Abstract
We investigated treatment effects on parenting self-efficacy and parent cognitive errors, and whether these parent cognitions are related to short- and long-term outcomes in parenting behaviors in psychosocial treatment for youth with Attention-Deficit/Hyperactivity Disorder, Predominantly Inattentive Presentation (ADHD-I). In a randomized controlled trial across 2 sites (University of California, San Francisco and University of California, Berkeley), 199 children between the ages of 7 and 11 were randomized to the Child Life and Attention Skills program (CLAS, n = 74), Parent-Focused Treatment (PFT, n = 74), or Treatment as Usual (TAU, n = 51). Parents reported on self-efficacy, cognitive errors, positive parenting, and negative parenting prior to treatment, immediately after treatment, and in the next school year at follow-up. Compared to TAU, CLAS and PFT had higher post-treatment parenting self-efficacy, and CLAS alone had lower post-treatment parent cognitive errors. At follow-up, only CLAS had improved parent cognitive errors compared to TAU. No other between-group differences were found in parenting self-efficacy or cognitive errors. Improved parenting self-efficacy was associated with improved post-treatment negative parenting outcomes for PFT and CLAS, and improved parent cognitive errors were also related to improvements in positive and negative post-treatment parenting outcomes for CLAS. Post-treatment parenting self-efficacy mediated follow-up negative parenting outcomes for CLAS and post-treatment parent cognitive errors mediated improved follow-up positive and negative parenting outcomes for CLAS. PFT and CLAS led to enhanced parenting self-efficacy, and CLAS appears especially robust in improving parent cognitive errors both in the short- and long-term. Pathways provide support for the possibility of parent cognitions as mediators of treatment effects on parenting; clinical focus on such cognitions may be useful.
Keywords: parenting self-efficacy, parent cognitive errors, ADHD-inattentive presentation, psychosocial treatment, parenting
Attention-Deficit/Hyperactivity Disorder (ADHD) is one of the most widely diagnosed childhood psychological disorders (American Psychiatric Association, 2013), with the Predominantly Inattentive Presentation of ADHD (ADHD-I) being the most common presentation in community settings (Willcutt, 2012). A number of empirically-supported behavioral treatments for ADHD have been identified (Evans, Owens, & Bunford, 2014; Fabiano et al., 2009; Pfiffner & Haack, 2014). Most studies, however, have focused on children with the Combined Presentation of ADHD, which includes elevated hyperactivity/impulsivity in addition to inattention. ADHD-I is associated with substantial academic, social, and psychological risks (e.g., American Psychiatric Association, 2013; Uchida, Spencer, Faraone, & Biederman, 2015). It is essential to identify empirically supported interventions for this presentation. Only one research program has developed and examined the effectiveness of psychosocial interventions specifically for ADHD-I (Pfiffner et al., 2007, 2014).
Pfiffner et al. (2007; 2014) developed the Child Life and Attention Skills (CLAS) program, a multi-component, integrated psychosocial treatment including behavioral parent training (BPT), teacher involvement, and child skills training, which is tailored for children with ADHD-I. This program uniquely targets multiple agents of change (children, teachers, parents), and is different from traditional BPT, which typically focuses on parents to effect change. A two-site randomized controlled trial (RCT) compared CLAS to Parent-Focused Treatment (PFT), which involved only the BPT component of CLAS, and to Treatment As Usual (TAU; Pfiffner et al., 2014). CLAS showed benefits beyond PFT on all teacher-rated child outcomes as well as parent-rated child organizational skills, and both treatments showed improved parent-rated inattention, organization, and impairment compared to TAU.
A subsequent study by Haack, Villodas, McBurnett, Hinshaw, and Pfiffner (2016) revealed that both CLAS and PFT resulted in post-treatment improvements in negative parenting, and only CLAS led to improved positive parenting, compared to TAU. In addition, Haack et al. (2016) showed that negative parenting mediated CLAS and PFT effects on parent- and teacher-rated child outcomes, and positive parenting mediated treatment effects on parent-rated outcomes for CLAS alone. These findings are consistent with past research demonstrating parenting as a possible mechanism of treatment change for externalizing difficulties (e.g., Beauchaine, Webster-Stratton, & Reid, 2005; Chronis-Tuscano et al., 2011; Gardner, Hutchings, Bywater, & Witaker, 2010; Hinshaw et al., 2000). However, potential mechanisms underlying treatment-related parenting outcomes remain underexplored. We posit that parent cognitions, comprising parents’ thoughts about their children and themselves as parents, may be associated with and potentially contribute to treatment-related improved parenting.
Parenting Self-Efficacy
Parenting self-efficacy represents one type of parent cognition. Self-efficacy is generally characterized by beliefs in one’s ability to act successfully (Bandura, 2012). Parenting self-efficacy represents a specific domain of such beliefs. Parents with high self-efficacy believe that they are able to successfully parent their child. Research by Bandura (2012) and others (e.g., Berry & West, 1993; Chwalisz, Altmaier, & Russell, 1992; Wells-Parker, Miller, & Topping, 1990) provides significant support for the links between self-efficacy and self-regulation of emotion, thought, motivation, and action, all of which can influence outcomes through such behaviors as persistence and active problem-solving. Prior research suggests that parenting self-efficacy exerts important effects on parenting (e.g., Coleman & Karraker, 1997; Teti & Gelfand, 1991), and low self-efficacy is related to harsh, coercive, withdrawn, and helpless parenting (e.g., Bondy & Mash, 1999; Bugental, Lyon, Krantz, & Cortez, 1997; Johnston & Ohan, 2005; Thomas, O’Brien, Clarke, Liu, & Chronis-Tuscano, 2015).
Parents of children with ADHD are more likely to perceive themselves to be low in parenting self-efficacy (e.g., Johnston & Mash, 2001), and studies show significant improvement in parenting self-efficacy as a function of receiving BPT. For instance, Pisterman et al. (1992) found improved parenting self-efficacy both immediately and three months after attending a parent training group for preschoolers with ADHD, compared with a control group. Similarly, Anastopolous, Shelton, DuPaul, and Guevremont (1993) found greater parenting self-esteem compared to waitlist controls after BPT and at two-month follow-up. Loren et al. (2015) also found that parents reported increased confidence in managing child behavior after a parent group for ADHD. In addition, a recent review of parental cognitive and affective outcomes following behavioral treatment for children with behavior disorders indicated that BPT was related to improved parenting self-efficacy, with medium to large effect sizes (Colalillo & Johnston, 2016).
In turn, parenting self-efficacy may be linked to BPT outcomes for ADHD. BPT promotes parental learning and use of strategies, which requires motivation, self-regulation, and persistence, all of which can be influenced by self-efficacy. In a two-stage heuristic model by Hoza, Johnston, Pillow, and Ascough (2006), initial parent cognitions are theorized to influence treatment initiation, and parent cognitions during treatment may impact treatment effects. Limited studies examine the links between parenting self-efficacy and treatment initiation and response, although existing research suggests that an association is possible. For instance, Jiang, Gurm, and Johnston (2014) found that parenting self-efficacy is related to parents’ believing in behavioral strategies as effective. In addition, van den Hoofdakker et al. (2010) found that high pre-treatment levels of parenting self-efficacy were related to better BPT child outcomes. Similarly, Hoza et al.’s (2000) research from the MTA study (the largest multi-modal treatment study of ADHD) showed that low pre-treatment levels of maternal self-esteem and paternal self-efficacy were related to more negative treatment effects on child outcome. In addition, Johnston, Mah, and Regambal (2010) asked mothers of children with ADHD to complete a BPT session and then report on their strategy use 1 week later. Mothers with higher pre-session levels of parenting self-efficacy viewed these strategies as more effective, which predicted more positive follow-up experiences. Still, no studies to our knowledge examine whether parenting self-efficacy may potentially mediate BPT effects on parenting behavior.
Parent Cognitive Errors
Parent cognitive errors represent a second important type of parent cognition. Beck (1963) described cognitive errors as biases in information processing consistent with the negative and hopeless views associated with depression. Specific to the parenting domain, parent cognitive errors reflect overly negative and helpless beliefs that parents hold with respect to their child and their parenting. Such beliefs reflect parents’ underlying negative internal, global, and stable attributions regarding their children and their parenting, and are likely related to parenting self-efficacy (Hoza et al., 2000; Johnston, Reynolds, Freeman, & Geller, 1998; Kaiser et al., 2009). These errors are important to examine among parents of children with ADHD, given the high likelihood of depressed symptoms in these parents (Chronis, Gamble, Roberts, & Pelham, 2006; Johnston & Mash, 2001), along with evidence that these parents tend to view their children’s misbehavior as global, stable, and caused by internal factors (e.g., Johnston & Freeman, 1997).
Although research on the link between parenting and cognitive errors per se is lacking, cognitive errors are a hallmark of depression (Beck, 1963). Substantial research shows that parental depression negatively influences child outcomes, and is related to negative, coercive, and disengaged parenting (e.g., Hoffman, Crnic, & Baker, 2006; Lovejoy, Graczyk, O’Hare, & Neuman, 2000). Research also shows associations between negative internal, global, and stable attributions for child misbehavior and parenting behaviors, such as over-reactivity and harsh discipline (Johnston & Ohan, 2005; Miller, 1995; Slep and O’Leary, 1998; Smith & O’Leary, 1995), as well as child outcomes (Nix et al., 1999). Such research on parental depression and attributions suggests that parent cognitive errors may well be related to parenting difficulties.
Depressogenic cognitive errors may impede progress in parent training. For instance, parents who are feeling negative and hopeless about their children’s behavior may be less likely to initiate and/or engage in treatment. No studies to our knowledge have examined BPT outcomes on parent cognitive errors, yet changes in parental depressive symptoms after parent training appear minimal. For instance, Wells et al. (2000) found no between-treatment differences in treatment outcomes on parental depression in the MTA dataset. Similarly, Chacko et al. (2009) found no improvement on parental depressive symptoms between BPT and a control group. Colalillo and Johnston’s (2016) review indicates that parent training benefits are weaker for characteristics that are more distal to parenting, such as parent depressive symptoms.
Few studies examine whether parent cognitive errors are related to BPT outcome. However, pre-treatment parental depressive symptoms are predictive of lower treatment response (e.g., Owens et al., 2003), suggesting that cognitive errors may also be related to treatment outcomes. In contrast, Hoza et al. (2000) showed no relation between pre-treatment levels of general depressogenic cognitive errors and treatment outcomes in the MTA sample, yet they used a measure of cognitive errors specific to oneself rather than cognitive errors specific to parenting and children. Indeed, in this same study, Hoza et al. (2000) found that fathers’ more negative internal attributions of their children prior to treatment were related to worse treatment effects, which supports the idea that cognitive errors more proximal to parenting and children may be related to treatment outcomes. No studies to our knowledge investigate whether parent cognitive errors may be potential mediators of BPT effects on parenting behavior.
Kaiser et al. (2009) extended the limited literature on parent cognitive errors by developing a measure of cognitive errors specific to parenting. This measure was used to assess parent cognitive errors in a pilot sample of families from the first cohort of the larger RCT of psychosocial treatments for ADHD-I described above (Pfiffner et al., 2014). Using hierarchical multiple regressions and change scores, they found that changes in post-treatment cognitive errors were related to changes in post-treatment parenting, which provide preliminary indications that improved parent cognitive errors may be linked to enhanced parenting.
Current Study
Here, we extend research on parent cognitions and psychosocial treatment by (1) evaluating treatment effects on parenting self-efficacy and parent cognitive errors, and (2) examining treatment outcomes in parenting self-efficacy and parent cognitive errors as related to treatment-related improvements in self-reported parenting at post-treatment and follow-up. We predicted that both CLAS and PFT would lead to improved post-treatment parenting self-efficacy and parent cognitive errors compared to TAU. We also predicted that improvements in parenting self-efficacy and parent cognitive errors would be related to positive effects of CLAS and PFT on negative and positive parenting at post-treatment. Analyses of follow-up outcomes were secondary as we were primarily interested in post-treatment outcomes, which were most proximal to the intervention. However, follow-up analyses were included to provide preliminary data relevant to the question of parent cognitions as potential mediators of treatment effects. In general, we expected that similar to post-treatment predictions, treatment effects on parent cognitions would be related to follow-up parenting outcomes.
Methods
Participants
199 children across two sites (University of California, San Francisco and University of California, Berkeley) participated and were recruited via school principals, mental health providers, learning specialists, pediatricians, online parent networks or professional associations, and word of mouth in the community. Participating children were required to have a primary DSM-IV diagnosis of ADHD-I (confirmed via diagnostic interview), a Full Scale IQ > 80, an age between 7–11 years (grades 2–5), the ability to participate in scheduled groups, a school proximity within 45 minutes of study site to allow for the clinician to conduct school meetings, and teacher consent to participate in school-based treatment. Children needed to be living with at least one parent for the past year and to be attending school full time in a regular classroom. Exclusion criteria included those with a developmental disability or neurological illness, those taking non-stimulant psychoactive medication (given inability to withhold medication to confirm ADHD-I diagnosis), and those who were to initiate or change medication in the near future. Total household income was below $50,000 for 14%, $50,000–100,000 for 27%, $100,000–$150,000 for 28%, and more than $150,000 for 31% of families. Detailed child and family demographics are presented in Table 1. The majority of primary parents were biological mothers (167), followed by 13 biological fathers, 10 adoptive mothers, 3 adoptive fathers, 2 stepmothers, 1 grandmother, and 3 other caregivers. Less than 5% of youth were taking medication for ADHD at randomization. All but one of these children were receiving stimulant medication.
Table 1. Child and family demographics of sample.
| CLAS M(SD) |
PFT M(SD) |
TAU M(SD) |
|
|---|---|---|---|
| Child age | 8.78 (1.15) | 8.7 (1.2) | 8.37 (1.13) |
| WISC FSIQ | 103.64 (11.04) | 102.67 (11.32) | 105.47 (11.53) |
| Child gender (% boys) | 51.4 | 64.9 | 58.8 |
| Child ethnicity (%) | |||
| Caucasian | 55.4 | 59.5 | 43.1 |
| African-American | 5.4 | 5.4 | 3.9 |
| Hispanic/Latino | 12.2 | 14.9 | 25.5 |
| Asian/Pacific Islander | 9.5 | 9.5 | 3.9 |
| Mixed/Other | 17.6 | 10.8 | 23.5 |
| Parent education (% college grads) | 83.5 | 80.8 | 78.4 |
| On medication at randomization (%) | 6.8 | 1.4 | 2 |
| Single-parent household (%) | 9.5 | 16.2 | 11.8 |
| KSADS Inattention symptoms | 7.5 (1.06) | 7.88 (1.12) | 7.5 (1.15) |
| KSADS HI symptoms | 1.21 (1.16) | 1.32 (1.27) | 1.12 (1.12) |
| KSADS Comorbid ODD (%) | 5.1 | 6.8 | 5.3 |
| KSADS Comorbid Anxiety (%) | 6.8 | 10.2 | 5.3 |
| KSADS Comorbid Depression (%) | 1.7 | 1.7 | 2.6 |
Note. CLAS = Child Life and Attention Skills Treatment; PFT = Parent-Focused Treatment; TAU = Treatment as Usual; WISC = Wechsler Intelligence Scale for Children; FSIQ = Full Scale IQ; KSADS = Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children; HI = Hyperactivity/Impulsivity; ODD = Oppositional Defiant Disorder
Procedure
Written informed consent (approved by the Committee on Human Research at University of California, San Francisco and University of California, Berkeley) was completed with parents, and children provided written assent. Screening and diagnosis occurred in three stages: 1) initial telephone screening with parents and teachers, 2) parent and teacher completion of the Child Symptom Inventory (CSI-4; Gadow & Sprafkin, 1994) and Impairment Rating Scale (IRS; Fabiano et al., 2006), and 3) diagnostic interviews by a licensed clinical psychologist, who completed comprehensive assessments via the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS-PL; Kaufman et al., 1997). There was 100% diagnostic agreement between independent clinicians of randomly selected K-SADS interviews. Children completed the Wechsler Intelligence Scale for Children-IV (WISC-IV, Wechsler, 2003), and parents received an assessment report. Parents were compensated for post-treatment (CLAS and PFT: $50, TAU: $150) and follow-up measures (CLAS and PFT: $100, TAU: $150). Teachers received compensation for pre-treatment ($50), post-treatment ($75), and follow-up measures ($75). Teachers in CLAS also received $100 for involvement in teacher consultations.
Six cohorts of children (M = 33 per cohort; range of 24–43) spanning 2009–2012 participated. Children were randomized to CLAS (36 at site 1 and 38 at site 2), PFT (36 at site 1 and 38 at site 2), or TAU (24 at site 1 and 27 at site 2). Treatment occurred over 10 to 13 weeks, with assessments immediately after treatment and 5 to 7 months after treatment (follow-up: October or November of the following school year).
Treatment Conditions
Child Life and Attention Skills Treatment (CLAS; Pfiffner et al., 2014)
CLAS was developed based on existing evidence-based treatments and is comprised of three manualized components: 1) Parent: ten 90-minute parent group meetings and up to six 30-minute individual family meetings between the parent, child, and clinician, 2) Child: ten 90-minute child group meetings, and 3) School: one 30 minute teacher orientation, and up to five 30-minute meetings between the teacher, parent, child, and clinician, as well as booster sessions.
Parent Component
The parent component was based on existing evidence-based parent training programs (Barkley, 1987; Forehand & McMahon, 1981). Weekly group sessions included introduction, review, and trouble-shooting of parenting strategies (e.g., attending, reinforcement, star chart). Biweekly individual family sessions focused on honing parenting skills development for the particular family. CLAS families also learned how to establish, monitor, and reinforce the classroom intervention, and how to prompt and reinforce skills taught in the child component. The sixth session of the parent program involved managing parent cognitive errors, which included discussing the impact of such cognitions and changing them.
Child component
The child component of CLAS was adapted from an empirically-supported ADHD social skills intervention (Pfiffner & McBurnett, 1997). Weekly group session content involved using instruction, modeling, practice, and feedback to improve independence (e.g., academic, organization, homework, and daily living skills) and social competence. Skills generalization was encouraged via group-based rewards for stars that children earned for skills use outside of session. Parents joined the child group at the end of the session to review session content and plan for shared parent-child homework when needed.
Classroom component
The classroom component was adapted from evidence-based classroom management strategies (Fabiano et al., 2010; Pfiffner, 2011). The teacher orientation involved an overview of ADHD-I and the daily report card (i.e., Classroom Challenge) targeting behavior goals selected by the teacher for each student. Classroom Challenge meetings were conducted between parents, children, and teachers to discuss these goals, which were rated three times per day by the teacher, and shaped through the program with the assistance of the CLAS clinician. These meetings also included discussion of classroom accommodations to improve attention and behavior, and teachers also learned about skills taught in the child group.
Parent Focused Treatment (PFT)
The PFT condition involved only the parent component of CLAS, which was identical to the CLAS parent component except training on working with teachers and reinforcing child component skills was not provided. The program included an identical session targeting maladaptive parent cognitions. The same number of parent groups and individual family meetings were employed, although children were not present in PFT individual family meetings. Teachers received information about ADHD-I and classroom strategies, and could contact clinicians with questions.
Booster/Maintenance Treatment for CLAS and PFT
Between post-treatment and follow-up, CLAS and PFT families were invited to attend monthly booster sessions (CLAS with parents and children; PFT with parents only) after the 10- to 13-week core intervention. These sessions focused on reviewing and trouble-shooting strategies. At the start of the school year and prior to follow-up, CLAS families were also encouraged to discuss their child’s functioning with their new teacher and have a consultation meeting with the CLAS clinician if needed.
Treatment as Usual (TAU)
Those in the TAU condition received a list of community treatment providers after their baseline assessment. They did not receive CLAS or PFT treatments, but were invited to a two-session parenting workshop after follow-up assessment. Between baseline and post-treatment periods, 14% of the children in the TAU group received medication (all except one child received stimulant medication, 33% received psychotherapy (child therapy, family therapy, or parenting group), 51% received educational interventions (tutoring, special education services at school), and 53% received classroom accommodations (such as behavioral charts, extra testing time, modified homework, preferential seating). Between post-treatment and follow-up, 21% received medication (all except two children received stimulant medication), 38% received psychotherapy, 52% received educational interventions, and 55% received accommodations in the classroom. For further information, please see Pfiffner et al. (2014).
Therapists followed detailed manuals with specific instructions regarding sequence and content of topics, and weekly conference calls to discuss sessions and clinical issues occurred to maintain cross-site fidelity. Therapists completed fidelity checklists after each session, with high ratings of amount of content covered (94% for CLAS parent group, 98% for PFT parent group, 96% for CLAS child group). Fidelity checklists were also completed by independent observers for the majority of the CLAS and PFT group sessions, and inter-rater reliability was greater than 97%. In both treatments, close to 100% of session content was covered. For further details, please see Pfiffner et al. (2014).
Measures
Parent Cognitive Error Questionnaire (PCEQ; Kaiser et al., 2009)
The PCEQ is a 24-item parent-report questionnaire assessing cognitive errors related to attributions of negative child behavior and parenting. This measure is based on two psychometrically-sound measures of general cognitive errors (i.e., Cognitive Error Questionnaire [Lefebvre, 1981] and Child Negative Cognitive Error Questionnaire [Leitenberg, Yost, & Carroll-Wilson, 1986]), but assesses cognitions specific to parenting and child behavior. A sample item is you tell your child to put away his/her backpack and then come to the dinner table right away. Your child disappears into his/her bedroom. After 10 minutes, you sigh to yourself and think, ‘my child never does anything he/she is supposed to do’. Parents then rate on a 5-point scale ranging from almost exactly like I would think to not at all like I would think, with higher scores reflecting higher errors. Internal consistency was shown via Cronbach’s alphas of .90 at baseline, .89 at post-treatment, and .90 at follow-up, and convergent validity with parental depressive symptoms was shown by rs = .25 to .32, ps < .001.
Parenting Sense of Competence Scale (PSOC; Johnston & Mash, 1989)
The PSOC is a 17-item parent-report measure that yields subscales of parenting Efficacy and Satisfaction. The Efficacy subscale was used, which includes 7 items measuring parenting self-efficacy, with adequate psychometric properties. A sample item is the problems of taking care of a child are easy to solve once you know how your actions affect your child, an understanding I have acquired. Parents rate on a 6-point scale ranging from strongly disagree to strongly agree, with higher scores indicating higher efficacy. Internal consistency was adequate, with Cronbach’s alphas of .77 at baseline, .79 at post-treatment, and .80 at follow-up for this sample.
Parenting
The Alabama Parenting Questionnaire (APQ; Shelton, Frick, & Wootton, 1996) is a 42-item parent-report measure assessing five categories of parenting practices (Involvement, Positive Parenting, Poor Monitoring/Supervision, Inconsistent Discipline, and Corporal Punishment). A sample item is you reward or give something extra to your child for obeying you or behaving well. Parents rate on a 5-point scale ranging from never to always, with higher scores representing higher levels of the particular parenting category. The Parent-Child Relationship Questionnaire-Brief Version (PCRQ; Furman & Giberson, 1995) is a 40-item parent-report measure that evaluates five dimensions of parent-child relationships (Warmth, Disciplinary Warmth, Power Assertion, Personal Relationship, and Possessiveness). A sample item is how much do you and this child care about each other? Parents respond on a 5-point scale ranging from hardly at all to extremely. The APQ and PCRQ have adequate psychometric properties (Furman & Giberson, 1995; Shelton et al. 1996). Positive and negative parenting composite scores composed of items from the APQ and PCRQ were created, based on the results of factor analyses by prior researchers (Hinshaw et al., 2000; Wells et al., 2000). The positive parenting composite involves 40 items from the APQ Involvement and Positive Parenting and the PCRQ Warmth and Disciplinary Warmth subscales. The negative parenting composite includes 24 items from the APQ Inconsistent Discipline and Corporal Punishment and the PCRQ Power Assertion subscales. Cronbach’s alphas at baseline, post-treatment, and follow-up, respectively, were .90, .91, and .91 for positive parenting and .79, .77, and .81 for negative parenting, demonstrating adequate internal consistency.
Data Analysis Plan
To test the effects of treatment on parent cognition outcomes, general linear models were estimated and tested using IBM SPSS Version 23 with post-treatment and follow-up parent cognitions as dependent variables and respective pre-treatment or baseline parent cognitions as covariates. For models with significant findings, Bonferroni pairwise comparisons were carried out to test specific contrasts of treatment comparisons. To investigate inter-individual outcomes in parenting self-efficacy and parent cognitive errors as related to inter-individual outcomes in positive and negative self-reported parenting practices as a function of treatment, Structural Equation Modeling (SEM) was conducted in Mplus Version 7.4, using bias-corrected bootstrapped confidence intervals with 5000 bootstrap draws. Indicators such as the Comparative Fit Index (CFI; Bentler, 1990), the Root Mean Square Error of Approximation (RMSEA; Steiger, 1990), and the Standardized Root Mean Square Residual (SRMR; Hu & Bentler, 1999) were used to assess overall model fit using current guidelines (Hu & Bentler, 1999). Significance values were used to determine individual path fit and indirect effects of parent cognitions.
Results
1.41% of data were missing at baseline, 3.78% of data were missing at post-treatment, and 7.87% of values were missing at follow-up. Missing values appeared to be related to attrition. Prior to post-assessment, four families discontinued their participation, and prior to follow-up, eight families ended their involvement. Mean scale substitution was used by SPSS for subscales with less than 1/3rd of missing data for descriptive and treatment outcome analyses. Multiple imputations led to similar patterns in treatment outcome analyses. Full Information Maximum Likelihood estimation was used by Mplus.
Treatment Effects
Parenting self-efficacy
Treatment type was predictive of post-treatment parenting self-efficacy, F(2, 184) = 7.96, p < .001, ƞp2 = .08. Compared to TAU, CLAS, p < .01, and PFT, p < .01, yielded higher parenting self-efficacy. PFT and CLAS were not significantly different from each other. Means (and standard errors) are 4.29 (.07) for CLAS, 4.25(.07) for PFT, and 3.86 (.09) for TAU. No between-group differences in follow-up self-efficacy were found.
Parent cognitive errors
Treatment type was predictive of post-treatment parent cognitive errors, F(2, 185) = 4.29, p < .05, ƞp2 = .04. CLAS yielded lower cognitive errors than TAU, p < .05. CLAS and PFT did not differ significantly in cognitive errors, and neither did PFT and TAU. Means (and standard errors) are 1.49 (.04) for CLAS, 1.58 (.04) for PFT, and 1.67 (.05) for TAU. Treatment type was predictive of follow-up parent cognitive errors, F(2, 177) = 3.20, p < .05, ƞp2 = .04. CLAS yielded improved cognitive errors compared to TAU, p = .05. CLAS and PFT did not differ significantly in cognitive errors, nor did PFT and TAU. Means (and standard errors) are 1.48 (.04) for CLAS, 1.58 (.04) for PFT, and 1.64 (.05) for TAU.
Path Analyses
Post-treatment outcomes
Figures 1 and 2 display path models with PFT and CLAS dummy-coded in comparison to TAU. PFT and CLAS were treatment variables, parenting self-efficacy and parent cognitive errors were post-treatment variables, and negative and positive parenting were post-treatment variables. Baseline parenting self-efficacy, negative parenting, and positive parenting were entered as covariates. Both models showed good fit, with non-significant chi-square tests of model fit, CFI of 1.00, RMSEA of .00, and SRMR values of (a) .03 (model with post-treatment parenting) and (b) .02 (model with follow-up parenting). Results (see Table 2) showed that improved parenting self-efficacy was related to CLAS improvements on post-treatment negative parenting, β = −.07, p < .05, and PFT improvements in post-treatment negative parenting, β = −.06, p < .05. Data also revealed marginally significant associations for self-efficacy for CLAS and PFT on post-treatment positive parenting, β = .04, p < .06, β = .04, p < .06, respectively. CLAS was associated with improved post-treatment parent cognitive errors, which were related to improved post-treatment positive parenting, β = .04, p < .05, and negative parenting, β = −.10, p < .01.
Figure 1. Path analyses from treatment to post-treatment parenting self-efficacy to post-treatment parenting.

Note. † p < .06; *p <.05; **p <.01; ***p <.001. Coefficients in the model are standardized
Figure 2. Path analyses from treatment to post-treatment parent cognitive errors to post-treatment parenting.

Note. † p < .10; *p <.05; **p <.01; ***p <.001. Coefficients in the model are standardized.
Table 2. Indirect effects for parent cognitions between treatment type and post-treatment and follow-up parenting.
| CLAS | PFT | |||
|---|---|---|---|---|
|
|
||||
| Outcomes | Parenting Self-Efficacy Indirect Effect (95% CI) |
Parent Cognitive Errors Indirect Effect (95% CI) |
Parenting Self-Efficacy Indirect Effect (95% CI) |
Parent Cognitive Errors Indirect Effect (95% CI) |
| Post-treatment Positive Parenting | .04†(−.001, .08) | .04* (.01, .08) | .04† (−.001, .07) | .02 (−.01, .05) |
| Post-treatment Negative Parenting | −.07*(−.12, −.01) | −.10** (−.16, −.03) | −.06* (−.11, −.01) | −.05 (−.11, .01) |
| Follow-up Positive Parenting | .03 (−.01, .07) | .03* (.003, .06) | .03 (−.01, .06) | .02 (−.01, .04) |
| Follow-up Negative Parenting | −.05* (−.10, −.004) | −.07* (−.12, −.01) | −.05†(−.09, .001) | −.03 (−.08, .01) |
Note. CLAS = Child Life and Attention Skills Treatment; PFT = Parent-Focused Treatment; 95% CI = bias-corrected bootstrapped 95% confidence intervals. Indirect effects represent standardized coefficients.
p < .06;
p < .05;
p < .01.
Follow-up outcomes
Figures 3 and 4 display path models with PFT and CLAS dummy-coded as predictors in comparison to TAU, post-treatment parenting self-efficacy and parent cognitive errors as mediators, and follow-up negative and positive parenting as outcomes. Baseline parent cognitive errors, negative parenting, and positive parenting were covaried. Both models exhibited good fit, as displayed by non-significant chi-square tests of model fit, CFI of 1.00, RMSEA of .00, and SRMR of .02. Results (see Table 2) showed improved post-treatment parenting self-efficacy mediated CLAS effects on follow-up negative parenting, β = −.05, p < .05. In addition, there was a marginally significant indirect effect by self-efficacy for PFT on followup negative parenting, β = −.05, p < .06. Findings also showed that improved parent cognitive errors mediated CLAS effects on positive parenting, β = .03, p < .05, and negative parenting, β = −.07, p < .05, both at follow-up.
Figure 3. Path analyses from treatment to post-treatment parenting self-efficacy to follow-up parenting.
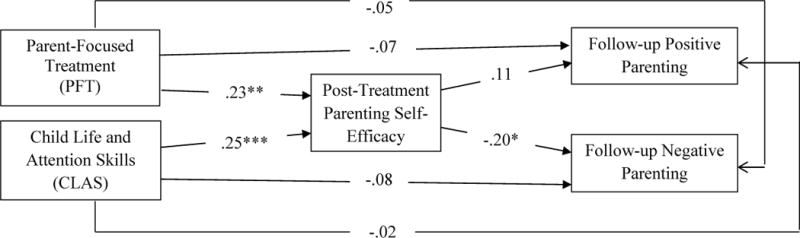
Note. *p <.05; **p <.01; ***p <.001. Coefficients in the model are standardized.
Figure 4. Path analyses from treatment to post-treatment parent cognitive errors to follow-up parenting.

Note. *p <.05; **p <.01; ***p <.001. Coefficients in the model are standardized.
Discussion
We examined treatment outcomes on parent cognitions and investigated outcomes in parent cognitions as related to psychosocial treatment effects on self-reported parenting practices. Consistent with predictions, CLAS and PFT led to increased post-treatment parenting self-efficacy, compared to TAU. However, only CLAS led to improved post-treatment and follow-up parent cognitive errors compared to TAU. Treatment outcomes in parenting self-efficacy were related to CLAS and PFT effects on parenting, and CLAS effects on parent cognitive errors were related to CLAS improvement on parenting. These results are consistent with the possibility that parent cognitions may potentially mediate between treatment and parenting.
Treatment Effects on Parenting Self-Efficacy and Parent Cognitive Errors
Both CLAS and PFT led to improved parental perceptions of their ability to parent successfully, which is unsurprising given that parents learn parenting strategies in BPT and experience success in doing so. Effect sizes of improvements in parenting self-efficacy and parent cognitive errors were in the medium range. Only CLAS resulted in significant reductions to post-treatment parent cognitive errors compared to TAU, an unexpected finding given that PFT included an identical parent session focusing on reducing maladaptive cognitions. In addition, only CLAS led to sustained improvement in parent cognitive errors at follow-up compared to TAU. The multi-component nature of CLAS, with its multiple agents of change (e.g., teachers, children, parents), the greater quantity of psychosocial treatment, and/or the greater potency of CLAS may have led to improved parent cognitive errors, which were sustained across time.
Outcomes in Parenting Self-Efficacy relate to Treatment Effects on Parenting
Treatment-related improved parenting self-efficacy was related to improved post-treatment negative parenting for both PFT and CLAS, and follow-up negative parenting for CLAS. Furthermore, self-efficacy was marginally significantly associated with post-treatment PFT and CLAS positive parenting and follow-up negative parenting for PFT. These path analyses are in line with the possibility of self-efficacy mediating between treatment and parenting. Research indicates that self-efficacy influences the level of distress one experiences in reaction to difficult situations. Those with high perceived efficacy may actively problem-solve whereas those with low self-efficacy may exhibit avoidant behavior or deplete their energy in relieving internal distress (e.g., Bandura, 1991; Chwalisz et al., 1992). Self-efficacy may be linked to BPT outcomes via increased parental self-regulation, which in turn leads to greater treatment engagement and more effective use of strategies (e.g., Mah & Johnston, 2008).
The association of treatment outcomes on parenting self-efficacy between treatment and parenting appears significant and most powerful for negative rather than positive parenting. Reducing negative parenting may require more difficult behavioral self-regulation in situations of higher emotional salience (e.g., Mazursky-Horowitz et al., 2015; Metcalfe & Mischel, 1999). In addition, self-regulation in such situations may entail a neurocognitive executive function (EF) process distinct from the EF processes typically used in affectively neutral contexts (e.g., Zelazo & Carlson, 2012). Negative parenting involves such behaviors as threatening to punish a child and not following through, allowing children to talk themselves out of punishments, and yelling at a child, whereas positive parenting includes having a friendly talk with a child, playing or having fun with a child, and praising a child. One can speculate how the need for self-regulation of negative parenting may be greater in situations of high emotional salience, in comparison to positive parenting. Negative parenting may be harder to control, which perhaps may allow for the benefits of self-efficacy (e.g., increased self-regulation) to exert a greater impact.
Outcomes in Parent Cognitive Errors relate to Treatment Effects on Parenting
Reduced parent cognitive errors were related to improvements in both positive and negative parenting at post-treatment and follow-up positive and negative parenting for CLAS alone. Such significant pathways are consistent with the possibility that parent cognitive errors may potentially mediate parenting. Parent cognitive errors reflect thoughts related to attributions regarding one’s child and parenting, and research indicates that such attributions can influence emotional and behavioral responses (e.g., Geller & Johnston, 1995; Joiner & Wagner, 1996; Smith & O’Leary, 1995). Hopeless attributions are related to more negative parenting and child outcomes, and positive changes in such thoughts can improve parenting (e.g., Johnston & Ohan, 2005). CLAS was the only treatment that led to significantly improved cognitive errors compared to TAU, which suggests the presence of CLAS-specific treatment components contributing to this effect. It is possible that maladaptive parental thoughts may be more amenable to change when treatment targets multiple agents of change. Seeing others involved in treatment may encourage parents to reduce negative thoughts/feelings of primary responsibility for child misbehavior. The strengths-based CLAS child group may render parents less likely to make negative assumptions and attributions regarding their children if they are seeing positive effort from their children. It is also possible that parents are less likely to hold persistent cognitive errors when greater positive change occurs, as is the case in CLAS. These possibilities are not mutually-exclusive and are likely interconnected.
Limitations and Future Directions
The nature of our path analyses limits interpretations of causality. However, our study represents a first step in demonstrating pathways consistent with mediation, our interpretations of parent cognitions as potentially influencing parenting are consistent with existing literature, and we do not mean to preclude reverse effects in which parenting behavior affects parent cognitions. Future studies will need to assess early parent cognitions and parenting at various points during active treatment to predict later parenting outcomes. A further limitation involves the lack of between-treatment differences in negative or positive parenting at follow-up, which can complicate interpretation of outcomes in cognitive errors being related to sustained treatment effects on parenting at follow-up. We argue that such non-significant treatment differences do not diminish the value of knowing that improved parent cognitions are related to parenting at follow-up, regardless of the level of negative and positive parenting in comparison to other treatments. Understanding post-treatment improvements in parent cognitions can provide important information regarding future parenting. Furthermore, analyses examined inter-individual outcomes rather than intra-individual change, and future studies are recommended to examine how changes in parent cognitions relate to treatment effects within individuals.
By design, participants were of ADHD-I presentation, and results may therefore not extend to youth featuring prominent hyperactivity-impulsivity. Children with such presentations are more likely to exhibit defiance and disruption, and parent cognitions for these presentations may be more negative than for children with ADHD-I (e.g., Johnston, Chen, & Ohan, 2006). Future research should examine similar analyses for children with other ADHD presentations. Future studies should also determine the generalizability of these results to populations of other ethnicities and socioeconomic statuses.
Parent-reported questionnaires were used to measure parental cognitions and parenting behavior, and rater bias may have contributed to results. It is difficult to determine a valid alternative to self-report measures to assess parent cognitions. However, it is possible to have more objective measures of parenting, and further replication with methods such as behavioral observations is necessary. The validity of our parenting measures however, is underscored by their psychometric properties and mediation of treatment effects on parent- and teacher-rated improvements in child outcomes (Haack et al., 2016).
We conducted this study in the context of an RCT comparing CLAS to PFT and TAU. Although parent cognitive errors improved only in CLAS, one cannot definitively tease apart the specific mechanism in CLAS that may have led to such effects. Given that both PFT and CLAS involved parent curriculum that addressed cognitive errors, it is quite possible that CLAS-linked involvement of multiple agents led to such outcomes. Yet it is also possible that some other CLAS-unique factor led to such improvements. Future studies could investigate the specific and/or non-specific treatment factors necessary to change parent cognitive errors.
Clinical Implications
Given that treatment outcomes in both parenting self-efficacy and parent cognitive errors are significantly related to treatment effects on parenting, understanding how parent cognitions improve during treatment may help clinicians understand current and future parenting. To the extent that parent cognitions may mediate parenting, it may be helpful for treatments to place greater emphasis on improving parent cognitions. Although prior research examining parent training with cognitive additions is mixed (e.g., Kaminski, Valle, Filene, & Boyle, 2008), such research commonly involved cognitive enhancements within a single session or parts of sessions. Our findings suggest that parenting self-efficacy is enhanced by both parent-focused and multi-component treatment. However, a single session dose of cognitive strategies in parent training may not be enough to result in meaningful improvements to parent cognitive errors in particular. To reduce these cognitive errors, it may be helpful to devote greater session time to cognitive strategies (e.g., Chronis et al., 2006; Sanders & McFarland, 2001) or as suggested by multi-component CLAS findings, include multiple agents of change. Although parent training alone can enhance parenting self-efficacy, an integrated, collaborative approach appears especially useful in meaningfully improving immediate and future parent cognitive errors, which are reflective of significant short- and long-term improvements in parenting.
Highlights.
An RCT examined psychosocial treatments (CLAS and PFT) for ADHD-Inattentive type.
CLAS and PFT led to improvements in post-treatment parenting self-efficacy.
CLAS alone led to reduced post-treatment and follow-up parent cognitive errors.
Improved self-efficacy was related to improved negative parenting for CLAS and PFT.
Reduced cognitive errors were related to improved positive and negative parenting in CLAS.
Acknowledgments
This work was supported by the National Institute of Mental Health (grant MH077671; Principal Investigators: Linda J. Pfiffner, contact P.I., and Stephen P. Hinshaw).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Washington: American Psychiatric Association; 2013. [Google Scholar]
- Anastopoulos AD, Shelton TL, DuPaul GJ, Guevremont DC. Parent training for attention-deficit hyperactivity disorder: Its impact on parent functioning. Journal of Abnormal Child Psychology. 1993;21:581–596. doi: 10.1007/BF00916320. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes. 1991;50:248–287. doi: 10.1016/0749-5978(91)90022-L. [DOI] [Google Scholar]
- Bandura A. On the functional properties of perceived self-efficacy revisited. Journal of Management. 2012;38:9–44. doi: 10.1177/0149206311410606. [DOI] [Google Scholar]
- Barkley RA. Defiant children. New York: Guilford Press; 1987. [Google Scholar]
- Beauchaine TP, Webster-Stratton C, Reid MJ. Mediators, moderators, and predictors of 1-year outcomes among children treated for early-onset conduct problems: A latent growth curve analysis. Journal of Consulting and Clinical Psychology. 2005;73:371. doi: 10.1037/0022-006X.73.3.371. [DOI] [PubMed] [Google Scholar]
- Beck AT. Thinking and depression: I. Idiosyncratic content and cognitive distortions. Archives of General Psychiatry. 1963;9:324–333. doi: 10.1001/archpsyc.1963.01720160014002. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berry JM, West RL. Cognitive self-efficacy in relation to personal mastery and goal setting across the life span. International Journal of Behavioral Development. 1993;16:351–379. [Google Scholar]
- Bondy EM, Mash EJ. Parenting efficacy, perceived control over caregiving failure, and mothers’ reactions to preschool children’s misbehavior. Child Study Journal. 1999;29:157–73. [Google Scholar]
- Bugental DB, Lyon JE, Krantz J, Cortez V. Who’s the boss? Differential accessibility of dominance ideation in parent–child relationships. Journal of Personality and Social Psychology. 1997;72:1297. doi: 10.1037/0022-3514.72.6.1297. [DOI] [Google Scholar]
- Chacko A, Wymbs BT, Wymbs FA, Pelham WE, Swanger-Gagne MS, Girio E, O’Connor B. Enhancing traditional behavioral parent training for single mothers of children with ADHD. Journal of Clinical Child & Adolescent Psychology. 2009;38:206–218. doi: 10.1080/15374410802698388. [DOI] [PubMed] [Google Scholar]
- Chronis AM, Gamble SA, Roberts JE, Pelham WE. Cognitive-behavioral depression treatment for mothers of children with attention-deficit/hyperactivity disorder. Behavior Therapy. 2006;37:143–158. doi: 10.1016/j.beth.2005.08.001. doi:0005-7894/06/0143-0158. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, O’Brien KA, Johnston C, Jones HA, Clarke TL, Raggi VL, Seymour KE. The relation between maternal ADHD symptoms and improvement in child behavior following brief behavioral parent training is mediated by change in negative parenting. Journal of Abnormal Child Psychology. 2011;39:1047–1057. doi: 10.1007/s10802-011-9518-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chwalisz K, Altmaier EM, Russell DW. Causal attributions, self-efficacy cognitions, and coping with stress. Journal of Social and Clinical Psychology. 1992;11:377–400. doi: 10.1521/jscp.1992.11.4.377. [DOI] [Google Scholar]
- Colalillo S, Johnston C. Parenting cognition and affective outcomes following parent management training: A systematic review. Clinical Child and Family Psychology Review. 2016;19:216–235. doi: 10.1007/s10567-016-0208-z. [DOI] [PubMed] [Google Scholar]
- Coleman PK, Karraker KH. Self-efficacy and parenting quality: Findings and future applications. Developmental Review. 1997;18:47–85. doi: 10.1006/drev.1997.0448. [DOI] [Google Scholar]
- Evans SW, Owens JS, Bunford N. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2014;43:527–551. doi: 10.1080/15374416.2013.850700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabiano GA, Pelham WE, Coles EK, Gnagy EM, Chronis-Tuscano A, O’Connor BC. A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder. Clinical Psychology Review. 2009;29:129–140. doi: 10.1016/j.cpr.2008.11.001. [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Pelham WE, Waschbusch DA, Gnagy EM, Lahey BB, Chronis AM, Burrows-MacLean L. A practical measure of impairment: Psychometric properties of the Impairment Rating Scale in samples of children with attention deficit hyperactivity disorder and two school-based samples. Journal of Clinical Child and Adolescent Psychology. 2006;35:369–385. doi: 10.1207/s15374424jccp3503_3. [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Vujnovic RK, Pelham WE, Waschbusch DA, Massetti GM, Pariseau ME, Greiner AR. Enhancing the effectiveness of special education programming for children with attention deficit hyperactivity disorder using a daily report card. School Psychology Review. 2010;39:219. [Google Scholar]
- Forehand RL, McMahon RJ. Helping the noncompliant child: A clinician’s guide to parent training. New York: Guilford press; 1981. [Google Scholar]
- Furman W, Giberson RS. Identifying the links between parents and their children’s sibling relationships. Close Relationships and Socioemotional Development. 1995;7:95–108. [Google Scholar]
- Gadow KD, Sprafkin JN. Child symptom inventory 4: Screening and norms manual. Stony Brook, NY: Checkmate Plus; 2002. [Google Scholar]
- Gardner F, Hutchings J, Bywater T, Whitaker C. Who benefits and how does it work? Moderators and mediators of outcome in an effectiveness trial of a parenting intervention. Journal of Clinical Child & Adolescent Psychology. 2010;39:568–580. doi: 10.1080/15374416.2010.486315. [DOI] [PubMed] [Google Scholar]
- Geller J, Johnston C. Predictors of mother’s responses to child noncompliance: Attributions and attitudes. Journal of Clinical Child Psychology. 1995;24:272–278. doi: 10.1207/s15374424jccp2403_4. [DOI] [Google Scholar]
- Haack LM, Villodas M, McBurnett K, Hinshaw S, Pfiffner LJ. Parenting as a mechanism of change in psychosocial treatment for youth with ADHD, predominantly inattentive presentation. Journal of Abnormal Child Psychology. 2016 doi: 10.1007/s10802-016-0199-8. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Wells KC, Kraemer HC, Abikoff HB, Arnold LE, Hoza B. Family processes and treatment outcome in the MTA: Negative/ineffective parenting practices in relation to multimodal treatment. Journal of Abnormal Child Psychology. 2000;28:555–568. doi: 10.1023/A:1005183115230. [DOI] [PubMed] [Google Scholar]
- Hoffman C, Crnic KA, Baker JK. Maternal depression and parenting: Implications for children’s emergent emotion regulation and behavioral functioning. Parenting: Science and Practice. 2006;6:271–295. doi: 10.1207/s15327922par0604_1. [DOI] [Google Scholar]
- Hoza B, Johnston C, Pillow DR, Ascough JC. Predicting treatment response for childhood attention-deficit/hyperactivity disorder: Introduction of a heuristic model to guide research. Applied and Preventive Psychology. 2006;11:215–229. doi: 10.1016/j.appsy.2005.11.001. [DOI] [Google Scholar]
- Hoza B, Owens JS, Pelham WE, Swanson JM, Conners CK, Hinshaw SP, Kraemer HC. Parent cognitions as predictors of child treatment response in attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology. 2000;28:569–583. doi: 10.1023/A:1005135232068. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Jiang Y, Gurm M, Johnston C. Child impairment and parenting self-efficacy in relation to mothers’ views of ADHD treatments. Journal of Attention Disorders. 2014;18:532–541. doi: 10.1177/1087054712443412. [DOI] [PubMed] [Google Scholar]
- Johnston C, Chen M, Ohan J. Mothers’ attributions for behavior in nonproblem boys, boys with attention deficit hyperactivity disorder, and boys with attention deficit hyperactivity disorder and oppositional defiant behavior. Journal of Clinical Child and Adolescent Psychology. 2006;35:60–71. doi: 10.1207/s15374424jccp3501_6. [DOI] [PubMed] [Google Scholar]
- Johnston C, Freeman W. Attributions for child behavior in parents of children without behavior disorders and children with attention-deficit-hyperactivity disorder. Journal of Consulting and Clinical Psychology. 1997;65:636–645. doi: 10.1037/0022-006X.65.4.636. [DOI] [PubMed] [Google Scholar]
- Johnston C, Mah JW, Regambal M. Parenting cognitions and treatment beliefs as predictors of experience using behavioral parenting strategies in families of children with attention-deficit/hyperactivity disorder. Behavior Therapy. 2010;41:491–504. doi: 10.1016/j.beth.2010.02.001. [DOI] [PubMed] [Google Scholar]
- Johnston C, Mash EJ. A measure of parenting satisfaction and efficacy. Journal of Clinical Child and Adolescent Psychology. 1989;18:167–175. doi: 10.1207/s15374424jccp1802_8. [DOI] [Google Scholar]
- Johnston C, Mash EJ. Families of children with attention-deficit/hyperactivity disorder: Review and recommendations for future research. Clinical Child and Family Psychology Review. 2001;4:183–207. doi: 10.1023/A:1017592030434. [DOI] [PubMed] [Google Scholar]
- Johnston C, Ohan JL. The importance of parental attributions in families of children with attention-deficit/hyperactivity and disruptive behavior disorders. Clinical Child and Family Psychology Review. 2005;8:167–182. doi: 10.1007/s10567-005-6663-6. [DOI] [PubMed] [Google Scholar]
- Johnston C, Reynolds S, Freeman WS, Geller J. Assessing parent attributions for child behavior using open-ended questions. Journal of Clinical Child Psychology. 1998;27:87–97. doi: 10.1207/s15374424jccp2701_10. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Wagner KD. Parental, child-centered attributions and outcome: A meta-analytic review with conceptual and methodological implications. Journal of Abnormal Child Psychology. 1996;24:37–52. doi: 10.1007/BF01448372. [DOI] [PubMed] [Google Scholar]
- Kaiser NM, Hinshaw SP, Pfiffner LJ. Parent cognitions and behavioral parent training: Engagement and outcomes. The ADHD Report. 2009;18:6–12. [Google Scholar]
- Kaminski JW, Valle LA, Filene JH, Boyle CL. A meta-analytic review of components associated with parent training program effectiveness. Journal of Abnormal Child Psychology. 2008;36:567–589. doi: 10.1007/s10802-007-9201-9. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Ryan N. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Lefebvre MF. Cognitive distortion and cognitive errors in depressed psychiatric and low back pain patients. Journal of Consulting and Clinical Psychology. 1981;49:517. doi: 10.1037/0022-006X.49.4.517. [DOI] [PubMed] [Google Scholar]
- Leitenberg H, Yost LW, Carroll-Wilson M. Negative cognitive errors in children: Questionnaire development, normative data, and comparisons between children with and without self-reported symptoms of depression, low self-esteem, and evaluation anxiety. Journal of Consulting and Clinical Psychology. 1986;54:528. doi: 10.1037/0022-006X.54.4.528. [DOI] [PubMed] [Google Scholar]
- Loren RE, Vaughn AJ, Langberg JM, Cyran JE, Proano-Raps T, Smolyansky BH, Epstein JN. Effects of an 8-session behavioral parent training group for parents of children with ADHD on child impairment and parenting confidence. Journal of Attention Disorders. 2015;19:158–166. doi: 10.1177/1087054713484175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/S0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Mah JW, Johnston C. Parental social cognitions: Considerations in the acceptability of and engagement in behavioral parent training. Clinical Child and Family Psychology Review. 2008;11:218–236. doi: 10.1007/s10567-008-0038-8. [DOI] [PubMed] [Google Scholar]
- Mazursky-Horowitz H, Felton JW, MacPherson L, Ehrlich KB, Cassidy J, Lejuez CW, Chronis-Tuscano A. Maternal emotion regulation mediates the association between adult attention-deficit/hyperactivity disorder symptoms and parenting. Journal of Abnormal Child Psychology. 2015;43:121–131. doi: 10.1007/s10802-014-9894-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metcalfe J, Mischel W. A hot/cool-system analysis of delay of gratification: Dynamics of willpower. Psychological Review. 1999;106:3. doi: 10.1037/0033-295X.106.1.3. [DOI] [PubMed] [Google Scholar]
- Miller SA. Parents’ attributions for their children’s behavior. Child Development. 1995;66:1557–1584. doi: 10.1111/j.1467-8624.1995.tb00952.x. [DOI] [PubMed] [Google Scholar]
- Nix RL, Pinderhughes EE, Dodge KA, Bates JE, Pettit GS, McFadyen-Ketchum SA. The relation between mothers’ hostile attribution tendencies and children’s externalizing behavior problems: The mediating role of mothers’ harsh discipline practices. Child Development. 1999;70:896–909. doi: 10.1111/1467-8624.00065. [DOI] [PubMed] [Google Scholar]
- Owens EB, Hinshaw SP, Kraemer HC, Arnold LE, Abikoff HB, Cantwell DP, Hoza B. Which treatment for whom for ADHD? Moderators of treatment response in the MTA. Journal of Consulting and Clinical Psychology. 2003;71:540. doi: 10.1037/0022-006X.71.3.540. [DOI] [PubMed] [Google Scholar]
- Pfiffner LJ. All about ADHD: The complete practical guide for classroom teachers. 2nd. New York, NY: Scholastic; 2011. [Google Scholar]
- Pfiffner LJ, Haack LM. Behavior management for school-aged children with ADHD. Child and Adolescent Psychiatric Clinics of North America. 2014;23:731–746. doi: 10.1016/j.chc.2014.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfiffner LJ, Hinshaw SP, Owens E, Zalecki C, Kaiser NM, Villodas M, McBurnett K. A two-site randomized clinical trial of integrated psychosocial treatment for ADHD-inattentive type. Journal of Consulting and Clinical Psychology. 2014;82:1115. doi: 10.1037/a0036887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfiffner LJ, McBurnett K. Social skills training with parent generalization: Treatment effects for children with attention deficit disorder. Journal of Consulting and Clinical Psychology. 1997;65:749. doi: 10.1037/0022-006X.65.5.749. [DOI] [PubMed] [Google Scholar]
- Pfiffner LJ, Mikami AY, Huang-Pollock C, Easterlin B, Zalecki C, McBurnett K. A randomized, controlled trial of integrated home-school behavioral treatment for ADHD, predominantly inattentive type. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1041–1050. doi: 10.1097/chi.0b013e318064675f. [DOI] [PubMed] [Google Scholar]
- Pisterman S, Firestone P, McGrath P, Goodman JT, Webster I, Mallory R, Goffin B. The role of parent training in treatment of preschoolers with ADDH. American Journal of Orthopsychiatry. 1992;62:397. doi: 10.1037/h0079356. [DOI] [PubMed] [Google Scholar]
- Sanders MR, McFarland M. Treatment of depressed mothers with disruptive children: A controlled evaluation of cognitive behavioral family intervention. Behavior Therapy. 2001;31:89–112. doi: 10.1016/S0005-7894(00)80006-4. [DOI] [Google Scholar]
- Shelton KK, Frick PJ, Wootton J. Assessment of parenting practices in families of elementary school-age children. Journal of Clinical Child Psychology. 1996;25:317–329. doi: 10.1207/s15374424jccp2503_8. [DOI] [Google Scholar]
- Slep AMS, O’Leary SG. The effects of maternal attributions on parenting: An experimental analysis. Journal of Family Psychology. 1998;12:234. doi: 10.1037/0893-3200.12.2.234. [DOI] [Google Scholar]
- Smith AM, O’Leary SG. Attributions and arousal as predictors of maternal discipline. Cognitive Therapy and Research. 1995;19:459–471. doi: 10.1007/BF02230412. [DOI] [Google Scholar]
- Steiger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Teti DM, Gelfand DM. Behavioral competence among mothers of infants in the first year: The mediational role of maternal self-efficacy. Child Development. 1991;62:918–929. doi: 10.1111/j.1467-8624.1991.tb01580.x. [DOI] [PubMed] [Google Scholar]
- Thomas SR, O’Brien KA, Clarke TL, Liu Y, Chronis-Tuscano A. Maternal depression history moderates parenting responses to compliant and noncompliant behaviors of children with ADHD. Journal of Abnormal Child Psychology. 2015;43:1257–1269. doi: 10.1007/s10802-014-9957-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchida M, Spencer TJ, Faraone SV, Biederman J. Adult outcome of ADHD: An overview of results from the MGH longitudinal family studies of pediatrically and psychiatrically referred youth with and without ADHD of both sexes. Journal of Attention Disorders. 2015 doi: 10.1177/1087054715604360. Advance online publication. [DOI] [PubMed] [Google Scholar]
- van den Hoofdakker BJ, Nauta MH, van der Veen-Mulders L, Sytema S, Emmelkamp PM, Minderaa RB, Hoekstra PJ. Behavioral parent training as an adjunct to routine care in children with attention-deficit/hyperactivity disorder: Moderators of treatment response. Journal of Pediatric Psychology. 2010;35:317–326. doi: 10.1093/jpepsy/jsp060. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler intelligence scale for children-4th edition (WISC-IV) San Antonio, TX: Harcourt Assessment; 2003. [Google Scholar]
- Wells KC, Epstein JN, Hinshaw SP, Conners CK, Klaric J, Abikoff HB, Hechtman L. Parenting and family stress treatment outcomes in attention deficit hyperactivity disorder (ADHD): An empirical analysis in the MTA study. Journal of Abnormal Child Psychology. 2000;28:543–553. doi: 10.1023/A:1005131131159. [DOI] [PubMed] [Google Scholar]
- Wells-Parker E, Miller DI, Topping JS. Development of control-of-outcome scales and self-efficacy scales for women in four life roles. Journal of Personality Assessment. 1990;54:564–575. doi: 10.1080/00223891.1990.9674020. [DOI] [PubMed] [Google Scholar]
- Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: A meta-analytic review. Neurotherapeutics. 2012;9:490–499. doi: 10.1007/s13311-012-0135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelazo PD, Carlson SM. Hot and cool executive function in childhood and adolescence: Development and plasticity. Child Development Perspectives. 2012;6:354–360. doi: 10.1111/j.1750-8606.2012.00246.x. [DOI] [Google Scholar]


