Abstract
Objective
To test whether emergency contraception use in reproductive-aged cancer survivors is higher than in the general U.S. population and evaluate factors associated with use among survivors.
Design
A retrospective cohort study compared emergency contraception use between cancer survivors in the Reproductive Window Study on ovarian function after cancer and the general population in the 2006–2010 National Survey for Family Growth. In cross-sectional analysis of survivors, multivariable models tested associations between participant characteristics and emergency contraception use.
Setting
Participants from population-based cancer registries, physician and advocacy group referrals
Patients
616 female cancer survivors ages 18–40
Intervention
None
Main outcome
Self-reported emergency contraception use
Results
Mean age of survivors was 33.4+4.7, at a mean of 7.5 years since diagnosis. Breast (22%), Hodgkin lymphoma (18%) and leukemia (8%) were the most common cancers. Since diagnosis, 156 (25.3%) used emergency contraception, 60% because of not contracepting. Age-adjusted prevalence of use was higher in survivors than the general population (28.3% [95%CI 24.7–31.9] versus 12.0% [95%CI 11.1–12.9], p<0.001). In multivariable analysis among survivors, non-white race (PR 1.3, 95%CI 1.0–1.8, p=0.05), breast cancer (PR 0.6, 95 CI 0.4–1.0, p=0.04), partnered relationship (PR 0.6, 95%CI 0.5–0.9, p=0.003) and older age (age 36–40 versus 31–35) (PR 0.7, 95%CI 0.5–1.0, p=0.05) were associated with emergency contraception.
Conclusions
Female young adult cancer survivors were significantly more likely to use emergency contraception compared to the general population. Populations including non-white survivors have a higher risk, suggesting differences in family planning care. Strategies to improve contraception and decrease the need for emergency contraception are needed.
Keywords: emergency contraception, family planning, young adult cancer survivors, cancer survivorship
Introduction
Prevention of unintended pregnancy contributes to improved health outcomes for women and children.(1) For the estimated 360,000 female young adult cancer survivors who are ages 15 to 39 and live in the United States, family planning and use of highly effective contraception are of particular importance. While many young adult cancer survivors underwent therapies that increase infertility risk, the majority of survivors maintain fertility.(2–4) This population faces higher pregnancy health risks than women without a history of cancer.(5–7) Moreover, social and cancer-specific milestones may delay cancer survivors’ readiness for pregnancy, thus necessitating effective family planning methods.(8)
Contraception is a major concern for many female young adult cancer survivors.(9, 10) Yet, rates of contraception and use of highly effective contraceptive methods are lower in cancer survivors than in the general population.(11–13) While unintended pregnancy rates are largely unknown, cohort studies have described pregnancy termination rates ranging from 8–20% in female cancer survivors, and some data show higher pregnancy termination rates in cancer survivors compared to their siblings.(6, 14, 15)
Emergency contraception refers to contraceptives used after sexual intercourse to prevent pregnancy. Emergency contraception can be used because of unprotected intercourse, concerns about contraceptive failure, and/or incorrect contraceptive use. Levonorgestrel, ulipristal, combined oral contraceptive pills and copper intrauterine devices (IUD) are methods of emergency contraception.(16) Used within 5 days of unprotected intercourse, emergency contraception can prevent up to 95% of pregnancies; however, emergency contraception is not the optimal or most effective approach to family planning. Currently, there are no restrictions on emergency contraception use by women with cancer, but there is a dearth of data on their uptake in this population.(17)
This study compared prevalence of emergency contraception use in female young adult cancer survivors and women in the general U.S. population. We hypothesized that utilization would be higher in cancer survivors than the general population. Secondarily, we examined participant characteristics associated with emergency contraception use and hypothesized higher rates of use with younger age and non-hormone responsive cancer types.
Materials and methods
Study population
A retrospective cohort study was conducted using patient-reported data from the Reproductive Window Study, a cross-sequential study on ovarian function in cancer survivors. Eligibility criteria for the Reproductive Window Study included: cancer diagnosis between ages 15–35, ages 18–40 at study enrollment, completion of primary cancer treatment, and presence of at least one ovary. The following cancer types were included: breast, blood and leukemia, lymphoma, gynecologic (cervix, uterus, ovary), intestines, gall bladder, pancreas, bone, soft tissue tumor of bone/fat, skin, and thyroid. For the current analysis on emergency contraception utilization, we included Reproductive Window Study participants who were recruited between March 2015 and May 2017, had a uterus, and reported sexual activity with a male partner in their lifetime. Using questions from the National Survey of Family Growth, sexual orientation and prior vaginal sexual intercourse were ascertained to exclude participants who had not had vaginal sexual intercourse with a male partner and would therefore not be at risk for unintended pregnancy. Participants were recruited from the California and Texas Cancer Registries (38.1%), University of California, San Diego Health System (27.8%), cancer advocacy organizations (9.7%), physician referrals (5.5 %), and other sources (18.8%). The State of California Committee for the Protection of Human Subjects and the institutional review boards at the University of California, San Diego and the Texas Department of State Health Services approved this study.
Data collection
Participants provided informed consent and completed an online questionnaire to report demographics, cancer and treatment characteristics, partner status, pregnancy history, hysterectomy and/or oophorectomy, and family planning behavior. Family planning behavior, including emergency contraception use, was assessed using questions derived from the National Survey of Family Growth (NSFG), 2006–2010 cycle.(18, 19) Reproductive Window Study participants were asked to report the number of times they had used emergency contraception since their cancer diagnosis and reasons for use in order to assess emergency contraception utilization since cancer diagnosis. Participants could select from three standardized choices as to why they used emergency contraception: did not use birth control, worry that the birth control method did not work, and some other reason.
Emergency contraception utilization in cancer survivors was compared to that of the general population reported by the 2006–2010 NSFG Cycle. The NSFG is a population-based study conducted by the Centers for Disease Control and Prevention to study family life, marriage and divorce rates, pregnancy and infertility rates, use of contraception, and overall men and women’s health in the United States. From 2006–2010, a nationally representative sample of 12,279 women ages 15–44 years was interviewed using standardized questionnaires with a 78% response rate.(20) During the survey, women were asked to report the number of times they had used emergency contraception and reasons for use, in order to assess lifetime utilization of emergency contraception. For the current analyses, we restricted the NSFG dataset to those with ages 18–40, comparable to the age range in the Reproductive Window Study.
Statistical analysis
Descriptive characteristics were calculated using frequency and percentages. Emergency contraception utilization was categorized as ever use and use once, twice or three or more times. The primary comparison was emergency contraception utilization between cancer survivors and women in the general U.S. population. Then, a cross-sectional analysis was conducted within cancer survivors to determine which participant characteristics were associated with increased emergency contraception utilization since cancer diagnosis.
To compare age-adjusted utilization of emergency contraception between cancer survivors and the general U.S. population, NSFG sampling weights were applied, and the cancer survivor population was age-standardized using the NSFG population as the standard.(21) For the general population, emergency contraception utilization was calculated among women who had ever had vaginal, heterosexual intercourse, regardless of current contraception or pregnancy status. (22) Accordingly, the cancer survivor emergency contraception utilization rate was calculated from participants who reported prior vaginal, heterosexual intercourse. SAS PROC SURVEYFREQ was used to estimate proportions, 95% confidence intervals and p-values for comparisons between cancer survivors and the general U.S. population.
Within the cancer survivor population, multivariable log-binomial regression models were used to estimate associations between participant characteristics and emergency contraception utilization, while adjusting for confounding.(23, 24) Variables associated with emergency contraception use at p≤0.05 were included in multivariable models. Statistical significance was set at p≤0.05. All analyses were conducted using SAS software v9.4 (Cary, NC).
Results
Six hundred and sixteen cancer survivors were included (Figure 1, Table 1). The mean age ±standard deviation at enrollment was 33.4±4.7 years, and the mean number of years since cancer diagnosis was 7.5± 5.3 years. The majority of participants were white (73%), college educated (75%), and in partnered relationships (72%). Twenty-four percent of participants reported Hispanic ethnicity. The most common cancer types were breast (22%), Hodgkin lymphoma (18%) and leukemia (8%). In this cohort, 68% underwent surgery, 62% underwent chemotherapy, 50% underwent radiation therapy and 4% received bone marrow or stem cell transplants.
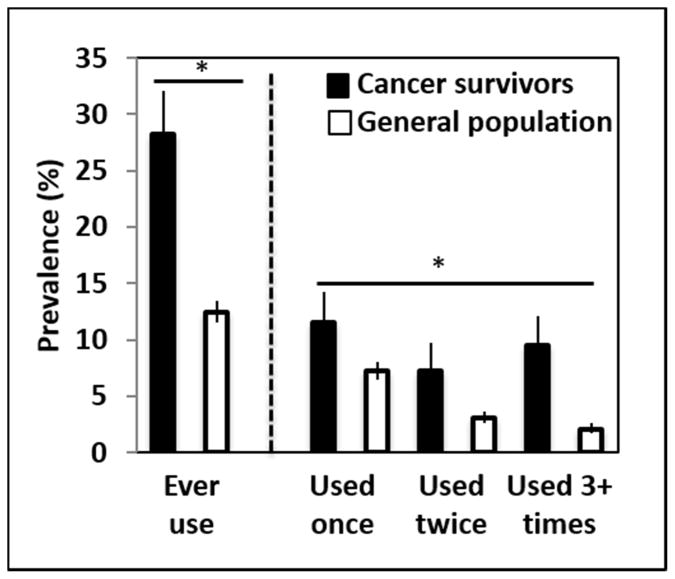
Figure 1.
Prevalence and 95% confidence interval of ever use and number of uses of emergency contraception in cancer survivors and the general U.S. population. Proportions reflect age-adjusting the cancer survivor population to match the age distribution of the NSFG population restricted to ages 18 to 40, applying sampling weights to the NSFG to yield U.S. population estimates. *p<0.001 by Chi-square test of proportions.
Table 1.
Descriptive characteristics of female cancer survivors and women in the general U.S. population
| Characteristic | Cancer Survivors No. (%)a (n=616) | General Population No. (%)b (n= 47709) |
|---|---|---|
|
| ||
| Current age (y) | ||
| 18 – 24 | 35 (5.8) | 15,005 (31.5) |
| 25 – 30 | 138 (23.0) | 12,490 (26.2) |
| 31 – 35 | 215 (35.8) | 9,277 (19.5) |
| 36 – 40 | 213 (35.4) | 10,824 (22.7) |
|
| ||
| Race | ||
| White | 451 (73.2) | 35,249 (73.9) |
| Black or African American | 14 (2.3) | 7,219 (15.1) |
| Other | 151 (24.5) | 5,241 (11) |
|
| ||
| Hispanic Ethnicity | 145 (23.5) | 8,174 (17.1) |
|
| ||
| BMI (kg/m2) | ||
| <18.5 | 151 (25.2) | 8,241 (17.5) |
| 18.5–24.9 | 262 (43.7) | 15,888 (33.6) |
| 25–29.9 | 85 (14.2) | 10,359 (21.9) |
| > 30 | 101 (16.9) | 12,729 (27.0) |
|
| ||
| Education | ||
| Did not complete college | 155 (25.2) | 34,835 (73.0) |
| College graduate and beyond | 461 (74.8) | 12,874 (27.0) |
|
| ||
| Income | ||
| <$51,000 | 158 (27.2) | 28,470 (59.7) |
| ≥$51,000 | 422 (72.8) | 19,239 (40.3) |
|
| ||
| Partnered Relationship | 446 (72.4) | 26,741 (56) |
|
| ||
| Ever been pregnant | 312 (50.6) | 30,800 (64.6) |
|
| ||
| Ever had live birth | 262 (42.5) | 27,287 (57.2) |
|
| ||
| Years since cancer diagnosis | - | |
| ≤2 | 74 (12.0) | - |
| >2–5 | 158 (25.6) | - |
| >5 | 384 (62.3) | - |
|
| ||
| Cancer Diagnosisc | - | |
| Breast | 137 (22.2) | - |
| Leukemia and lymphomas | 206 (33.4) | - |
| Gynecologic | 48 (7.8) | - |
| Gastrointestinal | 15 (2.4) | - |
| Bone and soft tissue tumors | 38 (6.2) | |
| Skin | 24 (3.9) | - |
| Thyroid | 148 (24.0) | - |
|
| ||
| Surgery for cancer | 418 (67.9) | - |
|
| ||
| Chemotherapy | 384 (62.3) | - |
|
| ||
| Radiation therapy | 305 (49.5) | - |
|
| ||
| Bone marrow or stem cell transplant | 27 (4.4) | - |
Numbers do not sum up to 616 for some variables due to missing data.
General population as reported by the National Survey for Family Growth 2006–2010 cycle. Numbers are expressed in thousands and are based on applying sampling weights to 9652 respondents aged 18–40 years.(20) Cancer-related variables were not collected by the survey.
Gynecologic cancer = cervix, uterus, ovary; Gastrointestinal cancer = pancreas, gallbladder, stomach, small intestine, colon, appendix, rectum
Since their cancer diagnosis, 156 cancer survivors (25.3%) reported use of emergency contraception; among these survivors, 40% used emergency contraception once, 26% used it twice, and 34% used it at least three times. The self-reported reasons for emergency contraception use were unprotected intercourse (60%), fear of contraceptive method failure (43%), and some other reason (6%).
Age-adjusted comparisons of emergency contraception utilization in cancer survivors and the general population are summarized in Figure 2. Cancer survivors were more likely to use emergency contraception than the general population (28.3% [95% CI 24.8–32.1] versus 12.5% [95% CI 11.5–13.5], p<0.001). Additionally, cancer survivors had higher rates of repeat use of emergency contraception when compared to the general population (p<0.001), with 16.8% reporting use 2+ times compared to 5.2% in the general U.S. population.
In bivariable analyses among cancer survivors, several demographic, cancer and reproductive characteristics differed between women who used emergency contraception since cancer diagnosis and women who did not use emergency contraception (Table 2). Survivors who reported emergency contraception use were younger than those who reported no use (p<0.001). Survivors who used emergency contraception were also more likely to self-report a non-white race (34.0% versus 24.3%, p=0.02) and Hispanic ethnicity (28.9% versus 21.7%, p=0.07), compared to non-users. Current income, education, and body mass index were not related to emergency contraception use.
Table 2.
Participant characteristics by emergency contraception use in cancer survivors (n=616)a
| Characteristic | Emergency Contraception Use No. (%) (N=156) | No Emergency Contraception Use No. (%) (N=460) | P-value |
|---|---|---|---|
|
| |||
| Current age (y) | <0.001 | ||
| 18 – 24 | 11 (7.2) | 24 (5.4) | |
| 25 – 30 | 55 (36.2) | 83 (18.5) | |
| 31 – 35 | 51 (33.6) | 164 (36.5) | |
| 36 – 41 | 35 (23.0) | 178 (39.6) | |
|
| |||
| Race | 0.02 | ||
| White | 103 (66.0) | 348 (75.7) | |
| Black or African American | 7 (4.5) | 7 (1.5) | |
| Other | 46 (29.5) | 105(22.8) | |
|
| |||
| Hispanic ethnicity | 45 (28.9) | 100 (21.7) | 0.07 |
|
| |||
| BMI (kg/m2) | 0.14 | ||
| <18.5 | 40 (26.9) | 111 (24.7) | |
| 18.5–24.9 | 72 (48.3) | 190 (42.2) | |
| 25–29.9 | 13 (8.7) | 72 (16.0) | |
| > 30 | 24 (16.1) | 77 (17.1) | |
|
| |||
| Education | 0.79 | ||
| Did not complete college | 38 (24.4) | 117 (25.4) | |
| College graduate and beyond | 118 (75.6) | 343 (74.6) | |
|
| |||
| Income | 0.32 | ||
| <$51,000 | 45 (28.8) | 113 (24.6) | |
| ≥$51,000 | 105 (67.3) | 317 (68.9) | |
|
| |||
| Years since cancer diagnosis | 0.04 | ||
| ≤2 | 11 (7.1) | 63 (13.7) | |
| >2–5 | 36 (23.1) | 122 (26.5) | |
| >5 | 109 (69.9) | 275 (59.8) | |
|
| |||
| Cancer diagnosisb | 0.001 | ||
| Breast | 18 (11.5) | 119 (25.9) | |
| Leukemia and lymphomas | 52 (33.3) | 154 (33.5) | |
| Gynecologic | 14 (9.0) | 34 (7.4) | |
| Gastrointestinal | 3 (1.9) | 12 (2.6) | |
| Bone and soft tissue tumors | 14 (9.0) | 24 (5.2) | |
| Skin | 8 (5.1) | 16 (3.5) | |
| Thyroid | 47 (30.1) | 101 (22.0) | |
|
| |||
| Surgery for cancer | 100 (64.1) | 318 (69.1) | 0.25 |
|
| |||
| Chemotherapy | 87 (55.8) | 297 (64.6) | 0.05 |
|
| |||
| Radiation therapy | 72 (46.2) | 233 (50.7) | 0.33 |
|
| |||
| Bone marrow or stem cell transplant | 4 (2.6) | 23 (5.0) | 0.09 |
|
| |||
| Partnered relationship | 91 (58.3) | 355 (77.2) | <0.001 |
|
| |||
| Ever been pregnant | 64 (41.0) | 248 (53.9) | 0.005 |
|
| |||
| Ever had live birth | 50 (32.1) | 212 (46.1) | 0.002 |
Numbers do not sum up to 616 for some variables due to missing data.
Gynecologic cancer = cervix, uterus, ovary; Gastrointestinal cancer = pancreas, gallbladder, stomach, small intestine, colon, appendix, rectum
Among cancer characteristics, emergency contraception users were less likely to be breast cancer survivors (11.5% versus 25.9%, p=0.002) and less likely to have had prior chemotherapy (51.2% vs. 64.5%, p=0.05) than non-users. Surgery, radiation and stem cell transplant were not associated with use of emergency contraception. Among reproductive characteristics, emergency contraception users were less likely to be in a partnered relationship (58.3 vs. 77.2%, p<0.0001), have a prior pregnancy, or a prior live birth than non-users.
Crude and adjusted prevalence ratios were estimated using log-binomial regression models (Table 3). These models included current age, race, cancer type, chemotherapy, partnered relationship and prior live birth. Due to collinearity of years since cancer diagnosis and age, as well as prior live birth with prior pregnancy, years since cancer diagnosis and prior pregnancy were not included. Estimates from the multi-variable model were attenuated compared to unadjusted estimates. In the adjusted model, non-white race (prevalence ratio [PR] 1.3, 95% CI 1.0–1.7, p=0.05) was significantly associated with higher use of emergency contraception. Breast cancer diagnosis (PR 0.6, 95% CI 0.4–1.0, p=0.04), being in a partnered relationship (PR 0.6, 95% CI 0.5–0.9) and older age (age 36–40 versus age 31–35) (PR 0.7, 95% CI 0.5–1.0, p=0.05) were significantly associated with lower prevalence of reported emergency contraception use.
Table 3.
Unadjusted and adjusted prevalence ratios (PR) for ever use of emergency contraception since cancer diagnosis among cancer survivors (n=616)
| Unadjusted PR (95% CI) | p-value | Adjusted PR (95% CI) | p-value | |
|---|---|---|---|---|
|
| ||||
| Race | ||||
| Non-white | 1.4 (1.1–1.9) | 0.02 | 1.3 (1.0–1.7) | 0.05 |
| White | Reference | Reference | ||
|
| ||||
| Current age | ||||
| 18–24 | 1.3 (0.8–2.4) | 0.31 | 0.9 (0.5–1.6) | 0.71 |
| 25–30 | 1.7 (1.2–2.3) | 0.001 | 1.4 (1.0–1.9) | 0.06 |
| 31–35 | Reference | - | Reference | - |
| 36–40 | 0.7 (0.5–1.0) | 0.06 | 0.7 (0.5–1.0) | 0.05 |
|
| ||||
| Breast cancer diagnosis | 0.5 (0.3–0.7) | <0.001 | 0.6 (0.4–1.0) | 0.04 |
| Other cancer diagnosis | Reference | Reference | ||
|
| ||||
| Chemotherapy | 0.8 (0.6–1.0) | 0.05 | 0.8 (0.6–1.0) | 0.09 |
| No chemotherapy | Reference | Reference | ||
|
| ||||
| Partnered relationship | 0.5 (0.4–0.7) | <0.001 | 0.6 (0.5–0.9) | 0.003 |
| Not partnered | Reference | Reference | ||
|
| ||||
| Ever live birth | 0.6 (0.5–0.9) | 0.003 | 0.9 (0.7–1.3) | 0.67 |
| Never live birth | Reference | Reference | ||
Discussion
For female young adult cancer survivors, prevention of unintended pregnancy is important to maternal and child health. While emergency contraception use should reduce the risk of unintended pregnancy, emergency contraception is not the most effective method for preventing pregnancy. This study showed significantly higher use of emergency contraception in reproductive-aged cancer survivors when compared to women in the general U.S. population. Specifically, one out of four cancer survivors reported emergency contraception use since their cancer diagnosis. In addition to the high proportion of survivors reporting emergency contraception use, the majority of them reported multiple episodes of use of emergency contraception. Taken together with non-contraception as the primary reason for emergency contraception use, these data support a clinically important need to improve family planning services in this population. Moreover, there are populations of cancer survivors who may merit more clinical intervention, including women who are non-white, have had breast cancer, and/or are not in a partnered relationship.
There are limited prior data on rates of emergency contraception use in cancer survivors. In a separate, smaller cohort of 289 reproductive-aged female cancer survivors, the absolute rate of use was around 10%, lower than our estimated 28.3%.(11) The difference with this cohort may be attributed to population differences. The prior cohort was recruited from fertility preservation programs and young adult cancer advocacy groups, compared to the current cohort, which included substantial recruitment from two population-based state cancer registries and is likely to be more generalizable.
Higher use of emergency contraception in cancer survivors was hypothesized based on prior findings that cancer survivors contracept less frequently and use less effective methods compared to the general population.(11) Accordingly, we observed that non-contraception was the most frequent reason for using emergency contraception (60%), but fear of contraceptive method failure was also highly cited (43%) in why emergency contraception was used. There are also prior data demonstrating that accessing family planning care is associated with higher uptake of more effective methods of contraception.(11) The clinical relevance of these two observations is that improved family planning care is needed, as there are medically safe and effective long-acting reversible contraception (LARC) methods including intrauterine devices (IUD) and implants that can be used in all cancer survivors in need of birth control, including women with estrogen-sensitive cancers. (16) LARC methods require accessing gynecologic care, a challenge in the young cancer survivor population that has significant loss to follow up care.1 As use of LARCs remains limited in this population, a potential intervention associated with improving LARC uptake includes family planning care.(13) Importantly, reproductive specialists who see young cancer survivors for fertility are also trained gynecologists and thus have an opportunity to counsel on effective contraception alongside fertility preservation. We hypothesize that increasing exposure of survivors to family planning services may ultimately help to decrease the need for emergency contraception by improving uptake of effective contraception.
Several demographic, cancer and reproductive characteristics were associated with emergency contraception use, identifying populations at increased risk. In the general U.S. population, non-Hispanic white women (11%) and Hispanic women (11%) were more likely to have ever used emergency contraception compared to non-Hispanic black women (7.9%), a finding inconsistent with results of the present study.(22) In the general population, differences in emergency contraception use by race and ethnicity may have arisen in part due to confounding by sociodemographic characteristics such as income and education. In contrast, our population had high rates of completing college education and higher income attainment, limiting confounding by these factors. Alternatively, differences in contraceptive knowledge by race and ethnicity may contribute to differential use of emergency contraception. For example, racial and ethnic minority female Veterans had less contraceptive knowledge than white female Veterans in all knowledge domains, and contraceptive knowledge is associated with improved behavior.(25, 26) The observation that age was related to emergency contraception use in cancer survivors was consistent with data from the general U.S. population; only 5% of women aged 30–44 years had ever used emergency contraception compared to 23% of women aged 20–24.(22)
The finding that breast cancer diagnosis was related to less emergency contraception use may be due to patient concern of exposures to estrogen- or progestin-based emergency contraception methods in the setting of hormone receptor-sensitive tumors. (27) Within the US Medical Eligibility for Contraceptive Use (USMEC), emergency contraception is designated as category 1, no restriction, or 2, benefits outweigh risks, for women with non-hormonally mediated cancer types, rendering breast cancer patients with hormone receptive-negative disease eligible.(16) Moreover, the copper IUD, a non-hormonal method, can be used as effective and safe emergency contraception method in all breast cancer survivors with continued long-term efficacy. These USMEC recommendations are important to discuss with breast cancer survivors and their healthcare providers.
Prior chemotherapy was associated with decreased emergency contraception use, with attenuation in multivariable analysis. We recently reported that prior chemotherapy was also associated with non-contraception, and in a mediation model, 59% of the association between prior chemotherapy and contraception was explained by patient-reported perception of infertility.(28) We did not look at the relationship between current perception of infertility and prior use of emergency contraception because of temporality, but we speculate that prior chemotherapy may render patients to perceive themselves as being infertile and hence result not only in increased non-contraception, but also in decreased use of emergency contraception.
Strengths of this study include recruitment of reproductive-aged cancer survivors from two large state cancer registries. Our sample included a sizeable Hispanic population, but had lower representation of African American survivors. Utilization of questions derived from a long-standing national survey of reproductive health enabled comparisons between cancer survivors and contemporary reproductive-aged women in the U.S., although ascertaining responses via web-based questionnaires in this study may have garnered different chances of disclosure compared to in-person NSFG interviews. Several limitations should be discussed. We lack data on the rate of unintended pregnancy in cancer survivors and how much that is decreased by emergency contraception use. Among cancer survivors we assessed emergency contraception use only since cancer diagnosis, inherently less than “lifetime use” as determined by the NSFG for the general U.S. population. Despite the shorter opportunity for use by cancer survivors, we observed higher emergency contraception use compared to the general population and thus the gap between the two groups may be larger than what the current study found. While we age-adjusted the cancer survivor population to match the general population, because of smaller numbers, we were not able to similarly address differences between the study samples for race, income and education. In considering how these differences can bias the results, with regard to race, because black survivors were more likely to use emergency contraception than white survivors, the smaller proportion of black survivors compared to the proportion of black white women in the general population likely resulted in a lower emergency contraception use estimate among survivors related to race; the resulting uncontrolled confounding would bias results toward the null. Higher education attainment, often collinear with income, is associated with more emergency contraception use in the general population. Although we did not observe this association among cancer survivors, it remains possible that higher emergency contraception use in cancer survivors is in part due to higher education attainment. Finally, some caution regarding generalizability is to be noted for a population recruited for a study on reproductive health.
Conclusions
Our study provides novel evidence on emergency contraception use in female young adult survivors when compared to women in the general U.S. population. Improving family planning counseling, including at the time of fertility preservation counseling by reproductive specialists, to increase use of effective contraception and decrease need for emergency contraception in order to prevent unintended pregnancy is both needed and desired by this vulnerable patient population. Additionally, our study showed emergency contraception use was higher in populations of cancer survivors, including non-white survivors. As emergency contraception use follows non-contraception or inadequate contraception, there may be racial differences in family planning care among female young adult cancer survivors.
Acknowledgments
Funding: The study was funded by NIH HD080952-04.
Dr. Dietz is employed by bluebird bio, Inc, which has not sponsored or otherwise been involved in this research.
Footnotes
Conflict of Interest: There are no conflicts of interest to disclose for any authors.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature. Stud Fam Plann. 2008;39:18–38. doi: 10.1111/j.1728-4465.2008.00148.x. [DOI] [PubMed] [Google Scholar]
- 2.Barton SE, Najita JS, Ginsburg ES, Leisenring WM, Stovall M, Weathers RE, et al. Infertility, infertility treatment, and achievement of pregnancy in female survivors of childhood cancer: a report from the Childhood Cancer Survivor Study cohort. Lancet Oncol. 2013;14:873–81. doi: 10.1016/S1470-2045(13)70251-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Green DM, Sklar CA, Boice JD, Jr, Mulvihill JJ, Whitton JA, Stovall M, et al. Ovarian failure and reproductive outcomes after childhood cancer treatment: results from the Childhood Cancer Survivor Study. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2009;27:2374–81. doi: 10.1200/JCO.2008.21.1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chow EJ, Stratton KL, Leisenring WM, Oeffinger KC, Sklar CA, Donaldson SS, et al. Pregnancy after chemotherapy in male and female survivors of childhood cancer treated between 1970 and 1999: a report from the Childhood Cancer Survivor Study cohort. Lancet Oncol. 2016;17:567–76. doi: 10.1016/S1470-2045(16)00086-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shliakhtsitsava K, Romero SAD, Dewald SR, Su HI. Pregnancy and child health outcomes in pediatric and young adult leukemia and lymphoma survivors: a systematic review. Leuk Lymphoma. 2018;59:381–97. doi: 10.1080/10428194.2017.1352097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Green DM, Whitton JA, Stovall M, Mertens AC, Donaldson SS, Ruymann FB, et al. Pregnancy outcome of female survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Am J Obstet Gynecol. 2002;187:1070–80. doi: 10.1067/mob.2002.126643. [DOI] [PubMed] [Google Scholar]
- 7.Anderson C, Engel SM, Mersereau JE, Black KZ, Wood WA, Anders CK, et al. Birth Outcomes Among Adolescent and Young Adult Cancer Survivors. JAMA oncology. 2017;3:1078–84. doi: 10.1001/jamaoncol.2017.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dominick SA, Whitcomb BW, Gorman JR, Mersereau JE, Chung K, Su HI. Factors associated with pregnancy attempts among female young adult cancer survivors. J Cancer Surviv. 2014;8:571–9. doi: 10.1007/s11764-014-0369-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karaoz B, Aksu H, Kucuk M. A qualitative study of the information needs of premenopausal women with breast cancer in terms of contraception, sexuality, early menopause, and fertility. Int J Gynaecol Obstet. 2010;109:118–20. doi: 10.1016/j.ijgo.2009.11.027. [DOI] [PubMed] [Google Scholar]
- 10.Murphy D, Klosky JL, Termuhlen A, Sawczyn KK, Quinn GP. The need for reproductive and sexual health discussions with adolescent and young adult cancer patients. Contraception. 2013;88:215–20. doi: 10.1016/j.contraception.2012.08.041. [DOI] [PubMed] [Google Scholar]
- 11.Dominick SA, McLean MR, Whitcomb BW, Gorman JR, Mersereau JE, Bouknight JM, et al. Contraceptive Practices Among Female Cancer Survivors of Reproductive Age. Obstet Gynecol. 2015;126:498–507. doi: 10.1097/AOG.0000000000000963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quinn MM, Letourneau JM, Rosen MP. Contraception after cancer treatment: describing methods, counseling, and unintended pregnancy risk. Contraception. 2014;89:466–71. doi: 10.1016/j.contraception.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 13.Maslow BS, Morse CB, Schanne A, Loren A, Domchek SM, Gracia CR. Contraceptive use and the role of contraceptive counseling in reproductive-aged women with cancer. Contraception. 2014;90:79–85. doi: 10.1016/j.contraception.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Winther JF, Boice JD, Jr, Svendsen AL, Frederiksen K, Olsen JH. Induced abortions in Danish cancer survivors: a population-based cohort study. Journal of the National Cancer Institute. 2009;101:687–9. doi: 10.1093/jnci/djp064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gawade PL, Oeffinger KC, Sklar CA, Green DM, Krull KR, Chemaitilly W, et al. Lifestyle, distress, and pregnancy outcomes in the Childhood Cancer Survivor Study cohort. Am J Obstet Gynecol. 2015;212:47e1–10. doi: 10.1016/j.ajog.2014.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.U.S. Medical Eligibility Criteria for Contraceptive Use. Morbidity and Mortality Weekly Report. 3. Vol. 65. Center for Disease Control and Prevention; 2016. [DOI] [PubMed] [Google Scholar]
- 17.Patel A, Schwarz EB Society of Family P. Cancer and contraception. Release date May 2012. SFP Guideline #20121. Contraception. 2012;86:191–8. doi: 10.1016/j.contraception.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 18.Prevention CfDCa. National Survey of Family Growth. Centers for Disease Control and Prevention: Centers for Disease Control and Prevention; 2017. 2006–2010:NSFG: Public Use Data Files, Codebooks, and Documentation. [Google Scholar]
- 19.National Comprehensive Cancer Network Guidelines for Treatment of Cancer by Site. In. Vol. 2017.
- 20.Lepkowski JM, Mosher WD, Davis KE, Groves RM, Van Hoewyk J. The 2006–2010 National Survey of Family Growth: sample design and analysis of a continuous survey. Vital Health Stat. 2010;2:1–36. [PubMed] [Google Scholar]
- 21.Jones JMW, Daniels K. Current contraceptive use in the United States, 2006–2010, and changes in patterns of use since 1995. National Health Statistics Reports. :1–25. [PubMed] [Google Scholar]
- 22.Daniels K, Jones J, Abma J. Use of emergency contraception among women aged 15–44: United States, 2006–2010. NCHS Data Brief. 2013:1–8. [PubMed] [Google Scholar]
- 23.Wacholder S. Binomial regression in GLIM: estimating risk ratios and risk differences. Am J Epidemiol. 1986;123:174–84. doi: 10.1093/oxfordjournals.aje.a114212. [DOI] [PubMed] [Google Scholar]
- 24.McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–3. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 25.Rosenfeld E, Callegari LS, Sileanu FE, Zhao X, Schwarz EB, Mor MK, et al. Racial and ethnic disparities in contraceptive knowledge among women veterans in the ECUUN study. Contraception. 2017;96:54–61. doi: 10.1016/j.contraception.2017.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frost JJ, Lindberg LD, Finer LB. Young adults’ contraceptive knowledge, norms and attitudes: associations with risk of unintended pregnancy. Perspect Sex Reprod Health. 2012;44:107–16. doi: 10.1363/4410712. [DOI] [PubMed] [Google Scholar]
- 27.Mody SK, Panelli DM, Hulugalle A, Su HI, Gorman JR. Contraception concerns, utilization and counseling needs of women with a history of breast cancer: a qualitative study. Int J Womens Health. 2017;9:507–12. doi: 10.2147/IJWH.S136120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hadnott TSS, Medica A, Whitcomb B, Su HI. American Society of Reproductive Medicine. 2017. Perception of Fertility Potential is Associated with Contraceptive Behavior in Female Young Adult Cancer Survivors. [Google Scholar]