Abstract
Glenoid bone loss and capsular deficiency represent critical points of arthroscopic Bankart repair failures. The purpose of this Technical Note is to present an all-arthroscopic bone block procedure associated with arthroscopic subscapularis augmentation for treating glenohumeral instability with glenoid bone loss and anterior capsulolabral deficiency. Two glenoid tunnels are set up from the posterior to the anterior side using a dedicated bone block guide, and 4 buttons are used to fix the graft to the glenoid. The subscapularis tenodesis is performed using a suture tape anchor. This combined arthroscopic technique (bone block associated with arthroscopic subscapularis augmentation) could be a valid and safe alternative to the arthroscopic or open Latarjet procedures.
The cause of anterior shoulder instability is not completely known,1, 2, 3, 4, 5, 6, 7 and its surgical management remains controversial. Few studies have been carried out on post-traumatic capsular elongation and hyperlaxity or on the healing process of the soft tissue on the glenoid edges after the first dislocation and after capsulolabral repair.8, 9 Lately, the correlations among glenoid bone loss (GBL), humeral head defects, and instability have been studied.10 Recent papers show the biomechanical aspects of restoring the glenoid width using bone augmentation and the role of the anterior capsule in recentering the humeral head on the glenoid fossa.2, 11, 12 Furthermore, severe bone lesions of the glenoid rim and the Hill-Sachs defect on the humeral head are associated with poor-quality capsular tissues.2, 3, 7, 13
Arthroscopic Bankart repair is the most popular surgical treatment of traumatic and atraumatic recurrent shoulder instability, and its failure rate is reported to be from 15% to 64%, especially in unselected patients with severe GBL.3, 5, 14 The association of GBL and capsular inconsistence represents the real limit of a standard arthroscopic anterior capsulorrhaphy or an isolated bone graft procedure.15, 16, 17, 18, 19 The remplissage technique has been proposed as a support for engaging Hill-Sachs lesions, but the results are controversial when the anterior capsule is insufficient, and failures are reported to be from 4% to 15%.20 Currently, the open or arthroscopic Latarjet procedures are considered to be the most effective techniques for treatment in cases of severe bone defects and poor-quality anterior soft tissue due to the coracoid transfer and conjoint tendon action, with a recurrence between 0% and 5%.14, 18, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32 Also, the conjoined tendon transfer allows stability restoration with no significant range-of-motion loss and a low recurrence rate.33
Open and arthroscopic J-bone graft, considered to be much more anatomical approaches,34 can provide glenoid bone restoration, but certain technical aspects of the graft preparation and glenoid implant have led to low popularity of these procedures. An operation consisting of an all-arthroscopic bone graft glenoid augmentation using posterior instruments for glenoid drilling and graft stabilization was described,35, 36 and it seemed to be more reproducible compared with the J-graft technique.
Considering the recent positive experience using partial subscapularis tenodesis on the glenoid rim, known as arthroscopic subscapularis augmentation (ASA),37, 38, 39, 40, 41 to treat recurrent anterior instability with capsular inconsistence and moderate GBL, we decided to apply both techniques—free bone block and ASA (arthroscopic subscapularis augmentation and bone block)—in the treatment of severe GBL (10% to 25%) associated with anterior capsular insufficiency.
Preoperative Assessment
External rotation test in ER1 (Walch test) is performed on the contralateral side to assess capsular laxity. A 3-dimensional computed tomography scan with multiplanar reconstructions of the glenoid neck and a digital subtraction of the humeral head are performed. The Pico surface area method42 is used to quantify the percentage of inferior glenoid deficiency compared with the contralateral shoulder. The indication is a GBL >20%.
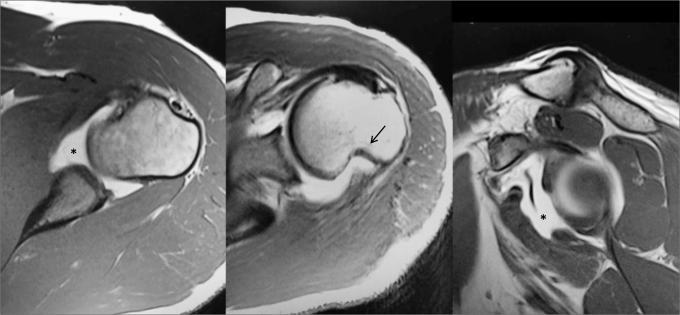
An arthro–magnetic resonance imaging is performed to assess capsulolabral and Hill-Sachs lesions (Fig 1).
Fig 1.
Arthro-MRI is useful to detect Hill-Sachs lesions (arrow) and anterior capsulolabral deficiency (asterisk). Left shoulder, axial/axial/sagittal view. (MRI, magnetic resonance imaging.)
Surgical Technique
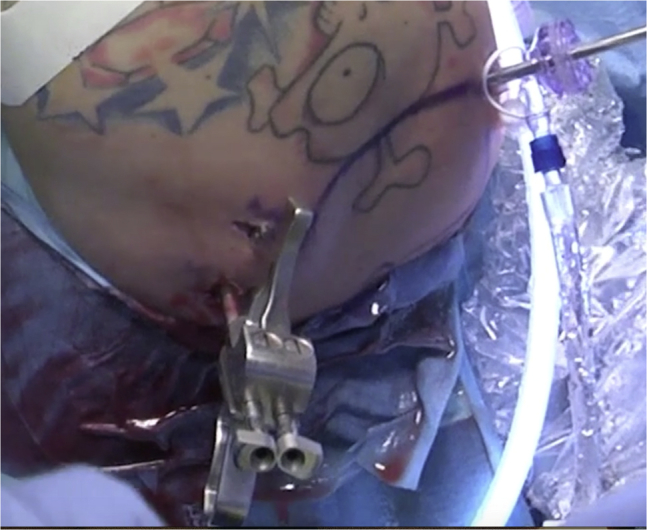
An arthroscopic subscapularis augmentation and bone block technique is performed with the patient in a lateral decubitus position; the arm is kept in 40° of abduction and 15° of forward flexion with a balanced suspension of 5 to 10 lb (Star Sleeve Traction System; Arthrex, Naples, FL). Arthroscopy is performed with a 30° arthroscope and an arthroscopic pump maintaining pressure at 60 mm Hg. The posterior portal for the arthroscope is created 10 mm lateral to the standard portal so 1 cm medial and 5 mm inferior to the acromial edge (Fig 2; Table 1).
Fig 2.

A posterior portal is created 1 cm lateral to the standard portal for the introduction of the glenoid drilling guide.
Table 1.
Pearls and Pitfalls
| 1. The surgeon should create the posterior portal 10 mm lateral to the standard portal |
| 2. The surgeon should enlarge the posterior portal with radiofrequency to make the entrance of the hook easier |
| 3. The guide hook should be placed at the center of the glenoid defect |
| 4. The surgeon should enlarge the anteroinferior portal in the rotator interval very well, while retrieving out the cannula |
| 5. The metal cannula could take a wrong path |
| 6. The North and the South must be marked in the graft and the South has to be passed first, keeping guidewires in a parallel position |
| 7. The surgeon should keep the arm in neutral rotation and tape sutures in traction in a parallel position while the anchor for tenodesis is inserted into the bone |
| 8. Anchor bone hole should be made over the top of the glenoid edge |
The same portal is used to insert the posterior guide in a correct position on the glenoid, thus avoiding the creation of an accessory posterior portal. Anterosuperior and anterior portals are created in the rotator interval, and 2 cannulas (diameter: 8 mm and 6 mm) are used. The anterior and posterior glenohumeral joint structures are inspected to assess any anteroinferior labral detachment, SLAP lesions, capsular deficiency, anterior glenoid defects, and Hill-Sachs lesions.
Arthroscopic tools from both anterior portals are used alternatively to prepare the glenoid neck.
Graft Preparation
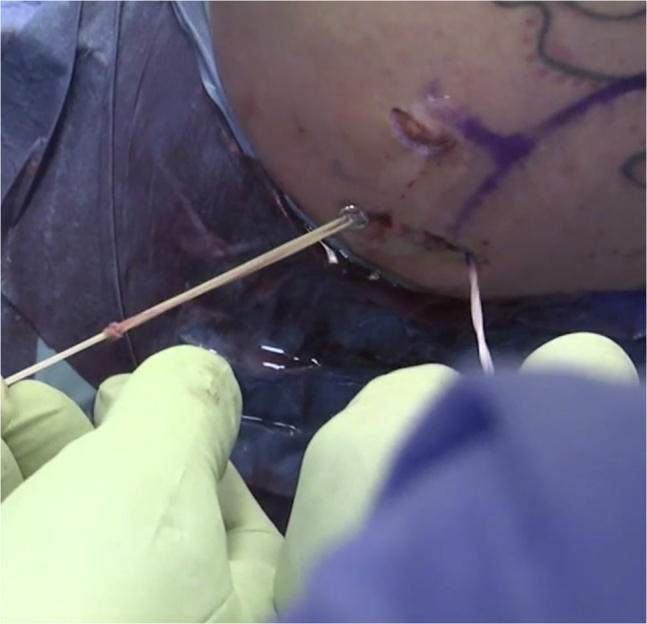
The graft is tailored from an iliac crest allograft so that it is compatible with the glenoid bone defect. The graft dimensions are 20 mm × 9 mm × 9 mm. Two 2.8-mm drill holes are made 10 mm apart and 5 mm from each edge of the graft (Fig 3).
Fig 3.
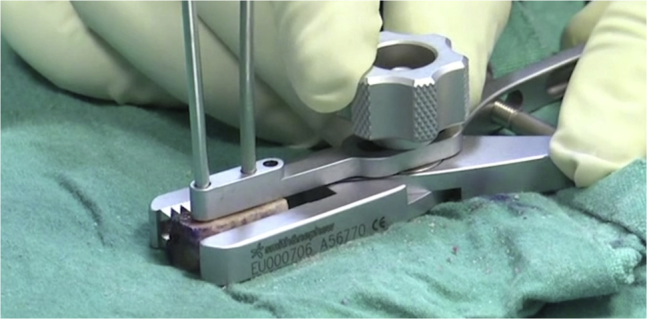
Two 2.8-mm drill holes are made 10 mm apart and 5 mm from each edge of the graft.
The size of the graft is mandatory because harvesting the graft with 2 metallic buttons increases the thickness such that a larger graft cannot slide into a dedicated 15-mm metal cannula (Smith & Nephew, London, England), and the exact position of the 2 holes is also important. Each looped guidewire (Smith & Nephew) is fed through the holes prepared in the graft, exiting on the cortical side (Fig 4), and is harvested with 2 endobottons (Smith & Nephew).
Fig 4.
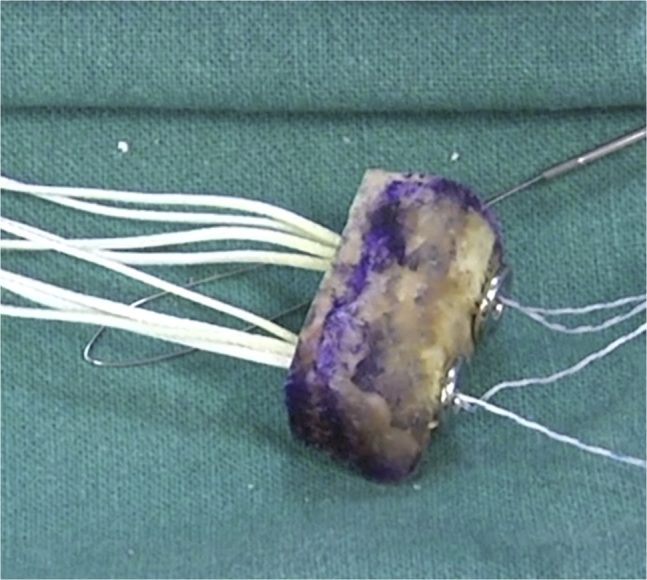
The graft preassembled with the suture.
Bone Block Procedure
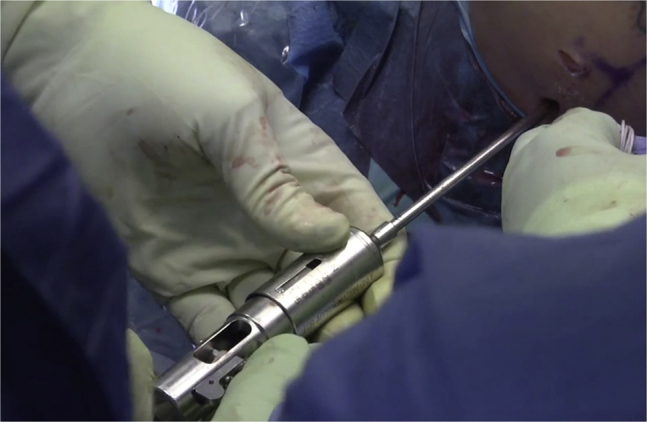
Care is taken to introduce the guide (Smith & Nephew) parallel to the glenoid surface and to have the bone tunnels perfectly perpendicular to the anterior glenoid neck (Fig 5).
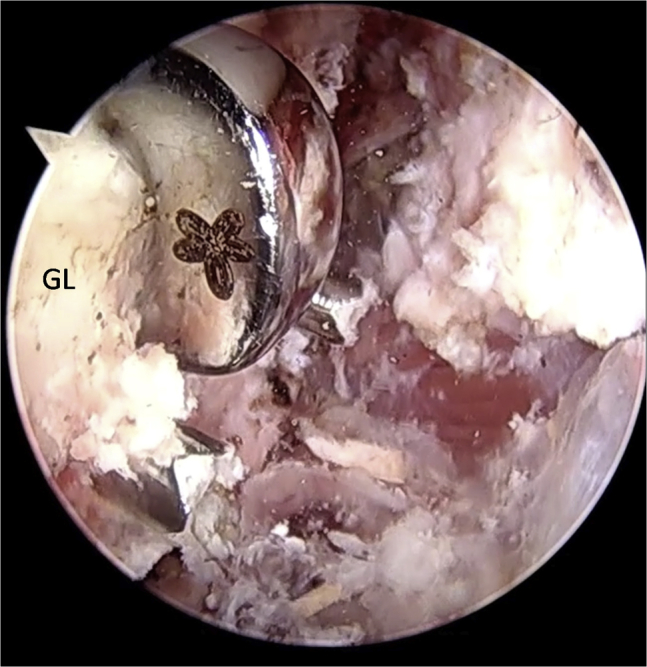
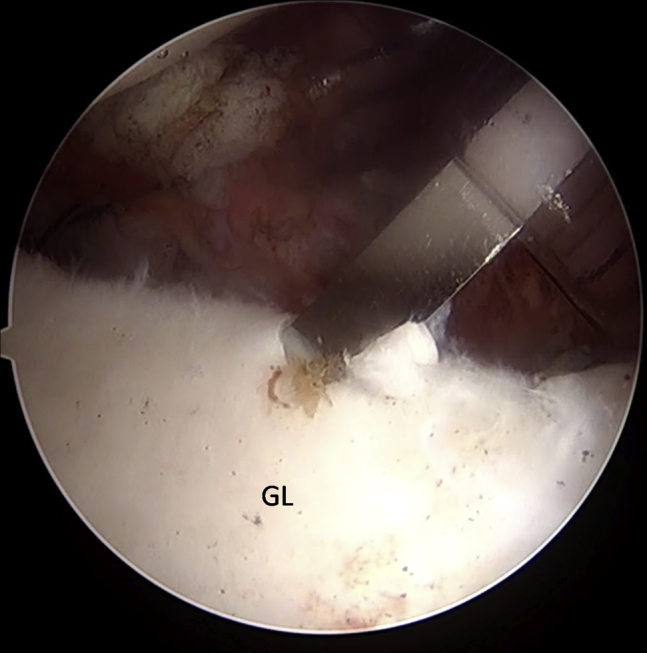
Fig 5.
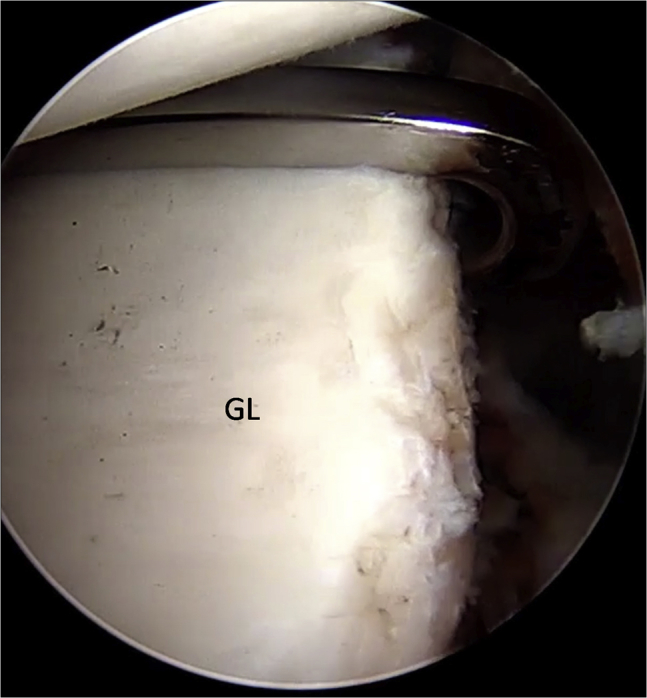
Left shoulder, anterior on the right and posterior on the left, an arthroscope from the anterosuperior portal, and a hook guide from the posterior portal. The hook of the guide is passed parallel to the glenoid face, and it is advanced over the anterior edge. (GL, glenoid.)
The hook of this guide is inserted through the posterior portal. The hook is passed parallel to the glenoid face to avoid damage to the articular surface, and it is advanced over the anterior edge. The guide's hook is placed at the center of the anterior glenoid defect. It is mandatory to align the glenoid guide with the posterior and anterior glenoid rims, according to the Taverna technique.36 Once the guide is positioned, a bullet is placed in each hole of the guide (Fig 6).
Fig 6.
Left shoulder, view from posterior. Once the guide is positioned and aligned with the posterior and anterior glenoid rims, a bullet is placed in each hole of the guide.
A 2.8-mm sleeved drill is placed in each bullet and advanced until it comes out from the anterior aspect of the glenoid. The drills are placed 5 mm below the cortical edge of the glenoid rim, parallel to one another and 10 mm apart. The inner drill is removed leaving the cannulated outer sleeve (Fig 7).
Fig 7.
Left shoulder, anterior on the right and posterior on the left, an arthroscope from the anterosuperior portal. The inner drill is removed leaving the cannulated outer sleeve. (GL, glenoid.)
Once drilling is completed, the bullets are removed posteriorly. Flexible looped guidewires (Smith & Nephew) are introduced into the joint by passing 1 wire through each sleeve in a posterior to anterior direction. Each guidewire is retrieved using a loop grasper (Fig 8), which is passed through the cannula introduced through the rotator interval. The wires are separated and stored. The drill sleeves are removed after this step is completed. At this point, the inferior 8-mm anterior cannula is removed and is replaced by a metal cannula with a diameter of 15 mm suitable for passing the graft attached to the 2 buttons.
Fig 8.
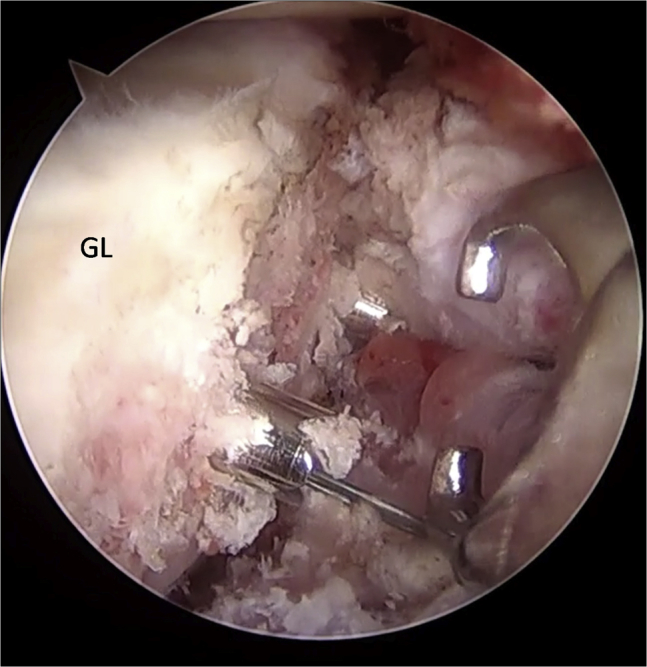
Left shoulder, anterior on the right and posterior on the left, an arthroscope from the anterosuperior portal, and a loop grasper from the anteroinferior portal. Each flexible looped guidewire, introduced into the joint by passing 1 wire through each sleeve in a posterior to anterior direction, is retrieved using a loop grasper. (GL, glenoid.)
The drill is placed through the superior cortex and exits the flattened cancellous side. The holes created correspond to the distance of the cannulated drill sleeves previously placed in the glenoid neck.
The anterior implants are fed with the preassembled suture through the end of the looped guidewire using a classic slip-knot. This is achieved by passing the loop of the lead suture through the looped guidewire and feeding the implant through the lead suture. The graft is slid toward the end of the guidewires to lodge the implant. It is important to first retrieve the inferior suture from the anterior portal, and when the whole graft is inside the joint, to retrieve the superior suture. It is important to carefully visualize the position of the graft from the posterior and superior portals. It is possible to correct the graft position by alternatively retrieving the inferior and superior wires using the superior cannula with a probe hook. Anterior round endobuttons (Smith & Nephew) are advanced until they lay flat on the bone block. The graft is tipped to allow insertion into the 15-mm cannula and advanced by pulling the guidewire out posteriorly (Fig 9).
Fig 9.

Left shoulder, view from anterior, a metal cannula in the anteroinferior portal, and an arthroscopic cannula in the anterosuperior portal. The graft with the preassembled suture is advanced through a 15-mm metal cannula.
The suture advances the implant until the graft is flush with the glenoid anterior neck (Fig 10), with each suture exiting the skin posteriorly. The graft should not be too medial nor too much lateral, so it must not overflow the articular surface. The posterior implants are placed on the transporter by advancing the instrument through each eyelet of the posterior round endobutton. We then pass the sutures through the transporter and retract the transporter to allow the suture to pass through the eyelets of the posterior round endobutton.
Fig 10.
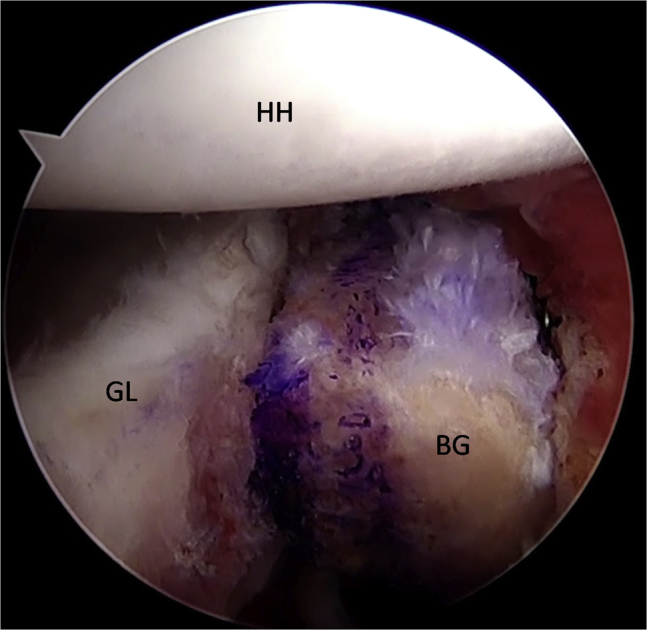
Left shoulder, anterior on the right and posterior on the left, an arthroscope from the anterosuperior portal. The graft is advanced until it sits flush on the glenoid neck. (BG, bone graft; GL, glenoid; HH, humeral head.)
The posterior round endobuttons are advanced using a sliding knot until they are flush with the posterior face of the glenoid (Fig 11). A suture tensioner device is used to secure the posterior round endobuttons (Fig 12). Once the implant is tensioned, we secure it with half hitches and cut suture tails.39, 40, 41
Fig 11.
Left shoulder, view from posterior. The posterior round endobuttons are advanced using a sliding knot until they are flush with the posterior face of the glenoid.
Fig 12.
Left shoulder, view from posterior. The suture tensioner device is used to secure the posterior round endobuttons.
ASA Technique
The upper third of the subscapularis tendon—as described in the Maiotti technique38—is usually fixed at 3 (R) or 9 (L) o'clock positions on the glenoid neck. In this technique, the tenodesis bone holes are placed on the anterior glenoid edge in an upper position, slightly over the top of the glenoid edge (at 10 o'clock in the left shoulders and 2 o'clock in the right shoulders), to avoid possible interference with the upper glenoid tunnel used for the fixation of the graft (Fig 13).
Fig 13.
Left shoulder, anterior on the right and posterior on the left, an arthroscope from the anterosuperior portal. A suture anchor bone hole is made at 10 o'clock position on the anterior glenoid edge. (GL, glenoid.)
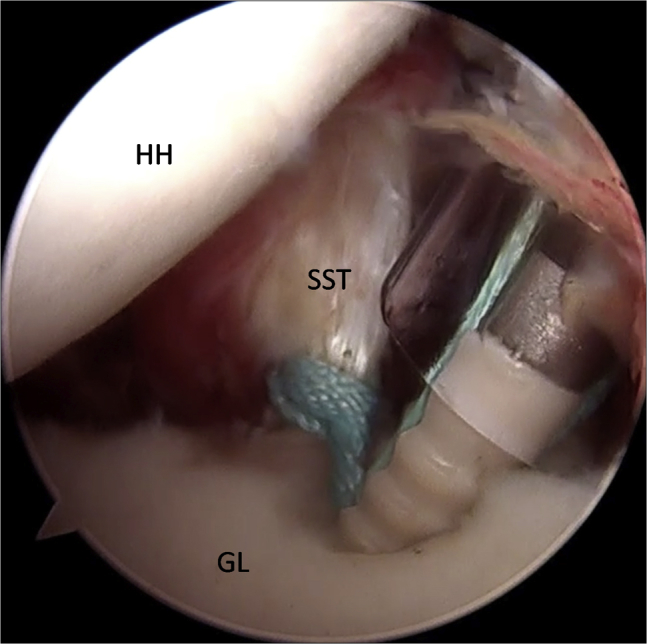
A second reason is that by elevating the subscapularis, it is possible to shift the inferior capsulolabral complex up to get a better covering of the graft. The middle upper third of the subscapularis tendon is penetrated approximately 5 mm from its superior border with a suture-passing device loaded with tape (Ultra Tape; Smith & Nephew) slightly flush to the articular surface in the mediolateral position just over the graft (Fig 14).
Fig 14.
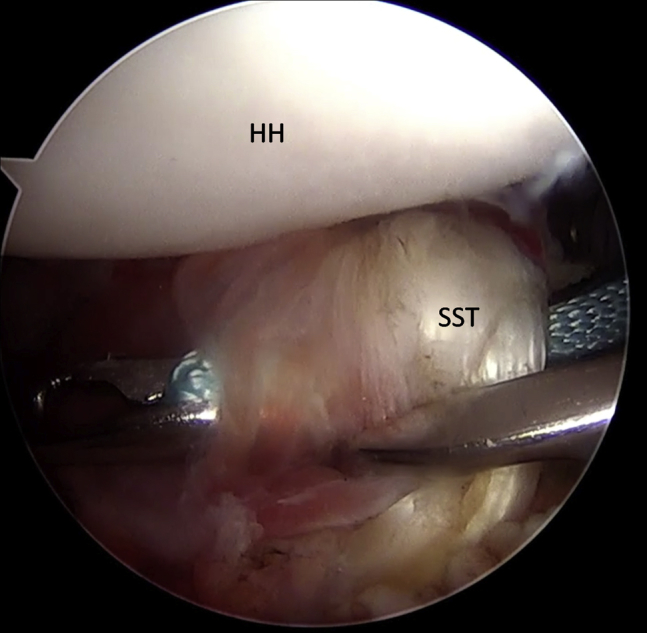
Left shoulder, anterior on the right and posterior on the left, an arthroscope from the posterior portal, and a suture-passing device from the anteroinferior portal. The middle upper third of the subscapularis tendon is penetrated with a suture-passing device loaded with the tape. (HH, humeral head; SST, subscapularis tendon.)
Next, one of the free ends is passed out through the upper cannula with a suture retriever and then passed again into the lower cannula (Fig 15).
Fig 15.

Left shoulder, view from anterior. The tape is carried out through the cannula with a suture retriever and then passed again in the other cannula.
A punch device proved extremely useful to assess the direction and depth of the anchor bone hole. At this point, a loop is created, and both free ends of the tape are passed through the anchor's eyelet (2.9-mm Bioraptor, Smith & Nephew); then, the anchor is pushed along the tape toward the bone hole (Fig 16). It is possible to use a 2.9-mm Pushlock anchor (Arthrex) too.
Fig 16.

Left shoulder, view from anterior. Both free ends of the tape are passed through the 2.9-mm anchor's eyelet and the anchor is pushed along the tape toward the bone hole from the anteroinferior portal.
Although the anchor is inserted into the bone (Fig 17), the tape sutures are kept in traction in a parallel position, and care is taken to keep the arm in neutral rotation to avoid excessive tension on the tissue repair. It is important to control the insertion of the anchor's eyelet and tape, thereby maintaining the correct direction before impacting. Advancement of the subscapularis tendon over the graft, effective closure of the anterior pouch, and a posterior shifting of the humeral head in a correct position centered on the glenoid socket can be clearly visible and assessed by arthroscopic examination from the posterior and anterosuperior portals (Fig 18; Video 1).
Fig 17.
Left shoulder, anterior on the right and posterior on the left, an arthroscope from the posterior portal, and an anchor from the anteroinferior portal. The anchor is inserted into the bone. (GL, glenoid; HH, humeral head; SST, subscapularis tendon.)
Fig 18.
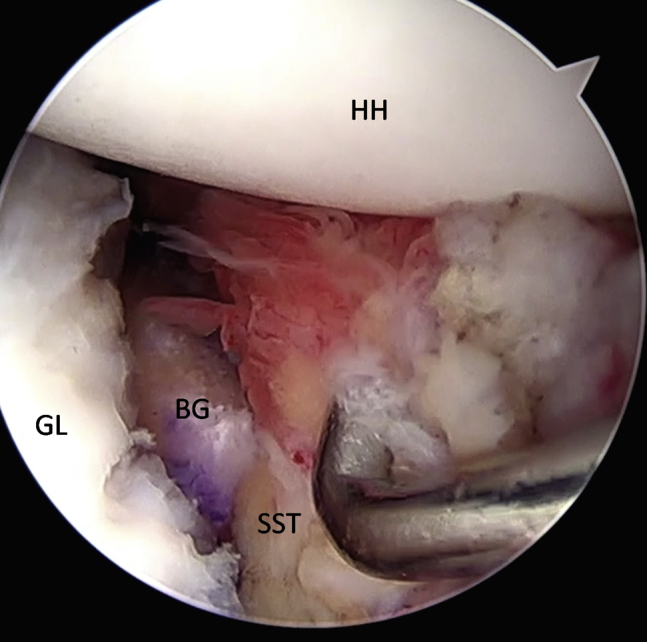
Left shoulder. Final view from the anterosuperior portal showing the closure of the anterior pounce on the bone graft and subscapularis tenodesis. (BG, bone graft; GL, glenoid; HH, humeral head; SST, subscapularis tendon.)
Discussion
The optimal treatment of recurrent complex anterior instability associated with significant GBL and capsular inconsistency has not yet been entirely established.6, 22, 43, 44, 45, 46 Considering the current literature, the open or arthroscopic Latarjet should be the most reliable procedure for GBL restoration and anterior capsular deficiency due to the well-known biomechanical “triple effect.” However, this technique modifies the coracohumeral arc anatomy and leads to a high rate of complications. Therefore, the need to find other less invasive and more anatomical techniques is mandatory, especially in young patients affected by shoulder hyperlaxity or capsular deficiency where recurrences are higher.
An all-arthroscopic technique using 3 cortical free bone grafts using 4 buttons to stabilize the graft from back to front has been described.35, 36 This consists of a system to fix a graft on the glenoid bone neck using a mechanical compression from back to front, avoiding Latarjet's complications related to anterior screw fixation. Moreover, this technique avoids anatomical modification of the coracoacromial arch.39, 41
A shaped substitute for bone graft has been recently realized. This Xenograft (Osteoplant Bioteck SPA, Torino, Italy) was harvested from the proximal humeral epiphysis of the horse. The graft was completely deantigenated enzymatically using Zimoteck. The graft can be preformed with the holes for the buttons, thus allowing greater precision and reduced operating times (Fig 19).
Fig 19.
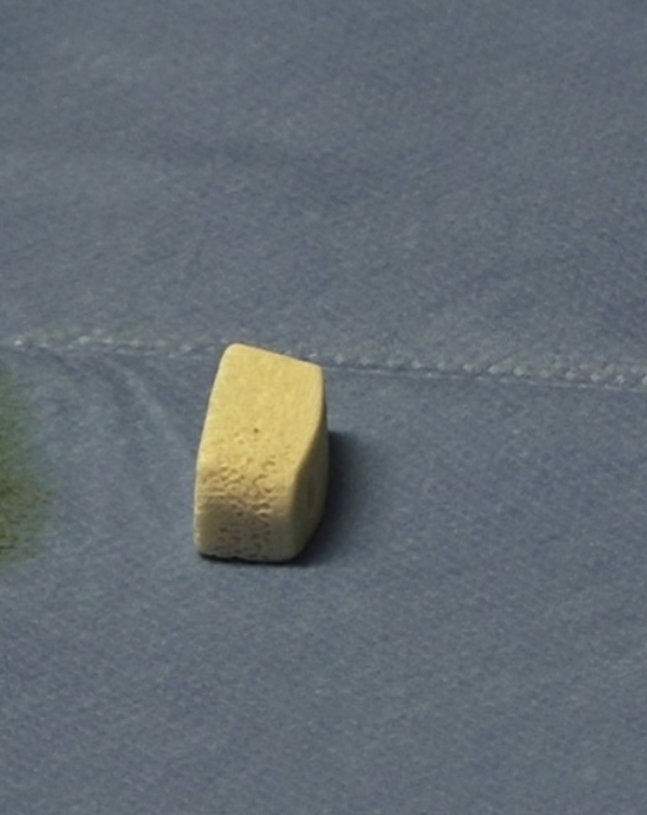
The preformed Xenograft.
Using this technique, after the stabilization of the anterior glenoid graft, a Bankart repair is mandatory to center the head on the glenoid fossa. In cases of recurrent instability, the percentage of anterior capsule inconsistency can be very high, and this problem can create conditions not conducive to obtaining a good result. A technique consisting of a partial subscapularis tenodesis augmenting the Bankart repair, to treat anterior recurrent instability with moderate GBL and capsular deficiency, was proposed in 2013.34 In 2015, the first short-term follow-up series reported very good clinical results with recurrences of 2.5% without impairment of external rotation.35 The sling effect of the upper subscapularis tenodesis was described,47 and its function as an anterior barrier in recentering the humeral head was shown in a biomechanical study on specimens.38 In a contemporary publication of a multicenter study, the reproducibility of this combination of the Bankart repair and the ASA technique was confirmed showing good results relative to failures without compromising external rotation.36
The stabilization of the bone graft with 4 buttons can certainly be considered an improvement, and the procedure avoids the risk of mechanical contact with the humeral head and a nonorthogonal pressure on the fixation strength of the graft on the glenoid bone defect. The partial subscapularis tenodesis allows the recentering of the head, pushing it posteriorly and acting in a way opposite to that of the remplissage technique, creating a lift-up effect on the inferior capsule. The procedure achieved closure of the axillary pouch and increased the contact between the graft, the subscapularis muscle, and the residual capsule.
In conclusion, we think that this technique could be a valid and safer alternative to the arthroscopic or open Latarjet procedures. Moreover, this procedure is a low-risk technique that can be performed using only 3 portals and not 5 as for the arthroscopic Latarjet; graft compression is perpendicular and not oblique allowing a better healing; the present technique is more anatomic, not modifying the coracoacromial arch (Table 2). Finally, the use of a preformed graft could consistently reduce the surgical time. The association of both procedures can be easily performed after an adequate training by surgeons having a good skills level for arthroscopic shoulder surgery.
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
|
|
Footnotes
The authors report the following potential conflicts of interest or sources of funding: E.T. receives grants, personal fees, and nonfinancial support from Smith & Nephew, during the conduct of the study; and grants, personal fees, and nonfinancial support from Smith & Nephew, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic subscapularis augmentation and bone block technique consisting of a bone graft associated with a subscapularis tenodesis for treating glenohumeral instability with glenoid bone loss and anterior capsulolabral deficiency. In this procedure (performed in the lateral decubitus position), 2 glenoid tunnels are set up from the posterior to the anterior side using a dedicated bone block guide, and 4 buttons are used to fix the graft to the glenoid. The subscapularis tenodesis is performed using a suture tape anchor. At the end of the procedure, the humeral head is recentered.
References
- 1.Alkaduhimi H., van der Linde J.A., Willigenburg N.W., Paulino Pereira N.R., van Deurzen D.F., van den Bekerom M.P. Redislocation risk after an arthroscopic Bankart procedure in collision athletes: A systematic review. J Shoulder Elbow Surg. 2016;25:1549–1558. doi: 10.1016/j.jse.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 2.Arciero R.A., Parrino A., Bernhardson A.S. The effect of a combined glenoid and Hill-Sachs defect on glenohumeral stability: A biomechanical cadaveric study using 3-dimensional modeling of 142 patients. Am J Sports Med. 2015;43:1422–1429. doi: 10.1177/0363546515574677. [DOI] [PubMed] [Google Scholar]
- 3.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 4.Di Giacomo G., de Gasperis N., Scarso P. Bipolar bone defect in the shoulder anterior dislocation. Knee Surg Sports Traumatol Arthrosc. 2016;24:479–488. doi: 10.1007/s00167-015-3927-7. [DOI] [PubMed] [Google Scholar]
- 5.Shin S.J., Koh Y.W., Bui C. What is the critical value of glenoid bone loss at which soft tissue Bankart repair does not restore glenohumeral translation, restricts range of motion, and leads to abnormal humeral head position? Am J Sports Med. 2016;44:2784–2791. doi: 10.1177/0363546516656367. [DOI] [PubMed] [Google Scholar]
- 6.Symeonides P.P. Reconsideration of the Putti-Platt procedure and its mode of action in recurrent traumatic anterior dislocation of the shoulder. Clin Orthop Relat Res. 1989;246:8–15. [PubMed] [Google Scholar]
- 7.Symeonides P.P. The significance of the subscapularis muscle in the pathogenesis of recurrent anterior dislocation of the shoulder. J Bone Joint Surg Br. 1972;54:476–483. [PubMed] [Google Scholar]
- 8.Marco S.M., Lafuente J.L.Á., Ibán M.A.R., Heredia J.D. Controversies in the surgical management of shoulder instability: Associated soft tissue procedures. Open Orthop J. 2017;11:989–1000. doi: 10.2174/1874325001711010989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonazza N.A., Liu G., Leslie D.L., Dhawan A. Trends in surgical management of shoulder instability. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117712476. 2325967117712476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cautiero F., Russo R., Di Pietto F., Sabino G. Computerized tomographic assessment and clinical evaluation in shoulder instability treated with the Latarjet-Patte procedure using one screw and washer. Muscles Ligaments Tendons J. 2017;7:26–33. doi: 10.11138/mltj/2017.7.1.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alvi H.M., Monroe E.J., Muriuki M., Verma R.N., Marra G., Saltzman M.D. Latarjet fixation: A cadaveric biomechanical study evaluating cortical and cannulated screw fixation. Orthop J Sports Med. 2016;4 doi: 10.1177/2325967116643533. 2325967116643533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fortun C.M., Wong I., Burns J.P. Arthroscopic iliac crest bone grafting to the anterior glenoid. Arthrosc Tech. 2016;5:e907–e912. doi: 10.1016/j.eats.2016.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cole B.J., Warner J.J. Arthroscopic versus open Bankart repair for traumatic anterior shoulder instability. Clin Sports Med. 2000;19:19–48. doi: 10.1016/s0278-5919(05)70294-5. [DOI] [PubMed] [Google Scholar]
- 14.Degen R.M., Camp C.L., Werner B.C., Dines D.M., Dines J.S. Trends in bone-block augmentation among recently trained orthopaedic surgeons treating anterior shoulder instability. J Bone Joint Surg Am. 2016;98:e56. doi: 10.2106/JBJS.15.01478. [DOI] [PubMed] [Google Scholar]
- 15.Cole B.J., L'Insalata J., Irrgang J., Warner J.J. Comparison of arthroscopic and open anterior shoulder stabilization: A two to six-year follow-up study. J Bone Joint Surg Am. 2000;82:1108–1114. doi: 10.2106/00004623-200008000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Field L., Savoie F., Griffith P. A comparison of open and arthroscopic Bankart repair. J Shoulder Elbow Surg. 1999;8:195. [Google Scholar]
- 17.Kleiner M.T., Payne W.B., McGarry M.H., Tibone J.E., Lee T.Q. Biomechanical comparison of the Latarjet procedure with and without capsular repair. Clin Orthop Surg. 2016;8:84–91. doi: 10.4055/cios.2016.8.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lafosse L., Lejeone E., Bouchard A., Kakuda C., Gobezie R., Kochhar T. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy. 2007;23:1242.e1–1242.e5. doi: 10.1016/j.arthro.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 19.Provencher M.T., Mologne T.S., Hongo M., Zhao K., Tasto J.P., An K.N. Arthroscopic versus open rotator interval closure: Biomechanical evaluation of stability and motion. Arthroscopy. 2007;23:583–592. doi: 10.1016/j.arthro.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 20.Wolf E.M., Arianjam A. Hill-Sachs remplissage, an arthroscopic solution for the engaging Hill-Sachs lesion: 2- to 10-year follow-up and incidence of recurrence. J Shoulder Elbow Surg. 2014;23:814–820. doi: 10.1016/j.jse.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 21.Allain J., Goutallier D., Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am. 1998;80:841–852. doi: 10.2106/00004623-199806000-00008. [DOI] [PubMed] [Google Scholar]
- 22.An V.V., Sivakumar B.S., Phan K., Trantalis J. A systematic review and meta-analysis of clinical and patient-reported outcomes following two procedures for recurrent traumatic anterior instability of the shoulder: Latarjet procedure vs. Bankart repair. J Shoulder Elbow Surg. 2016;25:853–863. doi: 10.1016/j.jse.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 23.Cassagnaud X., Maynou C., Mestdagh H. Résultats cliniques et tomodensitométriques d’une série continue de 106 butées de Latarjet-Patte au recul moyen de 7.5 ans. Rev Chir Orthop Reparatrice Appar Mot. 2003;89:683–692. [PubMed] [Google Scholar]
- 24.Latarjet M. [Treatment of recurrent dislocation of the shoulder] Lyon Chir. 1954;49:994–997. [PubMed] [Google Scholar]
- 25.Matton D., Van Looy F., Geens S. Recurrent anterior dislocations of the shoulder joint treated by the Bristow-Latarjet procedure: Historical review, operative technique and results. Acta Orthop Belg. 1992;58:16–22. [PubMed] [Google Scholar]
- 26.Russo R., Togo F., Jannelli E. The surgical treatment of recurrent anterior dislocation of the shoulder. Ital J Orthop Traumatol. 1990;16:183–189. [PubMed] [Google Scholar]
- 27.Russo R., Togo F., Vernaglia Lombardi L., Ciccarelli M. Latarjet and Latarjet Patte technique treating antero inferior shoulder instability. Ital J Orthop Traumatol. 1998;24:444–449. Risultati a distanza su una casistica di 211 pazienti. ISSN:0390-0134. [Google Scholar]
- 28.Steffen V., Hertel R. Rim reconstruction with autogenous iliac crest for anterior glenoid deficiency: Forty-three instability cases followed for 5-19 years. J Shoulder Elbow Surg. 2013;22:550–555. doi: 10.1016/j.jse.2012.05.038. [DOI] [PubMed] [Google Scholar]
- 29.Torg J.S., Balduini F.C., Bonci C. A modified Bristow-Helfet-May procedure for recurrent dislocation and subluxation of the shoulder: Report of two hundred and twelve cases. J Bone Joint Surg Am. 1987;69:904–913. [PubMed] [Google Scholar]
- 30.Vander Maren C., Geulette B., Lewalle J. [Coracoid process abutment according to Latarjet versus the Bankart operation: A comparative study of the results in 50 cases] Acta Orthop Belg. 1993;59:147–155. [in French] [PubMed] [Google Scholar]
- 31.Tasaki A., Morita W., Yamakawa A. Combined arthroscopic Bankart repair and coracoid process transfer to anterior glenoid for shoulder dislocation in rugby players: Evaluation based on ability to perform sport-specific movements effectively. Arthroscopy. 2015;31:1693–1701. doi: 10.1016/j.arthro.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 32.Athwal G.S., Meislin R., Getz C., Weinstein D., Favorito P. Short-term complications of the arthroscopic Latarjet procedure: A North American experience. Arthroscopy. 2016;32:1965–1970. doi: 10.1016/j.arthro.2016.02.022. [DOI] [PubMed] [Google Scholar]
- 33.Douoguih W.A., Goodwin D., Churchill R., Paulus M., Maxwell A. Conjoined tendon transfer for traumatic anterior glenohumeral instability in patients with large bony defects and anterior capsulolabral deficiency. Arthroscopy. 2018;34:12–20. doi: 10.1016/j.arthro.2017.06.044. [DOI] [PubMed] [Google Scholar]
- 34.Pauzenberger L., Dyrna F., Obopilwe E. Biomechanical evaluation of glenoid reconstruction with an implant-free J-bone graft for anterior glenoid bone loss. Am J Sports Med. 2017;45:2849–2857. doi: 10.1177/0363546517716927. [DOI] [PubMed] [Google Scholar]
- 35.Taverna E., Golanò P., Pascale V., Battistella F. An arthroscopic bone graft procedure for treating anterior-inferior glenohumeral instability. Knee Surg Sports Traumatol Arthrosc. 2008;16:872–875. doi: 10.1007/s00167-008-0541-y. [DOI] [PubMed] [Google Scholar]
- 36.Taverna E., D'Ambrosi R., Perfetti C., Garavaglia G. Arthroscopic bone graft procedure for anterior-inferior glenohumeral instability. Arthrosc Tech. 2014;3:e653–e660. doi: 10.1016/j.eats.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Russo R., Della Rotonda G., Cautiero F. Arthroscopic Bankart repair associated with subscapularis augmentation (ASA) versus open Latarjet to treat recurrent anterior shoulder instability with moderate glenoid bone loss: Clinical comparison of two series. Musculoskelet Surg. 2017;101:75–83. doi: 10.1007/s12306-016-0446-8. [DOI] [PubMed] [Google Scholar]
- 38.Maiotti M., Massoni C. Arthroscopic augmentation with subscapularis tendon in anterior shoulder instability with capsulolabral deficiency. Arthrosc Tech. 2013;2:e303–e310. doi: 10.1016/j.eats.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maiotti M., Russo R., Zanini A., Schreoter S., Massoni C., Bianchedi D. Arthroscopic Bankart repair and subscapularis augmentation: An alternative technique treating anterior shoulder instability with bone loss. J Shoulder Elbow Surg. 2016;25:898–906. doi: 10.1016/j.jse.2015.09.025. [DOI] [PubMed] [Google Scholar]
- 40.Maiotti M., Massoni C., Russo R., Zanini A., Schreoter S., Bianchedi D. Arthroscopic subscapularis augmentation of Bankart repair in chronic anterior shoulder instability with bone loss less than 25% and capsular deficiency: Clinical multicenter study. Arthroscopy. 2017;33:902–909. doi: 10.1016/j.arthro.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 41.Schröter S., Krämer M., Welke B. The effect of the arthroscopic augmentation of the subscapularis tendon on shoulder instability and range of motion: A biomechanical study. Clin Biomech. 2016;38:75–83. doi: 10.1016/j.clinbiomech.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 42.Baudi P., Righi P., Bolognesi D. How to identify and calculate glenoid bone deficit. Chir Organi Mov. 2005;90:145–152. [PubMed] [Google Scholar]
- 43.Kempf J.F., Gleyze P., Iserin A., Nerisson D. Arthroscopie. Elsevier; Paris: 1999. Traitement arthroscopique des instabilités chroniques antérieures de l’épaule; pp. 357–372. [PubMed] [Google Scholar]
- 44.Morrey B.F., Janes J.M. Recurrent anterior dislocation of the shoulder: Long-term follow-up of the Putti-Platt and Bankart procedures. J Bone Joint Surg Am. 1976;58:252–256. [PubMed] [Google Scholar]
- 45.Rowe C., Patel D., Southmayd W. The Bankart procedure: A long-term end result study. J Bone Joint Surg Am. 1978;60:1–16. [PubMed] [Google Scholar]
- 46.Wymenga A.B., Morshuis W.J. Factors influencing the early results of the Bristow-Latarjet technique. Acta Orthop Belg. 1988;54:76–82. [PubMed] [Google Scholar]
- 47.Klungsøyr P.J., Guldal F., Vagstad T., Klungsøyr J.A. A new subscapular sling operation to stabilize the shoulder. A cadaver study. J Exp Orthop. 2015;2:12. doi: 10.1186/s40634-015-0028-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic subscapularis augmentation and bone block technique consisting of a bone graft associated with a subscapularis tenodesis for treating glenohumeral instability with glenoid bone loss and anterior capsulolabral deficiency. In this procedure (performed in the lateral decubitus position), 2 glenoid tunnels are set up from the posterior to the anterior side using a dedicated bone block guide, and 4 buttons are used to fix the graft to the glenoid. The subscapularis tenodesis is performed using a suture tape anchor. At the end of the procedure, the humeral head is recentered.