindful or observing when you are doing daily household chores.” Participants were encouraged to follow the order of the online modules to practice mindfulness exercises progressively. Parents were compensated with a $15 gift card for each group session attended to offset travel/gas costs, as well as small incentives for completing online modules.
OSMEs were primarily audio files, with two videos of yoga exercises all available on the ADAPT website (see Table 1 for a list of OSMEs). Brief OSMEs also allowed room for other home practice of behavioral parenting skills assigned by group facilitators, maximizing the likelihood of busy parents finding time to practice, and were consistent with ADAPT’s core message of “small steps to success.”
Measures
Deployment status was dummy-coded as 1 = deployed, 0 = non-deployed.
Group attendance was recorded and computed as a percentage of sessions attended.
OSMEs engagement was measured by the total number of online “clicks” related to OSMEs. The ADAPT supplemental website tracked each time a participant clicked on an OSME. The “clicks” were also labeled by a specific day in real time. Thus, “engaged parents” refer to those who engaged in the OSMEs at least once (engagement≥1). A little over one third (37.2%) of the fathers engaged in the OSMEs, in comparison to over half (51.6%) of mothers.
Dispositional mindfulness was assessed at baseline (prior to the intervention) and follow-up at 6-month post-intervention, shortly after the intervention ended, using the Five Facet Mindfulness Questionnaire (FFMQ; Baer 2006). This scale is based on a factor analysis of items from five preexisting scales that measure mindfulness and enables the measurement of multiple dimensions of mindfulness. Research supports its applicability in different samples, its good internal consistency reliability, and convergent, discriminant, and construct validity (Baer et al. 2008). The five facets are: 1) observing - attending to or noticing internal and external stimuli, such as sensations, emotions, cognitions, sights, sounds, and smells; 2) describing - noting or mentally labeling these stimuli with words; 3) acting with awareness - attending to one’s current actions, as opposed to behaving automatically or absent-mindedly; 4) non-judging of inner experience - refraining from evaluation of one’s sensations, cognitions, and emotions; and 5) non-reactivity to inner experience - allowing thoughts and feelings to come and go, without attention getting caught up in them. The scale has 39 items rated on a 5-point scale (1=never or very rarely true, 5 = very often or always true). The composite scores were used in this study to indicate dispositional mindfulness. Data were collected at two time points: baseline (Cronbach’s α = .89) and follow-up (Cronbach’s α = .92).
Data Analyses
We followed several steps in data analyses. To examine patterns of engagement, frequency of use of OSMEs over 14 weeks was depicted for attendees and non-attendees separately. Next, to examine the relationship between baseline levels of mindfulness and engagement, we used hurdle model for hypothesis testing to address issues related to the excess of zero counts in engagement (a dispersion test indicated significant overdispersion in the data, ps < .001). The excessive zeros suggested that there were likely two types of participants in the sample – the disengaged (i.e., zero counts in engagement) versus the engaged (one or more counts in engagement). Two parts can be estimated in a hurdle model: a logistic part for odds ratio (OR) and a Poisson/negative binomial part for incidence rate ratio (IRR) (Zeileis et al. 2008). We performed hurdle models with Poisson and negative binomial distributions, and used a Vuong test to select the better-fitting model. Group attendance was also included in the hurdle models. Mothers and fathers were tested separately to avoid issues related to nonindependence in the data. Finally, to test whether engagement had an impact on the increased dispositional mindfulness at follow-up among engaged parents, hierarchical multiple regression analyses were performed, while controlling for baseline mindfulness and covariates. A small portion of engaged mothers were deployed so deployment status was included as a covariate; all engaged fathers were deployed. Fathers and mothers were analyzed separately. Of note, we checked the models, and all assumptions of hierarchical multiple regression were met.
Missing data
There were no missing data for the first and second research questions. The FFMQ at 6-month follow-up for engaged parents had non-negligible missing data (12.7%; 21/165 non-respondents). Little’s MCAR test was performed to examine if the missing data were associated with baseline levels of mindfulness, group attendance, parent age, or engagement. The results showed that the data were missing at random, χ2 (4) = 4.04, p = .40. In addition, t tests showed that the missing data were not associated with gender, deployment status, education, annual household income (ps > .05). Thus, for the third hypothesis, list-wise deletion was applied to missing data for reporting results; we also conducted the regressions in Mplus7.4 using Full Information Maximization Likelihood (FIML) to account for missing data to confirm the results.
Results
Out of the total 370 parents, 271 were attendees and 99 were non-attendees of the face-to-face groups (73.2% vs. 26.8%). Among the attendees, 15.9% attended 1–3 sessions, 18.8% attended 4–7 sessions, 24.7% attended 8–10 sessions, and 40.6% attended 11 or more sessions (maximum 14 sessions). In total, parents clicked on OSMEs 2,423 times. Out of the total 370 parents, 165 were engaged parents and 205 did not engage at all (44.6% vs. 55.4%). Gender differences testing showed that mothers engaged in the OSMEs significantly more than fathers, t (359) = −2.86, p < .01, d = .30, in agreement with what has been reported elsewhere (Doty et al. 2016). Engaged fathers were all deployed, and engaged mothers were mostly non-deployed (82.7%). The means and standard deviations for group attendance and OSMEs engagement, stratified by gender and attendee/engagement status, are reported in Table 2. Pearson bivariate correlations were computed, and showed that engagement was significantly associated with parent gender (r = .15, p < .01), and group attendance (r = .27, p < .001); both correlation coefficients were weak. Engagement was marginally associated with deployment status (r = .10, p = .05), although deployment status was confounded with gender. In addition, among engaged parents, a paired t-test showed that parents’ dispositional mindfulness score was significantly higher at follow-up (M = 135.18, SD = 19.13) compared to baseline (M = 129.75, SD = 16.13), t (143) = −4.94, p < .001, d = 0.41.
Table 2.
Descriptive statistics of face-to-face group attendance and online supplemental mindfulness exercise (OSME) engagement
| Variable | Group | N | M | SD |
|---|---|---|---|---|
| Group attendance (%) | All | 370 | 46.06 | 39.99 |
| Father | 180 | 42.90 | 36.69 | |
| Mother | 190 | 49.05 | 37.31 | |
| Father attendee | 126 | 61.28 | 27.77 | |
| Mother attendee | 145 | 64.27 | 29.02 | |
| Engagement | All | 370 | 6.55 | 9.69 |
| Father | 180 | 5.09 | 8.49 | |
| Mother | 190 | 7.93 | 10.55 | |
| Engaged father | 67 | 13.67 | 8.73 | |
| Engaged mother | 98 | 15.38 | 10.06 |
Note: Attendee refers to participants who attended to at least one group session. Engaged father/mother refers to participants who clicked on OSMEs at least once.
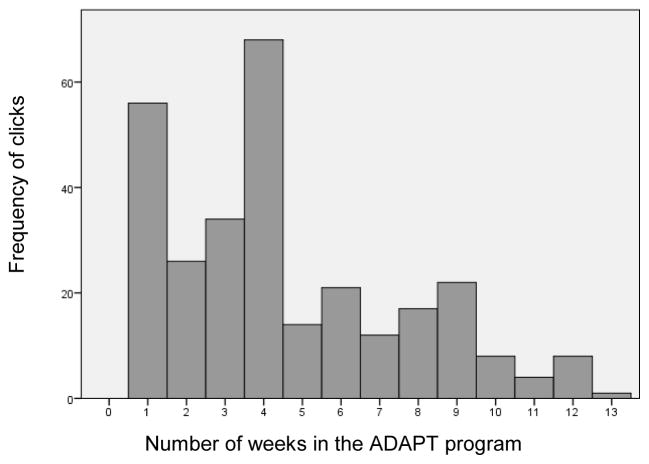
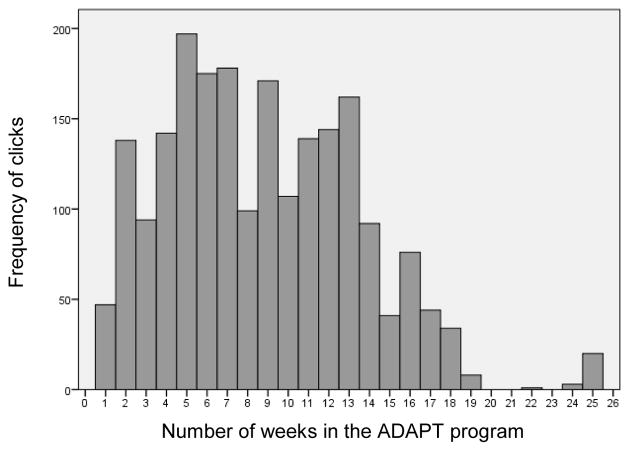
Engagement patterns between non-attendees and attendees were plotted separately, shown in Figure 2 and Figure 3, respectively. Among the non-attendees, OSMEs engagement occurred mostly during the first month of the program but diminished dramatically afterwards. Among the attendees, engagement was highest during the fifth week, and fluctuated while remaining relatively high throughout the program compared to the non-attendees. A small portion of parents also engaged in OSMEs after the 14-week face-to-face program ended. Follow-up t-tests showed that during the first month of the intervention period, non-attendees and attendees did not differ significantly in their average weekly frequencies of use, t (129) = −.48, p = 0.63, which were on average 0.46 clicks (SD = 1.48) for non-attendees and 0.39 clicks (SD = 0.96) for attendees. However, there was a statistically significant difference in average weekly frequencies of use between the two groups during intervention period (i.e., 13 weeks): each week on average non-attendees had 0.23 clicks (SD = 0.58) whereas attendees had 0.51 clicks (SD = 0.70), t (208) = 3.92, p < .001, d = 0.42.
Figure 2.
Frequency of clicking on online supplemental mindfulness exercises per week in non-attendees (n = 99)
Figure 3.
Frequency of clicking on online supplemental mindfulness exercises per week in attendees (n = 271)
We used baseline levels of mindfulness to predict engagement while controlling for group attendance. The results from Vuong tests strongly preferred negative binomial hurdle models (ps< .001). Results showed a trend towards significance between mothers’ baseline levels of mindfulness and the odds ratio of having zero engagement, OR = −.015, Z = −1.66, p = .10. This tentatively suggested that mothers with higher baseline levels of mindfulness would have greater odds ratio of not engaging; however, this effect was only marginally significant and very small. There was no significant relationship between fathers’ baseline levels of mindfulness and engagement (ps > .15).
Focusing on the engaged parents (including both attendees and non-attendees), hierarchical linear regression analyses were conducted to examine if engagement significantly predicted dispositional mindfulness at 6-month follow-up after controlling for baseline mindfulness, deployment status (mothers only), and group attendance. For fathers (Table 3), baseline mindfulness was entered at stage one and significantly predicted dispositional mindfulness at 6-month follow-up, F (1,55) = 101.76, p < .001. Baseline dispositional mindfulness accounted for 65% of the variance in dispositional mindfulness at follow-up. When face-to-face group attendance and engagement were entered in the second and third steps, neither of the models showed significant F change. The results showed that engagement did not significantly predict dispositional mindfulness at 6-month follow-up above and beyond baseline mindfulness and face-to-face group attendance for fathers.
Table 3.
Summary of hierarchical weighted regression analysis predicting dispositional mindfulness at follow-up in fathers (n = 57)
| Model 1 | Model 2 | Model 3 | Pearson Correlations | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| Variable | B | SEB | β | B | SEB | β | B | SEB | β | 1 | 2 | 3 | 4 |
| 1. Baseline FFMQ | 1.10 | .11 | .81*** | 1.10 | .11 | .81*** | 1.10 | .11 | .81*** | 1.00 | −.10 | −.07 | .81*** |
| 2. Attendance | 1.53 | 5.54 | .02 | 1.17 | 5.92 | .02 | 1.00 | −.32** | −.06 | ||||
| 3. OSME engagement | −.04 | .21 | −.02 | 1.00 | −.08 | ||||||||
| R2 | .65 | .65 | .65 | ||||||||||
| ΔR2 | .65 | .00 | .00 | ||||||||||
| F Change | 101.76*** | .08 | .03 | ||||||||||
Note: OSME = Online supplemental mindfulness exercises; FFMQ = Five Facets Mindfulness Questionnaire; 4 = FFMQ at follow-up.
p< .05;
p< .001.
For mothers (Table 4), baseline dispositional mindfulness and military deployment of mothers were entered at stage one to control for effects of exposure to military deployment. The results showed that baseline dispositional mindfulness and military deployment contributed significantly to the regression model, F (2,84) = 39.50, p < .001, and these two predictors accounted for 49% of the variance in dispositional mindfulness at 6-month follow-up in mothers. When group attendance was added in the second step, the model did not show a significant F change. Engagement was entered in the third step and was found to account for an additional 3% of the variance in dispositional mindfulness above and beyond baseline dispositional mindfulness, deployment status, and group attendance in mothers (Cohen’s f2 = .05), F (4, 82) = 21.28, p < .001. The four independent variables combined accounted for 51% of the variance in dispositional mindfulness at 6-month follow-up in mothers.
Table 4.
Summary of hierarchical weighted regression analysis predicting dispositional mindfulness at follow-up in mothers (n = 87)
| Model 1 | Model 2 | Model 3 | Pearson Correlations | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| Variable | B | SEB | β | B | SEB | β | B | SEB | β | 1 | 2 | 3 | 4 | 5 |
| 1. Baseline FFMQ | .77 | .09 | .71*** | .77 | .09 | .71*** | .77 | .09 | .71*** | 1.00 | .35** | −.04 | .04 | .70*** |
| 2. Deployment status | −2.31 | 4.00 | −0.05 | −2.31 | 4.03 | −.05 | −2.98 | 3.97 | −.06 | 1.00 | −.06 | .10 | .20* | |
| 3. Group attendance | .06 | 4.59 | .00 | .81 | 4.52 | .01 | 1.00 | −.09 | −.02 | |||||
| 4. OSMEs engagement | .29 | .14 | .16* | 1.00 | .18* | |||||||||
| R2 | .49 | .49 | .51 | |||||||||||
| ΔR2 | .49 | .00 | .03 | |||||||||||
| F Change | 39.50*** | .00 | 4.12* | |||||||||||
Note: OSME = Online supplemental mindfulness exercises; FFMQ = Five Facets Mindfulness Questionnaire; 5 = FFMQ at follow-up.
p< .05;
p< .001
Discussion
The current study examined parent engagement in online mindfulness exercises within a mindfulness-informed parent training program for postdeployed military families. Understanding how parents interact with online mindfulness exercises provides important information that can inform implementation strategies. Given the obstacles families face in attending in-person parent training programs (Spoth and Redmond 2000), it is important for interventionists to continually strategize new and effective ways to deliver programs and resources to families. Our findings demonstrated differential OSME engagement patterns between parents who attended at least one group sessions (attendees) and their counterparts who never attended (non-attendees). Interestingly, differences only emerged one month into the intervention. Gender and group attendance significantly predicted OSME engagement. To our surprise, parents’ baseline levels of mindfulness was not associated with their engagement. Finally, for mothers only, engagement in OSMEs predicted changes in their dispositional mindfulness score at 6-month follow-up. Parents who attended at least one face-to-face group session, engaged significantly more in the OSMEs throughout the program, compared to non-attendees’ limited engagement during the first month of the intervention. An online format for delivering short mindfulness exercises is likely insufficient to improve mindfulness in the absence of the support, discussion, and practice associated with face-to-face group sessions.
Engagement in a program is typically concerned with enrollment, attendance, and/or retention (Butler and Titus 2015), but it can also be indexed by participants’ practice behaviors (Baydar and Webster-Stratton 2003). In this study, engagement was measured by parents “clicking” on the exercises, which was interpreted as attempts to practice mindfulness. Mothers’ engagement was significantly and positively associated with small but significant increases in dispositional mindfulness 6-month from baseline assessment. There is a well-studied positive relationship between mindfulness home practice and dispositional mindfulness in mindfulness-based programs (Carmody and Baer 2008). What is still lacking is research on this practice-outcome relationship in the context of a parenting program integrating mindfulness into an existing “best-practice” program.
Our findings resonate with those of an earlier study in which online usage of mindfulness exercises significantly predicted small but significant reductions in depressive symptoms following an online Acceptance and Commitment Therapy/ACT program (Van Gemert-Pijnen et al. 2014). Interestingly, in their study, participants’ engagement in online mindfulness exercises decreased significantly over time, whereas in our study, the engagement was somewhat stable throughout the intervention period for attendees. One might argue that this difference is attributable to the ADAPT program including face-to-face group sessions.
Parental deployment places a unique stressor on families, and it has been well-documented that previously deployed service members are at risk for mental health problems such as PTSD, depression, anxiety, and substance use (Hoge et al. 2006; Milliken et al. 2007). Our finding of the engagement-outcome relationship may not be generalizable to mothers from other types of families, as this is a unique parent sample. Regarding the nonsignificant findings in fathers, it is possible that deployed fathers might have not achieved detectable improvements in dispositional mindfulness because of their greater risk for PTSD symptoms than mostly civilian mothers. The goal of incorporating brief, additive mindfulness exercises into the ADAPT curriculum was to assist previously deployed service members to be aware of their thoughts and feelings, to be more present while parenting. However, alleviating experiential avoidance and improving dispositional mindfulness may take longer and/or require more than the short exercises provided within ADAPT. A prior study tested the impact of a mindfulness training adjunct in residential PTSD treatment for veterans, and did not detect a significant improvement in mindfulness (Owen et al. 2012). Mindfulness-informed programs may not be sufficient to improve dispositional mindfulness for this population. Alternatively, more intensive mindfulness-based programs may be more likely to improve mindfulness for previously deployed service members. On the other hand, extended mindfulness exercises are recommended for veterans with PTSD (Vujanovic et al. 2011). More empirical data is needed to inform intervention strategies to help postdeployed military fathers engage in mindfulness practices more effectively.
It is worth noting that our methodological approach contributes to the literature as it is unbiased by self-report measures of online engagement in mindfulness exercises. Engagement was measured with a novel and objective measure – using computer log tracking rather than parents’ self-report to track participants’ attempts to practice the OSMEs. This measure provided a more accurate depiction of the “ebb and flow” of attempted mindfulness practice over time. Because dispositional mindfulness was measured via self-report, we also avoided mono-method bias. To ensure that online “clicks” mean actual practice, future research may improve on this measurement strategy by adding features to track actual practice (e.g. requiring answers to a post-practice question).
How might engagement with OSMEs be sustained in order to strengthen dispositional mindfulness, especially among non-attending parents? We speculate that additional tools to promote interactivity with facilitators and peers (e.g., telehealth options) may help to ensure and sustain mindfulness practice. Research shows that parents are already using multiple technologies to fulfill their parenting goals (Walker and Rudi 2014). Interventionists can apply this information to developing and implementing prevention programming for parents who are already technologically savvy. For example, research shows that of parents who use discussion boards, a majority use them to seek information and advice, and gain support from others (Walker and Rudi 2014). Online-delivered mindfulness exercises within a parent training program could consider incorporating effective, interactive technology tool to mimic the environment parents experience when they attend a face-to-face parenting program.
Regardless of the format being mindfulness-based or mindfulness-informed, dispositional mindfulness is considered a core outcome of engaging in mindfulness exercises. In the literature, some researchers have used different scales to measure dispositional mindfulness (e.g. Parent et al. 2010), or measured state mindfulness instead (such as mindful parenting; Coatsworth et al. 2015). Nonetheless, both dispositional mindfulness and mindful parenting have yielded similar results in associations with child behavior problems and parenting variables (Jones et al. 2014). The integration of mindfulness into a Social Interaction Learning model offers an opportunity to extend knowledge of what constitutes effective parenting (Snyder et al. 2013). Further studies may assess the role of dispositional mindfulness as either a mediator or moderator of theoretically-conceptualized parenting-related intervention outcomes (Harnett and Dawe 2012). For example, the ADAPT program involves teaching parents about emotion-related parenting (or emotion coaching), which may be a correlate of parents’ dispositional mindfulness that warrants further investigations (Snyder et al. 2013).
Limitations
Some limitations of the current study should be emphasized. First, our analyses did not involve an experimental design and thus a causal relationship cannot be drawn between OSMEs engagement and dispositional mindfulness. Future studies should use experimental designs to test this hypothesis, which will inform the identification of different user groups and optimize intervention engagement and outcomes. Second, a small portion of participants were offered additional monetary incentives for online module completion, and we were unable to ascertain how that might have affected our findings. Third, OSMEs data (gathered via software to track clicks on the OSMEs) may or may not indicate mindfulness practice. In addition, we were unable to ascertain whether and to what extent parents downloaded the OSMEs to their MP3 device and used them without going online. Thus, it is unknown to what degree that may impact our conclusions. Fourth, we did not measure whether and to what degree participants were exposed to other mindfulness-related resources online or offline prior to, or concurrent with the intervention. Fifth, while the majority of ADAPT facilitators had completed an MBSR course prior to facilitating ADAPT sessions, it is important to note that facilitators were not experienced meditators. Finally, our findings, particularly those about military fathers, may not be generalizable to other samples.
Despite its limitations, the current study builds upon previous research to examine how parents engage with and benefit from low dose online supplemental mindfulness exercises (OSMEs) in a mindfulness-informed parenting program context using website-logged data. Brief self-paced OSMEs, coupled with persistent engagement, may be an effective strategy to enhance parenting practices and bring psychosocial benefits by enhancing dispositional mindfulness among parents, and mothers in particular. It is assumed that engagement leads to enhanced mindfulness, but the nature of the dose-response relationship is still unknown, particularly in the context of a mindfulness-informed parent training program. Finally, from the perspective of service provision, helping parents to select “bona fide” mindfulness resources and effective mindfulness exercises is important, as parents have concerns about the trustworthiness of online health information (Myers-Walls and Dworkin 2016). This is particularly crucial when interventionists themselves are not meditators, or when parents do not attend to face-to-face group sessions.
Acknowledgments
This study was funded by grants from National Institute of Drug Abuse (R01-DA030114) and U.S. Department of Agriculture, Agriculture Experiment Station (1008164) to Abigail H. Gewirtz. We are thankful to the families who participated in the study.
Footnotes
Ethics and Informed Consent
This study was approved by the Institutional Review Board of the University of Minnesota – Twin Cities. Formal consent was obtained from all participants before the study was conducted.
Author Contributions
NZ: conceptualized the research questions, conducted data analyses, and wrote the paper. JHR: assisted with the conceptualizations, interpretation of results and implications, and writing of the study. OZ: collaborated with the research design and data analyses, and wrote part of the results. AHG: supervised the study and collaborated in the writing and editing of the manuscript.
References
- Baer RA. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, … Williams JMG. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15:329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Baker CN, Arnold DH, Meagher S. Enrollment and attendance in a parent training prevention program for conduct problems. Prevention Science. 2011;12:126–138. doi: 10.1007/s11121-010-0187-0. [DOI] [PubMed] [Google Scholar]
- Baydar N, Reid MJ, Webster- Stratton C. The role of mental health factors and program engagement in the effectiveness of a preventive parenting program for Head Start mothers. Child Development. 2003;74:1433–1453. doi: 10.1111/1467-8624.00616. [DOI] [PubMed] [Google Scholar]
- Bazzano A, Wolfe C, Zylowska L, Wang S, Schuster E, Barrett C, Lehrer D. Mindfulness-Based Stress Reduction (MBSR) for parents and caregivers of individuals with developmental disabilities: A community-based approach. Journal of Child and Family Studies. 2013;24:1–11. doi: 10.1007/s10826-013-9836-9. [DOI] [Google Scholar]
- Benn R, Akiva T, Arel S, Roeser RW. Mindfulness training effects for parents and educators of children with special needs. Developmental Psychology. 2012;48:1476–1487. doi: 10.1037/a0027537. [DOI] [PubMed] [Google Scholar]
- Black DS, Semple RJ, Pokhrel P, Grenard JL. Component processes of executive function—mindfulness, self-control, and working memory—and their relationships with mental and behavioral health. Mindfulness. 2011;2:179–185. doi: 10.1007/s12671-011-0057-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bögels SM, Lehtonen A, Restifo K. Mindful parenting in mental health care. Mindfulness. 2010;1:107–120. doi: 10.1007/s12671-010-0014-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bögels SM, Hellemans J, van Deursen S, Römer M, van der Meulen R. Mindful parenting in mental health care: Effects on parental and child psychopathology, parental stress, parenting, coparenting, and marital functioning. Mindfulness. 2014;5:536–551. doi: 10.1007/s12671-013-0209-7. [DOI] [Google Scholar]
- Breitenstein SM, Gross D, Christophersen R. Digital delivery methods of parenting training interventions: A systematic review. Worldviews on Evidence-Based Nursing. 2014;11:168–176. doi: 10.1111/wvn.12040. [DOI] [PubMed] [Google Scholar]
- Brockman C, Snyder J, Gewirtz A, Gird SR, Quattlebaum J, Schmidt N, … Zettle R. Relationship of service members’ deployment trauma, PTSD symptoms, and experiential avoidance to postdeployment family reengagement. Journal of Family Psychology. 2016;30(1):52–62. doi: 10.1037/fam0000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown FL, Whittingham K, Boyd RN, McKinlay L, Sofronoff K. Does Stepping Stones Triple P plus Acceptance and Commitment Therapy improve parent, couple, and family adjustment following paediatric acquired brain injury? A randomised controlled trial. Behaviour Research and Therapy. 2015;73:58–66. doi: 10.1016/j.brat.2015.07.001. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Butler AM, Titus C. Systematic review of engagement in culturally adapted parent training for disruptive behavior. Journal of Early Intervention. 2015;37:300–318. doi: 10.1177/1053815115620210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmody J, Baer R. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine. 2008;31:23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- Chandra A, Lara-Cinisomo S, Jaycox LH, Tanielian T, Burns RM, Ruder T, Han B. Children on the homefront: The experience of children from military families. Pediatrics. 2010;125(1):16–25. doi: 10.1542/peds.2009-1180. [DOI] [PubMed] [Google Scholar]
- Chartrand MM, Frank DA, White LF, Shope TR. Effect of parents’ wartime deployment on the behavior of young children in military families. Archives of Pediatrics & Adolescent Medicine. 2008;162:1009–1014. doi: 10.1001/archpedi.162.11.1009. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. A systematic review of neurobiological and clinical features of mindfulness meditations. Psychological Medicine. 2010;40:1239–1252. doi: 10.1017/S0033291709991747. [DOI] [PubMed] [Google Scholar]
- Coatsworth JD, Duncan LG, Greenberg MT, Nix RL. Changing parent’s mindfulness, child management skills and relationship quality with their youth: Results from a randomized pilot intervention trial. Journal of Child and Family Studies. 2010;19(2):203–217. doi: 10.1007/s10826-009-9304-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coatsworth JD, Duncan LG, Nix RL, Greenberg MT, Gayles JG, Bamberger KT, … Demi MA. Integrating mindfulness with parent training: effects of the Mindfulness-Enhanced Strengthening Families Program. Developmental Psychology. 2015;51:26–35. doi: 10.1037/a0038212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins WA, Maccoby EE, Steinberg L, Hetherington EM, Bornstein MH. Contemporary research on parenting: The case for nature and nurture. American Psychologist. 2000;55:218–232. doi: 10.1037/0003-066X.55.2.218. [DOI] [PubMed] [Google Scholar]
- Crane RS, Brewer J, Feldman C, Kabat-Zinn J, Santorelli S, Williams JMG, Kuyken W. What defines mindfulness-based programs? The warp and the weft. Psychological Medicine. 2017;47:990–999. doi: 10.1017/S0033291716003317. [DOI] [PubMed] [Google Scholar]
- Crane RS. Implementing mindfulness in the mainstream: Making the path by walking it. Mindfulness. 2017;8:585–594. doi: 10.1007/s12671-016-0632-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doty JL, Rudi JH, Pinna KLM, Hanson SK, Gewirtz AH. If you build it, will they come? Patterns of Internet-based and face-to-face participation in a parenting program for military families. Journal of Medical Internet Research. 2016;18:e169. doi: 10.2196/jmir.4445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan M, Lenhart A, Lampe C, Ellison NB. Parents and social media. 2015 Retrieved from Pew Internet and American Life Project website: http://www.pewinternet.org/2015/07/16/parents-and-social-media/
- Dykens EM, Fisher MH, Taylor JL, Lambert W, Miodrag N. Reducing distress in mothers of children with autism and other disabilities: A randomized trial. Pediatrics. 2014;134:e454–463. doi: 10.1542/peds.2013-3164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton KM, Hoge CW, Messer SC, Whitt AA, Cabrera OA, McGurk D, … Castro CA. Prevalence of mental health problems, treatment need, and barriers to care among primary care-seeking spouses of military service members involved in Iraq and Afghanistan deployments. Military Medicine. 2008;173(11):1051–1056. doi: 10.7205/milmed.173.11.1051. [DOI] [PubMed] [Google Scholar]
- Forgatch MS, Gerald PR, Gewirtz AH. Looking forward: The promise of widespread implementation of parent training programs. Perspectives on Psychological Science. 2013;8:682–694. doi: 10.1177/1745691613503478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forgatch MS, Gewirtz AH. The evolution of the Oregon model of parent management training: An intervention for antisocial behavior in children and adolescents. In: Weisz JR, Kazdin AE, editors. Evidence-Based Psychotherapies for Children and Adolescents. 3. New York: Guilford Press; 2017. [Google Scholar]
- Gewirtz AH, Erbes CR, Polusny MA, Forgatch MS, DeGarmo DS. Helping military families through the deployment process: Strategies to support parenting. Professional Psychology, Research and Practice. 2011;42:56–62. doi: 10.1037/a0022345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, DeGarmo DS, Zamir O. Testing a military family stress model. Family Process. 2017 doi: 10.1111/famp.12282. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert P. Introducing compassion-focused therapy. Advances in Psychiatric Treatment. 2009;15(3):199–208. [Google Scholar]
- Gottman JM, Katz LF, Hooven C. Parental meta-emotion philosophy and the emotional life of families: Theoretical models and preliminary data. Journal of Family Psychology. 1996;10:243–268. doi: 10.1037/0893-3200.10.3.243. [DOI] [Google Scholar]
- Gottman JM, Katz LF, Hooven C. Meta-emotion: How families communicate emotionally. Mahwah: Lawrence Erlbaum Associates; 1997. [Google Scholar]
- Harnett PH, Dawe S. The contribution of mindfulness- based therapies for children and families and proposed conceptual integration. Child and Adolescent Mental Health. 2012;17:195–208. doi: 10.1111/j.1475-3588.2011.00643.x. [DOI] [PubMed] [Google Scholar]
- Haydicky J, Shecter C, Wiener J, Ducharme JM. Evaluation of MBCT for adolescents with ADHD and their parents: Impact on individual and family functioning. Journal of Child and Family Studies. 2013;24:1–19. doi: 10.1007/s10826-013-9815-1. [DOI] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: An experiential approach to behavior change. New York: Guilford Press; 2003. [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. Journal of the American Medical Association. 2006;295:1023–1032. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- Jha AP, Stanley Ea, Kiyonaga A, Wong L, Gelfand L. Examining the protective effects of mindfulness training on working memory capacity and affective experience. Emotion. 2010;10:54–64. doi: 10.1037/a0018438. [DOI] [PubMed] [Google Scholar]
- Jones L, Hastings RP, Totsika V, Keane L, Rhule N. Child behavior problems and parental well-being in families of children with autism: The mediating role of mindfulness and acceptance. American Journal on Intellectual and Developmental Disabilities. 2014;119:171–185. doi: 10.1352/1944-7558-119.2.171. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living. New York: Delta; 1990. [Google Scholar]
- Kearney DJ, McDermott K, Malte C, Martinez M, Simpson TL. Association of participation in a mindfulness program with measures of PTSD, depression and quality of life in a veteran sample. Journal of Clinical Psychology. 2012;68:101–116. doi: 10.1002/jclp.20853. [DOI] [PubMed] [Google Scholar]
- Lester P, Peterson K, Reeves J, Knauss L, Glover D, Mogil C, … Beardslee W. The long war and parental combat deployment: Effects on military children and at-home spouses. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49:310–320. doi: 10.1016/j.jaac.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. Dialectical behavioral therapy: A cognitive behavioral approach to parasuicide. Journal of Personality Disorders. 1987;1:328–333. doi: 10.1521/pedi.1987.1.4.328. [DOI] [Google Scholar]
- Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298:2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- Myers-Walls JA, Dworkin J. Parenting education without borders: Web-based outreach. In: Ponzetti JJ, editor. Evidence-Based Parenting Education: A Global Perspective. New York: Routledge; 2016. pp. 123–139. [Google Scholar]
- Neece CL. Mindfulness-based stress reduction for parents of young children with developmental delays: Implications for parental mental health and child behavior problems. Journal of Applied Research in Intellectual Disabilities. 2014;27:174–186. doi: 10.1111/jar.12064. [DOI] [PubMed] [Google Scholar]
- Owens GP, Walter KH, Chard KM, Davis PA. Changes in mindfulness skills and treatment response among veterans in residential PTSD treatment. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4:221–228. doi: 10.1037/a0024251. [DOI] [Google Scholar]
- Patterson GR. The next generation of PMTO models. The Behavior Therapist. 2005;28(2):25–32. [Google Scholar]
- Parent J, Garai E, Forehand R, Roland E, Potts J, Haker K, … Compas BE. Parent mindfulness and child outcome: The roles of parent depressive symptoms and parenting. Mindfulness. 2010;1:254–264. doi: 10.1007/s12671-010-0034-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts LR, Neece CL. Feasibility of Mindfulness-Based Stress Reduction intervention for parents of children with developmental delays. Issues in Mental Health Nursing. 2015;36:592–602. doi: 10.3109/01612840.2015.1017063. [DOI] [PubMed] [Google Scholar]
- Snyder J, Gewirtz A, Schrepferman L, Gird SR, Quattlebaum J, Pauldine MR, … Hayes C. Parent–child relationship quality and family transmission of parent posttraumatic stress disorder symptoms and child externalizing and internalizing symptoms following fathers’ exposure to combat trauma. Development and Psychopathology. 2016;28:947–969. doi: 10.1017/S095457941600064X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder J, Low S, Bullard L, Schrepferman L, Wachlarowicz M, Marvin C, Reed A. Effective parenting practices: Social interaction learning theory and the role of emotion coaching and mindfulness. In: Larzelere RE, Morris AS, Harrist AW, editors. Authoritative parenting: Synthesizing nurturance and discipline for optimal child development. Washington D.C: American Psychological Association; 2013. pp. 189–210. [DOI] [Google Scholar]
- Singh NN, Lancioni GE, Winton ASW, Karazsia BT, Myers RE, Latham LL, Singh J. Mindfulness-Based Positive Behavior Support (MBPBS) for mothers of adolescents with autism spectrum disorder: Effects on adolescents’ behavior and parental stress. Mindfulness. 2014;5:646–657. doi: 10.1007/s12671-014-0321-3. [DOI] [Google Scholar]
- Spoth R, Redmond C. Research on family engagement in preventive interventions: Toward improved use of scientific findings in primary prevention practice. Journal of Primary Prevention. 2000;21:267–284. doi: 10.1023/A:1007039421026. [DOI] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness based cognitive therapy for depression. New York: Guilford; 2013. [Google Scholar]
- Van de Weijer-Bergsma E, Formsma AR, de Bruin EI, Bögels SM. The effectiveness of mindfulness training on behavioral problems and attentional functioning in adolescents with ADHD. Journal of Child and Family Studies. 2012;21:775–787. doi: 10.1007/s10826-011-9531-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Gemert-Pijnen JE, Kelders SM, Bohlmeijer ET. Understanding the usage of content in a mental health Intervention for depression: An analysis of log data. Journal of Medical Internet Research. 2014;16:e27. doi: 10.2196/jmir.2991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vujanovic AA, Niles B, Pietrefesa A, Schmertz SK, Potter CM. Mindfulness in the treatment of posttraumatic stress disorder among military veterans. Professional Psychology: Research and Practice. 2011;42:24–31. doi: 10.1037/a0022272. [DOI] [Google Scholar]
- Walker SK, Rudi JH. Parenting across the social ecology facilitated by information and communications technology: Implications for research and educational design. Journal of Human Sciences and Extension. 2014;2(2):15–32. [Google Scholar]
- Whittingham K, Sheffield J, Sofronoff K. Stress management for parents: Acceptance and Commitment Therapy. School of Psychology, University of Queensland; Brisbane, Australia: 2010. Unpublished manuscript. [Google Scholar]
- Whittingham K. Parents of children with disabilities, mindfulness and acceptance: A review and a call for research. Mindfulness. 2014;5:704–709. doi: 10.1007/s12671-013-0224-8. [DOI] [Google Scholar]
- Whittingham K, Sanders M, McKinlay L, Boyd RN. Parenting intervention combined with Acceptance and Commitment Therapy: A trial with families of children with cerebral palsy. Journal of Pediatric Psychology. 2016;41:531–542. doi: 10.1093/jpepsy/jsv118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeileis A, Kleiber C, Jackman S. Regression models for count data in R. Journal of Statistical Software. 2008;27(8):1–25. [Google Scholar]