Abstract
Biventricular pacing has revolutionised the treatment of heart failure in patients with sinus rhythm and left bundle branch block; however, left ventricular-lead placement is not always technically possible. Furthermore, biventricular pacing does not fully normalise ventricular activation and, therefore, the ventricular resynchronisation is imperfect. Right ventricular pacing for bradycardia may cause or worsen heart failure in some patients by causing dyssynchronous ventricular activation. His bundle pacing activates the ventricles via the native His-Purkinje system, resulting in true physiological pacing, and, therefore, is a promising alternate site for pacing in bradycardia and traditional CRT indications in cases where it can overcome left bundle branch block. Furthermore, it may open up new indications for pacing therapy in heart failure, such as targeting patients with PR prolongation, but a narrow QRS duration. In this article we explore the physiology, technology and potential roles of His bundle pacing in the prevention and treatment of heart failure.
Keywords: His bundle, pacing therapy, heart failure, left bundle branch block reversal, bradycardia pacing, atrial fibrillation
His bundle pacing in humans was first described in 1970 by Narula et al.[1] They demonstrated that it was possible to stimulate the His bundle to produce normal physiological ventricular activation via the His-Purkinje system. However, the first report of permanent His bundle pacing, by Deshmukh et al., did not occur until 2000.[2] In that study, His pacing was performed in a series of patients with impaired left ventricular systolic function and AF prior to atrioventricular (AV) node ablation.
The lack of dedicated tools for implantation initially hampered enthusiasm; however, the development of specially designed sheaths and leads for delivering permanent His bundle pacing has led to a renewed interest. The potential role of His pacing in heart failure is large: it may prevent the development of pacing-induced cardiomyopathy; it may be used as an alternative to biventricular pacing in patients with heart failure and left bundle branch block (LBBB); and it may extend pacing therapy in heart failure to patients with narrow QRS and PR prolongation by providing AV synchrony without inducing ventricular dyssynchrony.
Anatomy of the His Bundle and Implant Technique
The bundle of His extends from the compact AV node to the membranous interventricular septum, and measures approximately 20 mm in length. The bundle is a cord-like structure made up of multiple strands, which, even before the branching, are predestined to become the right or left bundle branches. His bundle pacing can be achieved by placing the lead at the atrial portion against the septum.
The most commonly used lead for His bundle pacing is the 69 cm Select Secure™ 3830 (Medtronic). This is a non-stylet-driven active fixation lead. Importantly, the screw forms part of the tip electrode allowing penetration of the capsule of the bundle of His and, therefore, direct stimulation of the His bundle fibres. The lead can be delivered to the His bundle region using either the specially-designed non-deflectable His delivery sheath (C315 43 cm; Medtronic) or a deflectable sheath (C304 69 cm; Medtronic). Unlike traditional lead placement that primarily uses fluoroscopic guidance, His lead placement primarily uses electrical mapping. An electrogram from the lead tip is displayed using placement via either a lab electrophysiology system or a standard pacing system analyser.
A His signal is targeted, aiming for the local ventricular electrogram to be approximately twice the amplitude of the atrial signal (Figure 1). To confirm successful His capture, a 12-lead ECG is used to assess the QRS morphology with pacing. Criteria used to establish whether His capture has occurred are well described.[3] Recently-published data suggests thresholds of <2.5 at 1 ms should be achieved.[3] An increase in pacing threshold is observed in ~10 % of patients, leading to shorter battery duration. There is also a higher rate of lead revisions (6.7 %) due to loss of capture or increased threshold.[4]
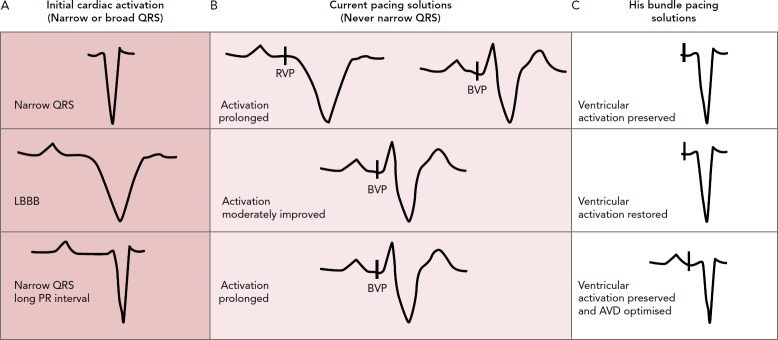
Figure 1: Electrical and Fluoroscopic Guidance for His Bundle Pacing.
Top: With electrical mapping a distinct, sharp His signal is found with a small atrial signal and large ventricular signal. Bottom: Fluoroscopic image of defibrillator with an atrial lead in the right atrial appendage, the defibrillator lead in the right ventricular apex and the His lead pacing the His bundle. A = atrium; H = his; V = right ventricle.
His bundle capture may be either selective or non-selective. With selective capture, only the His bundle fibres are stimulated and, therefore, activation occurs entirely via the His-Purkinje system. With non-selective capture both the His bundle fibres and local myocardium are captured. During non-selective capture a pseudo delta wave on the surface ECG is formed from local myocardial capture.
Indications
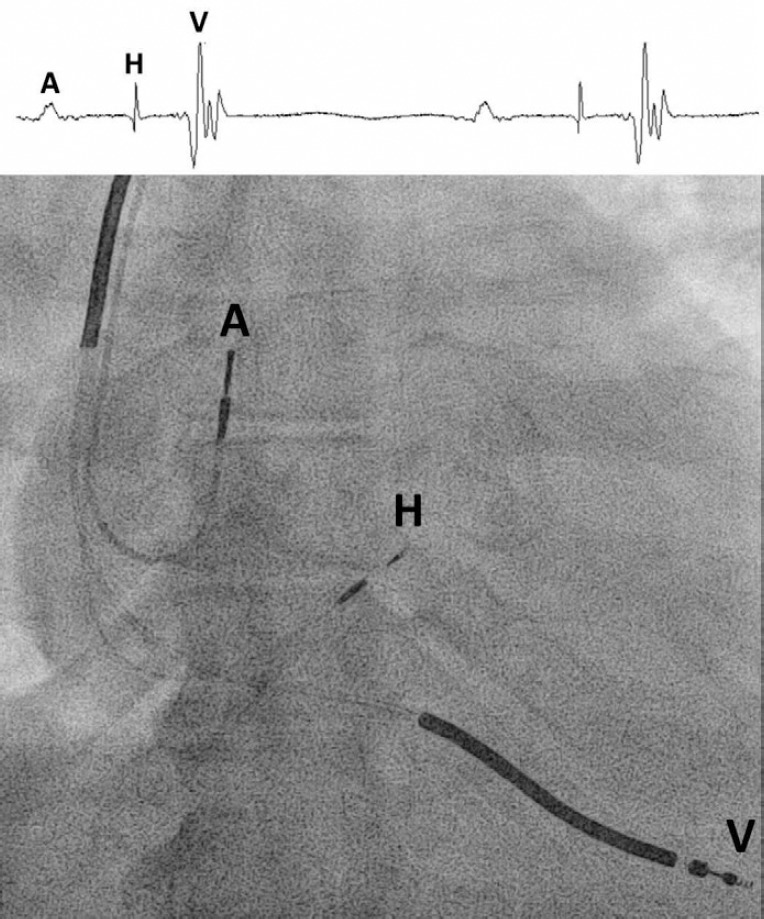
His pacing has the potential to provide better pacing solutions in several clinical situations compared with existing techniques. It may be useful in preventing pacing-induced cardiomyopathy, and pacing therapy may be an option for patients with existing heart failure in a range of settings (Figure 2).
Figure 2: Potential of His Bundle Pacing.
His bundle pacing across three classes of indications: (A) narrow QRS, (B) left bundle branch block (LBBB), and (C) long PR interval and narrow QRS. Right ventricular apical pacing (RVP) and biventricular pacing (BVP) do not completely restore narrow QRS. His bundle pacing fully maintains or restores narrow QRS and ventricular synchrony with atrioventricular delay optimisation.
His Pacing to Prevent Right Ventricular Pacing-induced Cardiomyopathy
Right ventricular apical pacing results in non-physiological dyssynchronous ventricular activation. This may lead to reverse ventricular remodelling and impaired cardiac function.[5–10] In the Dual Chamber and VVI Implantable Defibrillator (DAVID) trial, programming that promotes right ventricular pacing was associated with increased mortality and hospitalisations for heart failure in patients with a standard ICD indication, no pacing indication and impaired LVF.[5] Therefore, pacing algorithms have been developed to avoid right ventricular pacing.[11–13]
Biventricular pacing has been investigated as a way for mitigating the detrimental effects of ventricular pacing in patients who require high percentages of right ventricular pacing. In the Biventricular Versus Right Ventricular Pacing in Heart Failure Patients With Atrioventricular Block (BLOCK HF) study, biventricular pacing was associated with a lower incidence of death or urgent care visits for heart failure and significantly improved left ventricular end-diastolic volumes compared with right ventricular pacing.[14] This study included patients with heart failure, left ventricular ejection fraction <50 % and evidence of AV block.
However, in the Biventricular Pacing for Atrioventricular Block to Prevent Cardiac Desynchronisation (BIOPACE) trial, biventricular pacing failed to demonstrated superiority to right ventricular pacing in patients with normal LVF.[15] This was defined as left ventricular ejection fraction >45 %, but did not exclude patients with symptoms of heart failure. Therefore, right ventricular pacing should be avoided in patients with impaired LVF but biventricular pacing may not be the optimal way to prevent the adverse consequences since it does not produce true physiological pacing.[16] Furthermore, some patients with normal baseline ventricular function who received high percentages of right ventricular pacing develop pacing-induced cardiomyopathy.[17]
His pacing offers an elegant solution to potentially avoid pacing-induced deterioration in cardiac function. Since activation occurs via the normal conduction system, it does not result in ventricular dyssynchrony.[18] Compared with right ventricular pacing, His pacing results in improved LVF both acutely[19] and with chronic pacing.[20] Pacing-avoidance algorithms may be unnecessary, which has the advantage of allowing physiological AV delays to be programmed.
There have been no large randomised controlled-outcome studies comparing His pacing with right ventricular pacing; however, the available data are encouraging (Table 1). Data from observational studies show chronic His pacing, in patients with a bradycardia pacing indication, appears to be feasible and safe.[4] His pacing success rates have improved with the development of dedicated tools, and, in this population, successful His lead implantation occurs in 90 % of patients.
Table 1: Summary of Studies Investigating His Pacing for Heart Failure.
| Study | Total Patients and Inclusion Criteria | Study Design | His Pacing Success Rate | Outcomes | Summary |
|---|---|---|---|---|---|
| Bradycardia Pacing | |||||
| Zanon et al. 2008[22] | 12 | Non-randomised crossover study (3 months His pacing and 3 months RVP) | Only patients with confirmed His bundle pacing | Intra-patient myocardial perfusion (myocardial perfusion score) during His pacing compared to RVP | Myocardial perfusion score during His pacing was better than RVP |
| Catanzariti et al. 2013[18] | 26 | Non-randomised crossover study | Patients selected after successful His pacing established | Measurements of echocardiographic dyssynchrony parameters made during His pacing and RVP (intra-patient comparison) | Reduction of pacing-induced ventricular dyssynchrony with His pacing |
| Kronborg et al. 2014[20] | 38 (12 months His pacing and 12 months RVP) | Randomised double-blind crossover study | 84 % (32/38) Six patients had leads in high septal position and were still included in study | Left ventricular ejection fraction | Left ventricular ejection fraction was significantly higher during His pacing (55 % +/- 10 % versus 50 % +/- 11 %) |
| Vijayaraman et al. 2017[4] | 192 (94 His and 98 RVP) | Case control study | 80 % (75 from 94 attempted) | Death and heart failure hospitalisation | Death or heart failure was significantly lower in the His pacing group (32 % versus 53 %; HR 1.9) |
| Sharma et al. 2017[23] | 30 (post-prosthetic valve surgery) | Prospective observational | 93 % (28/30) | Feasibility of His pacing in this subgroup of patients | His bundle pacing was feasible and achieved pacing in 93 % of patients post-valve surgery |
| Shan et al. 2017[24] | 18 (upgrade from RVP to His pacing in RVP patients) | Prospective observational | 90 % (16/18) | Left ventricular ejection fraction, left ventricular end-diastolic dimensions, NYHA class and BNP | Reduced left ventricular end-diastolic dimensions and BNP. Improved ejection fraction and NYHA class |
| Abdelrahman et al. 2018[21] | 756 (332 His and 433 RVP) | Case control study | 92 % (302/332) | Death, heart failure hospitalisation and upgrade to BVP | Combined primary endpoint of death, heart failure hospitalisation and upgrade to BVP was significantly less in His pacing (HR 0.71) |
| Atrial Fibrillation (AV Node Ablation and His Pacing) | |||||
| Deshmukh et al. 2000[2] | 18 (dilated cardiomyopathy) | Prospective observational | 66 % (12/18) | Left ventricular dimensions and systolic function (ejection fraction and fractional shortening) | Reduced left ventricular dimensions and improved systolic function |
| Deshmukh et al. 2004[25] | 54 (cardiomyopathy and narrow QRS) | Prospective observational | 72 % (39/54) | Ejection fraction and functional class. In subset of 12 who also received an RV lead, comparison of cardiopulmonary exercise parameters between RVP and His pacing | Ejection fraction and NYHA class improved after His pacing. Improved exercise time and higher O2 uptake with His pacing compared to RV pacing |
| Occhetta et al. 2006[26] | 18 (AF and AV node ablation; 6 months RVP and 6 months His pacing) | Randomised blinded crossover | 89 % (16/18) | QOL score, NYHA, 6-minute walk test, left ventricular ejection fraction and ventricular synchrony | QOL score, NYHA, 6-minute walk test and left ventricular synchrony all improved with His pacing compared with both baseline and RVP |
| Vijayaraman et al. 2017[27] | 42 | Retrospective observational | 95 % (40/42) | Left ventricular ejection fraction and NYHA class | Left ventricular ejection fraction improved with His pacing and NYHA reduced |
| Huang et al. 2017[28] | 52 (all heart failure HFrEF and HFpEF) | Prospective observational | 80 % (42/52) | Left ventricular ejection fraction, left ventricular end-diastolic dimensions, NYHA class and use of diuretics at follow up | Increased left ventricular ejection fraction, reduced left ventricular end-diastolic dimensions, improved NYHA and reduced use of diuretics |
| Left Bundle Branch Block Reversal | |||||
| Barba-Pichardo et al. 2013[29] | 16 (failed coronary sinus cannulation) | Prospective observational | 56 % (13/16 achieved His pacing acutely, in 9/16 permanent His pacing was achieved) | Cardiac resynchronisation as defined by disappearance of LBBB, QRS duration shortening, improved NYHA class and echocardiographic parameters (left ventricular ejection fraction, left atrial and left ventricular dimensions) | Disappearance of LBBB, QRS shortening, improved NYHA class, improved echocardiographic parameters (reduced left atrial and left ventricular dimensions and increased left ventricular ejection fraction) with His pacing |
| Lustgarten etal. 2015[30] | 29 | Prospective crossover study (His and biventricular pacing) | 29 patients started, 21 QRS narrow acutely with His pacing, 17 randomised (high output, left ventricular lead failure), 12 completed follow up (complications: lead dislodged [His/left ventricular], failure to narrow, device dehiscence) | QOL assessment, left ventricular ejection fraction, NYHA and 6-minute walk test | Improved QOL, left ventricular ejection fraction, NYHA class and 6-minute walk test compared with baseline during both BVP and His pacing. No significant difference between the two modalities shown |
| Ajijola et al. 2017[31] | 21 | Retrospective observational | 76 % (16/21) | QRS duration, left ventricular ejection fraction, left ventricular dimensions and NYHA class | Reduced QRS duration and improved left ventricular ejection fraction, reduced left ventricular dimensions and reduced NYHA class with His pacing |
| Sharma et al. 2017[32] | 106 | Retrospective observational | 90% (95/106) | Left ventricular ejection fraction, NYHA and QRS duration | Improved left ventricular ejection fraction and NYHA. QRS duration shortening with His pacing |
AV = atrioventricular; BVP = biventricular pacing; HFpEF = heart failure with a preserved ejection fraction; HFrEF = heart failure with reduced ejection fraction; LBBB = left bundle branch block; NYHA = New York Heart Association; QOL = quality of life; RVP = right ventricular apical pacing.
A recent non-randomised case control study found that patients who received His pacing for a bradycardia indication had a lower incidence of death and hospitalisation for heart failure compared with a group of patients treated with right ventricular pacing.[21] A randomised controlled trial is now required to establish whether these encouraging results translate into clinical benefits in adequately-powered randomised control trials.
Heart Failure Patients with Atrial Fibrillation and Atrioventricular Node Ablation
His bundle pacing may deliver substantial benefits in patients with heart failure after AV node ablation for AF. In patients with AF and LBBB, the evidence for biventricular pacing is minimal, often limited to subgroup data from randomised controlled trials.[33] Observational data have suggested some benefit of AV node ablation and left ventricular lead implantation in this group to ensure 100 % biventricular pacing.[34,35] Permanent His bundle pacing may yet allow a more elegant solution if His bundle pacing allows reversal of LBBB.
Theoretically, His pacing is a better method for delivering pacing since the lead can be positioned distal to the ablation site, and can maintain normal conduction via the His-Purkinje system. This is also an option in patients with a narrow QRS where inadequate rate-controlled AF contributes to poor LVF.
Heart failure patients were the first group in which permanent His pacing was applied. Despite lacking dedicated tools for His pacing, Deshmukh et al. achieved successful His pacing in 60 % of patients and were able to successfully perform AV node ablation with the His lead in situ.[2] Improvements in left ventricular systolic function and left ventricular dimensions were observed.
Observational studies performed with dedicated tools for His pacing have found a higher rate of implant success (Table 1). A recent study successfully achieved permanent His pacing in 80 % of patients with both heart failure with a preserved ejection fraction and heart failure with reduced ejection fraction. These patients had AF and a narrow QRS, and despite rate-controlled AF they observed a reduction in hospital admissions, diuretic use, symptoms and improved cardiac function.[28] However, despite the benefits seen in observational data, no randomised controlled studies are available.
His Pacing to Deliver Ventricular Resynchronisation in Patients with Left Bundle Branch Block
Biventricular pacing, when delivered to patients with heart failure and LBBB, improves both morbidity and mortality.[36] However, even with biventricular pacing, symptom burden and mortality remain high.[36] Biventricular pacing delivers imperfect ventricular resynchronisation, with only modest reductions in QRS duration, and does not return left ventricular activation times to those seen in individuals with intrinsically narrow QRS.[16] Furthermore, when biventricular pacing is delivered to patients with a narrow QRS duration, or moderate QRS prolongation, it may actually prolong ventricular activation time and worsen dyssynchronous activation.[16,37]
There is significant potential to deliver additional improvements in cardiac function if more effective ventricular resynchronisation can be delivered.[38]
His bundle pacing is an alternative technique for delivering cardiac resynchronisation therapy. It can dramatically shorten QRS duration (Figure 3) and restore normal intrinsic activation patterns in some patients with ventricular conduction delays.
Figure 3: Left Bundle Branch Block Reversal with His Bundle Pacing.
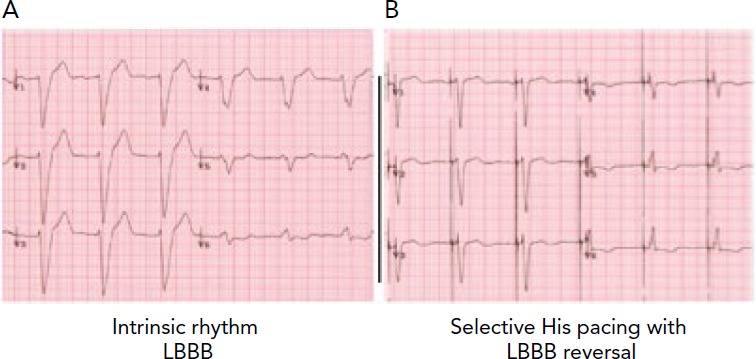
A: Left bundle branch block (LBBB) pattern at baseline. B: A narrow QRS is restored with His bundle pacing. A short isoelectric period is visible immediately after the pacing spike consistent with activation through the His bundle.
A number of mechanisms have been proposed for His bundle pacing narrowing or reversing a bundle branch block (Figure 4):
Figure 4: Mechanisms for Left Bundle Branch Block Reversal with His Bundle Pacing.
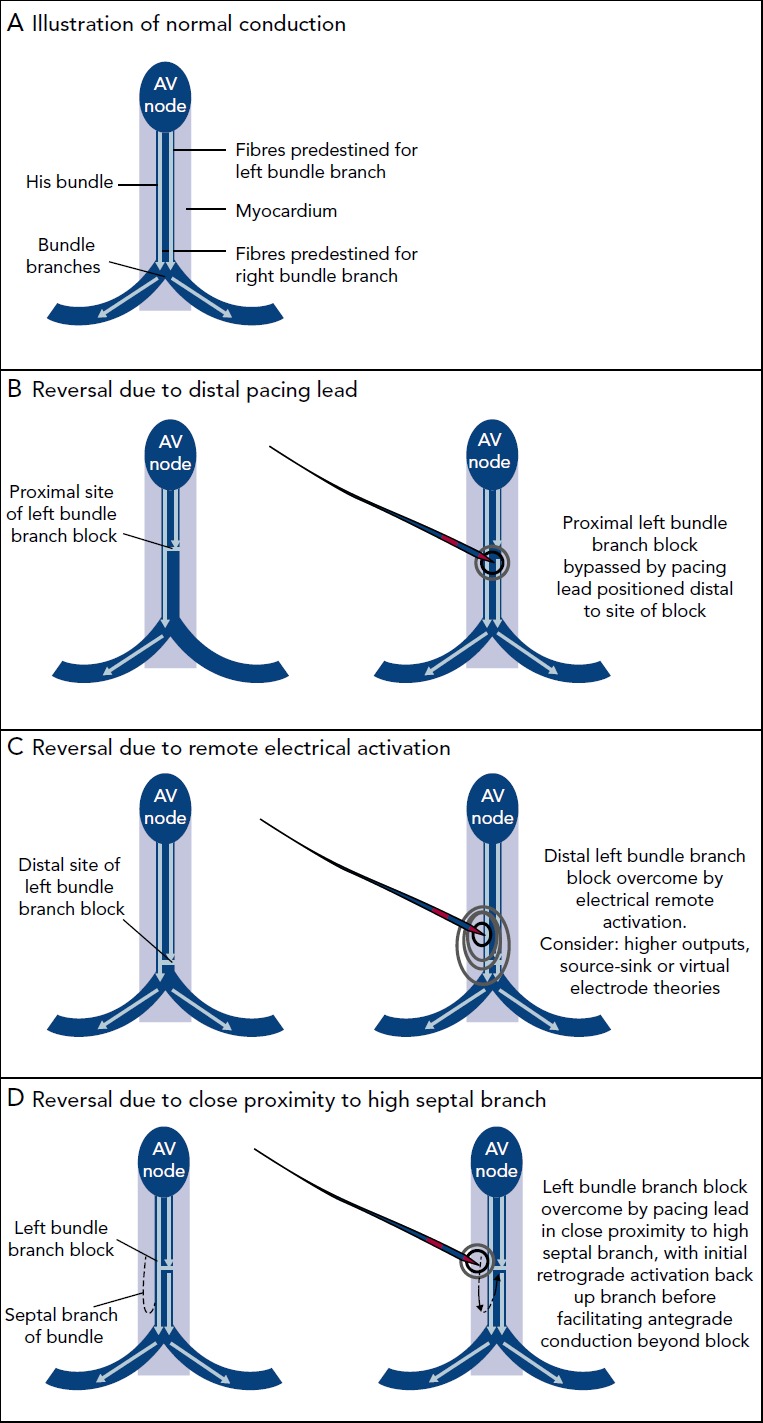
A: Normal ventricular activation, with activation from the atrioventricular (AV) node down the bundle of His and then into the left and right bundle branches. Fibres within the bundle of His are already predestined for their respective bundle branches. B: Proximal site of left bundle branch block (LBBB; left); pacing lead has been positioned in a site distal to this block allowing an electrical bypass of the LBBB, reversing the electrical abnormality (right). C: Distal site of LBBB where positioning the His pacing lead would not be possible (left); remote electrical activation with a more proximally-placed lead could reverse this electrical abnormality. This could occur because of increased pacing outputs, as a consequence of the source-sink-theory and a high likelihood of their being some diseased fibres already in the proximal location or the virtual electrode polarisation theory (right). D: Each bundle branch has multiple branches (left); high septal branch may fortuitously be activated with a conventionally placed His lead, resulting in retrograde activation down the branch back to a place in the bundle branch, which is distal to the site of block allowing antegrade activation from this site forward (right).
Positioning the pacing lead distal to the site of bundle branch block: fibres within the His bundle are arranged in strands predestined for the left or right bundle branches. Conduction delays within the His bundle are a common cause of bundle branch block and pacing distal to this can reverse it.[39,40]
Source-sink relationships: overcoming the block with sufficient stimulus to activate distal dormant tissue relying on either source-sink relationships during pacing versus intrinsic impulse propagation or the virtual electrode polarisation effects.
Retrograde activation: retrograde activation of the His-Purkinje system via capture of an upper septal branch allowing onward antegrade activation beyond a site of block.
His pacing has been shown to be feasible in this population of patients. Reductions in QRS duration have been observed in 70-92 % of patients with LBBB (Table 1). The reductions in QRS duration appear to be maintained even with chronic pacing, and mean thresholds are similar to those seen for left ventricular leads; for example, in one study thresholds to achieve this are 2.0 V at 1 ms (mean threshold 1.4 V at 1 ms). There has been no demonstrated correlation with QRS morphology and axis, and QRS normalisation patterns (i.e. even broad LBBB with left axis deviation where the lead is unlikely to be screwed in distally to the block).
No large randomised trial has been conducted comparing His pacing with biventricular pacing. Studies that have been carried out are summarised in Table 1. In these studies, the mean QRS reduction with His pacing is 46 ms. This compares with typical values of 20 ms seen with biventricular pacing.[41] Improvements in left ventricular ejection fraction and symptoms have been observed with His pacing.[31,42,43]
His pacing was initially assessed as a rescue strategy in cases where biventricular pacing failed,[29,32] and some authors have shown that His pacing is feasible as a primary strategy for cardiac resynchronisation.[30] In a crossover study, His pacing was more effective than biventricular pacing at reducing QRS duration in 72 % of patients (21/29). Two patients achieved QRS narrowing with His pacing but with high outputs, and six patients did not show any QRS narrowing with His pacing despite multiple sites tried. With improved technology and experience, permanent His pacing achieved QRS narrowing in 90 % of patients.[32] The reasons for failure in achieving QRS narrowing is not fully understood. It is possible this subgroup of patients have abnormal left ventricular conduction due to disease outside of the His bundle and, therefore, cannot be treated with His pacing, or the block is too severe to overcome. The proportion of patients with conduction delays caused by disease distal to the His bundle is not known.
His pacing has the advantage that it does not require the use of contrast and can often be performed more quickly than left ventricular lead placement. However, adequately powered randomised studies are required to compare this strategy for resynchronisation therapy with biventricular pacing. In 2016 recruitment started for the His Bundle Pacing Versus Coronary Sinus Pacing for Cardiac Resynchronisation Therapy (His-SYNC; NCT02700425) study, which is aiming to randomise 40 patients to either His pacing or biventricular pacing and will look at time to first cardiovascular hospitalisation or death.
Heart Failure in Patients with Narrow QRS and PR Prolongation
PR prolongation results in impaired left ventricular filling, and in patients with heart failure it is associated with a higher risk of death than those whose AV delay was within normal limits.[12] When biventricular pacing is delivered to patients with LBBB, those with PR prolongation appear to obtain greater benefit than those with a normal PR interval. In the Comparison of Medical Therapy, Pacing and Defibrillation in Heart Failure (COMPANION) trial, patients with a long PR interval had a 17 % greater relative risk reduction in heart failure admissions and death compared with those with a normal PR interval.[44] Biventricular pacing requires a compulsory shortening of the AV delay to ensure biventricular capture. This shortening of the AV delay appears to be one of the mechanisms by which biventricular pacing delivers its beneficial effect.[38]
Adjusting AV delay is known to change acute haemodynamic function.[45]
There PR prolongation may represent a treatment target in patients with heart failure and normal QRS duration or right bundle branch block (RBBB). Delivering biventricular pacing to this group of patients may induce ventricular dyssynchrony relative to normal intrinsic activation, which may offset some of the beneficial effects of AV delay shortening.[16] In the context of a normal QRS, biventricular pacing can increase mortality.[16,37,46]
His pacing has the advantage that it may allow AV delay to be optimised while normal intrinsic ventricular activation is maintained. We have previously demonstrated that acute haemodynamic function is improved with AV-optimised His bundle pacing in patients with heart failure and PR prolongation with either a normal QRS or RBBB.[47] The magnitude of acute haemodynamic corresponded to approximately 60 % of the benefit seen in patients with LBBB receiving biventricular pacing (Figure 5).
Figure 5: Acute Haemodynamic Improvements Seen with His Pacing in Narrow QRS and Long PR Interval.
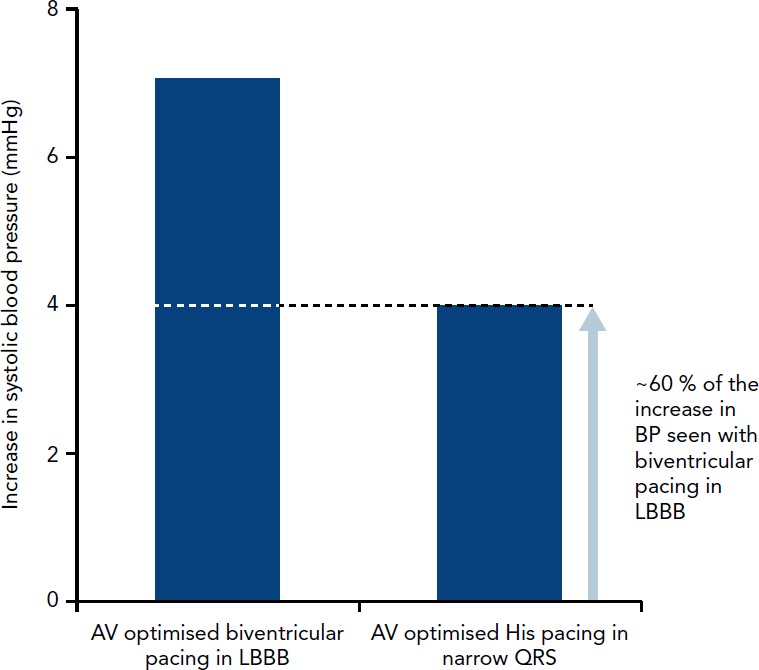
When compared to the acute haemodynamic studies that investigated atrioventricular (AV)- optimised biventricular pacing in left bundle branch block (LBBB), the acute blood pressure (BP) increase in a study of AV-optimised His pacing in patients with PR prolongation >200 ms showed approximately 60 % of the increase.[47]
The His Optimised Pacing Evaluated for Heart Failure Trial (HOPE-HF; NCT02671903) trial is a multicentre, double-blind, randomised, crossover study that aims to randomise 160 patients with PR prolongation (≥200 ms), left ventricular impairment (ejection fraction ≤40 %), and either narrow QRS (≤140 ms) or RBBB. Participants are first randomised to either 6 months with the His lead programmed on or off before crossing over to the alternate arm. The primary endpoint is exercise capacity measured using cardiopulmonary exercise testing. When randomised to the His pacing arm, the patients are set to an AV delay determined by our high resolution haemodynamic optimisation protocol.[45] If the results are positive then this would offer the potential of a new therapeutic option to a cohort of patients with heart failure who are not currently eligible for pacing therapy for heart failure.
Current Limitations
There is currently limited published data available for His pacing in any clinical setting. While pacing thresholds for His pacing in bradycardia appear to be stable, there is limited long-term follow-up data available. When His pacing is used to deliver ventricular resynchronisation in patients with bundle branch block, the pacing thresholds can be relatively high, though comparable to left ventricular pacing thresholds. This has the potential implications on battery longevity, though pacing is only required via a single lead (compared to biventricular pacing). Success rates for His lead implantation have been as low as 60 % without dedicated tools and experience. Success rates have improved with the development of dedicated tools; however, the range of tools currently available are still limited, and these could be further improved.
Adequately powered randomised control trials are required to investigate whether the theoretical advantages of physiological ventricular activation are achieved with His pacing and if the encouraging results in observational studies translate into clinical benefit.
Finally, current device-based algorithms do not dovetail with His bundle pacing and this pacing sphere could benefit from industry investment in His pacing customised algorithms.
Conclusion
His pacing is a novel pacing therapy that allows ventricular stimulation to occur via the normal conduction system. Therefore, it maintains normal ventricular activation in patients with a narrow QRS duration and may even reverse bundle branch block.
Technical limitations have restricted the use of this therapy despite its existence for over four decades. In recent years tools dedicated to His pacing have been developed, which have improved the ease with which His pacing can be delivered. His pacing is now technically feasible in most patients and has shown promising results in small, mainly non-randomised studies in various clinical situations.
His pacing may be beneficial in the prevention of pacing-induced cardiomyopathy, as an alternative to biventricular pacing in patients with heart failure and LBBB, and as a method for extending pacing therapy for heart failure to patients with narrow QRS and PR prolongation. Large randomised studies are now required to provide confirmation these promising results translate into proven clinical benefits.
Clinical perspective
His-bundle pacing is a feasible method for delivering permanent pacing. It produces physiological ventricular activation via the His-Purkinje system.
His pacing offers an alternative bradycardia pacing modality to right ventricular pacing and has the advantage that it does not cause intraventricular dyssynchrony.
His pacing can achieve cardiac resynchronisation in patients with heart failure and bundle branch block.
Data regarding safety, chronic sensing and pacing thresholds are encouraging, but data from larger registries is awaited.
Randomised controlled trial data to assess the benefits of His bundle pacing for bradycardia and heart failure indications are not yet available.
References
- 1.Narula OS, Scherlag BJ, Samet R. Pervenous pacing of the specialized conducting system in man: His bundle and A-V nodal stimulation. Circulation. 1970;41:77–87. doi: 10.1161/01.CIR.41.1.77. [DOI] [PubMed] [Google Scholar]
- 2.Deshmukh R, Casavant DA, Romanyshyn M, Anderson K. Permanent, direct His-bundle pacing: a novel approach to cardiac pacing in patients with normal His-Rurkinje activation. Circulation. 2000;101:869–77. doi: 10.1161/01.CIR.10L8.869. [DOI] [PubMed] [Google Scholar]
- 3.Vijayaraman R, Dandamudi G, Zanon F et al. Permanent His bundle pacing: recommendations from a multi-center HBR collaborative working group for standardization of definitions, implant measurements, and follow-up. Heart Rhythm. 2018;15:460–8. doi: 10.1016/j.hrthm.2017.10.039. [DOI] [PubMed] [Google Scholar]
- 4.Vijayaraman R, Naperkowski A, Subzposh FA Rermanent His bundle pacing: long-term lead performance and clinical outcomes. Heart Rhythm. 2017. epub ahead of press. [DOI] [PubMed]
- 5.Wilkoff BL, Cook JR, Epstein AE et al. Dual-chamber pacing or ventricular backup pacing in patients with an implantable defibrillator: the dual chamber and VVI implantable defibrillator (DAVID) trial. JAMA. 2002;288:3115–23. doi: 10.1001/jama.288.24.3115. [DOI] [PubMed] [Google Scholar]
- 6.Sweeney MO, Hellkamp AS, Ellenbogen KA et al. Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation. 2003;107:2932–37. doi: 10.1161/01.CIR.0000072769.17295.B1. [DOI] [PubMed] [Google Scholar]
- 7.Thambo JB, Bordachar R, Garrigue S et al. Detrimental ventricular remodeling in patients with congenital complete heart block and chronic right ventricular apical pacing. Circulation. 2004;110:3766–72. doi: 10.1161/01.CIR.0000150336.86033.8D. [DOI] [PubMed] [Google Scholar]
- 8.O’Keefe JH, Jr, Abuissa H, Jones RG et al. Effect of chronic right ventricular apical pacing on left ventricular function. Am J Cardiol. 2005;95:771–3. doi: 10.1016/j.amjcard.2004.11.034. [DOI] [PubMed] [Google Scholar]
- 9.Thackray SD, Witte KK, Nikitin NR et al. The prevalence of heart failure and asymptomatic left ventricular systolic dysfunction in a typical regional pacemaker population. Eur Heart J. 2003;24:1143–52. doi: 10.1016/S0195-668X(03)00199-4. [DOI] [PubMed] [Google Scholar]
- 10.Frias RA, Corvera JS, Schmarkey L et al. Evaluation of myocardial performance with conventional single-site ventricular pacing and biventricular pacing in a canine model of atrioventricular block. J Cardiovasc Electrophysiol. 2003;14:996–1000. doi: 10.1046/j.1540-8167.2003.02483.x. [DOI] [PubMed] [Google Scholar]
- 11.Gillis AM, Rurerfellner H, Israel CW et al. Reducing unnecessary right ventricular pacing with the managed ventricular pacing mode in patients with sinus node disease and AV block. Pacing Clin Electrophysiol. 2006;29:697–705. doi: 10.1111/j.1540-8159.2006.00422.x. [DOI] [PubMed] [Google Scholar]
- 12.Milasinovic G, Tscheliessnigg K, Boehmer A et al. Rercent ventricular pacing with managed ventricular pacing mode in standard pacemaker population. Europace. 2008;10:151–5. doi: 10.1093/europace/eum288. [DOI] [PubMed] [Google Scholar]
- 13.Yadav R, Jaswal A, Chennapragada S et al. Effectiveness of ventricular intrinsic preference (VIR) and ventricular autocapture (VAC) algorithms in pacemaker patients: results of the validate study. J Arrhythm. 2016;32:29–35. doi: 10.1016/jjoa.2015.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Curtis AB, Worley SJ, Adamson RB et al. Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med. 2013;368:1585–93. doi: 10.1056/NEJMoa1210356. [DOI] [PubMed] [Google Scholar]
- 15.Yu CM, Chan JY, Zhang Q et al. Biventricular pacing in patients with bradycardia and normal ejection fraction. N Engl J Med. 2009;361:2123–34. doi: 10.1056/NEJMoa0907555. [DOI] [PubMed] [Google Scholar]
- 16.Ploux S, Eschalier R, Whinnett ZI et al. Electrical dyssynchrony induced by biventricular pacing: implications for patient selection and therapy improvement. Heart Rhythm. 2015;12:782–91. doi: 10.1016/j.hrthm.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 17.Dreger H, Maethner K, Bondke H et al. Racing-induced cardiomyopathy in patients with right ventricular stimulation for >15 years. Europace. 2012;14:238–42. doi: 10.1093/europace/eur258. [DOI] [PubMed] [Google Scholar]
- 18.Catanzariti D, Maines M, Manica A et al. Rermanent His-bundle pacing maintains long-term ventricular synchrony and left ventricular performance, unlike conventional right ventricular apical pacing. Europace. 2013;15:546–53. doi: 10.1093/europace/eus313. [DOI] [PubMed] [Google Scholar]
- 19.Kronborg MB, Roulsen SH, Mortensen RT, Nielsen JC. Left ventricular performance during para-His pacing in patients with high-grade atrioventricular block: an acute study. Europace. 2012;14:841–46. doi: 10.1093/europace/eur368. [DOI] [PubMed] [Google Scholar]
- 20.Kronborg MB, Mortensen RT, Roulsen SH et al. His or para-His pacing preserves left ventricular function in atrioventricular block: a double-blind, randomized, crossover study. Europace. 2014;16:1189–96. doi: 10.1093/europace/euu011. [DOI] [PubMed] [Google Scholar]
- 21.Abdelrahman M, Subzposh FA, Beer D Clinical outcomes of His bundle pacing compared to right ventricular pacing. J Am Coil Cardiol. 2018. epub ahead of press. [DOI] [PubMed]
- 22.Zanon F, Bacchiega E, Rampin L et al. Direct His bundle pacing preserves coronary perfusion compared with right ventricular apical pacing: a prospective, cross-over mid-term study. Europace. 2008;10:580–7. doi: 10.1093/europace/eun089. [DOI] [PubMed] [Google Scholar]
- 23.Sharma RS, Subzposh FA, Ellenbogen KA, Vijayaraman R. Rermanent His-bundle pacing in patients with prosthetic cardiac valves. Heart Rhythm. 2017;14:59–64. doi: 10.1016/j.hrthm.2016.09.016. [DOI] [PubMed] [Google Scholar]
- 24.Shan R, Su L, Zhou X et al. Beneficial effects of upgrading to His bundle pacing in chronically paced patients with left ventricular ejection fraction <50%. Heart Rhythm. 2018;15:405–12. doi: 10.1016/j.hrthm.2017.10.031. [DOI] [PubMed] [Google Scholar]
- 25.Deshmukh RM, Romanyshyn M. Direct His-Bundle Racing: present and future. Pacing Clin Eiectrophysiol. 2004;27:862–70. doi: 10.1111/j.1540-8159.2004.00548.x. [DOI] [PubMed] [Google Scholar]
- 26.Occhetta E, Bortnik M, Magnani A et al. Rrevention of ventricular desynchronization by permanent para-Hisian pacing after atrioventricular node ablation in chronic atrial fibrillation: a crossover, blinded, randomized study versus apical right ventricular pacing. J Am Coil Cardiol. 2006;47:1938–45. doi: 10.1016/jjacc.2006.01.056. [DOI] [PubMed] [Google Scholar]
- 27.Vijayaraman R, Subzposh FA, Naperkowski A. Atrioventricular node ablation and His bundle pacing. Europace. 2017;19:iv10–6. doi: 10.1093/europace/eux263. [DOI] [PubMed] [Google Scholar]
- 28.Huang W, Su L, Wu S et al. Benefits of permanent His bundle pacing combined with atrioventricular node ablation in atrial fibrillation patients with heart failure with both preserved and reduced left ventricular ejection fraction. J Am Heart Assoc. 2017;6:e005309. doi: 10.1161/JAHA.116.005309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barba-Richardo R, Manovel Sanchez A, Fernandez-Gomez JM et al. Ventricular resynchronization therapy by direct His-bundle pacing using an internal cardioverter defibrillator. Europace. 2013;15:83–8. doi: 10.1093/europace/eus228. [DOI] [PubMed] [Google Scholar]
- 30.Lustgarten DL, Crespo EM, Arkhipova-Jenkins I et al. His-bundle pacing versus biventricular pacing in cardiac resynchronization therapy patients: a crossover design comparison. Heart Rhythm. 2015;12:1548–57. doi: 10.1016/j.hrthm.2015.03.048. [DOI] [PubMed] [Google Scholar]
- 31.Ajijola OA, Romero J, Vorobiof G et al. Hyper-response to cardiac resynchronization with permanent His bundle pacing: is parahisian pacing sufficient? Heart Rhythm Case Rep. 2015;1:429–33. doi: 10.1016/j.hrcr.2015.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sharma RS, Dandamudi G, Herweg B et al. Rermanent His-bundle pacing as an alternative to biventricular pacing for cardiac resynchronization therapy: a multicenter experience. Heart Rhythm. 2018;15:413–20. doi: 10.1016/j.hrthm.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 33.Tang AS, Wells GA, Talajic M et al. Cardiac-resynchronization therapy for mild-to-moderate heart failure. N Engl J Med. 2010;363:2385–95. doi: 10.1056/NEJMoa1009540. [DOI] [PubMed] [Google Scholar]
- 34.Gasparini M, Regoli F, Galimberti R et al. Cardiac resynchronization therapy in heart failure patients with atrial fibrillation. Europace. 2009;11:v82–6. doi: 10.1093/europace/eup273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gasparini M, Auricchio A, Regoli F et al. Four-year efficacy of cardiac resynchronization therapy on exercise tolerance and disease progression: the importance of performing atrioventricular junction ablation in patients with atrial fibrillation. J Am Coil Cardiol. 2006;48:734–43. doi: 10.1016/jjacc.2006.03.056. [DOI] [PubMed] [Google Scholar]
- 36.Cleland JG, Daubert JC, Erdmann E et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352:1539–49. doi: 10.1056/NEJMoa050496. [DOI] [PubMed] [Google Scholar]
- 37.Ruschitzka F, Abraham WT, Singh JR et al. Cardiac-resynchronization therapy in heart failure with a narrow QRS complex. N Engl J Med. 2013;369:1395–405. doi: 10.1056/NEJMoa1306687. [DOI] [PubMed] [Google Scholar]
- 38.Jones S, Lumens J, Sohaib SM et al. Cardiac resynchronization therapy: mechanisms of action and scope for further improvement in cardiac function. Europace. 2017;19:1178–86. doi: 10.1093/europace/euw136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Narula OS. Longitudinal dissociation in the His bundle. Bundle branch block due to asynchronous conduction within the His bundle in man. Circulation. 1977;56:996–1006. doi: 10.1161/01.CIR.56.6.996. [DOI] [PubMed] [Google Scholar]
- 40.El-Sherif N, Amay-Y-Leon F, Schonfield C et al. Normalization of bundle branch block patterns by distal His bundle pacing. Clinical and experimental evidence of longitudinal dissociation in the pathologic His bundle. Circulation. 1978;57:473–83. doi: 10.1161/01.CIR.57.3473. [DOI] [PubMed] [Google Scholar]
- 41.Abraham WT, Fisher WG, Smith AL et al. Cardiac resynchronization in chronic heart failure. N Engl J Med. 2002;346:1845–53. doi: 10.1056/NEJMoa013168. [DOI] [PubMed] [Google Scholar]
- 42.Wu G, Cai Y, Huang W, Su L. Hisian pacing restores cardiac function. J Eiectrocardiol. 2013;46:676–8. doi: 10.1016/jjelectrocard.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 43.Dabrowski R, Kleinrok A, Kozluk E, Opolski G. Rhysiologic resynchronization therapy: a case of His bundle pacing reversing physiologic conduction in a patient with CHF and LBBB during 2 years of observation. J Cardiovasc Eiectrophysiol. 2011;22:813–7. doi: 10.1111/j.1540-8167.2010.01949.x. [DOI] [PubMed] [Google Scholar]
- 44.Bristow MR, Saxon LA, Boehmer J et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004;350:2140–50. doi: 10.1056/NEJMoa032423. [DOI] [PubMed] [Google Scholar]
- 45.Whinnett ZI, Davies JE, Willson K et al. Haemodynamic effects of changes in atrioventricular and interventricular delay in cardiac resynchronisation therapy show a consistent pattern: analysis of shape, magnitude and relative importance of atrioventricular and interventricular delay. Heart. 2006;92:1628–34. doi: 10.1136/hrt.2005.080721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sohaib SM, Chen Z, Whinnett ZI et al. Meta-analysis of symptomatic response attributable to the pacing component of cardiac resynchronization therapy. Euro J Heart Fail. 2013;15:1419–28. doi: 10.1093/eurjhf/hft139. [DOI] [PubMed] [Google Scholar]
- 47.Sohaib SM, Wright I, Lim E et al. Atrioventricular optimized direct His bundle pacing improves acute hemodynamic function in patients with heart failure and RR interval prolongation without left bundle branch block. JACC Clin Electrophysiol. 2015;1:582–91. doi: 10.1016/jjacep.2015.08.008. [DOI] [PubMed] [Google Scholar]